Autonomic Function Recovery and Physical Activity Levels in Post-COVID-19 Young Adults after Immunization: An Observational Follow-Up Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
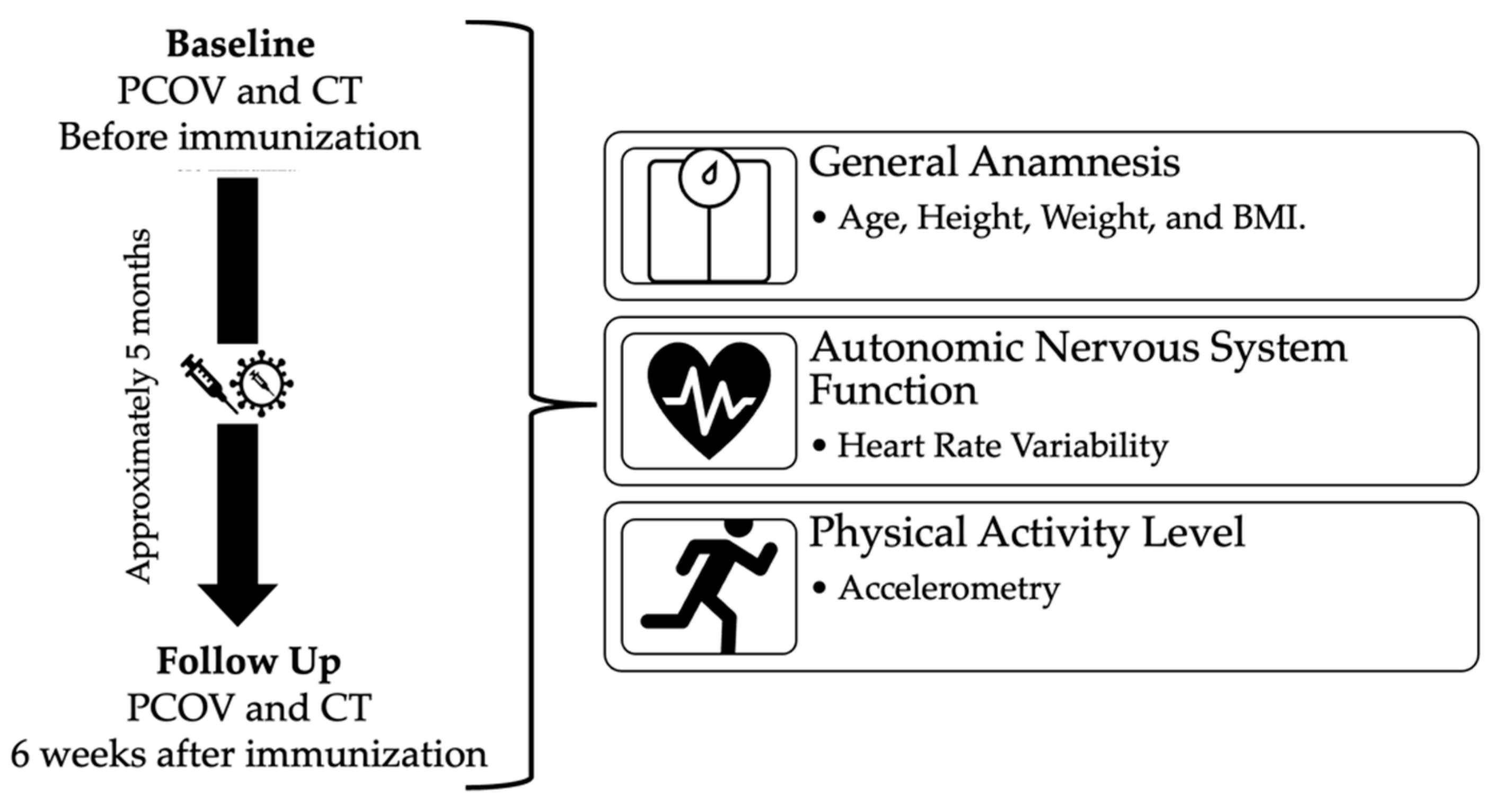
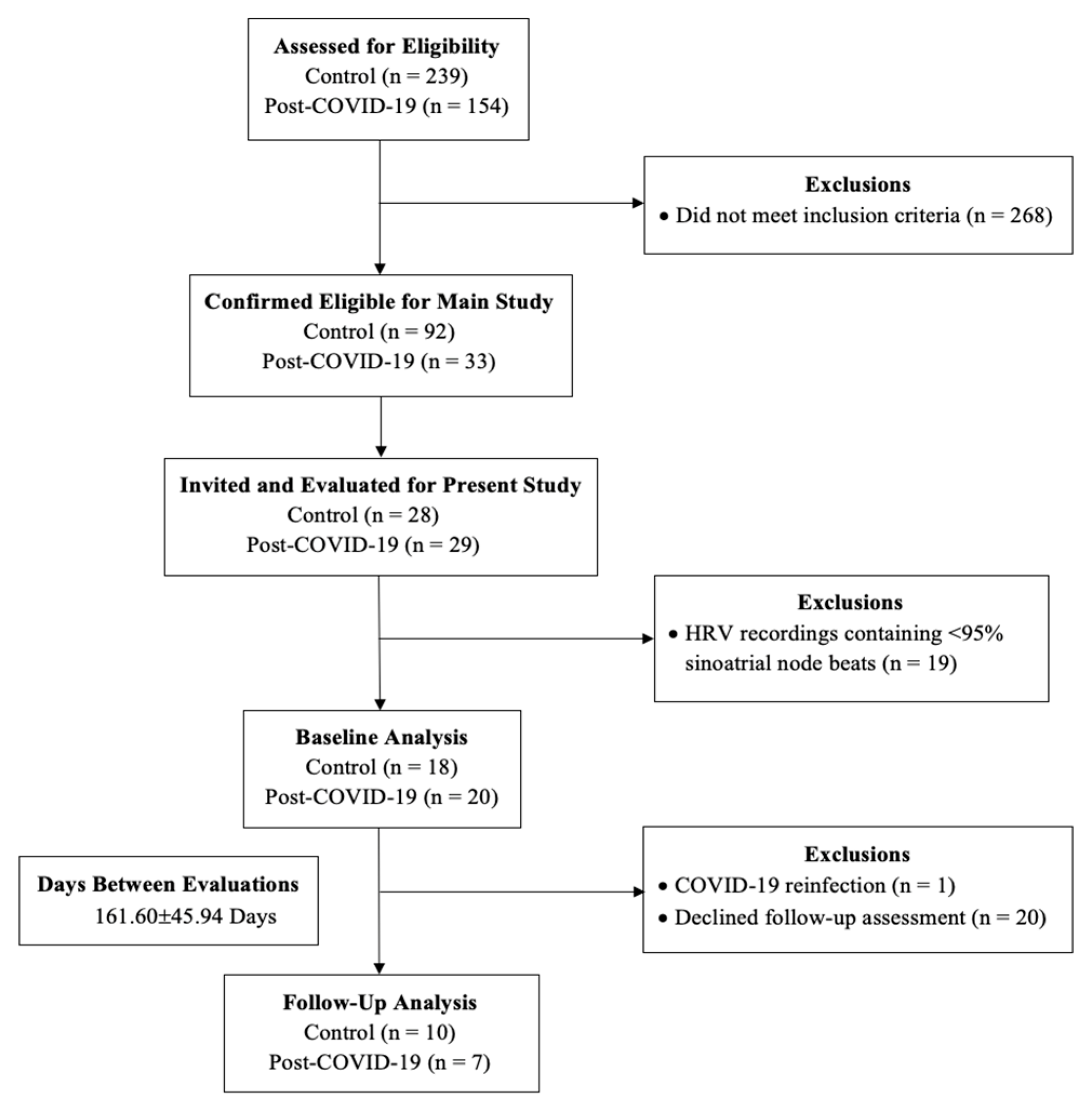
2.2. Study Design
2.3. Evaluations
2.3.1. Body Mass Index
2.3.2. Heart Rate Variability
2.3.3. Physical Activity Level
2.3.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Coronavirus (COVID-19) Dashboard 2022. Available online: https://covid19.who.int/ (accessed on 22 November 2022).
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Torocastro, M.; Panagopoulos, D.; Sutton, R.; Lim, P.B. Autonomic dysfunction in ‘long COVID’: Rationale, physiology and management strategies. Clin. Med. 2021, 21, e63. [Google Scholar] [CrossRef]
- Guilmot, A.; Maldonado Slootjes, S.; Sellimi, A.; Bronchain, M.; Hanseeuw, B.; Belkhir, L.; Yombi, J.C.; De Greef, J.; Pothen, L.; Yildiz, H.; et al. Immune-mediated neurological syndromes in SARS-CoV-2-infected patients. J. Neurol. 2021, 268, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Buoite Stella, A.; Furlanis, G.; Frezza, N.A.; Valentinotti, R.; Ajcevic, M.; Manganotti, P. Autonomic dysfunction in post-COVID patients with and witfhout neurological symptoms: A prospective multidomain observational study. J. Neurol. 2022, 269, 587–596. [Google Scholar] [CrossRef]
- Pan, Y.; Yu, Z.; Yuan, Y.; Han, J.; Wang, Z.; Chen, H.; Wang, S.; Wang, Z.; Hu, H.; Zhou, L.; et al. Alteration of Autonomic Nervous System Is Associated With Severity and Outcomes in Patients With COVID-19. Front. Physiol. 2021, 12, 630038. [Google Scholar] [CrossRef] [PubMed]
- Asarcikli, L.D.; Hayiroglu, M.; Osken, A.; Keskin, K.; Kolak, Z.; Aksu, T. Heart rate variability and cardiac autonomic functions in post-COVID period. J. Interv. Card. Electrophysiol. 2022, 63, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Marques, K.C.; Silva, C.C.; Trindade, S.D.S.; Santos, M.C.S.; Rocha, R.S.B.; Vasconcelos, P.F.D.C.; Quaresma, J.A.S.; Falcão, L.F.M. Reduction of Cardiac Autonomic Modulation and Increased Sympathetic Activity by Heart Rate Variability in Patients With Long COVID. Front. Cardiovasc. Med. 2022, 9, 862001. [Google Scholar] [CrossRef] [PubMed]
- Stute, N.L.; Stickford, J.L.; Province, V.M.; Augenreich, M.A.; Ratchford, S.M.; Stickford, A.S.L. COVID-19 is getting on our nerves: Sympathetic neural activity and haemodynamics in young adults recovering from SARS-CoV-2. J. Physiol. 2021, 599, 4269–4285. [Google Scholar] [CrossRef] [PubMed]
- Freire, A.P.C.F.; Lira, F.S.; Morano, A.E.V.A.; Pereira, T.; Coelho-E-Silva, M.-J.; Caseiro, A.; Christofaro, D.G.D.; Marchioto Júnior, O.; Dorneles, G.P.; Minuzzi, L.G.; et al. Role of Body Mass and Physical Activity in Autonomic Function Modulation on Post-COVID-19 Condition: An Observational Subanalysis of Fit-COVID Study. Int. J. Environ. Res. Public Health 2022, 19, 2457. [Google Scholar] [CrossRef]
