Effects of Problem-Based Learning Strategies on Undergraduate Nursing Students’ Self-Evaluation of Their Core Competencies: A Longitudinal Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Research Design and Subjects
2.2. Measures
2.3. Data Collection and Analysis
3. Results
3.1. Characteristics of the Nursing Students
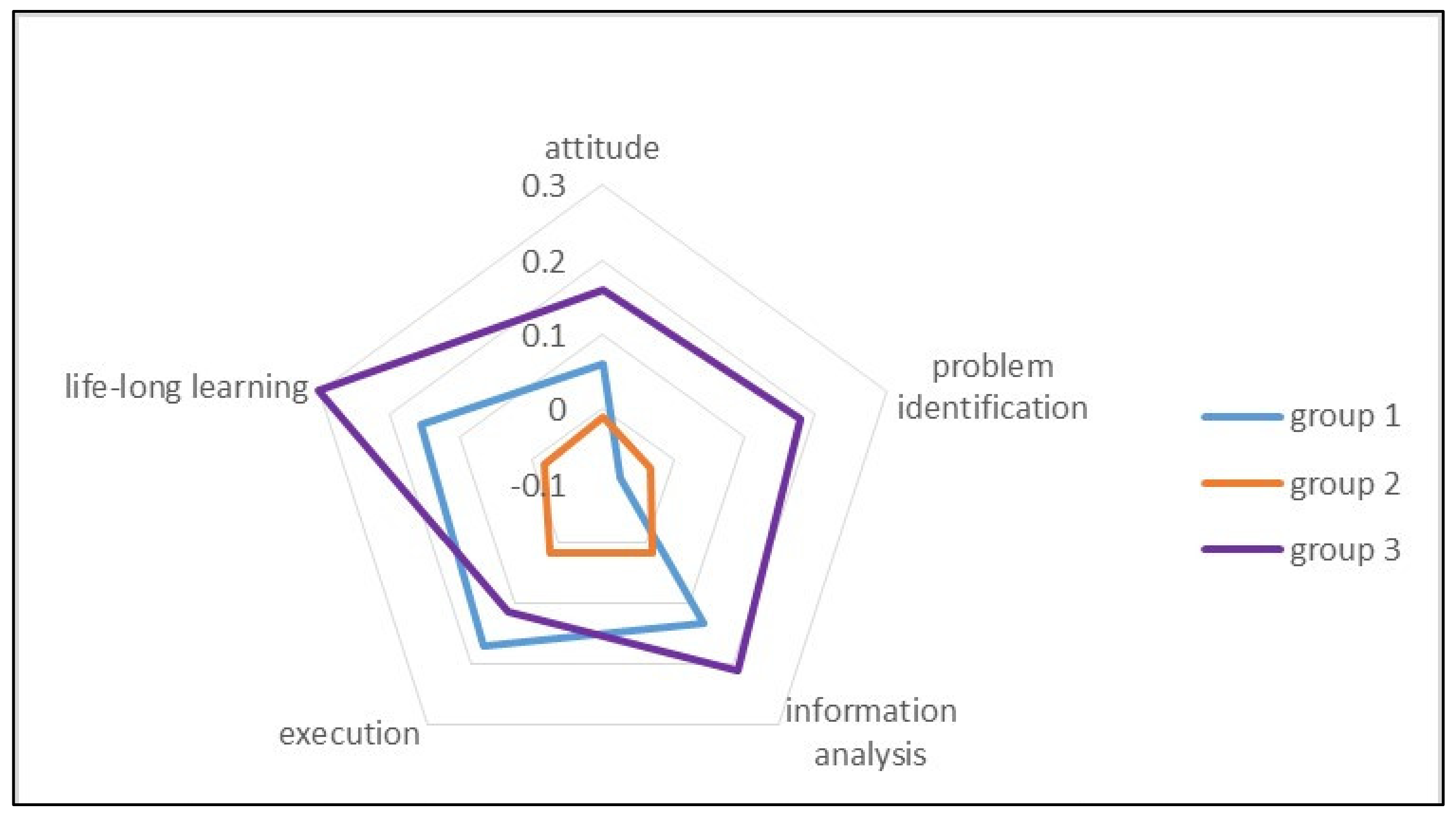
3.2. Comparison of the Differences in Students’ Self-Evaluations of Core Competencies between Groups
3.3. Predicted Changes in the Students’Sself-Evaluations of Their Core Competencies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Erstad, O.; Voogt, J. The Twenty-First Century Curriculum: Issues and Challenges. In Second Handbook of Information Technology in Primary and Secondary Education; Voogt, Í.J., Knezek, G., Christensen, R., Lai, K.-W., Eds.; Springer International Publishing: Cham, Switzerland, 2018. [Google Scholar] [CrossRef]
- Hodges, H.F. Preparing New Nurses with Complexity Science and Problem-Based Learning. J. Nurs. Educ. 2011, 50, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Salari, M.; Roozbehi, A.; Zarifi, A.; Tarmizi, R.A. Pure PBL, Hybrid PBL and Lecturing: Which one is more effective in developing cognitive skills of undergraduate students in pediatric nursing course? BMC Med. Educ. 2018, 18, 195. [Google Scholar] [CrossRef] [PubMed]
- Khatiban, M.; Falahan, S.N.; Amini, R.; Farahanchi, A.; Soltanian, A. Lecture-based versus problem-based learning in ethics education among nursing students. Nurs. Ethics 2018, 26, 1753–1764. [Google Scholar] [CrossRef] [PubMed]
- Khatiban, M.; Sangestani, G. The effects of using problem-based learning in the clinical nursing education on the students’ outcomes in Iran: A quasi-experimental study. Nurse Educ. Pract. 2014, 14, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Gewurtz, R.E.; Coman, L.; Dhillon, S.; Jung, B.; Solomon, P. Problem-based Learning and Theories of Teaching and Learning in Health Professional Education. J. Perspect. Appl. Acad. Pract. 2016, 4, 59–70. [Google Scholar] [CrossRef]
- Woods, C.; West, C.; Mills, J.; Park, T.; Southern, J.; Usher, K. Undergraduate student nurses’ self-reported preparedness for practice. Collegian 2015, 22, 359–368. [Google Scholar] [CrossRef]
- Billings, D.M.; Halstead, J.A. Teaching in Nursing-E-Book: A Guide for Faculty; Elsevier Health Sciences: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Chang, M.J.; Chang, Y.-J.; Kuo, S.-H.; Yang, Y.-H.; Chou, F.-H. Relationships between critical thinking ability and nursing competence in clinical nurses. J. Clin. Nurs. 2011, 20, 3224–3232. [Google Scholar] [CrossRef]
