Online Physical Exercise and Group Sessions to Increase and Maintain Physical Activity in Individuals with Type 2 Diabetes: A Single-Arm Feasibility Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
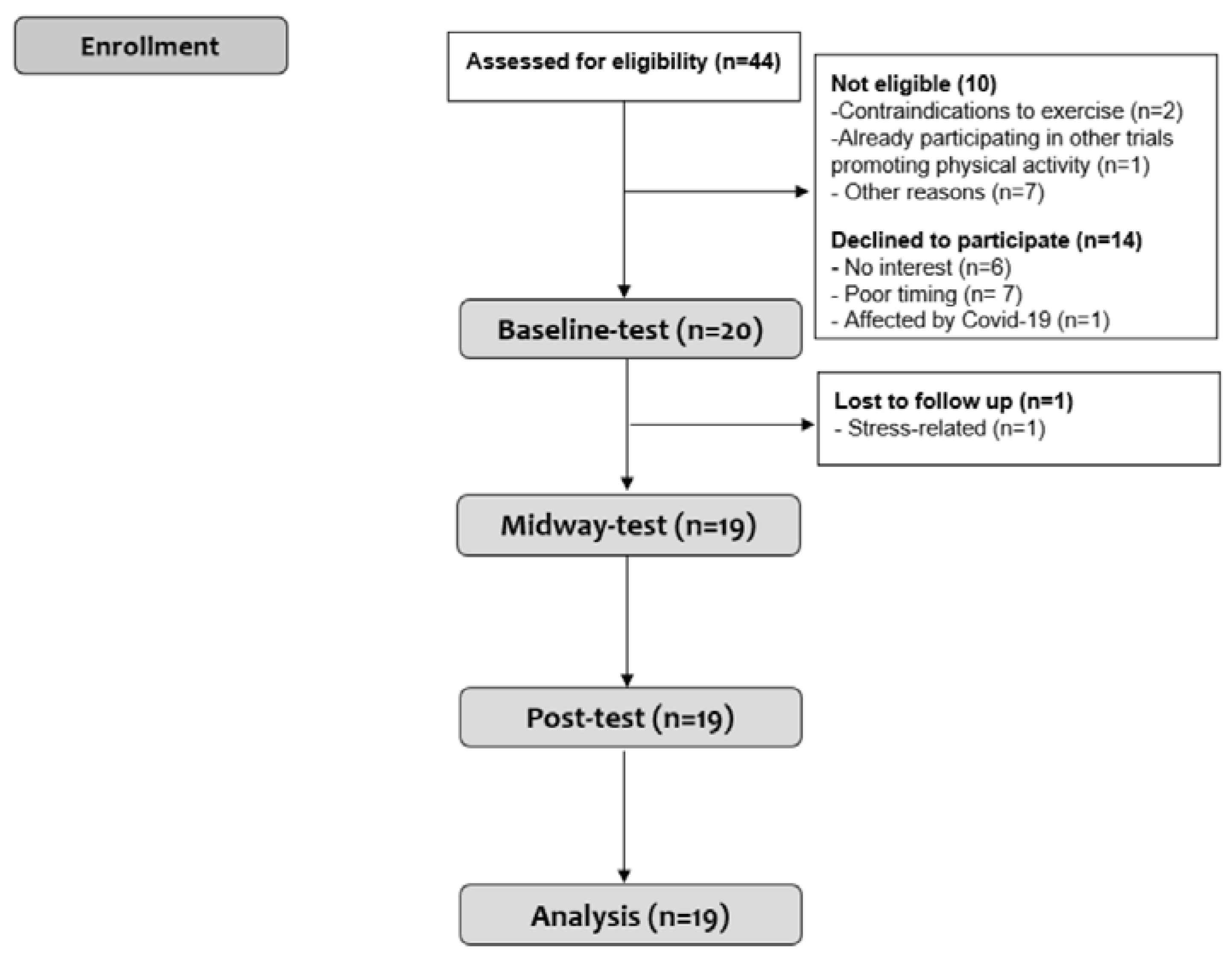
2.2. Participants
2.3. Study Intervention
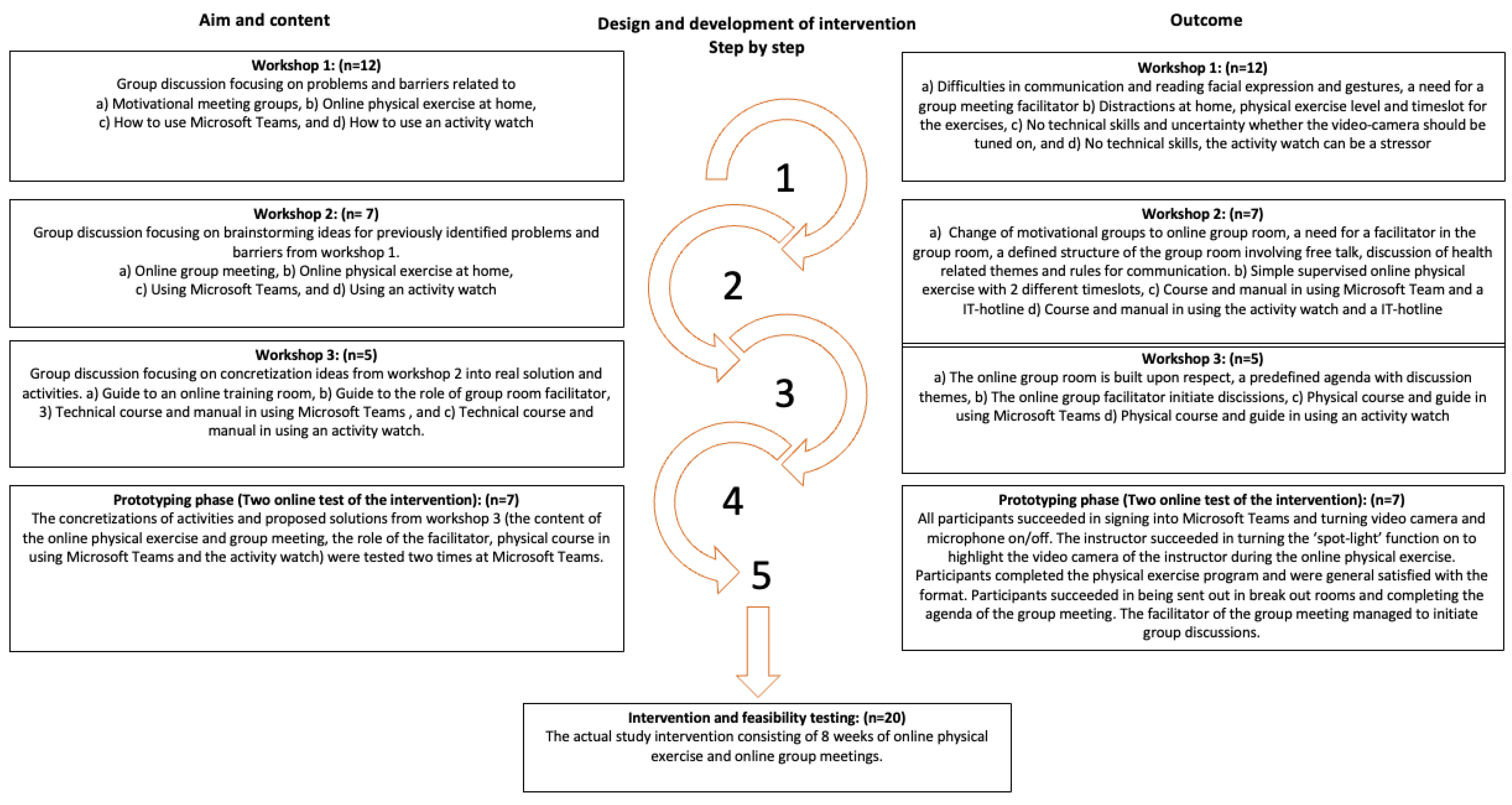
2.3.1. Development of the Intervention
