Psychosocial Support Programme Improves Adherence and Health Systems Experiences for Adolescents on Antiretroviral Therapy in Mpumalanga Province, South Africa
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
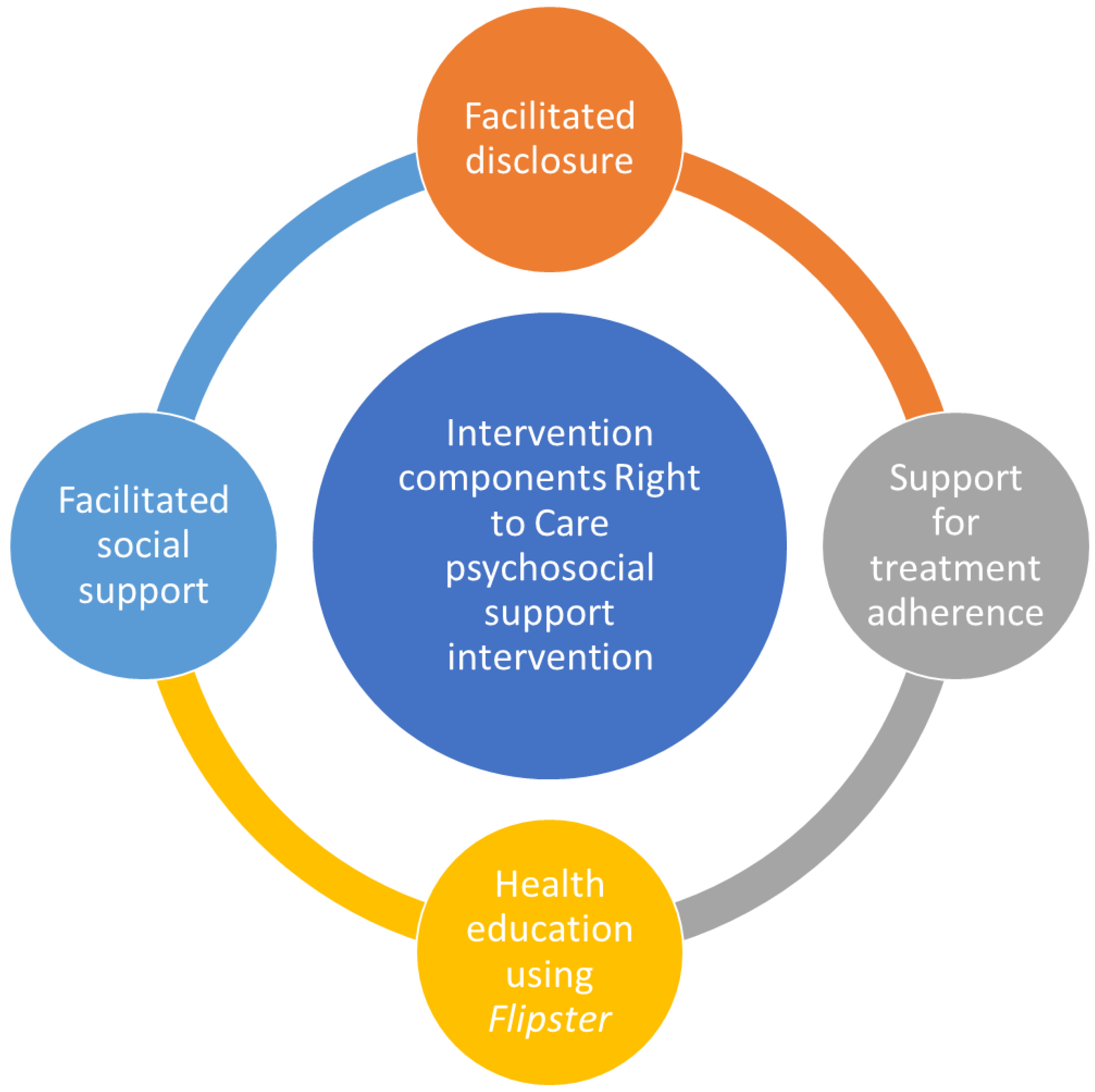
2.2. Overview of the Right to Care Psychosocial Support Intervention
2.3. Study Design, Sampling, and Data Collection
2.4. Data Analysis
2.5. Trustworthiness and Credibility
2.6. Ethics Approval and Informed Consent
3. Results
3.1. Pre-PSS Programme
3.2. Psychological Distress and Maladaptive Behaviours
3.2.1. Poor Mental Health
I cried [frequently cried] and did not want to go to school. 15-year-old, female Kanyamazane CHC
Additionally, others expressed feelings of hopelessness:
I felt like dying as I thought it’s over with my life: I was nine years [old] when I found out. 17-year-old female, Langloop CHC
3.2.2. Social Challenges
I no longer wanted to interact with anyone. 14-year-old female, Buffelspruit Clinic
Another stated:
I was angry at my parents, so I did not want to speak. 17-year-old female, Cunningmoore Clinic
3.2.3. Emotional Challenges
I became emotional and had low self-esteem after knowing my status. 14-year-old male, Naas CHC
I was furious and upset. 15-year-old female, Kanyamazane CHC
I was confused, not knowing what implications that [I] was supposed to have in my daily life. 13-year-old male, Cunningmoore Clinic
Back in the day, I was not getting much love [from family] before I even knew my status. It’s not nice for me, and it’s painful. 18-year-old male, Naas CHC
3.2.4. Substance Abuse
This [knowing my HIV-positive status] changed my life, and I started smoking and drinking (laughing). I even started smoking weed to make me high and come back late from friends going home. 16-year-old female, Langloop CHC
3.3. Health Literacy
Since it was flu medication, I would skip it since I didn’t know that I am [was] to drink [it] for a long time. 14-year-old male, Cunningmoore Clinic
3.4. Post-Intervention
3.5. Facilitated Disclosure of HIV Status
The white Doctor told me, and I was happy because I finally got an answer about what this medication was for, unlike not knowing. 14-year-old female, Langloop CHC
Another ALHIV reported:
…. because on the day they disclosed to me, other children were in the old clinic, and we were told that we were all the same. We all have the virus, and there is nothing to be afraid of. That made me feel happy because there were lots of us that day. 13-year-old female, Langloop CHC
My mother told me it does not start with me, and it does not end with me. I should also accept because it is not her fault, and as time went by, I started coming to the clinic and accepted since I am not the only one and I shall overcome it. 18-year-old female, Kanyamazane CHC
We feel like we have our whole life and future ahead of us irrespective of our status. 15-year-old male, Naas CHC
3.6. Health Education
- Importance of ARV Medication Adherence
I would get sick, and they [clinicians] found out that I was not taking my pills, and I was reprimanded for not taking my medications. I was told these pills would help me live … without the ART. I would get sick, lose weight, and end up dead. I continued taking them. I was also told always to eat my food so that by the time I take my pills, I have something in my stomach and should drink a lot of water. So, I took that and continued up until now. 13-year-old male, Naas CHC
- A Better Understanding of the Virus
It is important to take the medication, so you don’t have AIDS. The treatment makes the body strong and improves the immune system. 13-year-old female, Kanyamazane CHC
I think it’s fine so that the soldiers of the body can stay strong in our bodies. 18-year-old male, Kanyamazane CHC
- Improved Adherence
I was taking my treatment well, but when I got to grade 7, the problem began since I was not taking it well. At times I would take it, and other times I wouldn’t, so I would have a week without taking it, which happened for a month. When I went back to the clinic for my blood, that was when it was explained to my mother and me that I was not taking my treatment, so they explained more what happens when I do not take it, I will die, and from that day, I don’t miss taking my pills. 16- years-old male, Naas CHC
- Self-Management of ART