- Tenforde, M.W.; Kim, S.S.; Lindsell, C.J.; Billig Rose, E.; Shapiro, N.I.; Files, D.C.; Gibbs, K.W.; Erickson, H.L.; Steingrub, J.S.; Smithline, H.A.; et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health among Outpatients with COVID-19 in a Multistate Health Care Systems Network—United States, March–June 2020; Center for Disease Control and Prevention Stacks: New York, NY, USA, 2020. [Google Scholar]
- Porzionato, A.; Emmi, A.; Barbon, S.; Boscolo-Berto, R.; Stecco, C.; Stocco, E.; Macchi, V.; De Caro, R. Sympathetic activation: A potential link between comorbidities and COVID-19. FEBS J. 2020, 287, 3681–3688. [Google Scholar] [CrossRef]
- Daniela, M.; Catalina, L.; Ilie, O.; Paula, M.; Daniel-Andrei, I.; Ioana, B. Effects of Exercise Training on the Autonomic Nervous System with a Focus on Anti-Inflammatory and Antioxidants Effects. Antioxidants 2022, 11, 350. [Google Scholar] [CrossRef]
- Konig, M.F.; Powell, M.; Staedtke, V.; Bai, R.Y.; Thomas, D.L.; Fischer, N.; Huq, S.; Khalafallah, A.M.; Koenecke, A.; Xiong, R.; et al. Preventing cytokine storm syndrome in COVID-19 using α-1 adrenergic receptor antagonists. J. Clin. Investig. 2020, 130, 3345–3347. [Google Scholar] [CrossRef]
- Tabernero, E.; Ruiz, L.A.; España, P.P.; Méndez, R.; Serrano, L.; Santos, B.; Uranga, A.; González, P.; Garcia, P.; Torres, A.; et al. COVID-19 in young and middle-aged adults: Predictors of poor outcome and clinical differences. Infection 2022, 50, 179–189. [Google Scholar] [CrossRef]
- Skow, R.J.; Garza, N.A.; Nandadeva, D.; Stephens, B.Y.; Wright, A.N.; Grotle, A.K.; Young, B.E.; Fadel, P.J. Impact of COVID-19 on cardiac autonomic function in healthy young adults: Potential role of symptomatology and time since diagnosis. Am. J. Physiol. Heart Circ. Physiol. 2022, 323, H1206–h11. [Google Scholar] [CrossRef] [PubMed]
- Schumann, A.; Bär, K.J. Autonomic aging—A dataset to quantify changes of cardiovascular autonomic function during healthy aging. Sci. Data. 2022, 9, 95. [Google Scholar] [CrossRef]
- Libby, P.; Lüscher, T. COVID-19 is, in the end, an endothelial disease. Eur. Heart J. 2020, 41, 3038–3044. [Google Scholar] [CrossRef]
- Goldberger, J.J.; Arora, R.; Buckley, U.; Shivkumar, K. Autonomic Nervous System Dysfunction: JACC Focus Seminar. J. Am. Coll. Cardiol. 2019, 73, 1189–1206. [Google Scholar] [CrossRef] [PubMed]
- Brunner-La Rocca, H.P.; Esler, M.D.; Jennings, G.L.; Kaye, D.M. Effect of cardiac sympathetic nervous activity on mode of death in congestive heart failure. Eur. Heart J. 2001, 22, 1136–1143. [Google Scholar] [CrossRef] [PubMed]
