Spiritual Needs, Religious Coping and Mental Wellbeing: A Cross-Sectional Study among Migrants and Refugees in Germany
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
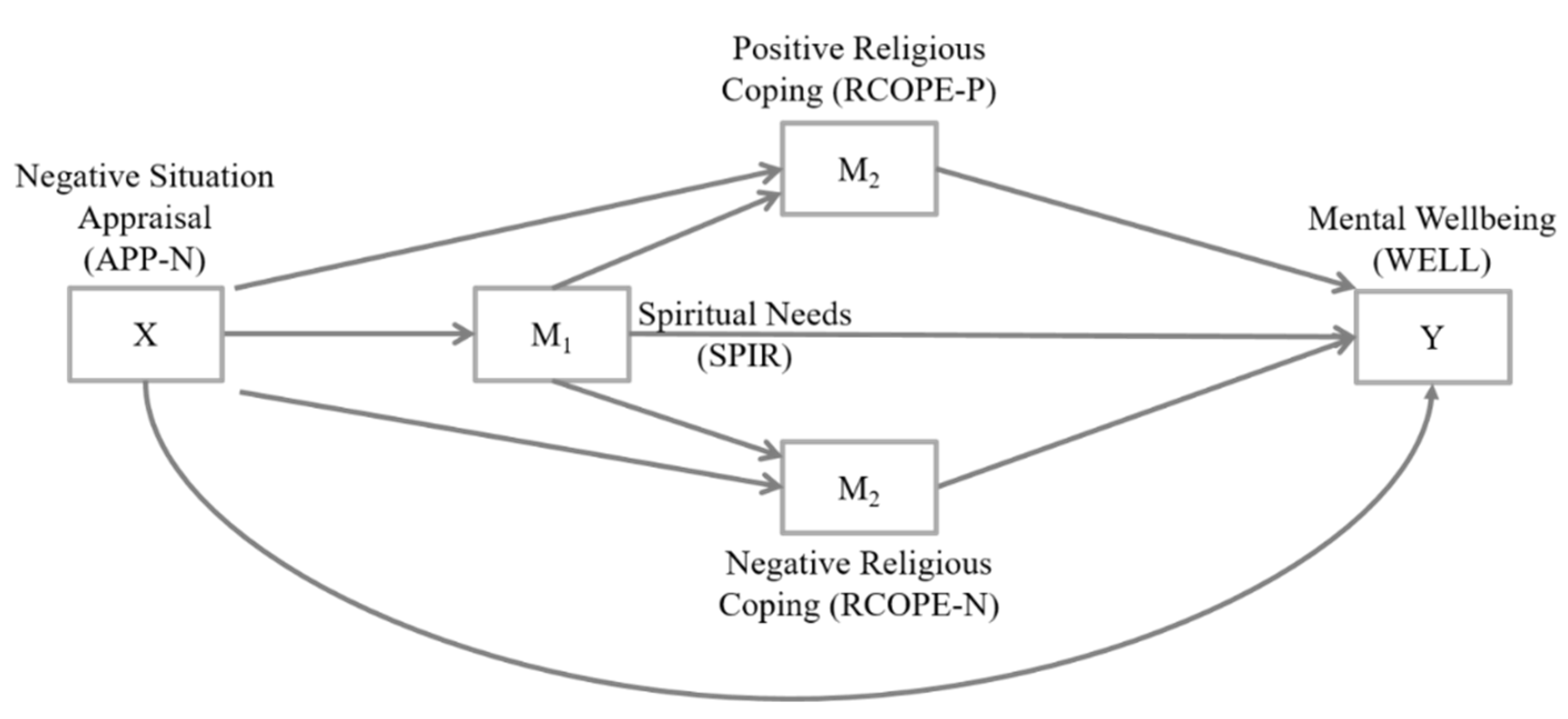
2.3. Data Analysis
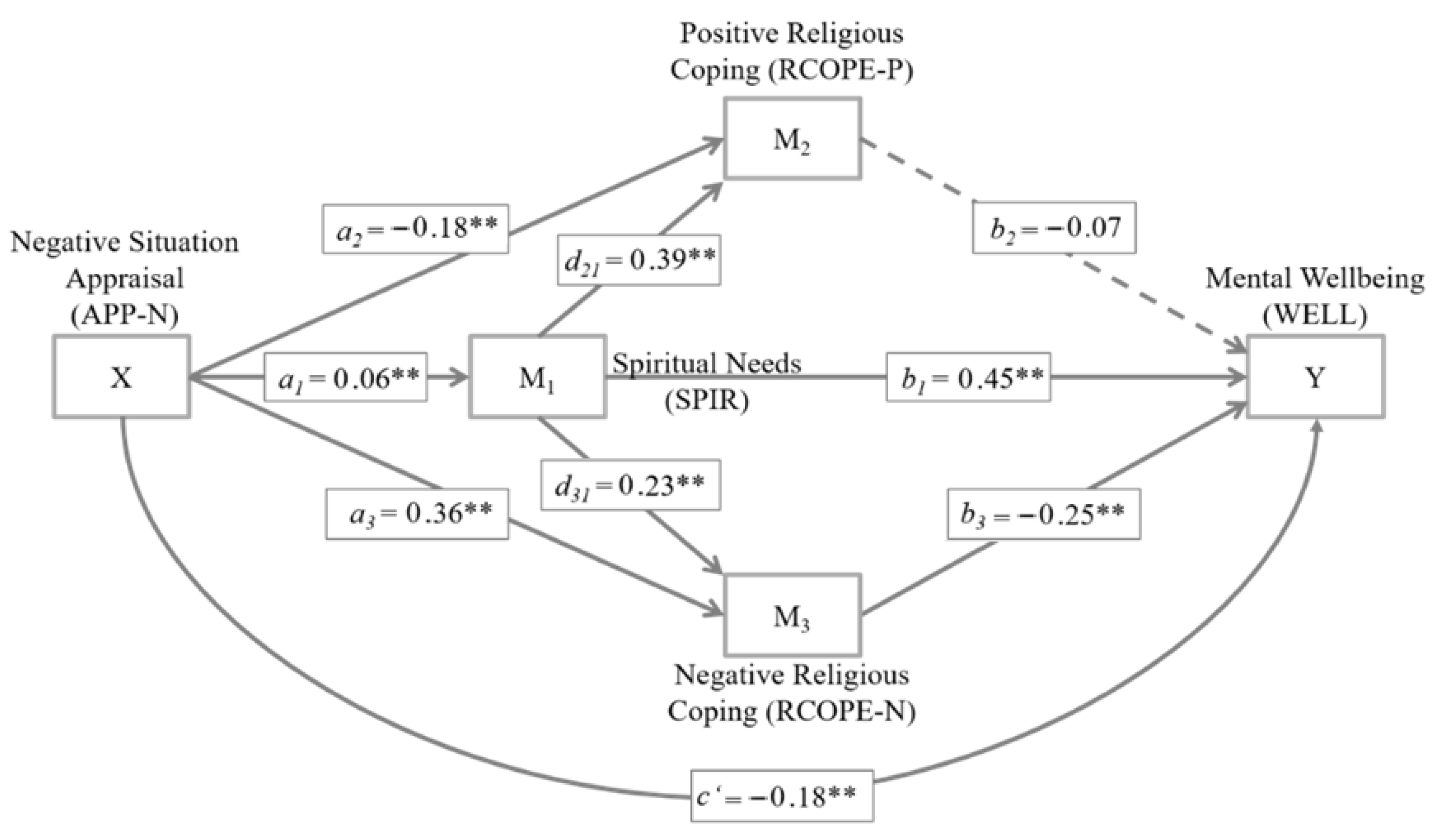
3. Results
4. Discussion
5. Practical Implications and Recommendations
6. Limitations and Future Studies
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- UNHCR—Refugee Statistics. Available online: https://www.unhcr.org/refugee-statistics/ (accessed on 15 January 2022).
- UNHCR—Germany. Available online: https://www.unhcr.org/germany.html (accessed on 15 January 2022).