I am taking responsibility [for] my health, and I remind myself every time, and even my little sister does remind me, and if I don’t take [it], she would even report to my mom. So, I thank her a lot she is always there to remind me. 18-year-old female, Kanyamazane CHC
3.7. Counselling and Encouragement
They encourage and tell us every day that we should take care of ourselves and take treatment on time so that we can be healthy kids, and sometimes they take us out for fun walks so that we can relieve stress, and that is very helpful to us as kids. 14-year-old female, Cunningmoore Clinic
3.8. Strengthened Social Support Network
3.8.1. Peer Support
This support group has helped me a lot. It is no longer like before, and I know that I am not alone and there’s more of us, and I can talk to someone about a challenge I have and ask if they have the same challenge and if so, we can get to share the solutions and remind each other to take treatment. At least now I have someone with experience just like me, and I can share [discuss] everything I encounter, and I am happy. 18-year-old male, Kanyamazane CHC
I like the fact that we meet and discuss similar problems. We are open to each other and share similar problems, and it’s nice to know there are others who are going through the same problems. 13-year-old female, Naas CHC
I take my treatment regularly because I am attending with others that are taking treatment. 13-year-old male, Kanyamazane CHC
Now I feel proud of myself. I no longer look down on myself. The support I’m getting from this group and home has significantly helped. 13-year-old female, Cunningmoore Clinic
3.8.2. Enhanced Parent/Caregiver Support
Since both my parents are taking it [ARV drugs],-that made me continue taking it because I know that I am not alone. 14-year-old male, Buffelspruit Clinic
She [mother] always makes sure that I take my ART regularly; even if she is at work, she calls to check if I have taken my ART. 13-year-old male, Langloop CHC
Television also helps. I know that every time ‘Generations’ plays on TV, it automatically reminds me to take my ART. 13-year-old male, Langloop CHC
I used to cry a lot and always wanted to be alone and not talk to anyone. I had a difficult time with my anger, but the person who was very supportive in my life was my grandmother. She helped me with the burden and made me understand that this virus was not a death sentence. 13-year-old female, Buffelspruit Clinic
3.8.3. Client–Clinician Relationship
Yes, it does help me because I can ask the nurse a lot of things, and with my peers as well, I can share whatever is bothering me, and if I forget to take my pills, I ask them what they do if they forget or if they don’t. So, it [is] beneficial. 18-year-old female, Buffelspruit Clinic
She [professional nurse] is very open and easy to talk to, and she is not the type of person who gets angry or even shout[s] at us. She behaves like us so that she can understand us better. 11-year-old female, Cunningmoore Clinic
On the experiences of quick access to health services, ALHIV stated that:
It’s great to meet in groups, we get assisted very fast and arrive home early because you don’t queue. 12-year-old male, Langloop CHC
So far, it is working for me because I don’t take time to queue when I am here, and here, I sit for an hour or 30 min. 15-year-old female, Kanyamazane CHC
3.9. Recommendations to Improve PSS
Before, if I am supposed to come on Sunday, they can call me in the morning and remind me. 13-year-old male, Langloop CHC
We will appreciate [it] if we [ALHIV] can have counsellors to motivate us maybe once or twice a year so that we can continue to take our ART with confidence because that encourages and give[s] us hope. 15-year-old female, Buffelspruit Clinic
If we can get a motivational speaker to motivate us about taking our ART, even if it can be twice a year. 14-year-old female, Naas CHC
Maybe help us [ALHIV] with transport to the facility because we are far. 14-year-old, female Langloop CHC
Our concern is that when we collect our medication, we have files, while those not on treatment don’t have files. So, we suggest a plan be made for us not to be publicised by files. 17-year-old female, Cunningmoore Clinic
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Category | Theme | Sub Theme | Codes | Quotations | ||
|---|---|---|---|---|---|---|
| Pre-intervention | ||||||
| Poor psychological well-being | Poor mental health | Depressive symptoms | I cried and did not want to go to school. 15-year-old female, Naas CHC | |||