- Wenner, M.M. Sympathetic activation in chronic anxiety: Not just at the “height” of stress. Editorial Focus on “Relative burst amplitude of muscle sympathetic nerve activity is an indicator of altered sympathetic outflow in chronic anxiety”. J. Neurophysiol. 2018, 120, 7–8. [Google Scholar] [CrossRef]
- Sallis, R.; Young, D.R.; Tartof, S.Y.; Sallis, J.F.; Sall, J.; Li, Q.; Smith, G.N.; Cohen, D.A. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients. Br. J. Sports Med. 2021, 55, 1099–1105. [Google Scholar] [CrossRef]
- Després, J.P. Severe COVID-19 outcomes—The role of physical activity. Nat. Rev. Endocrinol. 2021, 17, 451–452. [Google Scholar] [CrossRef]
- Hautala, A.J.; Kiviniemi, A.M.; Tulppo, M.P. Individual responses to aerobic exercise: The role of the autonomic nervous system. Neurosci. Biobehav. Rev. 2009, 33, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Fu, Q.; Levine, B.D. Exercise and the autonomic nervous system. Handb. Clin. Neurol. 2013, 117, 147–160. [Google Scholar] [PubMed]
- Pedersen, B.K.; Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25 (Suppl. S3), 1–72. [Google Scholar] [CrossRef] [PubMed]
- Fogelholm, M. Physical activity, fitness and fatness: Relations to mortality, morbidity and disease risk factors. A systematic review. Obes. Rev. 2010, 11, 202–221. [Google Scholar] [CrossRef] [PubMed]
- Leidman, E.; Duca, L.M.; Omura, J.D.; Proia, K.; Stephens, J.W.; Sauber-Schatz, E.K. COVID-19 Trends Among Persons Aged 0–24 Years—United States, March 1–12 December 2020; Morbidity and Mortality Weekly Report; Centers for Disease Control and Prevention: New York, NY, USA, 2021; pp. 88–94. [Google Scholar]
- Lira, F.S.; Pereira, T.; Guerra Minuzzi, L.; Figueiredo, C.; Olean-Oliveira, T.; Figueira Freire, A.P.C.; Coelho-e-Silva, M.J.; Caseiro, A.; Thomatieli-Santos, R.V.; Dos Santos, V.R.; et al. Modulatory Effects of Physical Activity Levels on Immune Responses and General Clinical Functions in Adult Patients with Mild to Moderate SARS-CoV-2 Infections—A Protocol for an Observational Prospective Follow-Up Investigation: Fit-COVID-19 Study. Int. J. Environ. Res. Public Health 2021, 18, 13249. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Strobe Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, X.; Jia, X.; Li, J.; Hu, K.; Chen, G.; Wei, J.; Gong, Z.; Zhou, C.; Yu, H.; et al. Risk factors for disease severity, unimprovement, and mortality in COVID-19 patients in Wuhan, China. Clin. Microbiol. Infect. 2020, 26, 767–772. [Google Scholar] [CrossRef]
- World Health Organization. Public Health Surveillance for COVID-19: Interim Guidance. 22 July 2022. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-SurveillanceGuidance-2022.2 (accessed on 22 November 2022).