- Hameed, S.; Sadiq, A.; Din, A.U. The increased vulnerability of refugee population to mental health disorders. Kansas J. Med. 2018, 11, 20–23. [Google Scholar] [CrossRef] [Green Version]
- Silove, D.; Ventevogel, P.; Rees, S. The contemporary refugee crisis: An overview of mental health challenges. World Psychiatry 2017, 16, 130–139. [Google Scholar] [CrossRef] [Green Version]
- Areba, E.M.; Duckett, L.; Robertson, C.; Savik, K. Religious coping, symptoms of depression and anxiety, and well-being among somali college students. J. Relig. Health 2018, 57, 94–109. [Google Scholar] [CrossRef] [Green Version]
- de Kleine, R.A.; Woud, M.L.; Ferentzi, H.; Hendriks, G.J.; Broekman, T.G.; Becker, E.S.; Van Minnen, A. Appraisal-based cognitive bias modification in patients with posttraumatic stress disorder: A randomised clinical trial. Eur. J. Psychotraumatol. 2019, 10, 1625690. [Google Scholar] [CrossRef] [Green Version]
- Fino, E.; Mema, D.; Russo, P.M. War trauma exposed refugees and posttraumatic stress disorder: The moderating role of trait resilience. J. Psychosom. Res. 2020, 129, 109905. [Google Scholar] [CrossRef]
- Borho, A.; Viazminsky, A.; Morawa, E.; Schmitt, G.M.; Georgiadou, E.; Erim, Y. The prevalence and risk factors for mental distress among Syrian refugees in Germany: A Register-based follow-up study. BMC Psychiatry 2020, 20, 1–13. [Google Scholar] [CrossRef]
- Nesterko, Y.; Jäckle, D.; Friedrich, M.; Holzapfel, L.; Glaesmer, H. Health care needs among recently arrived refugees in Germany: A cross-sectional, epidemiological study. Int. J. Public Health 2020, 65, 811–821. [Google Scholar] [CrossRef]
- Byrow, Y.; Pajak, R.; Specker, P.; Nickerson, A. Perceptions of mental health and perceived barriers to mental health help-seeking amongst refugees: A systematic review. Clin. Psychol. Rev. 2020, 75, 101812. [Google Scholar] [CrossRef]
- Markova, V.; Sandal, G.M.; Guribye, E. What do immigrants from various cultures think is the best way to cope with depression? Introducing the cross-cultural coping inventory. Front. Psychol. 2020, 11, 1599. [Google Scholar] [CrossRef]
- Renner, A.; Hoffmann, R.; Nagl, M.; Roehr, S.; Jung, F.; Grochtdreis, T.; König, H.H.; Riedel-Heller, S.; Kersting, A. Syrian refugees in Germany: Perspectives on mental health and coping strategies. J. Psychosom. Res. 2020, 129, 109906. [Google Scholar] [CrossRef]
- Zbidat, A.; Georgiadou, E.; Borho, A.; Erim, Y.; Morawa, E. The perceptions of trauma, complaints, somatization, and coping strategies among Syrian refugees in Germany-a qualitative study of an at-risk population. Int. J. Environ. Res. Public Health 2020, 17, 693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keyes, E.F. Mental health status in refugees: An integrative review of current research. Issues Ment. Health Nurs. 2009, 21, 397–410. [Google Scholar] [CrossRef] [PubMed]
- Slewa-Younan, S.; Uribe Guajardo, M.G.; Heriseanu, A.; Hasan, T. A systematic review of post-traumatic stress disorder and depression amongst Iraqi refugees located in western countries. J. Immigr. Minor. Health 2014, 17, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Fazel, M.; Wheeler, J.; Danesh, J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: A systematic review. Lancet 2005, 365, 1309–1314. [Google Scholar] [CrossRef]
- Bryant-Davis, T.; Wong, E.C. Faith to move mountains: Religious coping, spirituality, and interpersonal trauma recovery. Am. Psychol. 2013, 68, 675–684. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H.G.; King, D.E.; Carson, V.B. Handbook of Religion and Health, 2nd ed.; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Ager, A.; Ager, J. Faith, Secularism, and Humanitarian Engagement; Palgrave Macmillan: London, UK, 2015. [Google Scholar] [CrossRef]
- AbdAleati, N.S.; Mohd Zaharim, N.; Mydin, Y.O. Religiousness and mental health: Systematic review study. J. Relig. Health 2016, 55, 1929–1937. [Google Scholar] [CrossRef]
- Pandya, S.P. Spirituality for mental health and well-being of adult refugees in Europe. J. Immigr. Minor. Health 2018, 20, 1396–1403. [Google Scholar] [CrossRef]
