Rescue Emergencies Due to High-Altitude Illnesses Are Rare in Switzerland
Abstract
:1. Introduction
2. Material and Methods
2.1. Analyzed Population
2.2. Data Preparation
2.3. Statistical Analyses
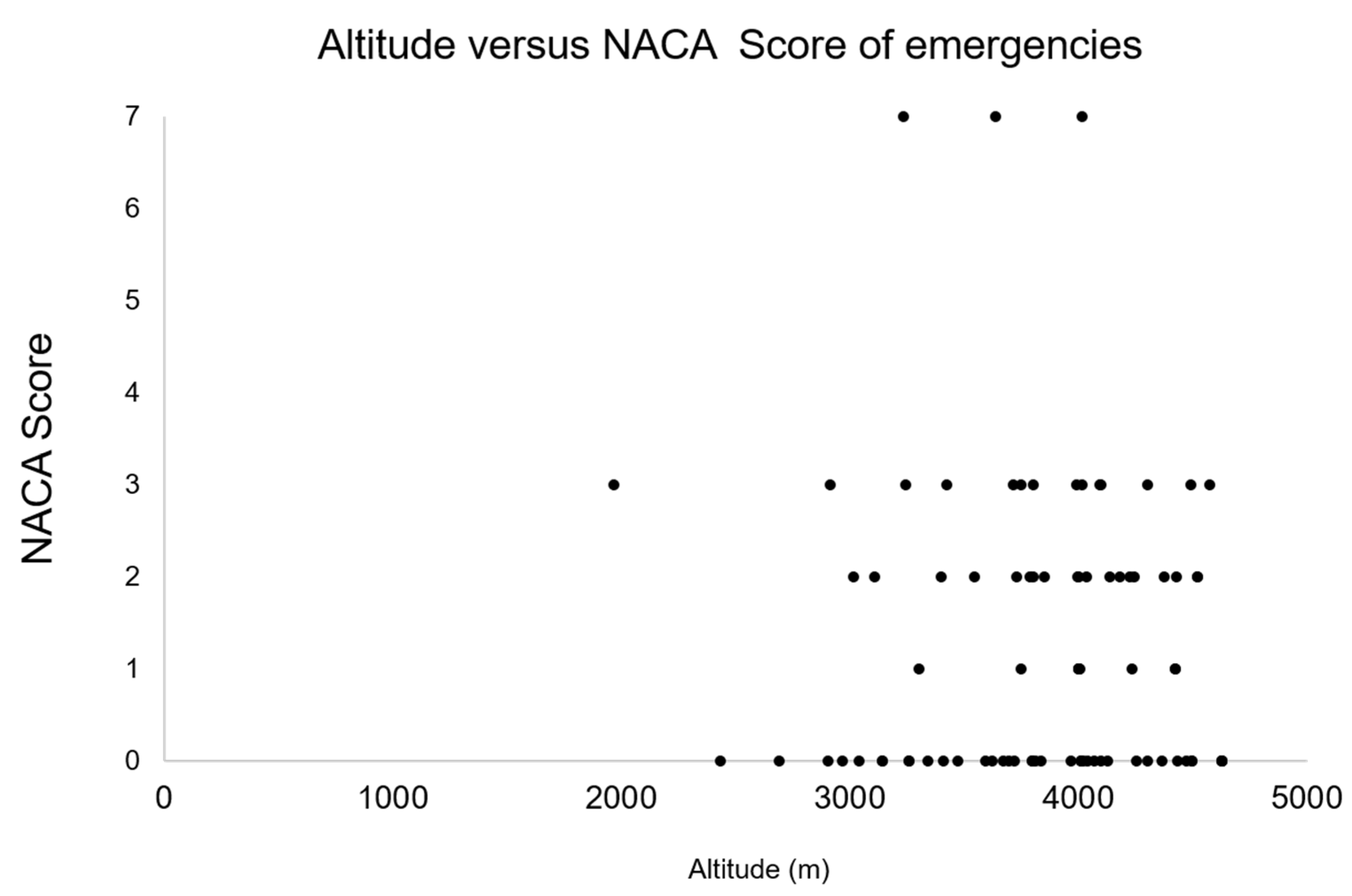
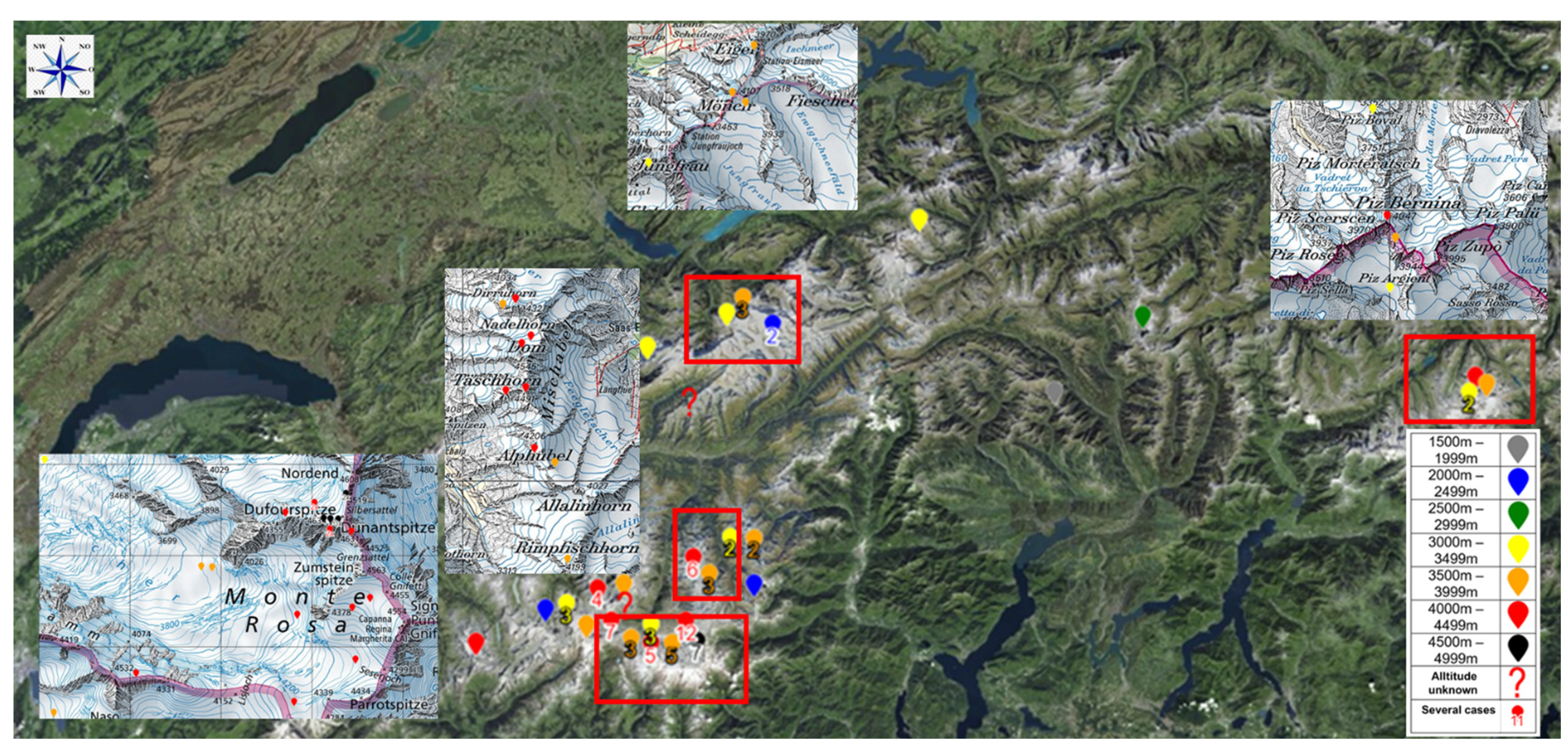
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lüthi, B. Übernachtungsstatistik SAC-Hütten 2019—Sommer der Rekorde. Available online: https://www.sac-cas.ch/de/der-sac/uebernachtungsstatistik-sac-huetten-2019-22231 (accessed on 21 June 2021).
- Mosimann, U. Haftung am Berg. Available online: https://have.ch/fileadmin/_migrated/content_uploads/01_Mosimann_Sicherheit_beim_Bergsport_Version_HAVE.pdf (accessed on 31 January 2020).
- Maggiorini, M.; Buhler, B.; Walter, M.; Oelz, O. Prevalence of acute mountain sickness in the Swiss Alps. Br. Med. J. 1990, 301, 853–855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, J. Acute Mountain Sickness. JAMA 2017, 318, 1840. [Google Scholar] [CrossRef] [PubMed]
- Imray, C.; Wright, A.; Subudhi, A.; Roach, R. Acute Mountain Sickness: Pathophysiology, Prevention, and Treatment. Prog. Cardiovasc. Dis. 2010, 52, 467–484. [Google Scholar] [CrossRef] [PubMed]
- Roach, R.; Hackett, P.H.; Oelz, O.; Bärtsch, P.; Luks, A.M.; MacInnis, M.; Baillie, J.K.; Achatz, E.; Albert, E.; Andrews, J.; et al. The 2018 Lake Louise Acute Mountain Sickness Score. High Alt. Med. Biol. 2018, 19, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Hackett, P.H.; Rennie, D. Rales, peripheral edema, retinal hemorrhage and acute mountain sickness. Am. J. Med. 1979, 67, 214–218. [Google Scholar] [CrossRef]