| Feelings of hopelessness | I felt like dying as I thought it’s over with my life: I was 9 years when I found out. 17-year-old female, Naas CHC | |||||
| Social challenges | Reclusive | Yes, my parents tried to reach out to me. 14-year-old female, Buffelspruit Clinic | ||||
| I no longer wanted to interact with anyone. 14-year-old female, Buffelspruit Clinic | ||||||
| I shut everyone out. 17-year-old female, Cunningmoore Clinic | ||||||
| Blaming parents | I was angry at my parents, so I did not want to speak. 17-year-old female, Naas CHC | |||||
| Emotional challenges | Low self-esteem | I became emotional and had low self-esteem. 14-year-old male, Naas CHC | ||||
| Feeling confused | I was confused not knowing what implications that was supposed to have in my day life. 13-year-old male, Cunningmoore Clinic | |||||
| Feeling of anger | I was furious and upset. 15-year-old female, Naas CHC | |||||
| Perceived feeling of lack of affection | Purple, M18: Not even back in the days I was not getting much love before I even knew my status. It’s not nice for me and its painful. 18-year-old male | |||||
| Behavioural challenges | Substance use | I started smoking. 14-year-old female, Naas CHC | ||||
| This changed my life and I started smoking and drinking (laughing) I even started smoking weed so that it would make me high and come back late from friends going home. 16-year-old female, Langloop CHC | ||||||
| Poor treatment literacy | Adherence challenges | No awareness of HIV status | Since it was flu medication, I would skip it since I didn’t know that I am to drink for a long time. 15-year-old male, Langloop CHC | |||
| Post intervention | Theme | Sub Theme | Codes | Quotations | ||
| Facilitated disclosure of HIV status | Improved psychological well-being | Feeling “happy” | The white Doctor told me, and I was happy because I finally got an answer of what this medication is for unlike not knowing. 14-year-old female, Langloop CHC | |||
| because on the day they disclosed to me there were other children in the old clinic, and we were told that we are all the same. Meaning we all have the virus and there is nothing to be afraid of, that made me feel happy because there were lots of us that day. 13-year-old female, Langloop CHC | ||||||
| I am happy because I know my status, unlike not knowing that I am HIV positive. I feel free now because I know my status. 18-year-old female, Naas CHC | ||||||
| Acceptance of HIV status | My mother told me it does not start with me, and it does not end with me. I should also accept because it is not her fault and as time went by, I started coming to the clinic and I accepted since I am not the only one and I shall overcome it. 18-year-old female, Naas CHC | |||||
| As time went by, I accepted because even my dad takes treatment, my uncle as well as my cousin. 19-year-old female, Naas CHC | ||||||
| Hope for the future | we feel like we have our full life and future ahead of us irrespective of our status. 15-year-old male, Naas CHC | |||||
| Health education | Improvement in treatment literacy | Importance of ARVs | I would get sick, and they found out that I was not taking my pills and they reprimanded me for not taking my pills. I was told these pills will help me live and I continued taking them. They also said I should always eat my food so by the time I take my pills I have something in my stomach and that I should drink a lot of water. So, I took that and continued up until now. 13-year-old male | |||
| It is good because it saves our life. 15 year-old male | ||||||
| ….. without your ART you will get sick and lose weight and you will end up dead. 13-year-old female, Langloop CHC | ||||||
| Better understanding of the virus | HIV knowledge and implications | I think its fine so that the soldiers of the body can stay strong in our bodies. 18-year-old male, Kanyamazane | ||||
| It is important to take the medication so that you don’t have AIDS. The treatment makes the body strong and improves the immune system. 13-year-old female | ||||||
| Improved adherence | Fear of dying motivated continuous uptake | To be honest I was taking my treatment well but when I got to grade 7 that is when the problem began since I was not taking it well. At times I would take it and other times I wouldn’t, so I would have a week without taking it and that happened for a month. When I went back to the clinic for my bloods that was when it was explained to me and my mother that I was not taking my treatment, so they explained more what happens when I do not take it, I will die and from that day, I don’t miss taking my pills. 13-year-old female | ||||