2.3.2. Intervention
2.4. Outcomes
2.4.1. Primary outcomes
2.4.2. Secondary Outcomes
Objective Outcomes
Self-Reported Outcomes
Participant Feedback
2.5. Sample Size
2.6. Statistical Analysis
2.7. Deviations from the Protocol
3. Results
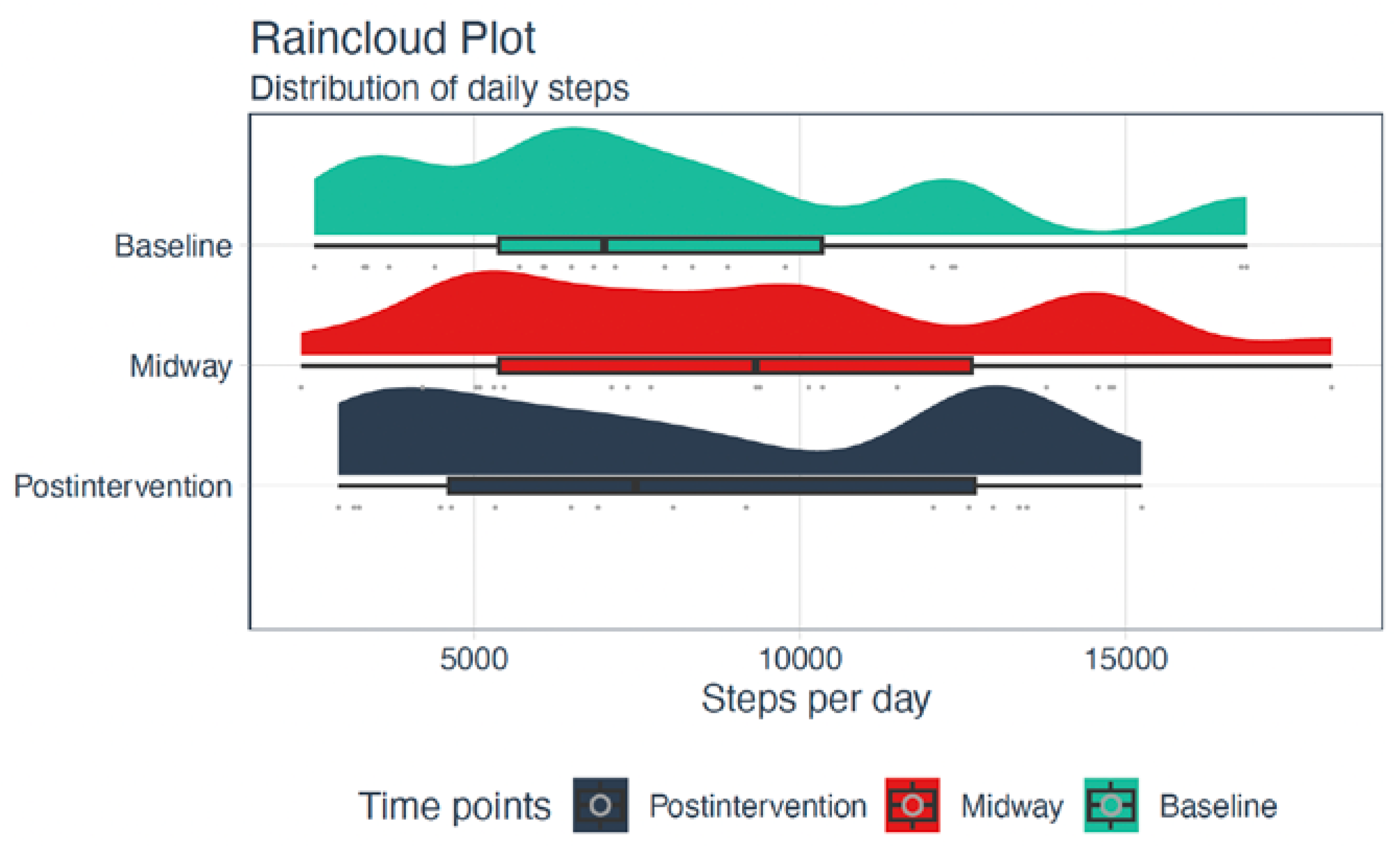
3.1. Primary Outcomes
3.2. Secondary Outcomes
3.3. Participant Feedback
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Davies, M.J.; Aroda, V.R.; Collins, B.S.; Gabbay, R.A.; Green, J.; Maruthur, N.M.; Rosas, S.E.; Del Prato, S.; Mathieu, C.; Mingrone, G.; et al. Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2022, 45, 2753–2786. [Google Scholar] [CrossRef]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020.