- McLellan, J. Religious responses to bereavement, grief, and loss among refugees. J. Loss Trauma 2014, 20, 131–138. [Google Scholar] [CrossRef]
- Buber-Ennser, I.; Goujon, A.; Kohlenberger, J.; Rengs, B. Multi-layered roles of religion among refugees arriving in Austria around 2015. Religions 2018, 9, 154. [Google Scholar] [CrossRef] [Green Version]
- Rayes, D.; Karnouk, C.; Churbaji, D.; Walther, L.; Bajbouj, M. Faith-based coping among arabic-speaking refugees seeking mental health services in berlin, Germany: An exploratory qualitative study. Front. Psychiatry 2021, 12, 14. [Google Scholar] [CrossRef]
- Ano, G.G.; Vasconcelles, E.B. Religious coping and psychological adjustment to stress: A meta-analysis. J. Clin. Psychol. 2005, 61, 461–480. [Google Scholar] [CrossRef] [PubMed]
- Helgeson, V.S.; Reynolds, K.A.; Tomich, P.L. A meta-analytic review of benefit finding and growth. J. Consult. Clin. Psychol. 2006, 74, 797–816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prati, G.; Pietrantoni, L. Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: A meta-analysis. J. Loss Trauma 2009, 14, 364–388. [Google Scholar] [CrossRef] [Green Version]
- Gladden, J. The coping skills of east African refugees: A literature review. Refug. Surv. Q. 2012, 31, 177–196. [Google Scholar] [CrossRef]
- Kuo, B.C.H. Coping, acculturation, and psychological adaptation among migrants: A theoretical and empirical review and synthesis of the literature. Health Psychol. Behav. Med. Open Access J. 2014, 2, 16–33. [Google Scholar] [CrossRef]
- Hodge, D.R. Spiritual assessment with refugees and other migrant populations: A necessary foundation for successful clinical practice. J. Relig. Spiritual. Soc. Work. Soc. Thought 2019, 38, 121–139. [Google Scholar] [CrossRef]
- Kartal, S.; Değirmenci, H.; Arslan, F. Ranking irrigation schemes based on principle component analysis in the arid regions of turkey. Agron. Res. 2019, 17, 456–465. [Google Scholar] [CrossRef]
- Acquaye, H.E.; Sivo, S.A.; Jones, K.D. Religious commitment’s moderating effect on refugee trauma and growth. Couns. Values 2018, 63, 57–75. [Google Scholar] [CrossRef] [Green Version]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: Berlin/Heidelberg, Germany, 1984. [Google Scholar]
- Emmons, R.A. Spirituality and intelligence: Problems and prospects. Int. J. Psychol. Relig. 2009, 21, 57–64. [Google Scholar] [CrossRef]
- Mickley, J.R.; Pargament, K.I.; Brant, C.R.; Hipp, K.M. God and the search for meaning among hospice caregivers. Hosp. J. 2017, 13, 1–17. [Google Scholar] [CrossRef]
- Sarizadeh, M.S.; Najafi, M.; Rezaei, A.M. The prediction of depression based on religious coping and the components of positive youth development in adolescents. Ment. Health Relig. Cult. 2020, 23, 216–228. [Google Scholar] [CrossRef]
- O’Brien, B.; Shrestha, S.; Stanley, M.A.; Pargament, K.I.; Cummings, J.; Kunik, M.E.; Fletcher, T.L.; Cortes, J.; Ramsey, D.; Amspoker, A.B. Positive and negative religious coping as predictors of distress among minority older adults. Int. J. Geriatr. Psychiatry 2019, 34, 54–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aflakseir, A.; Mahdiyar, M. The role of religious coping strategies in predicting depression among a sample of women with fertility problems in shiraz. J. Reprod. Infertil. 2016, 17, 117. [Google Scholar] [PubMed]
- Olson, M.M.; Trevino, D.B.; Geske, J.A.; Vanderpool, H. Religious coping and mental health outcomes: An exploratory study of socioeconomically disadvantaged patients. Explore 2012, 8, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Pargament, K.I.; Smith, B.W.; Koenig, H.G.; Perez, L. Patterns of positive and negative religious coping with major life stressors. J. Sci. Study Relig. 1998, 37, 710. [Google Scholar] [CrossRef]
- Büssing, A. Spiritual Needs in Research and Practice; Springer International Publishing: Berlin/Heidelberg, Germany, 2021. [Google Scholar] [CrossRef]