| Counselling and encouragement | They encourage and tell us every day that we should take care of ourselves, take treatment on time so that we can be healthy kids and sometimes they take us out for fun walks so that we can relieve stress and that is very helpful to us as kids. 13-year-old female | |||||
| because ART would help us on the virus that we have and that will encourage children to take their medication daily. 14-year-old female, Langloop CHC | ||||||
| Fear of consequences for not taking ARVs | I have accepted and there is someone who was admitted at Rob Fererra hospital two times and the 1st time he was there for 2 months and the 2nd time he was there for 6 months because of not taking treatment. I don’t want to end up like that so I am taking my medication. 18-year-old male | |||||
| Self-management of ART | Taking responsibility | No one reminds me about taking ART, I just take them by myself. 14-year-old female | ||||
| I am taking responsibility of my health and I remind myself every time and even my little sister does remind me and if I don’t take, she would even report to my mom. So, I thank her a lot she is always there to remind me. 18-year-old female | ||||||
| Self-reminders using TV programmes | Television also helps, like I know every time generations plays on tv it automatically reminds me to take my ART. 13-year-old male, Langloop CHC | |||||
| Understood the seriousness of HIV | Seriousness | It made me realise the seriousness of my status. 15-year-old female | ||||
| Strengthened social support network | Peer support | Feeling of not being alone | The support group was good because I felt I was not alone. 17-year-old female | |||
| It is no longer like before and I know that I am not alone and there’s more of us and I can talk to someone about a challenge I have and ask if they have the same challenge and if so we can get to share the solutions and remind each other to take treatment. At least now I do have someone who has experience just like me and I can share with everything I encounter, and I am happy. This support group has really helped me a lot. 18-year-old male | ||||||
| Sometimes I would feel like that, but I eventually saw one of the kids from school coming to the clinic and attending this group. That is when I saw that I am not alone. 19-year-old female | ||||||
| Know others taking ARVs | I take my treatment regularly because I am attending with others that are taking treatment. 13-year-old male, Kanyamazane | |||||
| Self-esteem | Yes, we need that peer- to-peer support so they can see that they are not the only ones and it’ll be easier for them to talk to us since we’re the same age. We will have confidence and our self-esteem will improve after they assist us. 18-year-old male | |||||
| Now I feel proud of myself. I know longer look down on myself. The support I’m getting from this group and home has helped a lot. 13-year-old female, Buffelspruit Clinic | ||||||
| Because it’s not easy to forget the time they tell you to take your ART. We use the same time to take medication so it’s not easy to forget. 13-year-old female, Langloop CHC | ||||||
| Share experiences | This group is really helping us as we get share similar experiences about life. 18-year-old male | |||||
| Share ideas on how to overcome challenges | We would talk about our medication, like what time others take their ART and other issues relating to our pills. 12-year-old male, Langloop CHC | |||||
| I think we should continue with the group because it helps, and we learn from each other, and it becomes easy for us to meet and collect our ART. 13-year-old female, Langloop CHC | ||||||
| I like the fact that we meet and discuss about similar problems. We are open to each other, and we share similar problems and its nice to know there are others who are going through the same problems as yourself. 13-year-old female, Naas CHC | ||||||
| Friendship | I love that we communicate and are open with each other. People do not go around gossiping and talking about our status with other people who are not part of this group. 13-year-old male, Naas CHC | |||||