- Nuttall, F.Q. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Malik, M. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Laborde, S.; Mosley, E.; Thayer, J.F. Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological Research—Recommendations for Experiment Planning, Data Analysis, and Data Reporting. Front. Psychol. 2017, 8, 213. [Google Scholar] [CrossRef]
- Vanderlei, L.C.; Pastre, C.M.; Hoshi, R.A.; Carvalho, T.D.; Godoy, M.F. Basic notions of heart rate variability and its clinical applicability. Rev. Bras. Cir. Cardiovasc. 2009, 24, 205–217. [Google Scholar] [CrossRef] [PubMed]
- Kubios. HRV in Evaluating ANS Function. 2022. Available online: https://www.kubios.com/hrv-ans-function/ (accessed on 22 November 2022).
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health. 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Chen, K.Y.; Freedson, P.S.; Buchowski, M.S.; Beech, B.M.; Pate, R.R.; Troiano, R.P. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008, 167, 875–881. [Google Scholar] [CrossRef]
- Sawilowsky, S.S. New Effect Size Rules of Thumb. J. Mod. Appl. Stat. Methods 2009, 8, 26. [Google Scholar] [CrossRef]
- Khammar, A.; Yarahmadi, M.; Madadizadeh, F. What Is Analysis of Covariance (ANCOVA) and How to Correctly Report Its Results in Medical Research? Iran J. Public Health. 2020, 49, 1016–1017. [Google Scholar] [CrossRef]
- Shouman, K.; Vanichkachorn, G.; Cheshire, W.P.; Suarez, M.D.; Shelly, S.; Lamotte, G.J.; Sandroni, P.; Benarroch, E.E.; Berini, S.E.; Cutsforth-Gregory, J.K.; et al. Autonomic dysfunction following COVID-19 infection: An early experience. Clin. Auton. Res. 2021, 31, 385–394. [Google Scholar] [CrossRef]
- Borovac, J.A.; D’Amario, D.; Bozic, J.; Glavas, D. Sympathetic nervous system activation and heart failure: Current state of evidence and the pathophysiology in the light of novel biomarkers. World J. Cardiol. 2020, 12, 373–408. [Google Scholar] [CrossRef] [PubMed]
- Choi, A.M.; Knobil, K.; Otterbein, S.L.; Eastman, D.A.; Jacoby, D.B. Oxidant stress responses in influenza virus pneumonia: Gene expression and transcription factor activation. Am. J. Physiol. 1996, 271, L383–L391. [Google Scholar] [CrossRef]
- Hassani, M.; Fathi Jouzdani, A.; Motarjem, S.; Ranjbar, A.; Khansari, N. How COVID-19 can cause autonomic dysfunctions and postural orthostatic syndrome? A Review of mechanisms and evidence. Neurol. Clin. Neurosci. 2021, 9, 434–442. [Google Scholar] [CrossRef]
- Boettger, M.K.; Schulz, S.; Berger, S.; Tancer, M.; Yeragani, V.K.; Voss, A.; Bär, K.J. Influence of age on linear and nonlinear measures of autonomic cardiovascular modulation. Ann. Noninvasive Electrocardiol. 2010, 15, 165–174. [Google Scholar] [CrossRef]