- Sischka, P.E.; Costa, A.P.; Steffgen, G.; Schmidt, A.F. The WHO-5 well-being index—Validation based on item response theory and the analysis of measurement invariance across 35 countries. J. Affect. Disord. Rep. 2020, 1, 100020. [Google Scholar] [CrossRef]
- Bech, P.; Gudex, C.; Staehr Johansen, K. The WHO (Ten) well-being index: Validation in diabetes. Psychother. Psychosom. 1996, 65, 183–190. [Google Scholar] [CrossRef]
- Zung, W.W.K.; Magill, M.; Moore, J.T.; George, D.T. Recognition and treatment of depression in a family medicine practice. J. Clin. Psychiatry 1983, 44, 3–6. [Google Scholar]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 well-being index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Büssing, A.; Balzat, H.J.; Heusser, P. Spiritual needs of patients with chronic pain diseases and cancer—Validation of the spiritual needs questionnaire. Eur. J. Med. Res. 2010, 15, 266–273. [Google Scholar] [CrossRef] [Green Version]
- Büssing, A.; Recchia, D.R.; Koenig, H.; Baumann, K.; Frick, E. Factor structure of the spiritual needs questionnaire (SpNQ) in persons with chronic diseases, elderly and healthy individuals. Religions 2018, 9, 13. [Google Scholar] [CrossRef] [Green Version]
- Büssing, A.; Koenig, H.G. Spiritual needs of patients with chronic diseases. Religions 2010, 1, 18–27. [Google Scholar] [CrossRef]
- Pargament, K.I.; Koenig, H.G.; Perez, L.M. The many methods of religious coping: Development and initial validation of the RCOPE. J. Clin. Psychol. 2000, 56, 519–543. [Google Scholar] [CrossRef]
- Pargament, K.; Feuille, M.; Burdzy, D. The brief RCOPE: Current psychometric status of a short measure of religious coping. Religions 2011, 2, 51–76. [Google Scholar] [CrossRef] [Green Version]
- Büssing, A.; Fischer, J. Interpretation of illness in cancer survivors is associated with health-related variables and adaptive coping styles. BMC Women’s. Health 2009, 9, 2. [Google Scholar] [CrossRef] [Green Version]
- Lachowicz, M.J.; Preacher, K.J.; Kelley, K. A novel measure of effect size for mediation analysis. Psychol. Methods 2017, 23, 244. [Google Scholar] [CrossRef] [Green Version]
- Li, J.B.; Yang, A.; Dou, K.; Cheung, R.Y. Self-control moderates the association between perceived severity of coronavirus disease 2019 (COVID-19) and mental health problems among the Chinese public. Int. J. Environ. Res. Public Health 2020, 17, 4820. [Google Scholar] [CrossRef]
- Kira, I.A.; Omidy, A.Z.; Ashby, J.S. Cumulative trauma, appraisal, and coping in Palestinian and American Indian adults: Two cross-cultural studies. Traumatol. Int. J. 2014, 20, 119–133. [Google Scholar] [CrossRef]
- Rand, K.L.; Cripe, L.D.; Monahan, P.O.; Tong, Y.; Schmidt, K.; Rawl, S.M. Illness appraisal, religious coping, and psychological responses in men with advanced cancer. Supportive Care Cancer 2011, 20, 1719–1728. [Google Scholar] [CrossRef]
- Adam, Z.; Ward, C. Stress, religious coping and wellbeing in acculturating Muslims. J. Muslim Ment. Health 2016, 10, 3–26. [Google Scholar] [CrossRef] [Green Version]
- Booij, S.H.; Snippe, E.; Jeronimus, B.F.; Wichers, M.; Wigman, J.T.W. Affective reactivity to daily life stress: Relationship to positive psychotic and depressive symptoms in a general population sample. J. Affect. Disord. 2018, 225, 474–481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCleary-Gaddy, A.T.; Miller, C.T. Negative religious coping as a mediator between perceived prejudice and psychological distress among African Americans: A structural equation modeling approach. Psycholog. Relig. Spiritual. 2018, 11, 257. [Google Scholar] [CrossRef]
- Ahles, J.J.; Mezulis, A.H.; Hudson, M.R. Religious coping as a moderator of the relationship between stress and depressive symptoms. Psycholog. Relig. Spiritual. 2016, 8, 228–234. [Google Scholar] [CrossRef]
- Lee, M.; Nezu, A.M.; Nezu, C.M. Positive and negative religious coping, depressive symptoms, and quality of life in people with HIV. J. Behav. Med. 2014, 37, 921–930. [Google Scholar] [CrossRef] [PubMed]