- Kwan, C.-Y.; Lee, M.-C. From Problem-Based Learning in Classrooms to Holistic Health Care in Workplaces with Special Emphasis in Chinese Societies. J. Med. Health 2018, 7, 1–15. [Google Scholar]
- Waldron, M.K.; Washington, S.L.; Montague, G.P. Cooperative Clinical Conferences: Nursing Student Pediatric Clinical Innovation. J. Nurs. Educ. 2016, 55, 416–419. [Google Scholar] [CrossRef] [PubMed]
- Missildine, K.; Fountain, R.; Summers, L.; Gosselin, K. Flipping the Classroom to Improve Student Performance and Satisfaction. J. Nurs. Educ. 2013, 52, 597–599. [Google Scholar] [CrossRef] [PubMed]
- Gustin, M.-P.; Abbiati, M.; Bonvin, R.; Gerbase, M.W.; Baroffio, A. Integrated problem-based learning versus lectures: A path analysis modelling of the relationships between educational context and learning approaches. Med. Educ. Online 2018, 23, 1489690. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Mejías, E.; Amezcua-Prieto, C.; Martínez-Ruiz, V.; Olvera-Porcel, M.C.; Jiménez-Moleón, J.J.; Lardelli Claret, P. Medical students’ satisfaction and academic performance with problem-based learning in practice-based exercises for epidemiology and health demographics. Innov. Educ. Teach. Int. 2015, 52, 510–521. [Google Scholar] [CrossRef]
- Taylor, T.R.D.D.; Mifflin, B. Problem-based learning: Where are we now? Med. Teach. 2008, 30, 742–763. [Google Scholar] [CrossRef] [PubMed]
- Edwards, D.; Hawker, C.; Carrier, J.; Rees, C. A systematic review of the effectiveness of strategies and interventions to improve the transition from student to newly qualified nurse. Int. J. Nurs. Stud. 2015, 52, 1254–1268. [Google Scholar] [CrossRef]
- Williams, B.; Richard, L.; Al Sayah, F. The influence of undergraduate education on professional practice transition: A comparative descriptive study. Nurse Educ. Today 2015, 35, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-F.; Lu, M.-S.; Chung, C.-C.; Yang, C.-M. A comparison of problem-based learning and conventional teaching in nursing ethics education. Nurs. Ethic 2010, 17, 373–382. [Google Scholar] [CrossRef]
- Choi, H. A problem-based learning trial on the Internet involving undergraduate nursing students. J. Nurs. Educ. 2003, 42, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Kwan, C.-Y. Problem-based Learning (PBL) in Medical Education in Taiwan: Observations and a Commentary. J. Med. Health 2017, 6, 1–11. [Google Scholar]
- Kong, L.-N.; Qin, B.; Zhou, Y.-Q.; Mou, S.-Y.; Gao, H.-M. The effectiveness of problem-based learning on development of nursing students’ critical thinking: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2013, 51, 458–469. [Google Scholar] [CrossRef]