- Laitinen, T.; Niskanen, L.; Geelen, G.; Länsimies, E.; Hartikainen, J. Age dependency of cardiovascular autonomic responses to head-up tilt in healthy subjects. J. Appl. Physiol. 2004, 96, 2333–2340. [Google Scholar] [CrossRef] [PubMed]
- Low, P.A.; Tomalia, V.A.; Park, K.J. Autonomic function tests: Some clinical applications. J. Clin. Neurol. 2013, 9, 1–8. [Google Scholar] [CrossRef]
- Vieluf, S.; Hasija, T.; Jakobsmeyer, R.; Schreier, P.J.; Reinsberger, C. Exercise-Induced Changes of Multimodal Interactions Within the Autonomic Nervous Network. Front. Physiol. 2019, 10, 240. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, M.; Langiano, E.; Falese, L.; Diotaiuti, P.; Cortis, C.; De Vito, E. Changes in Physical Activity Levels and Eating Behaviours during the COVID-19 Pandemic: Sociodemographic Analysis in University Students. Int. J. Environ. Res. Public Health 2022, 19, 5550. [Google Scholar] [CrossRef]
- Huber, B.C.; Steffen, J.; Schlichtiger, J.; Graupe, T.; Deuster, E.; Strouvelle, V.P.; Fischer, M.R.; Massberg, S.; Brunner, S. Alteration of physical activity during COVID-19 pandemic lockdown in young adults. J. Transl. Med. 2020, 18, 410. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; Ortiz-Ospin, E.; et al. Brazil: Coronavirus Pandemic Country Profile. Our World in Data 2022. Available online: https://ourworldindata.org/coronavirus/country/brazil (accessed on 22 November 2022).
- Mohamed, A.A.; Alawna, M. The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: A randomized control trial. J. Bodyw. Mov. Ther. 2021, 28, 425–432. [Google Scholar] [CrossRef]
- Gualano, B.; Lemes, I.R.; Silva, R.P.; Pinto, A.J.; Mazzolani, B.C.; Smaira, F.I.; Sieczkowska, S.M.; Aikawa, N.E.; Pasoto, S.G.; Medeiros-Ribeiro, A.C.; et al. Association between physical activity and immunogenicity of an inactivated virus vaccine against SARS-CoV-2 in patients with autoimmune rheumatic diseases. Brain Behav. Immun. 2022, 101, 49–56. [Google Scholar] [CrossRef]
- Montezano, A.C.; Touyz, R.M. Reactive oxygen species and endothelial function--role of nitric oxide synthase uncoupling and Nox family nicotinamide adenine dinucleotide phosphate oxidases. Basic Clin. Pharmacol. Toxicol. 2012, 110, 87–94. [Google Scholar] [CrossRef]
- Yen, C.J.; Hung, C.H.; Tsai, W.M.; Cheng, H.C.; Yang, H.L.; Lu, Y.J.; Tsai, K.L. Effect of Exercise Training on Exercise Tolerance and Level of Oxidative Stress for Head and Neck Cancer Patients Following Chemotherapy. Front. Oncol. 2020, 10, 1536. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Li, X.; He, T.; Ju, F.; Qiu, Y.; Tian, Z. Impact of Physical Activity on COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 14108. [Google Scholar] [CrossRef]
- Ling, Y.; Zhong, J.; Luo, J. Safety and effectiveness of SARS-CoV-2 vaccines: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 6486–6495. [Google Scholar] [CrossRef] [PubMed]