- American Diabetes Association Standards of Medical Care in Diabetes—2022 Abridged for Primary Care Providers. Clin. Diabetes 2022, 40, 10–38. [CrossRef] [PubMed]
- Ried-Larsen, M.; Johansen, M.Y.; MacDonald, C.S.; Hansen, K.B.; Christensen, R.; Wedell-Neergaard, A.S.; Pilmark, N.S.; Langberg, H.; Vaag, A.A.; Pedersen, B.K.; et al. Type 2 diabetes remission 1 year after an intensive lifestyle intervention: A secondary analysis of a randomized clinical trial. Diabetes Obes. Metab. 2019, 21, 2257–2266. [Google Scholar] [CrossRef]
- Schmidt, S.K.; Hemmestad, L.; MacDonald, C.S.; Langberg, H.; Valentiner, L.S. Motivation and Barriers to Maintaining Lifestyle Changes in Patients with Type 2 Diabetes after an Intensive Lifestyle Intervention (The U-TURN Trial): A Longitudinal Qualitative Study. Int. J. Environ. Res. Public Health 2020, 17, 7454. [Google Scholar] [CrossRef]
- Thorsen, I.K.; Kayser, L.; Teglgaard Lyk-Jensen, H.; Rossen, S.; Ried-Larsen, M.; Midtgaard, J. “I Tried Forcing Myself to do It, but Then It Becomes a Boring Chore”: Understanding (dis)engagement in Physical Activity Among Individuals With Type 2 Diabetes Using a Practice Theory Approach. Qual. Health Res. 2022, 32, 520–530. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, N.L.; Gold, R.S. The promise and challenge of eHealth interventions. Am. J. Health Behav. 2002, 26, 494–503. [Google Scholar] [CrossRef]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef]
- Wilke, J.; Mohr, L.; Yuki, G.; Bhundoo, A.K.; Jiménez-Pavón, D.; Laiño, F.; Murphy, N.; Novak, B.; Nuccio, S.; Ortega-Gómez, S.; et al. Train at home, but not alone: A randomised controlled multicentre trial assessing the effects of live-streamed tele-exercise during COVID-19-related lockdowns. Br. J. Sports Med. 2022, 56, 667–675. [Google Scholar] [CrossRef]
- Halbrook, M.; Blom, L.C.; Hurley, K.; Bell, R.J.; Holden, J.E. Relationships among motivation, gender, and cohesion in a sample of collegiate athletes. J. Sport Behav. 2012, 35, 61–77. [Google Scholar]
- Leask, C.F.; Sandlund, M.; Skelton, D.A.; Altenburg, T.M.; Cardon, G.; Chinapaw, M.J.M.; De Bourdeaudhuij, I.; Verloigne, M.; Chastin, S.F.M. and on behalf of theGrandStand, Safe Step and Teenage Girls on the Move Research Groups. Framework, principles and recommendations for utilising participatory methodologies in the co-creation and evaluation of public health interventions. Res. Involv. Engagem. 2019, 5, 2. [Google Scholar] [CrossRef]
- Hawkins, J.; Madden, K.; Fletcher, A.; Midgley, L.; Grant, A.; Cox, G.; Moore, L.; Campbell, R.; Murphy, S.; Bonell, C.; et al. Development of a framework for the co-production and prototyping of public health interventions. BMC Public Health 2017, 17, 689. [Google Scholar] [CrossRef]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016, 2, 64. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K.; Saltin, B. Evidence for prescribing exercise as therapy in chronic disease. Scand. J. Med. Sci. Sports 2006, 16 (Suppl. 1), 3–63. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.W. Stakeholder analysis: A pivotal practice of successful projects. In Proceedings of the Paper presented at Project Management Institute Annual Seminars & Symposium, Houston, TX, USA, 7–16 September 2000; Project Management Institute: Newtown Square, PA, USA, 2000. [Google Scholar]
- Redman, S.; Greenhalgh, T.; Adedokun, L.; Staniszewska, S.; Denegri, S. Co-production of knowledge: The future. BMJ 2021, 372, n434. [Google Scholar] [CrossRef] [PubMed]
- Rhon, D.I.; Fritz, J.M.; Kerns, R.D.; McGeary, D.D.; Coleman, B.C.; Farrokhi, S.; Burgess, D.J.; Goertz, C.M.; Taylor, S.L.; Hoffmann, T. TIDieR-telehealth: Precision in reporting of telehealth interventions used in clinical trials—Unique considerations for the Template for the Intervention Description and Replication (TIDieR) checklist. BMC Med. Res. Methodol. 2022, 22, 161. [Google Scholar] [CrossRef]
- Jelleyman, C.; Yates, T.; O’Donovan, G.; Gray, L.J.; King, J.A.; Khunti, K.; Davies, M.J. The effects of high-intensity interval training on glucose regulation and insulin resistance: A meta-analysis. Obes. Rev. 2015, 16, 942–961. [Google Scholar] [CrossRef]