- McMahon, M.A.; Christopher, K.A. Case Study Method and Problem-Based Learning: Utilizing the Pedagogical Model of Progressive Complexity in Nursing Education. Int. J. Nurs. Educ. Sch. 2011, 8, 1–16. [Google Scholar] [CrossRef]
- Pilcher, J. Promoting Learning Using Case-Based Strategies in Nursing Professional Development. J. Nurses Prof. Dev. 2018, 34, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Rico, R.; Ertmer, P.A. Examining the Role of the Instructor in Problem-centered Instruction. TechTrends 2015, 59, 96–103. [Google Scholar] [CrossRef]
- Hung, T.-M.; Tang, L.-C.; Ko, C.-J. How Mental Health Nurses Improve Their Critical Thinking Through Problem-Based Learning. J. Nurses Prof. Dev. 2015, 31, 170–175. [Google Scholar] [CrossRef]
- He, Y.; Du, X.; Toft, E.; Zhang, X.; Qu, B.; Shi, J.; Zhang, H.; Zhang, H. A comparison between the effectiveness of PBL and LBL on improving problem-solving abilities of medical students using questioning. Innov. Educ. Teach. Int. 2017, 55, 44–54. [Google Scholar] [CrossRef]
- Prosser, M.; Sze, D. Problem-based learning: Student learning experiences and outcomes. Clin. Linguist. Phon. 2013, 28, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Wosinski, J.; Belcher, A.E.; Dürrenberger, Y.; Allin, A.-C.; Stormacq, C.; Gerson, L. Facilitating problem-based learning among undergraduate nursing students: A qualitative systematic review. Nurse Educ. Today 2018, 60, 67–74. [Google Scholar] [CrossRef]
- Zhou, Z. An Empirical Study on the Influence of PBL Teaching Model on College Students’ Critical Thinking Ability. Engl. Lang. Teach. 2018, 11, 15–20. [Google Scholar] [CrossRef]
- Lee, M.; Wimmers, P.F. Validation of a performance assessment instrument in problem-based learning tutorials using two cohorts of medical students. Adv. Health Sci. Educ. Theory Pract. 2016, 21, 341–357. [Google Scholar] [CrossRef]
- Gholami, M.; Moghadam, P.K.; Mohammadipoor, F.; Tarahi, M.J.; Saki, M.; Toulabi, T.; Pour, A.H.H. Comparing the effects of problem-based learning and the traditional lecture method on critical thinking skills and metacognitive awareness in nursing students in a critical care nursing course. Nurse Educ. Today 2016, 45, 16–21. [Google Scholar] [CrossRef]
- Fernandez-Sola, C.; Granero-Molina, J.; Aguilera-Manrique, G.; Peredo-de Gonzales, M.H.; Castro-Sánchez, A.M.; Pérez Galdeano, A. Strategies to develop the nursing process and nursing care plans in the health system in Bolivia. Int. Nurs. Rev. 2011, 58, 392–399. [Google Scholar] [CrossRef]
