Relationship between Food Crushing and Oral Function in Older Adults Requiring Nursing Home Care: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Test Foods
2.3. Test 1 (Free Crush)
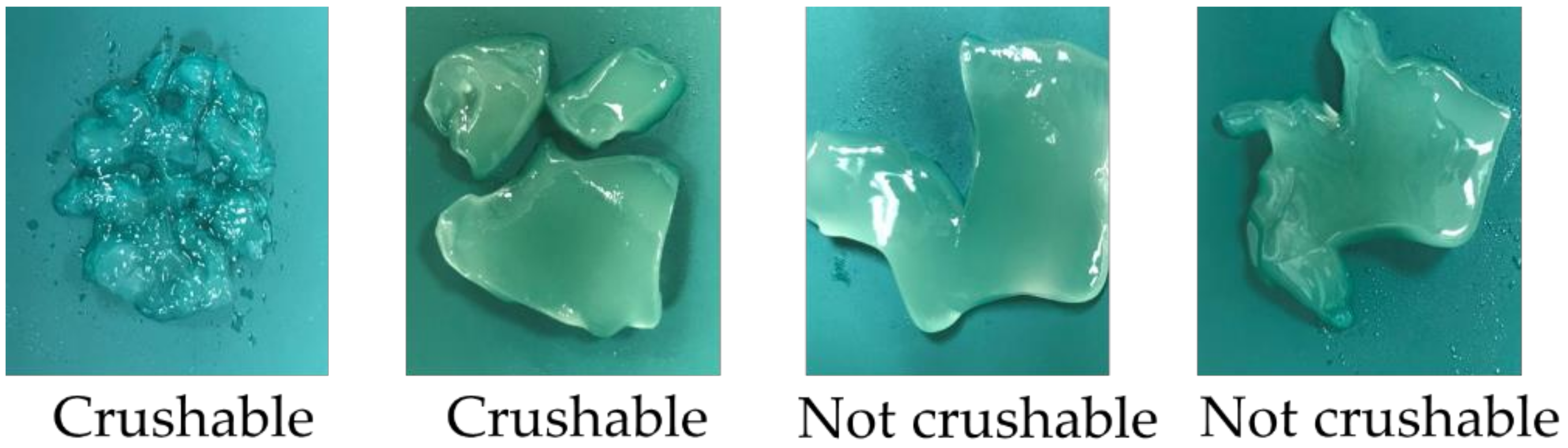
2.3.1. Crushability
2.3.2. Active Sites
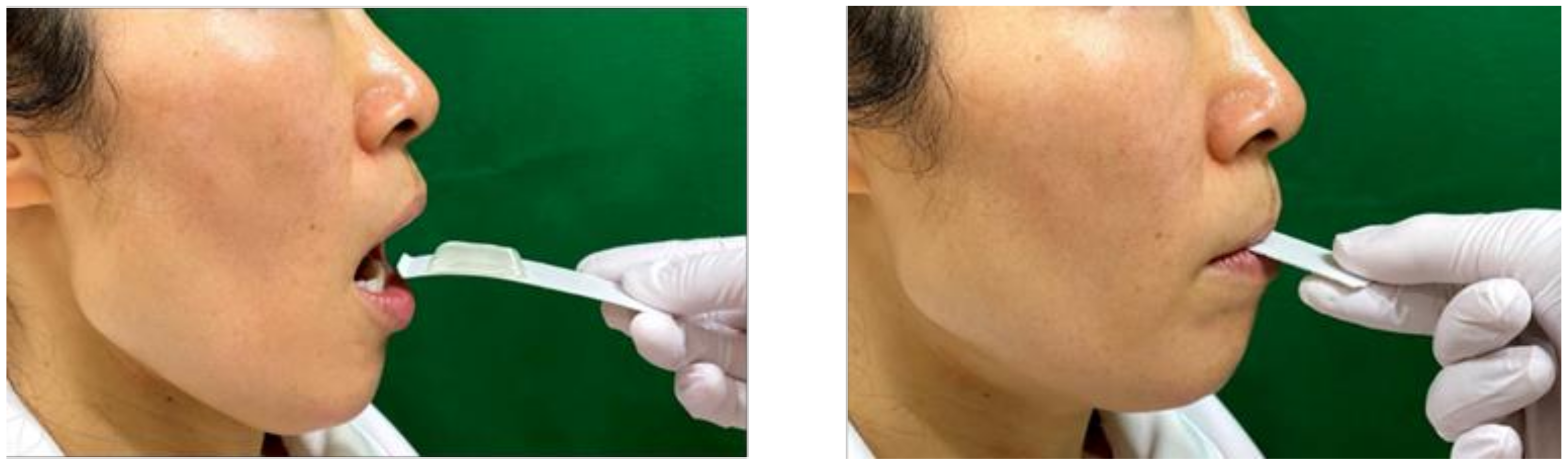
2.4. Test 2 (Tongue Crush)
2.5. Other Parameters of Assessment
2.6. Statistical Analyses
3. Results
3.1. Test 1 (Free Crush)
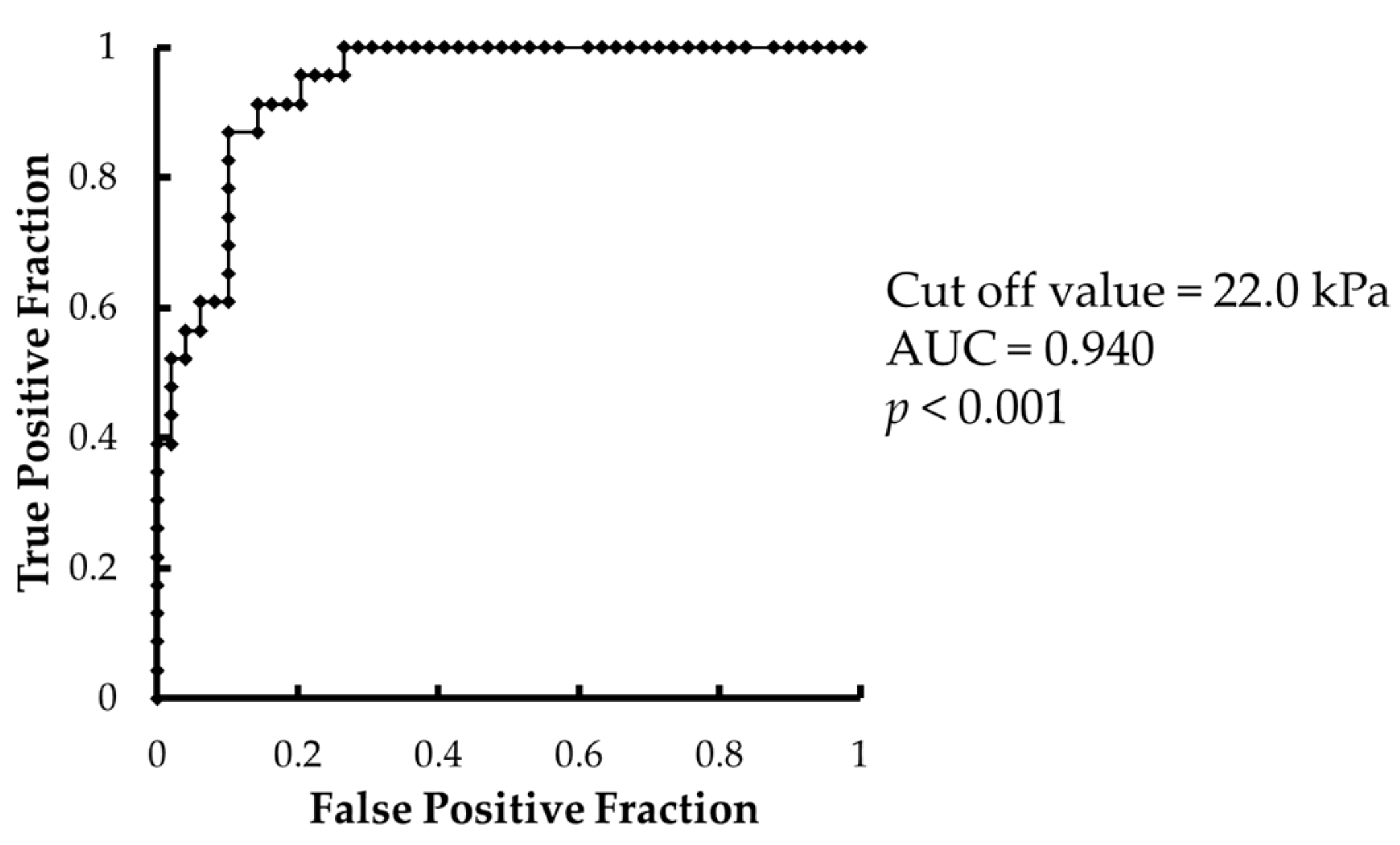
3.2. Test 2 (Tongue Crush)
3.3. Comparison of Crushing Method and the Hardness of the Test Food
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Health, Labour and Welfare (Japan). Vital Statistics of Japan. Available online: http://www.mhlw.go.jp/toukei/list/dl/62-28-02.pdf (accessed on 27 January 2022).