- Francis, B.; Gill, J.S.; Yit Han, N.; Petrus, C.F.; Azhar, F.L.; Ahmad Sabki, Z.; Said, M.A.; Ong Hui, K.; Chong Guan, N.; Sulaiman, A.H. Religious coping, religiosity, depression and anxiety among medical students in a multi-religious setting. Int. J. Environ. Res. Public Health 2019, 16, 259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, C.L.; Holt, C.L.; Le, D.; Christie, J.; Williams, B.R. Positive and negative religious coping styles as prospective predictors of well-being in African Americans. Psycholog. Relig. Spiritual. 2018, 10, 318–326. [Google Scholar] [CrossRef]
- Hebert, R.; Zdaniuk, B.; Schulz, R.; Scheier, M. Positive and negative religious coping and well-being in women with breast cancer. J. Palliat. Med. 2009, 12, 537–545. [Google Scholar] [CrossRef]
- Lee, J.-Y.; Choi, J.-S.; Kwon, J.S. Neurophysiological mechanisms of resilience as a protective factor in patients with internet gaming disorder: A resting-state EEG coherence study. J. Clin. Med. 2019, 8, 49. [Google Scholar] [CrossRef] [Green Version]
- Hickman, E.E.; Glass, C.R.; Arnkoff, D.B.; Fallot, R.D. Religious coping, stigma, and psychological functioning among HIV-positive African American women. Ment. Health Relig. Cult. 2013, 16, 832–851. [Google Scholar] [CrossRef]
- Pargament, K.I.; Koenig, H.G.; Tarakeshwar, N.; Hahn, J. Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically Ill elderly patients: A two-year longitudinal study. J. Health Psychol. 2004, 9, 713–730. [Google Scholar] [CrossRef]
- Ai, A.L.; Park, C.L.; Huang, B.; Rodgers, W.; Tice, T.N. Psychosocial mediation of religious coping styles: A study of short-term psychological distress following cardiac surgery. Personal. Soc. Psychol. Bull. 2007, 33, 867–882. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, T.P.; Laney, T.; Mezulis, A. Religious coping, stress, and depressive symptoms among adolescents: A prospective study. Psychol. Relig. Spiritual. 2012, 4, 19–30. [Google Scholar] [CrossRef] [Green Version]
- Pargament, K.I.; Brant, C.R. Religion and coping. In Handbook of Religion and Mental Health; Academic Press: Cambridge, MA, USA, 1998; pp. 111–128. [Google Scholar] [CrossRef]
- Forouzi, M.A.; Tirgari, B.; Safarizadeh, M.H.; Jahani, Y. Spiritual needs and quality of life of patients with cancer. Indian J. Palliat. Care 2017, 23, 437. [Google Scholar] [CrossRef] [PubMed]
- Wi, E.S.; Yong, J. Distress, depression, anxiety, and spiritual needs of patients with stomach cancer. Asian Oncol. Nurs. 2012, 12, 314–322. [Google Scholar] [CrossRef]
- Bekelman, D.B.; Dy, S.M.; Becker, D.M.; Wittstein, I.S.; Hendricks, D.E.; Yamashita, T.E.; Gottlieb, S.H. Spiritual well-being and depression in patients with heart failure. J. Gen. Intern. Med. 2007, 22, 470–477. [Google Scholar] [CrossRef]
- Bužgová, R.; Hajnová, E.; Sikorová, L.; Jarošová, D. Association between unmet needs and quality of life in hospitalised cancer patients no longer receiving anti-cancer treatment. Eur. J. Cancer Care 2014, 23, 685–694. [Google Scholar] [CrossRef]
- Steger, M.F.; Kashdan, T.B.; Sullivan, B.A.; Lorentz, D. Understanding the search for meaning in life: Personality, cognitive style, and the dynamic between seeking and experiencing meaning. J. Pers. 2008, 76, 199–228. [Google Scholar] [CrossRef]
- Davis, C.G.; Morgan, M.S. Finding meaning, perceiving growth, and acceptance of tinnitus. Rehabil. Psychol. 2008, 53, 128–138. [Google Scholar] [CrossRef]
- Stewart, W.C.; Adams, M.P.; Stewart, J.A.; Nelson, L.A. Review of clinical medicine and religious practice. J. Relig. Health 2012, 52, 91–106. [Google Scholar] [CrossRef]
- Fatima, S.; Sharif, S.; Khalid, I. How does religiosity enhance psychological well-being? Roles of self-efficacy and perceived social support. Psycholog. Relig. Spiritual. 2018, 10, 119–127. [Google Scholar] [CrossRef]
- Mozaffar, G.; Akbar, R. Religious commitment and self-efficacy in predicting the amount and type of perceived stress in university students. J. Res. Behav. Sci. 2011, 9, 269–278. [Google Scholar]