| Yes, this group is helping me. I am HIV positive, and I get to sit and listen to other HIV positive peers. 18-year-old male | ||||||
| I also like this group because I get friends who are also on ART and meet in one place where we help each other. 13-year-old female, Langloop CHC | ||||||
| Encouraging each other to adherence | We help one another by encouraging each other to take medication every day. 13-year-old female, Langloop CHC | |||||
| Coping | Not suffering alone, have comfort and opening to your groups. 14-year-old female, Buffelspruit Clinic | |||||
| Parents/caregiver support | Role model | Since both my parents are taking it, that made me to continue taking it because I know that I am not alone | ||||
| Family reminds of adherence | She always makes sure that I take my ART regularly, even if she is at work she calls just to check if I have taken my ART. 13-year-old male, Langloop CHC | |||||
| My mother reminds me to take ART everyday especially when I forget. 13-year-old female, Langloop CHC | ||||||
| Emotional support | I used to cry a lot and always wanted to be alone and not talk to anyone. I had a difficult time with my anger, but the person who was very supportive in my life was my grandmother. She helped me with the burden and made me understand that this virus was not a death sentence. 13-year-old female, Buffelspruit Clinic | |||||
| I get support from my mom and grandmother, and the rest of the family they don’t know, and even my brothers do not know. 16-year-old female, Cunningmoore Clinic | ||||||
| Client–clinician relationship | Bonding with clinician | Yes, it does help me because I can ask the nurse a lot of things, and with my peers as well, I can share whatever is bothering me and if I forget to take my pills, I ask them what do they do if they forget or if they don’t. So, it very helpful. 18-year-old female, Naas CHC | ||||
| Friendly healthcare worker | She (Professional nurse) is very open and easy to talk to and she is not the type of person who gets angry or even shout at us. She behaves like us so that she can understand us better. 18-year-old female, Naas CHC | |||||
| Improved Health service delivery | Quick access to treatment | It’s great to meet in the groups, we get assisted very fast and you arrive home very early because you don’t que. 12-year-old male, Langloop CHC | ||||
| So far it is working for me because I don’t take time to que when I am here and here, I just sit for an hour or 30min. 15-year-old female, Kanyamazane CHC | ||||||
| Recommendations to improve PSS | ||||||
| Reminders to collect medication | Before, let’s take if I am supposed to come on Sunday, they can call me in the morning and remind me. 13-year-old male, Langloop CHC | |||||
| Psychological motivation | We will appreciate if we can have counsellors to motivate us maybe once or twice a year so that we can continue to take our ART with confidence because that encourages and give us hope. 15-year-old female, Buffelspruit Clinic | |||||
| If we can get a motivational speaker to motivate us about taking our ART, even if it can be twice a year. 14-year-old female, Naas CHC | ||||||
| Help with transport to clinic | Maybe help us with transport to reach the facility because we stay far. 14-year-old female, Langloop CHC | |||||
| Clinical files of clients treated with confidentiality | Our concern is that when we go to collect our medication, we have files while those who are not on treatment don’t have files so we suggest that a plan be made for us not to be published by files. 17-year-old female, Cunningmoore Clinic | |||||
References
- Naidoo, K.; Munsami, A.; Archary, M. Adolescent antiretroviral management: Understanding the complexity of non-adherence. South Afr. Med. J. 2015, 105, 953. [Google Scholar] [CrossRef] [PubMed]
- Gittings, L.; Toska, C.; Hodes, R.; Cluver, L.; Zungu, N.; Govender, K.; Chademana, K.E.; Gutiérrez, V. Resourcing resilience: The case for social protection for HIV-positive children on antiretroviral treatment in Eastern and Southern Africa. Afr. J. AIDS Res. 2016, 15, 123–140. [Google Scholar]
- WHO. World Health Statistics; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- UNICEF. Turning the Tide against AIDS Will Require More Concentrated Focus on Adolescents and Young People; UNICEF: New York, NY, USA, 2017; pp. 1–9. Available online: https://data.unicef.org/topic/hivaids/adolescents-young-people/ (accessed on 19 March 2021).