- Hermel, M.; Sweeney, M.; Abud, E.; Luskin, K.; Criado, J.P.; Bonakdar, R.; Gray, J.; Ahern, T. COVID-19 Vaccination Might Induce Postural Orthostatic Tachycardia Syndrome: A Case Report. Vaccines 2022, 10, 991. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.; Reddy, S.; Arora, M. A Case of Postural Orthostatic Tachycardia Syndrome Secondary to the Messenger RNA COVID-19 Vaccine. Cureus 2021, 13, e14837. [Google Scholar] [CrossRef]
- Karimi Galougahi, K. Autonomic dysfunction post-inoculation with ChAdOx1 nCoV-19 vaccine. Eur. Heart J. Case Rep. 2021, 5, ytab472. [Google Scholar] [CrossRef]
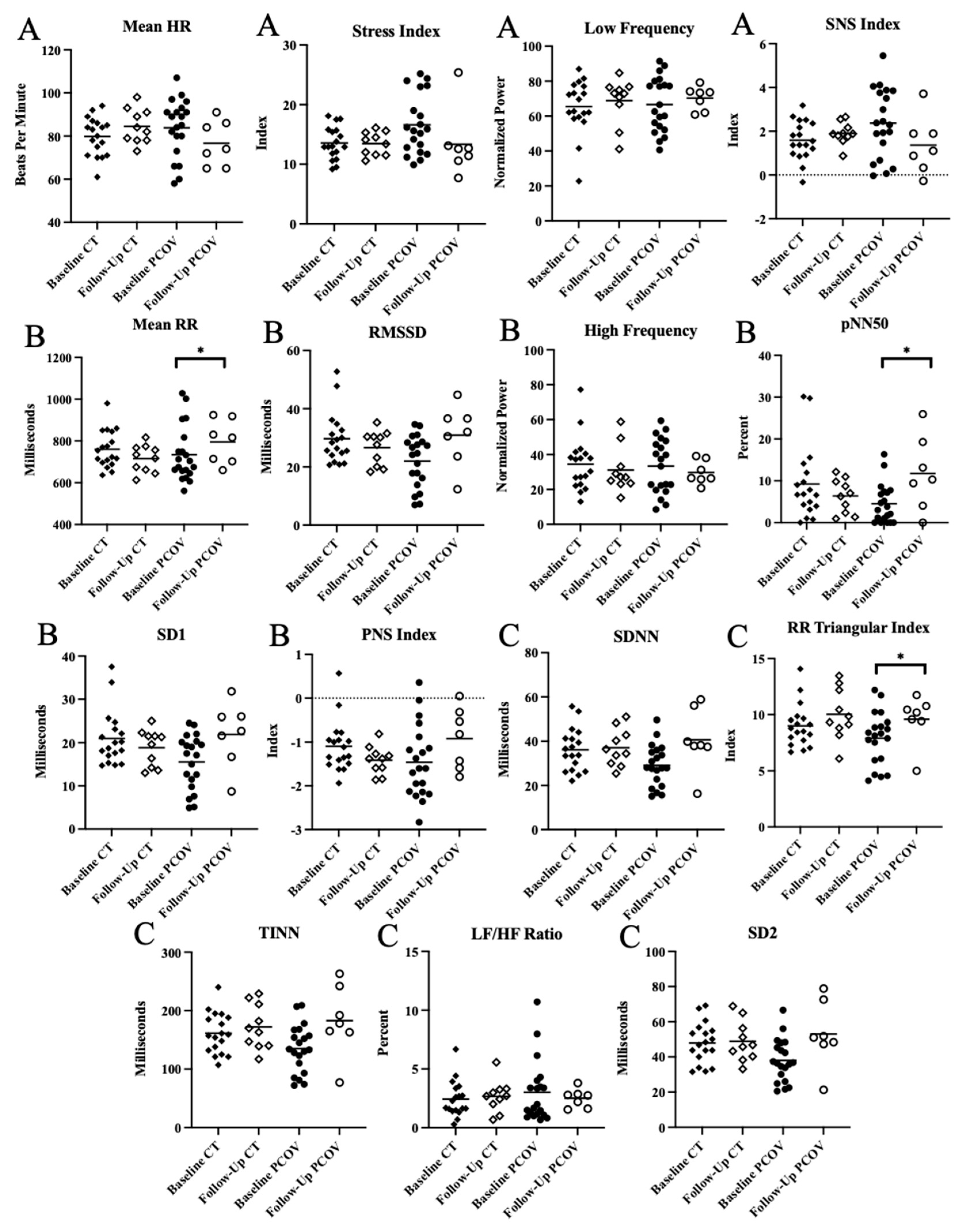
| Sympathetic Nervous System Activity | Unit | |
|---|---|---|
| Mean HR | bpm | Average heart rate |
| Stress Index | ~ | Baevsky’s stress index, a geometric measure of HRV |
| LF | nu | Relative power between 0.04 Hz to 0.15 Hz |
| SNS Index | ~ | Calculated based on the mean HR, Baevsky’s stress index, and SD2 in normalized units |
| Peripheral Nervous System Activity | ||
| Mean RR | ms | Average time of R-R intervals |
| RMSSD | ms | Square root of mean squared difference between adjacent RR intervals |
| HF | nu | Relative power between 0.15 Hz to 0.4 Hz |
| pNN50 | % | Percentage of successive RR intervals that differ by more than 50 ms |
| SD1 | ms | Poincaré plot standard deviation perpendicular the line of identity |
| PNS index | ~ | Calculated based on the mean RR, RMSSD, and SD1 in normalized units |
| Global Variability | ||
| SDNN | ms | Standard deviation of all normal RR intervals |
| RR Triangular Index | ~ | Integral of the density of the RR interval histogram divided by its height |
| TINN | ms | Width of RR interval histogram |
| LF/HF | % | Ratio of low- and high-frequency power |
| SD2 | ms | Poincaré plot standard deviation along the line of identity |
| Control | Post-COVID | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (n = 18) | Follow-Up (n = 10) | Intragroup Analysis | Baseline (n = 20) | Follow-Up (n = 7) | Intragroup Analysis | Intergroup Analysis | ||||||
| Median | Q1-Q3 | Median | Q1–Q3 | Difference between Means | Median | Q1-Q3 | Median | Q1–Q3 | Difference Between Means | 95% CI | p-Value | |
| Sex (M/F) | 13/5 | ~ | 8/2 | ~ | 9/11 | ~ | 4/3 | ~ | ~ | ~ | 0.1119 | |
| Age (years) | 26.66 | 21.11–31.41 | ~ | ~ | ~ | 28.47 | 24.73–33.77 | ~ | ~ | ~ | ~ | ~ |
| Weight (kg) | 71.65 | 57.85–88.85 | 62.70 | 51.20–103.60 | −1.67 ± 8.56 | 77.35 | 65.75–90.68 | 67.40 | 59.70–72.25 | -10.31 ± 6.73 | -2.20 to 6.25 | 0.4116 |
| Height (m) | 1.76 | 1.65–1.79 | 1.69 | 1.63–1.79 | −0.03 ± 0.04 | 1.71 | 1.61–1.77 | 1.70 | 1.64–1.76 | 0.004 ± 0.04 | −0.02 to 0.01 | 0.7348 |