- Snowling, N.J.; Hopkins, W.G. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: A meta-analysis. Diabetes Care 2006, 29, 2518–2527. [Google Scholar] [CrossRef]
- Borg, G. Perceived exertion as an indicator of somatic stress. Scand. J. Rehabil. Med. 1970, 2, 92–98. [Google Scholar]
- Schut, H.A.; Stam, H.J. Goals in rehabilitation teamwork. Disabil. Rehabil. 1994, 16, 223–226. [Google Scholar] [CrossRef]
- Avery, K.N.; Williamson, P.R.; Gamble, C.; O’Connell Francischetto, E.; Metcalfe, C.; Davidson, P.; Williams, H.; Blazeby, J.M. Informing efficient randomised controlled trials: Exploration of challenges in developing progression criteria for internal pilot studies. BMJ Open 2017, 7, e013537. [Google Scholar] [CrossRef]
- Axivity Ltd. AX3 User Manual. Available online: https://axivity.com/userguides/ax3/ (accessed on 5 February 2022).
- Common Terminology Criteria for Adverse Events (CTCAE). Available online: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm (accessed on 5 February 2022).
- What is a Serious Adverse Event? Available online: https://www.fda.gov/safety/reporting-serious-problems-fda/what-serious-adverse-event (accessed on 11 February 2022).
- Brønd, J.C.; Andersen, L.B.; Arvidsson, D. Generating ActiGraph Counts from Raw Acceleration Recorded by an Alternative Monitor. Med. Sci. Sports Exerc. 2017, 49, 2351–2360. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, A.; Del Din, S.; Barry, G.; Mathers, J.C.; Rochester, L. Instrumenting gait with an accelerometer: A system and algorithm examination. Med. Eng. Phys. 2015, 37, 400–407. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- World Health Organization (Regional Office for Europe). Wellbeing Measures in Primary Health Care/the DepCare Project: Report on a WHO Meeting: Stockholm, Sweden, 12–13 February 1998; World Health Organization (Regional Office for Europe): Copenhagen, Denmark, 1998.
- Bayliss, E.A.; Ellis, J.L.; Steiner, J.F. Seniors’ self-reported multimorbidity captured biopsychosocial factors not incorporated into two other data-based morbidity measures. J. Clin. Epidemiol. 2009, 62, 550–557.e551. [Google Scholar] [CrossRef] [PubMed]
- Lorig, K.R.; Sobel, D.S.; Ritter, P.L.; Laurent, D.; Hobbs, M. Effect of a self-management program on patients with chronic disease. Eff. Clin. Pract. 2001, 4, 256–262. [Google Scholar] [PubMed]
- Lasgaard, M. Reliability and validity of the Danish version of the UCLA Loneliness Scale. Personality and Individual Differences 2007, 42, 1359–1366. [Google Scholar] [CrossRef]
- Julious, S. Sample size of 12 per group rue of thumb for a pilot study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Lyngbaek, M.P.P.; Legaard, G.E.; Bennetsen, S.L.; Feineis, C.S.; Rasmussen, V.; Moegelberg, N.; Brinkløv, C.F.; Nielsen, A.B.; Kofoed, K.S.; Lauridsen, C.A.; et al. The effects of different doses of exercise on pancreatic β-cell function in patients with newly diagnosed type 2 diabetes: Study protocol for and rationale behind the "DOSE-EX" multi-arm parallel-group randomised clinical trial. Trials 2021, 22, 244. [Google Scholar] [CrossRef]
- Diabetesforeningen. Livet Med Diabetes; Diabetesforeningen: Moscow, Russia, 2021. [Google Scholar]
- Mortensen, S.R.; Kristensen, P.L.; Grøntved, A.; Ried-Larsen, M.; Lau, C.; Skou, S.T. Determinants of physical activity among 6856 individuals with diabetes: A nationwide cross-sectional study. BMJ Open Diabetes Res. Care 2022, 10, e002935. [Google Scholar] [CrossRef]
- Jansen, T.; Rademakers, J.; Waverijn, G.; Verheij, R.; Osborne, R.; Heijmans, M. The role of health literacy in explaining the association between educational attainment and the use of out-of-hours primary care services in chronically ill people: A survey study. BMC Health Serv. Res. 2018, 18, 394. [Google Scholar] [CrossRef]
- van Kessel, R.; Wong, B.L.H.; Clemens, T.; Brand, H. Digital health literacy as a super determinant of health: More than simply the sum of its parts. Internet Interv. 2022, 27, 100500. [Google Scholar] [CrossRef]
- Statens Serum Institut Alment Praktiserende Lægers Kontakt Med Patienter Med Type 2 Diabetes; Statens Serum Institut: Copenhagen, Denmark, 2015.