- Estripeaut, D.; Luciani, K.; García, R.; Banús, R.; Aguais, T.M.; Berrío, E.; Jenkins, A.; Smoot, S. Analysis of the social and psychosocial factors associated with adherence to antiretroviral therapy in adolescents with perinatal HIV-1 infection in Panama from a gender perspective. AIDS Care 2016, 28 (Suppl. S2), 66–72. Available online: https://search.proquest.com/docview/1803800134?accountid=14782%5Cnhttp://tewaharoa.victoria.ac.nz/openurl/64VUW/VUW_SERVICES_PAGE?ctx_ver=Z39.88-2004&ctx_enc=info:ofi/enc:UTF-8&rfr_id=ProQ%3Amedline&rft_val_fmt=&rft.genre=article&rft.jtitle=AIDS+care&rft (accessed on 4 July 2022). [CrossRef]
- Bernays, S.; Jarrett, P.; Kranzer, K.; Ferrand, R.A. Children growing up with HIV infection: The responsibility of success. Lancet 2014, 383, 1355–1357. [Google Scholar] [CrossRef]
- Pretorius, L.; Gibbs, A.; Crankshaw, T. Interventions targeting sexual and reproductive health and rights outcomes of young people living with HIV: A comprehensive review of current interventions from sub-Saharan Africa. Glob. Health Action 2015, 8, 28454. [Google Scholar] [CrossRef] [PubMed]
- Mupambireyi, Z.; Willis, N.; Pascoe, M.; Gwavava, E.; Khan, R.; Sammon, E.; Cowan, F. Exploring the clinical and psychosocial challenges faced by HIV perinatally infected young women in Harare, Zimbabwe around the time of their first pregnancy. In Proceedings of the 20th International AIDS Conference, Melbourne, Australia, 20–25 July 2014; p. 1827. [Google Scholar]
- Hashmi, S. Adolescence: An Age of Storm and Stress. Rev. Arts Humanit. 2013, 2, 19–33. [Google Scholar]
- Idele, P.; Gillespie, A.; Porth, T.; Suzuki, C.; Mahy, M.; Kasedde, S.; Luo, C. Epidemiology of HIV and AIDS Among Adolescents. JAIDS J. Acquir. Immune Defic. Syndr. 2014, 66, S144–S153. Available online: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00126334-201407011-00002 (accessed on 10 August 2022). [CrossRef]
- Haberer, J.; Mellins, C. Pediatric adherence to HIV antiretroviral therapy. Curr. HIV/AIDS Rep. 2009, 6, 194–200. [Google Scholar] [CrossRef]
- UNICEF. Adolescents Living with HIV: Developing and Strengthening Care and Support Services; UNICEF: New York, NY, USA, 2016. [Google Scholar]
- Skeen, S.A.; Sherr, L.; Croome, N.; Gandhi, N.; Roberts, K.J.; Macedo, A.; Tomlinson, M. Interventions to improve psychosocial well-being for children affected by HIV and AIDS: A systematic review. Vulnerable Child. Youth Stud. 2017, 12, 91–116. Available online: https://www.tandfonline.com/doi/full/10.1080/17450128.2016.1276656 (accessed on 15 June 2022). [CrossRef][Green Version]
- Vreeman, R.C.; McCoy, B.M.; Lee, S. Mental health challenges among adolescents living with HIV. J. Int. AIDS Soc. 2017, 20, 100–109. Available online: http://www.jiasociety.org/index.php/jias/article/view/21497 (accessed on 14 August 2022). [CrossRef]
- Sherr, L. Mental health—A bridge not so far. Lancet Glob. Health 2017, 5, e559–e560. Available online: http://linkinghub.elsevier.com/retrieve/pii/S2214109X17301833 (accessed on 8 August 2022). [CrossRef]
- Okonji, E.F.; van Wyk, B.; Mukumbang, F.C.; Hughes, G.D. Determinants of viral suppression among adolescents on antiretroviral treatment in Ehlanzeni district, South Africa: A cross-sectional analysis. AIDS Res. Ther. 2021, 18, 66. [Google Scholar] [CrossRef] [PubMed]
- Okonji, E.F.; van Wyk, B.; Mukumbang, F.C. Two-year retention in care for adolescents on antiretroviral therapy in Ehlanzeni District, South Africa: A baseline cohort analysis Two-year retention in care for adolescents on antiretroviral therapy in Ehlanzeni district, South Africa: A baseline c. AIDS Care 2022, 31, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Okonji, E.F.; van Wyk, B.; Mukumbang, F.C. Applying the biopsychosocial model to unpack a psychosocial support intervention designed to improve antiretroviral treatment outcomes for adolescents in South Africa. Pan Afr. Med. J. 2022, 41, 166. [Google Scholar] [CrossRef] [PubMed]
- Kyngäs, H. Inductive Content Analysis. In The Application of Content Analysis in Nursing Science Research; Springer International Publishing: Cham, Switzerland, 2020; pp. 13–21. Available online: http://link.springer.com/10.1007/978-3-030-30199-6_2 (accessed on 8 August 2022).