- Jeon, J.; Park, S. Self-Directed Learning versus Problem-Based Learning in Korean Nurse Education: A Quasi-Experimental Study. Healthcare 2021, 9, 1763. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.B.; Williams, B.A.; Yin, L.; Liu, M.; Fang, J.B.; Pang, D. Nursing students’ views on the effectiveness of problem-based learning. Nurse Educ. Today 2011, 31, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Alrahlah, A. How effective the problem-based learning (PBL) in dental education. A critical review. Saudi Dent. J. 2016, 28, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Compton, R.M.; Owilli, A.O.; Norlin, E.E.; Murdoch, N.L.H. Does problem-based learning in Nursing Education Empower Learning? Nurse Educ. Pract. 2020, 44, 2752. [Google Scholar] [CrossRef] [PubMed]
- Svensson, J.; Axén, A.; Andersson, E.K.; Hjelm, M. Nursing students’ experiences of what influences achievement of learning outcomes in a problem-based learning context: A qualitative descriptive study. Nurs. Open 2021, 8, 1863–1869. [Google Scholar] [CrossRef]
- Spiers, J.; Williams, B.; Gibson, B.; Kabotoff, W.; McIlwraith, D.; Sculley, A.; Richard, E. Graduate nurses’ learning trajectories and experiences of Problem Based Learning: A focused ethnography study. Int. J. Nurs. Stud. 2014, 51, 1462–1471. [Google Scholar] [CrossRef]
- Schmidt, H.G.; Rotgans, J.; Yew, E.H.J. The process of problem-based learning: What works and why. Med. Educ. 2011, 45, 792–806. [Google Scholar] [CrossRef]
- McLean, M.; Van Wyk, J.M.; Peters-Futre, E.M.; Higgins-Opitz, S.B. The small group in problem-based learning: More than a cognitive ‘learning’ experience for first-year medical students in a diverse population. Med. Teach. 2006, 28, e94–e103. [Google Scholar] [CrossRef]
- Jamshidi, H.; Maslakpak, M.H.; Parizad, N. Does problem-based learning education improve knowledge, attitude, and perception toward patient safety among nursing students? A randomized controlled trial. BMC Nurs. 2021, 20, 70. [Google Scholar] [CrossRef]
- Shin, I.-S.; Kim, J.-H. The effect of problem-based learning in nursing education: A meta-analysis. Adv. Health Sci. Educ. 2013, 18, 1103–1120. [Google Scholar] [CrossRef]
- Millanzi, W.C.; Kibusi, S.M. Exploring the effect of problem based facilitatory teaching approach on motivation to learn: A quasi-experimental study of nursing students in Tanzania. BMC Nurs. 2021, 20, 3. [Google Scholar] [CrossRef] [PubMed]
| Dimensions | Number of Items | Items Indicators |
|---|---|---|
| Learning Attitudes | 4 | I like solving problems regarding the group project with team members. I enjoy cooperative learning with team members. When I encounter a problem, I learn to think, understand and analyze the problem first. I have learned to tolerate and respect different opinions. |
| Problem Identification | 2 | I can identify problems from the case scenarios provided. I am familiar with problem-solving techniques. |