- Christensen, J.R.; Hesseldal, L.; Olesen, T.B.; Olsen, M.H.; Jakobsen, P.R.; Laursen, D.H.; Lauridsen, J.T.; Nielsen, J.B.; Søndergaard, J.; Brandt, C.J. Long-term weight loss in a 24-month primary care-anchored telehealth lifestyle coaching program: Randomized controlled trial. J. Telemed. Telecare 2022, 28, 764–770. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.C.; Coombes, J.S.; Jungbluth Rodriguez, K.; Hickman, I.J.; Keating, S.E. Effectiveness of exercise via telehealth for chronic disease: A systematic review and meta-analysis of exercise interventions delivered via videoconferencing. Br. J. Sport. Med. 2022, 56, 1042–1052. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, N.; Gubbels, S.P.; Schwartz, S.R.; Edlow, J.A.; El-Kashlan, H.; Fife, T.; Holmberg, J.M.; Mahoney, K.; Hollingsworth, D.B.; Roberts, R.; et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngol. Head. Neck Surg. 2017, 156, S1–S47. [Google Scholar] [CrossRef] [PubMed]
- Migueles, J.H.; Cadenas-Sanchez, C.; Ekelund, U.; Delisle Nyström, C.; Mora-Gonzalez, J.; Löf, M.; Labayen, I.; Ruiz, J.R.; Ortega, F.B. Accelerometer Data Collection and Processing Criteria to Assess Physical Activity and Other Outcomes: A Systematic Review and Practical Considerations. Sports Med. 2017, 47, 1821–1845. [Google Scholar] [CrossRef]

| Outcome | Green | Amber | Red |
|---|---|---|---|
| Participant recruitment | 24 participants recruited within 3 months | Fewer than 24 participants recruited within 3 months | Fewer than 12 participants recruited within 3 months |
| Completion of intervention | Minimum 75% of the participants complete postintervention | Minimum 50% of the participants complete postintervention | Fewer than 50% of the participants complete postintervention |
| Adherence to online physical exercise sessions 1 | Minimum 75% of the participants complete more than half of the online physical exercise sessions | Minimum 50% of the participants complete more than half of the physical exercise sessions | Fewer than 50% of the participants complete more than half of the physical exercise sessions |
| Adherence to online group meetings 2 | Minimum 75% of the participants complete more than half of the group meeting sessions | Minimum 50% of the participants complete more than half of the group meeting sessions | Fewer than 50% of the participants complete more than half of the group meeting sessions |
| Adherence to activity goals 3 | Minimum 75% of the participants set goals | Minimum 50% of the participants set goals | Fewer than 50% of the participants set goals |
| Burden of objectively measured physical activity | Minimum 80% of the participants did NOT find the objective outcome measures of the study so difficult that they would not participate in the study again | Minimum 70% of the participants did NOT find the objective outcome measures of the study so difficult that they would not participate in the study again | Fewer than 70% of the participants did NOT find the objective outcome measures of the study so difficult that they would not participate in the study again |
| Improvement of physical activity 4 | Minimum 50% of the participants have achieved improvements in physical activity at postintervention | Minimum 25% of the participants have achieved improvements in physical activity at postintervention | Fewer than 25% of the participants have achieved improvements in physical activity at postintervention |