- Maier, K.; Surzykiewicz, J. Mediated association between spirituality and life satisfaction in chronically Ill undergraduate students. Psycholog. Relig. Spiritual. 2020, 12, 311–323. [Google Scholar] [CrossRef]
- Kuo, B.C.H.; Arnold, R.; Rodriguez-Rubio, B. Mediating effects of coping in the link between spirituality and psychological distress in a culturally diverse undergraduate sample. Ment. Health Relig. Cult. 2013, 17, 173–184. [Google Scholar] [CrossRef] [Green Version]
- Pérez, J.E.; Rex Smith, A. Intrinsic religiousness and well-being among cancer patients: The mediating role of control-related religious coping and self-efficacy for coping with cancer. J. Behav. Med. 2014, 38, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Abu-Raiya, H.; Pargament, K.I. Religious coping among diverse religions: Commonalities and divergences. Psycholog. Relig. Spiritual. 2015, 7, 24–33. [Google Scholar] [CrossRef]
- Karekla, M.; Constantinou, M. Religious coping and cancer: Proposing an acceptance and commitment therapy approach. Cogn. Behav. Pract. 2010, 17, 371–381. [Google Scholar] [CrossRef]
- Sherman, A.C.; Simonton, S.; Latif, U.; Spohn, R.; Tricot, G. Religious struggle and religious comfort in response to illness: Health outcomes among stem cell transplant patients. J. Behav. Med. 2005, 28, 359–367. [Google Scholar] [CrossRef]
- Sabanciogullari, S.; Yilmaz, F.T. The effect of religious coping on hope level of cancer patients receiving chemotherapy. J. Relig. Health 2019, 60, 2756–2769. [Google Scholar] [CrossRef]
- Shamsalinia, A.; Pourghaznein, T.; Parsa, M. The relationship between hope and religious coping among patients with type 2 diabetes. Glob. J. Health Sci. 2016, 8, 208. [Google Scholar] [CrossRef]
- Lauricella, S.K.; Phillips, R.E.; Dubow, E.F. Religious coping with sexual stigma in young adults with same-sex attractions. J. Relig. Health 2017, 56, 1436–1449. [Google Scholar] [CrossRef]
- Trevino, K.M.; Pargament, K.I.; Cotton, S.; Leonard, A.C.; Hahn, J.; Caprini-Faigin, C.A.; Tsevat, J. Religious coping and physiological, psychological, social, and spiritual outcomes in patients with HIV/aids: Cross-sectional and longitudinal findings. AIDS Behav. 2007, 14, 379–389. [Google Scholar] [CrossRef]
- Ghorbani, N.; Watson, P.J.; Tahbaz, S.; Chen, Z.J. Religious and psychological implications of positive and negative religious coping in Iran. J. Relig. Health 2016, 56, 477–492. [Google Scholar] [CrossRef] [PubMed]
- Abu-Raiya, H.; Jamal, H. The links between religious coping and subjective well-being among Israeli-Muslims who lost a beloved person through death. Death Stud. 2019, 45, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Pargament, K.I.; Mahoney, A.; Exline, J.J.; Jones, J.W.; Shafranske, E.P. Envisioning an Integrative paradigm for the psychology of religion and spirituality. In APA Handbook of Psychology, Religion, and Spirituality: Context, Theory, and Research; Pargament, K.I., Exline, J.J., Jones, J.W., Eds.; American Psychological Association: Worcester, MA, USA, 2013; Volume 1, pp. 3–19. [Google Scholar] [CrossRef]
- Eltaiba, N. Counseling with muslim refugees: Building rapport. J. Soc. Work Pract. 2014, 28, 397–403. [Google Scholar] [CrossRef]
- Muruthi, B.A.; Young, S.S.; Chou, J.; Janes, E.; Ibrahim, M. “We pray as a family”: The role of religion for resettled Karen refugees. J. Fam. Issues 2020, 41, 1723–1741. [Google Scholar] [CrossRef]
| Variable | n | % |
|---|---|---|
| Educational status | ||
| Illiterate | 68 | 9.1 |
| Primary | 125 | 16.8 |
| Intermediate | 168 | 22.6 |
| Secondary | 92 | 12.4 |
| Post-secondary | 112 | 15.1 |
| Tertiary (university etc.) | 47 | 6.3 |
| No information | 132 | 17.7 |
| Family status | ||
| Married | 210 | 28.3 |
| Single | 448 | 60.2 |
| Widowed | 24 | 3.2 |
| No information | 62 | 8.3 |
| I came to Germany with … | ||
| Alone | 383 | 51.5 |
| My partner | 67 | 9.0 |
| My child/children | 34 | 4.6 |
| My partner and my child/children | 108 | 14.5 |
| No information | 152 | 20.4 |
| WELL | Spiritual Needs | Religious Coping | APP-N | ||||||