| Information Analysis | 3 | It is easy for me to find the appropriate references to meet course objectives. I can evaluate the credibility and reliability of data or information retrieved. I can conclude from the information retrieved. |
| Execution | 3 | I can come up with strategies to solve problems. I can provide safe and competent care when dealing with individual clients. I can apply communication skills to build a trusting nurse-patient relationship. |
| Lifelong Learning | 4 | I can connect academic learning to practical problems. I can apply the knowledge and skills I have learned to clinical practice and my personal life. I think I am a self-directed learner. I often think about how to improve my learning and problem-solving skills. |
| Group | Male, n (%) | Female, n (%) | X2 | Sig. |
|---|---|---|---|---|
| Group 1 | 22 (37.9) | 84 (31.8) | 1.940 | 0.379 |
| Group 2 | 16 (27.6) | 95 (36.0) | ||
| Group 3 | 20 (34.5) | 85 (32.2) |
| Variable | n | Mean | SD | Mean of Difference | SD of Difference | 95% C.I. | t | p-Value | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Learning attitude | |||||||||
| Group 1 pre | 106 | 3.7571 | 0.54167 | ||||||
| post | 106 | 3.6958 | 0.62010 | ||||||
| 0.06132 | 0.69933 | −0.07336 | 0.19600 | 0.903 | 0.369 | ||||
| Group 2 pre | 111 | 3.8333 | 0.67026 | ||||||
| post | 111 | 3.8446 | 0.53625 | ||||||
| −0.01126 | 0.58035 | −0.12043 | 0.09790 | −0.204 | 0.838 | ||||
| Group 3 pre | 105 | 4.0881 | 0.51653 | ||||||
| post | 105 | 3.9286 | 0.57566 | ||||||
| 0.15952 | 0.59860 | 0.04368 | 0.27537 | 2.731 | 0.007 | ||||
| Problem identification | |||||||||
| Group 1 pre | 106 | 3.2783 | 0.77791 | ||||||
| post | 106 | 3.3538 | 0.72692 | ||||||
| −0.07547 | 0.96558 | −0.26143 | 0.11049 | −0.805 | 0.423 | ||||
| Group 2 pre | 111 | 3.4640 | 0.77960 | ||||||
| post | 111 | 3.4955 | 0.69248 | ||||||
| −0.03153 | 0.76062 | −0.17460 | 0.11154 | −0.437 | 0.663 | ||||
| Group 3 pre | 106 | 3.8726 | 0.62129 | ||||||
| post | 106 | 3.6934 | 0.70566 | ||||||
| 0.17925 | 0.76591 | 0.03174 | 0.32675 | 2.409 | 0.018 | ||||
| Information analysis | |||||||||
| Group 1 pre | 106 | 3.6195 | 0.57171 | ||||||
| post | 106 | 3.4874 | 0.70699 | ||||||
| 0.13208 | 0.73848 | −0.01015 | 0.27430 | 1.841 | 0.068 | ||||
| Group 2 pre | 111 | 3.7447 | 0.71627 | ||||||
| post | 111 | 3.7297 | 0.60388 | ||||||
| 0.01502 | 0.62180 | −0.10195 | 0.13198 | 0.254 | 0.800 | ||||
| Group 3 pre | 106 | 4.0220 | 0.54872 | ||||||
| post | 106 | 3.8113 | 0.59986 | ||||||
| 0.21069 | 0.61088 | 0.09304 | 0.32834 | 3.551 | 0.001 | ||||
| Execution | |||||||||
| Group 1 pre | 106 | 3.7233 | 0.66424 | ||||||