| Adverse events | No or minor adverse events related to the intervention at postintervention | Fewer than five serious adverse events related to the intervention at postintervention | Five or more serious adverse events related to the intervention at postintervention |
| Characteristics | |
|---|---|
| Age, years | 60.4 ± 8.7 |
| Women, n (%) | 8 (40.0) |
| Ethnicity, n (%) | 18 (90.0) |
| Living alone, n (%) | 6 (30.0) |
| Educational level, n (%) | |
| Primary education | 3 (15.0) |
| Upper secondary or vocational | 7 (35.0) |
| Higher education | 10 (50.0) |
| BMI, n (%) | |
| Underweight/Normal | 0 |
| Overweight | 8 (40.0) |
| Obese Class I | 8 (40.0) |
| Obese Class II | 3 (15.0) |
| Obese Class III | 1 (5.0) |
| Diet score (healthy/medium healthy/unhealthy) a | 7/10/3 |
| Alcohol consumption (no alcohol/below risk group/above risk group) b | 7/12/1 |
| Smoking status (smoker/ex-smoker/never smoked) | 1/10/9 |
| Adherence to WHO recommendations on weekly physical activity c, n (%) | |
| Following recommendations | 5 (25.0) |
| Not following recommendations | 15 (75.0) |
| Adherence to recommendations on daily physical activity d, n (%) | |
| Inactivity | 3 (15.0) |
| Some physical activity | 13 (65.0) |
| Sufficient physical activity | 4 (20.0) |
| WHO-5-Well-Being Index total score, (0–100) | 78 [72–80] |
| Bayliss burden of illness measure | |
| Median number of comorbidities reported | 4 [2.5–6] |
| Median disease burden reported | 5.5 [1.5–9] |
| SEMCD6, (0–10) | 8 [5.7–8.7] |
| PSS total score, n (%) | |
| Low perceived stress | 1 (5.0) |
| Moderate perceived stress | 16 (80.0) |
| High perceived stress | 3 (15.0) |
| Loneliness scale, (3–9) | 3 [3–5] |
| Self-reported HbA1c (mmol/mol) * | 47 [38–48] |
| Research Progression Criteria | Evaluation | |
|---|---|---|
| Participant recruitment, actual n/desired n | 20/24 | Amber |
| Participants who completed the intervention, n (%) * | 19/20 (95.0) | Green |
| Adherence to online physical exercise sessions | ||
| Participants who completed half of the online physical exercise sessions, n (%) | 17/19 (89.5) | Green |
| Adherence to online group meetings | ||
| Participants who completed half of the online group meetings, n (%) | 16/19 (84.2) | Green |
| Adherence to goalsetting | ||
| Participants who set activity goals, n (%) | 19/19 (100.0) | Green |
| Burden of objectively measured physical activity | ||
| Participants who did not find the attachment and shipping too time-consuming, n (%) | 17/19 (89.5) | Green |
| Participants who found the numbers of days wearing the accelerometer appropriate, n (%) | 15/19 (79.9) | Amber |
| Improvement of physical activity | ||
| Participants who improved physical activity from baseline to postintervention, n (%) ** | 10/19 (62.5) | Green |
| Adverse events | ||
| Participants who experienced minor adverse events, n (%) | 9/19 | Green |
| Participants who experienced serious adverse events, n (%) | 1/19 | Amber |
| Baseline (before Week 1) | Midway (after Week 4) | Postintervention (after Week 8) | |
|---|---|---|---|
| Total | |||
| SB | 10.7 [9.4–11.6] | 10.2 [8.9–10.5] | 10.3 [9.0–10.8] |
| LPA | 136.8 [111.7–155.4] | 133.9 [109.5–162.6] | 129.2 [113.7–149.7] |
| MPA | 9.2 [5.7–18.9] | 11.7 [4.7–16.5] | 12.6 [4.6–29.5] |
| VPA | 0.3 [0.1–1.2] | 0.3 [0.1–0.9] | 0.3 [0.1–0.6] |