|---|---|---|---|---|---|---|---|---|---|
| SPIR | SPIR-EXIST | SPIR-GEN | SPIR-PEACE | SPIR-REL | RCOPE-P | RCOPE-N | |||
| M | 3.59 | 2.62 | 2.41 | 2.78 | 2.72 | 2.57 | 2.84 | 1.71 | 1.98 |
| SD | 1.09 | 0.58 | 0.78 | 0.65 | 0.67 | 0.79 | 0.77 | 0.79 | 0.97 |
| SE | 0.04 | 0.02 | 0.03 | 0.02 | 0.02 | 0.03 | 0.03 | 0.03 | 0.04 |
| Spiritual Needs | |||||||||
| Total (SPIR) | 0.28 ** | ||||||||
| Existential (SPIR-EXIST) | 0.33 ** | 0.84 ** | |||||||
| Generativity (SPIR-GEN) | 0.17 ** | 0.84 ** | 0.63 ** | ||||||
| Inner Peace (SPIR-PEACE) | 0.08 * | 0.66 ** | 0.33 ** | 0.50 ** | |||||
| Religious (SPIR-REL) | 0.27 ** | 0.83 ** | 0.67 ** | 0.58 ** | 0.32 ** | ||||
| Religious Coping | |||||||||
| Positive (RCOPE-P) | 0.06 | 0.32 ** | 0.14 ** | 0.30** | 0.24 ** | 0.33 ** | |||
| Negative (RCOPE-N) | −0.16 ** | 0.21 ** | 0.39 ** | 0.07 | −0.16** | 0.30 ** | 0.04 | ||
| Situation Appraisal | |||||||||
| Negative (APP-N) | −0.05 | 0.11 ** | 0.29 ** | −0.01 | −0.11** | 0.15 ** | −0.22 ** | 0.44 ** | |
| Consequent | Antecedent | ANOVA Regression Result | ||||
|---|---|---|---|---|---|---|
| X (APP-N) | M1 (SPIR) | M2 (RCOPE-P) | M3 (RCOPE-N) | |||
| M1 (SPIR) | B | 0.06 | R2 = 0.01 F(1, 742) = 8.51, p < 0.01 | |||
| SE B | 0.02 | |||||
| β | 0.11 ** | |||||
| M2 (RCOPE-P) | B | −0.18 | 0.39 | R2 = 0.12 F(2, 742) = 52.61, p < 0.001 | ||
| SE B | 0.03 | 0.05 | ||||
| β | −0.23 ** | 0.30 ** | ||||
| M3 (RCOPE-N) | B | 0.36 | 0.23 | R2 = 0.24 F(2, 742) = 117.59, p < 0.001 | ||
| SE B | 0.03 | 0.04 | ||||
| β | 0.44 ** | 0.17 ** | ||||
| Y (WELL) | B | −0.18 | 0.45 | −0.07 | −0.25 ** | R2 = 0.09 F(4, 742) = 18.01, p < 0.001 |
| SE B | 0.05 | 0.07 | 0.05 | 0.06 | ||
| β | −0.16 ** | 0.24 ** | −0.05 | −0.18 ** | ||
| Effect | B | SE B | β | 95% CI | t | p | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Specific indirect effect through M1 (APP-N → SPIR → WELL) | 0.028 | 0.011 | 0.025 | 0.008 | 0.053 | ||
| Specific indirect effect through M2 (APP-N → RCOPE-P → WELL) | 0.013 | 0.010 | 0.012 | −0.007 | 0.035 | ||
| Specific indirect effect through M3 (APP-N → RCOPE-N → WELL) | −0.089 | 0.023 | −0.079 | −0.044 | −0.134 | ||
| Specific indirect serial effect through M1 and M2 (APP-N → SPIR → RCOPE-P → WELL) | −0.002 | 0.002 | −0.002 | −0.006 | 0.001 | ||
| Specific indirect serial effect through M1 and M3 (APP-N → SPIR → RCOPE-N → WELL) | −0.004 | 0.002 | −0.003 | −0.001 | −0.008 | ||
| Direct effect of APP-N on WELL (c’, controlled for mediators) | −0.176 | 0.046 | −0.157 | −0.266 | −0.086 | −3.83 | <0.001 |
| Total effect of APP-N on WELL (c, direct and indirect effects) | −0.044 | 0.041 | −0.039 | −0.124 | 0.037 | −1.06 | 0.289 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maier, K.; Konaszewski, K.; Skalski, S.B.; Büssing, A.; Surzykiewicz, J. Spiritual Needs, Religious Coping and Mental Wellbeing: A Cross-Sectional Study among Migrants and Refugees in Germany. Int. J. Environ. Res. Public Health 2022, 19, 3415. https://doi.org/10.3390/ijerph19063415
Maier K, Konaszewski K, Skalski SB, Büssing A, Surzykiewicz J. Spiritual Needs, Religious Coping and Mental Wellbeing: A Cross-Sectional Study among Migrants and Refugees in Germany. International Journal of Environmental Research and Public Health. 2022; 19(6):3415. https://doi.org/10.3390/ijerph19063415
Chicago/Turabian StyleMaier, Kathrin, Karol Konaszewski, Sebastian Binyamin Skalski, Arndt Büssing, and Janusz Surzykiewicz. 2022. "Spiritual Needs, Religious Coping and Mental Wellbeing: A Cross-Sectional Study among Migrants and Refugees in Germany" International Journal of Environmental Research and Public Health 19, no. 6: 3415. https://doi.org/10.3390/ijerph19063415
APA StyleMaier, K., Konaszewski, K., Skalski, S. B., Büssing, A., & Surzykiewicz, J. (2022). Spiritual Needs, Religious Coping and Mental Wellbeing: A Cross-Sectional Study among Migrants and Refugees in Germany. International Journal of Environmental Research and Public Health, 19(6), 3415. https://doi.org/10.3390/ijerph19063415