| post | 106 | 3.5535 | 0.69142 | ||||||
| 0.16981 | 0.74783 | 0.02579 | 0.31383 | 2.338 | 0.021 | ||||
| Group 2 pre | 111 | 3.8228 | 0.66183 | ||||||
| post | 111 | 3.8048 | 0.63161 | ||||||
| 0.01802 | 0.63220 | −0.10090 | 0.13693 | 0.300 | 0.765 | ||||
| Group 3 pre | 106 | 3.9937 | 0.59269 | ||||||
| post | 106 | 3.8805 | 0.68265 | ||||||
| 0.11321 | 0.67281 | −0.01637 | 0.24278 | 1.732 | 0.086 | ||||
| Life-long learning | |||||||||
| Group 1 pre | 106 | 3.6840 | 0.65946 | ||||||
| post | 106 | 3.5283 | 0.66576 | ||||||
| 0.15566 | 0.75786 | 0.00971 | 0.30161 | 2.115 | 0.037 | ||||
| Group 2 pre | 111 | 3.6847 | 0.75431 | ||||||
| post | 111 | 3.7027 | 0.64975 | ||||||
| −0.01802 | 0.68234 | −0.14637 | 0.11033 | −0.278 | 0.781 | ||||
| Group 3 pre | 106 | 4.0896 | 0.58268 | ||||||
| post | 106 | 3.7901 | 0.75288 | ||||||
| 0.29953 | 0.67119 | 0.17026 | 0.42879 | 4.595 | <0.000 | ||||
| Total scale | |||||||||
| Group 1 pre | 106 | 3.6468 | 0.49657 | ||||||
| post | 106 | 3.5454 | 0.57674 | ||||||
| 0.10142 | 0.61106 | −0.01627 | 0.21910 | 1.709 | 0.090 | ||||
| Group 2 pre | 111 | 3.7314 | 0.63063 | ||||||
| post | 111 | 3.7365 | 0.52928 | ||||||
| −0.00507 | 0.51020 | −0.10104 | 0.09090 | −0.105 | 0.917 | ||||
| Group 3 pre | 105 | 4.0327 | 0.49404 | ||||||
| post | 105 | 3.8304 | 0.58558 | ||||||
| 0.20238 | 0.51206 | 0.10328 | 0.30148 | 4.050 | <0.000 | ||||
| Dependent Variable | Parameter | B | S.E. | 95% Wald C.I. | Wald X2 | p-Value | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Learning attitude | 1 Group 3 | 0.223 | 0.0783 | 0.070 | 0.377 | 8.141 | 0.004 |
| 1 Group 2 | 0.159 | 0.0749 | 0.013 | 0.306 | 4.532 | 0.033 | |
| 2 time 2 | 0.063 | 0.0665 | −0.067 | 0.193 | 0.899 | 0.343 | |
| 3 Group 3 × time 2 | 0.084 | 0.0880 | −0.089 | 0.256 | 0.904 | 0.342 | |
| 4 Group 2 × time 2 | −0.084 | 0.0865 | −0.254 | 0.085 | 0.949 | 0.330 | |
| Problem identification | 1 Group 3 | 0.347 | 0.0954 | 0.160 | 0.534 | 13.226 | 0.000 |
| 1 Group 2 | 0.134 | 0.0937 | −0.050 | 0.317 | 2.035 | 0.154 | |
| 2 time 2 | −0.057 | 0.0917 | −0.237 | 0.122 | 0.392 | 0.531 | |
| 3 Group 3 × time 2 | 0.259 | 0.1188 | 0.026 | 0.492 | 4.763 | ||
| 4 Group 2 × time 2 | 0.040 | 0.1167 | −0.189 | 0.269 | 0.116 | ||
| Information analysis | 1 Group 3 | 0.352 | 0.0873 | 0.181 | 0.523 | 16.260 | 0.000 |
| 1 Group 2 | 0.264 | 0.0873 | 0.093 | 0.435 | 9.171 | 0.002 | |
| 2 time 2 | 0.151 | 0.0705 | 0.013 | 0.290 | 4.605 | 0.032 | |
| 3 Group 3 × time 2 | 0.048 | 0.0911 | −0.131 | 0.226 | 0.276 | 0.600 | |
| 4 Group 2 × time 2 | −0.136 | 0.0917 | −0.316 | 0.044 | 2.193 | 0.139 | |
| Execution | 1 Group 3 | 0.294 | 0.0907 | 0.116 | 0.471 | 10.480 | 0.001 |