- Shimizu, A.; Maeda, K.; Tanaka, K.; Ogawa, M.; Kayashita, J. Texture-modified diets are associated with decreased muscle mass in older adults admitted to a rehabilitation ward. Geriatr. Gerontol. Int. 2018, 18, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Wong, F.M.F.; Ng, Y.T.Y.; Leung, W.K. Oral health and its associated factors among older institutionalized residents: A systematic review. Int. J. Environ. Res. Public Health 2019, 16, 4132. [Google Scholar] [CrossRef] [Green Version]
- Morisaki, N.; Miura, H.; Hara, S. Relationship between the nutritional status and the oral function among community-dwelling-Dependent elderly persons. Nihon Ronen Igakkai Zasshi 2015, 52, 233–242. (In Japanese) [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taji, T.; Yoshida, M.; Hiasa, K.; Abe, Y.; Tsuga, K.; Akagawa, Y. Influence of mental status on removable prosthesis compliance in institutionalized elderly persons. Int. J. Prosthodont. 2005, 18, 146–149. [Google Scholar] [PubMed]
- Nomura, Y.; Okada, A.; Kakuta, E.; Otsuka, R.; Sogabe, K.; Yamane, K.; Yamamoto, T.; Shigeta, Y.; Shigemoto, S.; Ogawa, T.; et al. Consistency of supplied food and dentition status of the elderly in residential care homes. BMC Oral Health 2019, 19, 74. [Google Scholar] [CrossRef] [Green Version]
- Minakuchi, S.; Takaoka, S.; Ito, J.; Shimoyama, K.; Uematsu, H. Factors affecting denture use in some institutionalized elderly people. Spec. Care Dent. 2006, 26, 101–105. [Google Scholar] [CrossRef] [PubMed]
- E-Stat. Statistics of Japan. Available online: https://www.e-stat.go.jp/dbview?sid=0003411675 (accessed on 27 January 2022).