| BMI (kg/m2) | 23.92 | 21.11–28.20 | 23.60 | 20.00–31.98 | −0.01 ± 2.29 | 25.45 | 23.13–31.34 | 23.53 | 19.76–26.41 | −3.58 ± 2.47 | −0.77 to 2.27 | 0.2982 |
| Days between Positive Test and Follow-Up | ~ | ~ | ~ | ~ | ~ | 37.50 | 24.75–70.50 | ~ | ~ | ~ | ~ | ~ |
| Physical Activity | ||||||||||||
| n = 16 | n = 8 | n = 16 | n = 4 | |||||||||
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | |||||
| Sedentary Activity (min/day) | 578.43 | 534.88–676.68 | 590.52 | 467.67–664.25 | −92.97 ± 98.48 | 499.59 | 467.05–593.48 | 601.15 | 493.50–646.97 | −33.88 ± 146.52 | −212.98 to 373.82 | 0.5550 |
| Light Activity (min/day) | 251.50 | 188.54–291.00 | 254.14 | 220.00–407.34 | 52.77 ± 33.62 | 285.15 | 206.75–432.30 | 258.48 | 235.24–306.71 | −42.21 ± 60.08 | −131.75 to 182.60 | 0.7260 |
| Moderate Activity (min/day) | 17.90 | 5.14–29.87 | 11.00 | 6.04–15.57 | −10.65 ± 8.58 | 13.36 | 9.25–33.72 | 27.86 | 23.78–32.25 | 4.73 ± 11.36 | −28.06 to 25.00 | 0.9004 |
| Vigorous Activity (min/day) | 3.65 | 0.00–15.82 | 0.00 | 0.00–2.36 | −7.73 ± 4.33 | 0.00 | 0.00–0.50 | 0.13 | 0.00–4.67 | 0.92 ± 1.00 | −10.63 to 3.26 | 0.2061 |
| MVPA (min/day) | 23.72 | 12.60–46.00 | 11.00 | 6.36–17.13 | −19.13 ± 11.86 | 14.79 | 9.57–34.04 | 31.06 | 24.92–32.72 | 5.51 ± 11.69 | −32.43 to 19.06 | 0.5756 |
| Steps Count (steps/day) | 6570.65 | 4994.12–7795.24 | 4822.72 | 3714.61–8585.47 | −1296.60 ± 1706.15 | 5231.86 | 3696.86–9601.29 | 6350.22 | 5996.22–7197.71 | 187.06 ± 1585.93 | −5935.78 to 4693.48 | 0.7998 |
| Total Time in BSB 30–60 min Bouts | 169.44 | 97.32–222.25 | 161.07 | 63.24–239.47 | −18.99 ± 39.95 | 91.36 | 73.36–134.18 | 137.36 | 98.78–187.97 | 30.67 ± 35.92 | −124.54 to 137.29 | 0.9157 |
| Total Time in BSB ≥ 60 min Bouts | 34.31 | 19.17–99.61 | 46.79 | 4.04–69.32 | −17.29 ± 22.46 | 17.63 | 8.86–29.32 | 30.07 | 2.25–57.36 | −4.35 ± 25.22 | −66.38 to 77.40 | 0.8678 |
| Control (n = 11) | Post-COVID (n = 7) | |||||
|---|---|---|---|---|---|---|
| Intragroup Analysis | Intragroup Analysis | Intergroup Analysis | ||||
| Dif Between Means | Dif Between Means | Unadjusted 95% CI | Unadjusted p-Value | Adjusted 95% CI | Adjusted p-Value | |
| SNS Activity | ||||||
| Mean HR | 4.67 ± 3.37 | −7.13 ± 5.59 | −25.83 to −4.33 | 0.0024 ** | −24.67 to −3.26 | 0.014 + |
| Stress Index | −0.10 ± 0.98 | −3.26 ± 2.26 | −0.60 to 6.51 | 0.0965 | −6.62 to 0.57 | 0.093 |
| LF (nu) | 3.35 ± 5.76 | 3.66 ± 6.17 | −31.16 to 2.17 | 0.0836 | −2.26 to 30.39 | 0.086 |
| SNS Index | 0.31 ± 0.31 | −1.01 ± 0.66 | −2.48 to −0.29 | 0.0068 ** | −2.50 to −0.32 | 0.015 + |
| PNS Activity | ||||||
| Mean RR | −44.54 ± 32.38 | 60.36 ± 55.35 * | 33.50 to 222.50 | 0.0097 ** | 33.72 to 225.51 | 0.012 + |
| RMSSD | −3.05 ± 3.15 | 8.95 ± 4.08 | −17.06 to 0.80 | 0.1088 | −0.79 to 17.35 | 0.071 |