| 1 Group 2 | 0.253 | 0.0855 | 0.085 | 0.421 | 8.739 | 0.003 | |
| 2 time 2 | 0.175 | 0.0707 | 0.037 | 0.314 | 6.142 | 0.013 | |
| 3 Group 3 × time 2 | −0.024 | 0.0957 | −0.211 | 0.164 | 0.061 | 0.805 | |
| 4 Group 2 × time 2 | −0.160 | 0.0924 | −0.341 | 0.021 | 3.002 | 0.083 | |
| Life-long learning | 1 Group 3 | 0.262 | 0.0943 | 0.077 | 0.446 | 7.697 | 0.006 |
| 1 Group 2 | 0.183 | 0.0863 | 0.014 | 0.352 | 4.506 | 0.034 | |
| 2 time 2 | 0.167 | 0.0724 | 0.025 | 0.309 | 5.339 | 0.021 | |
| 3 Group 3 × time 2 | 0.157 | 0.0971 | −0.033 | 0.347 | 2.609 | 0.106 | |
| 4 Group 2 × time 2 | −0.190 | 0.0969 | −0.379 | 0.000 | 3.824 | 0.051 | |
| Total scale | 1 Group 3 | 0.286 | 0.0766 | 0.136 | 0.436 | 13.902 | 0.000 |
| 1 Group 2 | 0.199 | 0.0719 | 0.058 | 0.340 | 7.683 | 0.006 | |
| 2 time 2 | 0.120 | 0.0580 | 0.006 | 0.234 | 4.291 | 0.038 | |
| 3 Group 3 × time 2 | 0.103 | 0.0774 | −0.049 | 0.254 | 1.758 | 0.185 | |
| 4 Group 2 × time 2 | −0.131 | 0.0755 | −0.278 | 0.017 | 2.993 | 0.084 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, Y.-C.A.; Lee, S.-H.; Hsu, M.-Y.; Shih, F.-F.; Yen, W.-J.; Huang, C.-Y.; Li, P.-C.; Hung, C.-Y.; Chuang, H.-L.; Kuo, C.-P. Effects of Problem-Based Learning Strategies on Undergraduate Nursing Students’ Self-Evaluation of Their Core Competencies: A Longitudinal Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 15825. https://doi.org/10.3390/ijerph192315825
Lu Y-CA, Lee S-H, Hsu M-Y, Shih F-F, Yen W-J, Huang C-Y, Li P-C, Hung C-Y, Chuang H-L, Kuo C-P. Effects of Problem-Based Learning Strategies on Undergraduate Nursing Students’ Self-Evaluation of Their Core Competencies: A Longitudinal Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(23):15825. https://doi.org/10.3390/ijerph192315825
Chicago/Turabian StyleLu, Yen-Chiao Angel, Shu-Hsin Lee, Ming-Yi Hsu, Fen-Fen Shih, Wen-Jiuan Yen, Cheng-Yi Huang, Pei-Ching Li, Ching-Yen Hung, Hsiao-Ling Chuang, and Ching-Pyng Kuo. 2022. "Effects of Problem-Based Learning Strategies on Undergraduate Nursing Students’ Self-Evaluation of Their Core Competencies: A Longitudinal Cohort Study" International Journal of Environmental Research and Public Health 19, no. 23: 15825. https://doi.org/10.3390/ijerph192315825
APA StyleLu, Y.-C. A., Lee, S.-H., Hsu, M.-Y., Shih, F.-F., Yen, W.-J., Huang, C.-Y., Li, P.-C., Hung, C.-Y., Chuang, H.-L., & Kuo, C.-P. (2022). Effects of Problem-Based Learning Strategies on Undergraduate Nursing Students’ Self-Evaluation of Their Core Competencies: A Longitudinal Cohort Study. International Journal of Environmental Research and Public Health, 19(23), 15825. https://doi.org/10.3390/ijerph192315825