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. Available online: https://academic.oup.com/intqhc/article-lookup/doi/10.1093/intqhc/mzm042 (accessed on 8 August 2022). [CrossRef]
- Tong, A.; Flemming, K.; McInnes, E.; Oliver, S.; Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med. Res. Methodol. 2012, 12, 181. Available online: http://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-12-181 (accessed on 8 August 2022). [CrossRef]
- Sørensen, K.; van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H.; (HLS-EU) Consortium Health Literacy Project European. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. Available online: http://www.biomedcentral.com/1471-2458/12/80 (accessed on 8 August 2022). [CrossRef]
- Mutumba, M.; Mugerwa, H.; Musiime, V.; Gautam, A.; Nakyambadde, H.; Matama, C.; Stephenson, R. Perceptions of Strategies and Intervention Approaches for HIV Self-Management among Ugandan Adolescents: A Qualitative Study. J. Int. Assoc. Provid. AIDS Care 2019, 18, 2325958218823246. [Google Scholar] [CrossRef]
- Haberer, J.E.; Cook, A.; Walker, A.S.; Ngambi, M.; Ferrier, A.; Mulenga, V.; Kityo, C.; Thomason, M.; Kabamba, D.; Chintu, C.; et al. Excellent adherence to antiretrovirals in HIV+ Zambian children is compromised by disrupted routine, HIV Nondisclosure, and Paradoxical Income Effects. PLoS ONE 2011, 6, e18505. [Google Scholar] [CrossRef]
- Cluver, L.D.; Hodes, R.J.; Toska, E.; Kidia, K.K.; Orkin, F.M.; Sherrf, L.; Meinck, F. ‘HIV is like a tsotsi. ARVs are your guns’: Associations between HIV-disclosure and adherence to antiretroviral treatment among adolescents in South Africa. AIDS 2015, 29, S57–S65. [Google Scholar] [CrossRef]
- Polisset, J.; Ametonou, F.; Arrive, E.; Aho, A.; Perez, F. Correlates of adherence to antiretroviral therapy in HIV-infected children in Lomé, Togo, West Africa. AIDS Behav. 2009, 13. [Google Scholar] [CrossRef] [PubMed]
- Ugwu, R.; Eneh, A. Factors influencing adherence to paediatric antiretroviral therapy in Portharcourt, South-South Nigeria. Pan Afr. Med. J. 2013, 16. [Google Scholar] [CrossRef] [PubMed]
- Arage, G.; Tessema, G.A.; Kassa, H. Adherence to antiretroviral therapy and its associated factors among children at South Wollo Zone Hospitals, Northeast Ethiopia: A cross-sectional study. BMC Public Health 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Müller, A.D.; Bode, S.; Myer, L.; Stahl, J.; von Steinbüchel, N. Predictors of adherence to antiretroviral treatment and therapeutic success among children in South Africa. AIDS Care 2011, 23, 129–138. [Google Scholar] [CrossRef]
- Nabukeera-Barungi, N.; Elyanu, P.; Asire, B.; Katureebe, C.; Lukabwe, I.; Namusoke, E.; Musinguzi, J.; Atuyambe, L.; Tumwesigye, N. Adherence to antiretroviral therapy and retention in care for adolescents living with HIV from 10 districts in Uganda. BMC Infect. Dis. 2015, 15. [Google Scholar] [CrossRef]
- Bhattacharya, M.; Dubey, A.P.; Sharma, M. Patterns of diagnosis disclosure and its correlates in HIV-infected north Indian children. J. Trop. Pediatr. 2011, 57, 405–411. [Google Scholar] [CrossRef]
- Turissini, M.L.; Nyandiko, W.M.; Ayaya, S.O.; Marete, I.; Mwangi, A.; Chemboi, V.; Warui, L.; Vreeman, R.C. The prevalence of disclosure of HIV status to HIV-infected children in Western Kenya. J. Pediatr. Infect. Dis. Soc. 2013, 2, 136–143. [Google Scholar] [CrossRef]
- Sirikum, C.; Sophonphan, J.; Chuanjaroen, T.; Lakonphon, S.; Srimuan, A.; Chusut, P.; Do, T.C.; Prasitsuebsai, W.; Puthanakit, T.; Ananworanich, J. HIV disclosure and its effect on treatment outcomes in perinatal HIV-infected Thai children. AIDS Care 2014, 26, 1144–1149. [Google Scholar] [CrossRef]
- Vreeman, R.C.; Scanlon, M.L.; Mwangi, A.; Turissini, M.; Ayaya, S.O.; Tenge, C.; Nyandiko, W.M. A cross-sectional study of disclosure of HIV status to children and adolescents in Western Kenya. PLoS ONE 2014, 9. [Google Scholar] [CrossRef]