- Carter, G.; Jancar, J. Sudden deaths in the mentally handicapped. Psychol. Med. 1984, 14, 691–695. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, M.J. Radiographic techniques and interpretation of abnormal swallowing in adult and elderly patients. Dysphagia 1993, 8, 356–358. [Google Scholar] [CrossRef]
- Cichero, J.A.Y.; Lam, P.; Steele, C.M.; Hanson, B.; Chen, J.; Dontas, O.R.; Duivestein, J.; Kayashita, J.; Lecko, C.; Murray, J.; et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: The IDDSI Framework. Dysphagia 2017, 32, 293–314. [Google Scholar] [CrossRef] [Green Version]
- Sakai, M.; Egashira, F.; Kanaya, S.; Kayashita, J. Comparison of food physical properties with reference to clinically effective stepwise swallowing foods. Jpn. J. Dysphagia Rehabil. 2006, 10, 239–248. (In Japanese) [Google Scholar]
- Okamoto, N.; Amano, N.; Nakamura, T.; Yanagi, M. Relationship between tooth loss, low masticatory ability, and nutritional indices in the elderly: A cross-sectional study. BMC Oral Health 2019, 19, 110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonni, I.; Riccardi, G.; Piancino, M.G.; Stretti, C.; Costantinides, F.; Paganelli, C. The influence of food hardness on the physiological parameters of mastication: A systematic review. Arch. Oral Biol. 2020, 120, 104903. [Google Scholar] [CrossRef]
- Park, H.S.; Kim, D.K.; Lee, S.Y.; Park, K.H. The effect of aging on mastication and swallowing parameters according to the hardness change of solid food. J. Texture Stud. 2017, 48, 362–369. [Google Scholar] [CrossRef]
- Universal Design Food. Japan Food Care Conference. Available online: https://www.udf.jp/outline/udf.html (accessed on 27 January 2022).
- Yamagata, Y.; Itadani, R.; Ikarashi, S.; Kayashita, A.; Niu, K.; Hikino, Y.; Kawashima, K.; Ooba, K.; Kayashita, J. Evaluation of classification of universal design foods corresponding to the code of japanese dysphagia diet 2013 by the JSDR dysphagia diet committee. Jpn. J. Dysphagia Rehabil. 2021, 25, 81–89. (In Japanese) [Google Scholar]
- Watanabe, E.; Tokoi, T.; Tsuji, H.; Shido, R.; Wakabayashi, H.; Abe, M.; Ishii, M.; Mihara, A.; Kayashita, J.; Kogirima, M. Measurement of meal hardness following code 4 in JDD2013. Jpn. J. Dysphagia Rehabil. 2020, 24, 130–142. (In Japanese) [Google Scholar]
- Wang, I.C. International Classification Systems for Texture-Modified Foods. Hu Li Za Zhi 2020, 67, 24–32. (In Japanese) [Google Scholar] [PubMed]
- Tomimatsu, H.; Yanagisawa, Y. Efforts using commercially available universal design food to improve the provision of meals at elder nursing home. J. Wayo Women’s Univ. 2020, 61, 91–102. (In Japanese) [Google Scholar]
- Hayashi, R.; Tsuga, K.; Hosokawa, R.; Yoshida, M.; Sato, Y.; Akagawa, Y. A novel handy probe for tongue pressure measurement. Int. J. Prosthodont. 2002, 15, 385–388. [Google Scholar]