| HF (nu) | −3.35 ± 5.76 | −3.62 ± 6.17 | −2.33 to 31.11 | 0.0864 | −30.33 to 2.40 | 0.089 |
| pNN50 | −2.84 ± 2.93 | 7.21 ± 2.61 * | −14.62 to 0.19 | 0.0553 | −0.21 to 14.88 | 0.056 |
| SD1 | −2.15 ± 2.24 | 6.35 ± 2.89 | −12.12 to 0.56 | 0.1038 | −0.55 to 12.32 | 0.07 |
| PNS index | −0.32 ± 0.20 | 0.54 ± 0.35 | 0.20 to 1.45 | 0.0091 ** | −0.20 to 1.47 | 0.013 + |
| Global Variability | ||||||
| SDNN | 0.91 ± 3.63 | 11.54 ± 4.69 | −20.92 to 0.96 | 0.0709 | −1.31 to 21.40 | 0.078 |
| RR Triangular Index | 1.02 ± 0.80 | 1.68 ± 1.01 * | −2.97 to 1.53 | 0.506 | −1.61 to 3.06 | 0.517 |
| TINN | 10.67 ± 14.25 | 47.86 ± 20.32 | −79.60 to 12.72 | 0.1434 | −14.20 to 81.68 | 0.153 |
| LF/HF | 0.23 ± 0.58 | −0.50 ± 1.03 | −3.00 to 0.75 | 0.2199 | −0.70 to 2.84 | 0.218 |
| SD2 | 0.97 ± 4.55 | 15.03 ± 6.17 | −27.16 to 1.65 | 0.0786 | −2.16 to 27.80 | 0.088 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freire, A.P.C.F.; Amin, S.; Lira, F.S.; Morano, A.E.v.A.; Pereira, T.; Coelho-E-Silva, M.-J.; Caseiro, A.; Christofaro, D.G.D.; Dos Santos, V.R.; Júnior, O.M.; et al. Autonomic Function Recovery and Physical Activity Levels in Post-COVID-19 Young Adults after Immunization: An Observational Follow-Up Case-Control Study. Int. J. Environ. Res. Public Health 2023, 20, 2251. https://doi.org/10.3390/ijerph20032251
Freire APCF, Amin S, Lira FS, Morano AEvA, Pereira T, Coelho-E-Silva M-J, Caseiro A, Christofaro DGD, Dos Santos VR, Júnior OM, et al. Autonomic Function Recovery and Physical Activity Levels in Post-COVID-19 Young Adults after Immunization: An Observational Follow-Up Case-Control Study. International Journal of Environmental Research and Public Health. 2023; 20(3):2251. https://doi.org/10.3390/ijerph20032251
Chicago/Turabian StyleFreire, Ana Paula Coelho Figueira, Shaan Amin, Fabio Santos Lira, Ana Elisa von Ah Morano, Telmo Pereira, Manuel-João Coelho-E-Silva, Armando Caseiro, Diego Giulliano Destro Christofaro, Vanessa Ribeiro Dos Santos, Osmar Marchioto Júnior, and et al. 2023. "Autonomic Function Recovery and Physical Activity Levels in Post-COVID-19 Young Adults after Immunization: An Observational Follow-Up Case-Control Study" International Journal of Environmental Research and Public Health 20, no. 3: 2251. https://doi.org/10.3390/ijerph20032251
APA StyleFreire, A. P. C. F., Amin, S., Lira, F. S., Morano, A. E. v. A., Pereira, T., Coelho-E-Silva, M.-J., Caseiro, A., Christofaro, D. G. D., Dos Santos, V. R., Júnior, O. M., Pinho, R. A., & Silva, B. S. d. A. (2023). Autonomic Function Recovery and Physical Activity Levels in Post-COVID-19 Young Adults after Immunization: An Observational Follow-Up Case-Control Study. International Journal of Environmental Research and Public Health, 20(3), 2251. https://doi.org/10.3390/ijerph20032251