- Dachew, B.A.; Tesfahunegn, T.B.; Birhanu, A.M. Adherence to highly active antiretroviral therapy and associated factors among children at the University of Gondar Hospital and Gondar Poly Clinic, Northwest Ethiopia: A cross-sectional institutional based study. BMC Public Health 2014, 14, 875. [Google Scholar] [CrossRef][Green Version]
- Biressaw, S.; Abegaz, W.E.; Abebe, M.; Taye, W.A.; Belay, M. Adherence to Antiretroviral Therapy and associated factors among HIV infected children in Ethiopia: Unannounced home-based pill count versus caregivers’ report. BMC Pediatr. 2013, 13, 132. [Google Scholar] [CrossRef] [PubMed]
- Biadgilign, S.; Deribew, A.; Amberbir, A.; Deribe, K. Adherence to highly active antiretroviral therapy and its correlates among HIV infected pediatric patients in Ethiopia. BMC Pediatr. 2008, 8, 53. [Google Scholar] [CrossRef] [PubMed]
- Okawa, S.; Mwanza Kabaghe, S.; Mwiya, M.; Kikuchi, K.; Jimba, M.; Kankasa, C.; Ishikawa, N. Psychological well-being and adherence to antiretroviral therapy among adolescents living with HIV in Zambia. AIDS Care 2018, 30, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Damulira, C.; Mukasa, M.N.; Byansi, W.; Nabunya, P.; Kivumbi, A.; Namatovu, P.; Namuwonge, F.; Dvalishvili, D.; Bahar, O.S.; Ssewamala, F.M. Examining the relationship of social support and family cohesion on ART adherence among HIV-positive adolescents in southern Uganda: Baseline findings. Vulnerable Child. Youth Stud. 2019, 14, 181–190. [Google Scholar] [CrossRef]
- Lam, P.K.; Naar-King, S.; Wright, K. Social support and disclosure as predictors of mental health in HIV-positive youth. AIDS Patient Care STDs 2007, 21, 20–29. [Google Scholar] [CrossRef]
- Zanoni, B.C.; Archary, M.; Subramony, T.; Sibaya, T.; Psaros, C.; Haberer, J.E. Disclosure, Social Support, and Mental Health are Modifiable Factors Affecting Engagement in Care of Perinatally-HIV Infected Adolescents: A Qualitative Dyadic Analysis. AIDS Behav. 2021, 25, 237–248. [Google Scholar] [CrossRef]
| Females | Males | |||
|---|---|---|---|---|
| Facility Name | 10 to 14 Years | 15 to 19 Years | 10 to 14 Years | 15 to 19 Years |
| Buffelspruit Clinic | 9 | - | - | - |
| Kanyamazane CHC | 9 | 12 | 9 | 12 |
| Cunningmoore Clinic | - | 3 | - | 3 |
| Langloop CHC | 4 | 4 | 4 | 4 |
| Mashinshing CHC | - | - | - | - |
| Naas CHC | 20 | 30 | 20 | 30 |
| Masibeka Clinic | - | - | - | - |
| Total | 42 | 49 | 33 | 49 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okonji, E.F.; Wyk, B.v.; Hughes, G.D.; Mukumbang, F.C. Psychosocial Support Programme Improves Adherence and Health Systems Experiences for Adolescents on Antiretroviral Therapy in Mpumalanga Province, South Africa. Int. J. Environ. Res. Public Health 2022, 19, 15468. https://doi.org/10.3390/ijerph192315468
Okonji EF, Wyk Bv, Hughes GD, Mukumbang FC. Psychosocial Support Programme Improves Adherence and Health Systems Experiences for Adolescents on Antiretroviral Therapy in Mpumalanga Province, South Africa. International Journal of Environmental Research and Public Health. 2022; 19(23):15468. https://doi.org/10.3390/ijerph192315468
Chicago/Turabian StyleOkonji, Emeka Francis, Brian van Wyk, Gail D. Hughes, and Ferdinand C. Mukumbang. 2022. "Psychosocial Support Programme Improves Adherence and Health Systems Experiences for Adolescents on Antiretroviral Therapy in Mpumalanga Province, South Africa" International Journal of Environmental Research and Public Health 19, no. 23: 15468. https://doi.org/10.3390/ijerph192315468
APA StyleOkonji, E. F., Wyk, B. v., Hughes, G. D., & Mukumbang, F. C. (2022). Psychosocial Support Programme Improves Adherence and Health Systems Experiences for Adolescents on Antiretroviral Therapy in Mpumalanga Province, South Africa. International Journal of Environmental Research and Public Health, 19(23), 15468. https://doi.org/10.3390/ijerph192315468