- Tsuga, K.; Maruyama, M.; Yoshikawa, M.; Yoshida, M.; Akagawa, Y. Manometric evaluation of oral function with a hand-held balloon probe. J. Oral Rehabil. 2011, 38, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Utanohara, Y.; Hayashi, R.; Yoshikawa, M.; Yoshida, M.; Tsuga, K.; Akagawa, Y. Standard values of maximum tongue pressure taken using newly developed disposable tongue pressure measurement device. Dysphagia 2008, 23, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Tsuga, K.; Yoshikawa, M.; Oue, H.; Okazaki, Y.; Tsuchioka, H.; Maruyama, M.; Yoshida, M.; Akagawa, Y. Maximal voluntary tongue pressure is decreased in Japanese frail elderly persons. Gerodontology 2012, 29, e1078–e1085. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Kikutani, T.; Tsuga, K.; Utanohara, Y.; Hayashi, R.; Akagawa, Y. Decreased tongue pressure reflects symptom of dysphagia. Dysphagia 2006, 21, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Robbins, J.; Levine, R.; Wood, J.; Roecker, E.B.; Luschei, E. Age effects on lingual pressure generation as a risk factor for dysphagia. J. Gerontol. A Biol. Sci. Med. Sci. 1995, 50, M257–M262. [Google Scholar] [CrossRef] [PubMed]
- Yamada, A.; Kanazawa, M.; Komagamine, Y.; Minakuchi, S. Association between tongue and lip functions and masticatory performance in young dentate adults. J. Oral Rehabil. 2015, 42, 833–839. [Google Scholar] [CrossRef]
- Rosenthal, A.J. Texture profile analysis—How important are the parameters? J. Texture Stud. 2010, 41, 672–684. [Google Scholar] [CrossRef]
- Hata, Y.; Shimizu, T.; Fujioka, S. Investigation of transit time of bolus through the oral cavity using gelatin jelly and thickened water. Jpn. J. Dysphagia Rehabil. 2007, 11, 97–103. (In Japanese) [Google Scholar]
- Komino, M.; Shiga, H. Changes in mandibular movement during chewing of different hardness foods. Odontology 2017, 105, 418–425. [Google Scholar] [CrossRef] [Green Version]
- Rubenstein, L.Z.; Harker, J.O.; Salvà, A.; Guigoz, Y.; Vellas, B. Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef] [Green Version]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. ‘Mini-mental state’: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Palmer, J.B.; Rudin, N.J.; Lara, G.; Crompton, A.W. Coordination of mastication and swallowing. Dysphagia 1992, 7, 187–200. [Google Scholar] [CrossRef] [PubMed]
- Lamy, M.; Mojon, P.; Kalykakis, G.; Legrand, R.; Butz-Jorgensen, E. Oral status and nutrition in the institutionalized elderly. J. Dent. 1999, 27, 443–448. [Google Scholar] [CrossRef]
- Kikutani, T.; Yoshida, M.; Enoki, H.; Yamashita, Y.; Akifusa, S.; Shimazaki, Y.; Hirano, H.; Tamura, F. Relationship between nutrition status and dental occlusion in community-dwelling frail elderly people. Geriatr. Gerontol. Int. 2013, 13, 50–54. [Google Scholar] [CrossRef]
- Kanehisa, Y.; Yoshida, M.; Taji, T.; Akagawa, Y.; Nakamura, H. Body weight and serum albumin change after prosthodontic treatment among institutionalized elderly in a long-term care geriatric hospital. Community Dent. Oral Epidemiol. 2009, 37, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Hiiemae, K.; Heath, M.R.; Heath GKazazoglu, E.; Murray, J.; Sapper, D.; Hamblett, K. Natural bites, food consistency and feeding behaviour in man. Arch. Oral Biol. 1996, 41, 175–189. [Google Scholar] [CrossRef]