| MVPA | 11.8 [5.8–22.2] | 14.3 [7.2–19.8] | 15.5 [6.2–30.5] |
| Daily steps | 6292 [4044–9336] | 8519 [5197–12068] | 7479 [4569–12780] |
| Weekdays | |||
| SB | 11.4 [9.4–12.9] | 10.6 [7.8–12.0] | 10.9 [7.3–12.6] |
| LPA | 136.8 [108.6–165.5] | 131.0 [109.0–168.7] | 112.3 [76.4–165.5] |
| MPA | 7.9 [3.1–21.4] | 4.8 [1.7–20.5] | 7.0 [1.4–21.5] |
| VPA | 0.2 [0–0.6] | 0.2 [0–0.5] | 0.2 [0–0.4] |
| MVPA | 8.3 [3.5–23.4] | 5.7 [1.8–21.7] | 7.6 [1.8–22.7] |
| Daily steps | 6620.5 [3775–9844] | 7298 [3508–12273] | 5910 [2709–13243] |
| Weekends | |||
| SB | 9.7 [6.1–11.2] | 10.7 [9.3–11.6] | 10.8 [9.2–11.8] |
| LPA | 113.2 [70.7–172.3] | 155.6 [118.5–195.2] | 152.8 [93.7–189.3] |
| MPA | 5.7 [0.8–11.7] | 10.2 [1.8–19.8] | 7.0 [3.3–33.2] |
| VPA | 0.2 [0–0.3] | 0.2 [0–0.5] | 0.2 [0–0.7] |
| MVPA | 6.0 [1.2–12.3] | 11.8 [2.0–23.3] | 9.3 [3.3–37.2] |
| Daily steps | 4468 [1820–9216] | 9405 [5237–14784] | 9786 [4326–14252] |
| Adherence to WHO recommendations on weekly physical activity a | |||
| Following recommendations | 4 (25.0) | 4 (25.0) | 6 (37.5) |
| Not following recommendations | 12 (75.0) | 12 (75.0) | 10 (62.5) |
| Adherence to recommendations on daily physical activity during a week b | |||
| Days with inactivity | 2.5 [1–6.5] | 3 [1–5.5] | 2.5 [1–5.5] |
| Days with some physical activity | 5.5 [2.5–7.5] | 3 [1–5] | 2.5 [1–4] |
| Days with sufficient physical activity | 0.5 [0–3] | 0.5 [0–1.5] | 1.5 [0–3] |
| Baseline (before Week 1) | Postintervention (after Week 8) | |
|---|---|---|
| BMI | 31.2 [28.7–33.7] | 31.2 [28.2–32.7] |
| PSS total score, (0–40) | 20 [18–23] | 19 [17–22] |
| Loneliness scale, (3–9) | 3 [3–5] | 3 [3–5] |
| SEMCD6, (0–10) | 8 [4.8–8.8] | 8.3 [6.7–9.0] |
| WHO-5 Wellbeing Index total score, (0–100) | 80 [72–80] | 80 [72–84] |
| Bayliss burden of illness measure | ||
| Median number of comorbidities | 4 [3–7] | 3 [2–6] |
| Median disease burden reported | 6 [1–9] | 7 [2–14] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mortensen, S.R.; Pedersen, M.E.; Skou, S.T.; Ried-Larsen, M. Online Physical Exercise and Group Sessions to Increase and Maintain Physical Activity in Individuals with Type 2 Diabetes: A Single-Arm Feasibility Study. Int. J. Environ. Res. Public Health 2023, 20, 2893. https://doi.org/10.3390/ijerph20042893
Mortensen SR, Pedersen ME, Skou ST, Ried-Larsen M. Online Physical Exercise and Group Sessions to Increase and Maintain Physical Activity in Individuals with Type 2 Diabetes: A Single-Arm Feasibility Study. International Journal of Environmental Research and Public Health. 2023; 20(4):2893. https://doi.org/10.3390/ijerph20042893
Chicago/Turabian StyleMortensen, Sofie Rath, Mathilde Espe Pedersen, Søren T. Skou, and Mathias Ried-Larsen. 2023. "Online Physical Exercise and Group Sessions to Increase and Maintain Physical Activity in Individuals with Type 2 Diabetes: A Single-Arm Feasibility Study" International Journal of Environmental Research and Public Health 20, no. 4: 2893. https://doi.org/10.3390/ijerph20042893
APA StyleMortensen, S. R., Pedersen, M. E., Skou, S. T., & Ried-Larsen, M. (2023). Online Physical Exercise and Group Sessions to Increase and Maintain Physical Activity in Individuals with Type 2 Diabetes: A Single-Arm Feasibility Study. International Journal of Environmental Research and Public Health, 20(4), 2893. https://doi.org/10.3390/ijerph20042893