- Yokoyama, S.; Hori, K.; Tamine, K.; Fuhiwara, S.; Inoue, M.; Maeda, Y.; Funami, T.; Ishihara, S.; Ono, T. Tongue pressure modulation for initial gel consistency in a different oral strategy. PLoS ONE 2014, 9, e91920. [Google Scholar] [CrossRef] [Green Version]
- Kojima, C.; Ohno, T.; Hasegawa, T.; Fujita, D. Influence of palatal height on the pattern of chewing semi-solid foods: A new proposition to the swallowing approach. Jpn. J. Dysphagia Rehabil. 2013, 17, 25–35. (In Japanese) [Google Scholar]
| Active Site | Mandibular Movement | Food Stay | How to Crush |
|---|---|---|---|
| Teeth–teeth | Cycle toward right or leftfor mastication | On teeth | By occlusion between maxillary and mandibular residual or artificial teeth |
| Teeth–ridge | Cycle toward right or left | On teeth or ridge | Between the maxillary or mandibular residual or artificial teeth and residual ridge in the opposing arch |
| Ridge–ridge | Cycle toward right or left | On ridge | Between the maxillary and mandibular ridges |
| Tongue | Cycle or up and down | On tongue | By pressing the test food between the tongue and palate |
| Presence or Absence of Occlusal Support | Total | p-Value | ||
|---|---|---|---|---|
| Present | Absent | |||
| Denture usage | ||||
| Yes | 31 (43.1%) | 5 (6.9%) | 36 (50.0%) | |
| No | 16 (22.2%) | 20 (27.8%) | 36 (50.0%) | <0.001 |
| Food form | ||||
| Normal food | 25 (34.7%) | 2 (2.8%) | 27 (37.5%) | |
| Chopped food | 18 (25.0%) | 17 (23.6%) | 35 (48.6%) | |
| Modified diet for dysphagia | 4 (5.6%) | 6 (8.3%) | 10 (13.9%) | <0.001 |
| Number of remaining teeth | 13.1 ± 9.6 | 4.5 ± 4.5 | <0.05 | |
| 47 (65.3%) | 25 (34.7%) | 72 (100%) | ||
| Teeth–Teeth | Teeth–Ridge | Ridge–Ridge | Tongue | Total | |
|---|---|---|---|---|---|
| Age | |||||
| (years) | 85.4 ± 6.6 | 86.7 ± 6.2 | 85.0 ± 4.9 | 85.3 ± 10.4 | |
| Sex, n (%) | |||||
| (Male) | 8 (11.1%) | 4 (5.6%) | 3 (4.2%) | 1 (1.4%) | 16 (22.2%) |
| (Female) | 33 (45.8%) | 11 (15.3%) | 7 (9.7%) | 5 (6.9%) | 56 (77.8%) |
| Occlusal support | |||||
| Present | 41 (56.9%) | 1 (1.4%) | 0 | 5 (6.9%) | 47 (65.3%) |
| Absent | 0 | 14 (19.4%) | 10 (13.9%) | 1 (1.4%) | 25 (34.7%) |
| Food form | |||||
| Normal food | 25 (34.7%) | 1 (1.4%) | 1 (1.4%) | 0 | 27 (37.5%) |
| Chopped food | 15 (20.8%) | 10 (13.9%) | 8 (11.1%) | 2 (2.8%) | 35 (48.6%) |
| Modified diet for dysphagia | 1 (1.4%) | 4 (5.6%) | 1 (1.4%) | 4 (5.6%) | 10 (13.9%) |
| ADL * | |||||
| Ambulatory | 21 (29.2%) | 5 (6.9%) | 5 (6.9%) | 0 | 31 (43.1%) |
| Wheelchair use | 19 (26.4%) | 9 (12.5%) | 5 (6.9%) | 4 (5.6%) | 37 (51.4%) |
| Bedridden | 1 (1.4%) | 1 (1.4%) | 0 | 2 (2.8%) | 4 (5.6%) |
| Nutrition status | |||||
| Good | 9 (12.5%) | 0 | 1 (1.4%) | 0 | 10 (13.9%) |
| At risk | 29 (40.3%) | 11 (15.3%) | 7 (9.7%) | 3 (4.2%) | 50 (69.4%) |
| Malnutrition | 3 (4.2%) | 4 (5.6%) | 2 (2.8%) | 3 (4.2%) | 12 (16.7%) |
| MMSE | |||||
| (score) | 18.2 ± 6.6 | 14.3 ± 5.5 | 13.4 ± 8.6 | 12.8 ± 7.0 | |
| Tongue pressure ** | |||||
| (kPa) | 18.8 ± 8.1 | 20.8 ± 9.0 | 19.0 ± 8.8 | 6.4 ± 3.9 | |
| 41 (56.9%) | 15 (20.8%) | 10 (13.9%) | 6 (8.3%) | 72 (100%) |
| Crushable | Not Crushable | p-Value | |
|---|---|---|---|
| SJ | |||
| Participants, n (%) | 70 (97.2%) | 2 (2.8%) | |
| (Active site) | |||
| Teeth–teeth | 41 (56.9%) | 0 | |
| Teeth–ridge | 15 (20.8%) | 0 | |
| Ridge–ridge | 10 (13.9%) | 0 | |
| Tongue | 4 (5.6%) | 2 (2.8%) | |
| Tongue pressure (kPa) | 18.6 ± 8.6 | 3.6 ± 1.0 | <0.05 |
| HJ | |||
| Participants | 62 (86.1%) | 10 (13.9%) | |
| (Active site) | |||
| Teeth–teeth | 41 (56.9%) | 0 | |
| Teeth–ridge | 12 (16.7%) | 3 (4.2%) | |
| Ridge–ridge | 9 (12.5%) | 1 (1.4%) | |
| Tongue | 0 | 6 (8.3%) | |
| Tongue pressure (kPa) | 19.4 ± 8.3 | 11.0 ± 8.7 | <0.01 |
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Active site | 0.10 | 0.02–0.48 | <0.01 |
| Presence or absence of occlusal support | 0.12 | 0.01–2.79 | 0.187 |
| MMSE | 1.08 | 0.90–1.29 | 0.389 |
| Tongue pressure (kPa) | 1.01 | 0.86–1.17 | 0.941 |
| Crushable | Not Crushable | p-Value | |
| SJ | |||
| Participants, n (%) | 64 (88.9%) | 8 (11.1%) | |
| Tongue pressure (kPa) | 20.1 ± 7.5 | 3.4 ± 1.4 | <0.001 |
| HJ | |||
| Participants | 23 (31.9%) | 49 (68.1%) | |
| Tongue pressure (kPa) | 26.8 ± 5.5 | 14.2 ± 6.9 | <0.001 |
| Test 1 (Free Crush) | Test 2 (Tongue Crush) | p-Value | |||
|---|---|---|---|---|---|
| Crushable | Not Crushable | Crushable | Not Crushable | ||
| Participants | |||||
| SJ | 70 | 2 | 64 | 8 | 0.0492 |
| HJ | 62 | 10 | 23 | 49 | <0.001 |
| p-value | 0.0159 | <0.001 | |||
| Tongue pressure (kPa) | |||||
| SJ | 18.6 ± 8.6 | 20.1 ± 7.5 | 0.305 | ||
| HJ | 19.4 ± 8.3 | 26.8 ± 5.5 | <0.001 | ||
| p-value | 0.615 | <0.001 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamawaki, K.; Mori, T.; Itaki, S.; Haruta, A.; Takeda, C.; Hiraoka, A.; Maruyama, M.; Yoshikawa, M.; Yoshida, M.; Tsuga, K. Relationship between Food Crushing and Oral Function in Older Adults Requiring Nursing Home Care: A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 3419. https://doi.org/10.3390/ijerph19063419
Yamawaki K, Mori T, Itaki S, Haruta A, Takeda C, Hiraoka A, Maruyama M, Yoshikawa M, Yoshida M, Tsuga K. Relationship between Food Crushing and Oral Function in Older Adults Requiring Nursing Home Care: A Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(6):3419. https://doi.org/10.3390/ijerph19063419
Chicago/Turabian StyleYamawaki, Kanako, Takahiro Mori, Sakiko Itaki, Azusa Haruta, Chiho Takeda, Aya Hiraoka, Mariko Maruyama, Mineka Yoshikawa, Mitsuyoshi Yoshida, and Kazuhiro Tsuga. 2022. "Relationship between Food Crushing and Oral Function in Older Adults Requiring Nursing Home Care: A Pilot Study" International Journal of Environmental Research and Public Health 19, no. 6: 3419. https://doi.org/10.3390/ijerph19063419
APA StyleYamawaki, K., Mori, T., Itaki, S., Haruta, A., Takeda, C., Hiraoka, A., Maruyama, M., Yoshikawa, M., Yoshida, M., & Tsuga, K. (2022). Relationship between Food Crushing and Oral Function in Older Adults Requiring Nursing Home Care: A Pilot Study. International Journal of Environmental Research and Public Health, 19(6), 3419. https://doi.org/10.3390/ijerph19063419