- Hackett, P.H. The incidence, importance, and prophylaxis of acute mountain sickness. Lancet 1976, 308, 1149–1155. [Google Scholar] [CrossRef]
- Singh, I.; Khanna, P.K.; Srivastava, M.C.; Lal, M.; Roy, S.B.; Subramanyam, C.S.V. Acute Mountain Sickness. N. Engl. J. Med. 1969, 280, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Houston, C.S. Incidence of acute mountain sickness. Am. Alp. J. 1985, 27, 162–165. [Google Scholar]
- Larson, E.B.; Roach, R.C.; Schoene, R.B.; Horbein, T.F. Acute mountain sickness and acetazolamide. Clinical efficacy and effect on ventilation. JAMA 1982, 248, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, A.B.; Mills, J.; Luce, J.M. Incidence of acute mountain sickness at intermediate altitude. JAMA 1980, 261, 732–734. [Google Scholar] [CrossRef]
- Mairer, K.; Wille, M.; Bücher, T.; Burtscher, M. Prevalence of Acute Mountain Sickness in the Eastern Alps. High Alt. Med. Biol. 2009, 10, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Bärtsch, P.; Mairbäurl, H.; Maggiorini, M.; Swenson, E.R. Physiological aspects of high-altitude pulmonary edema. J. Appl. Physiol. 2005, 98, 1101–1110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lundby, C. Going to altitude? Bring your vitamins! J. Physiol. 2010, 588, 4603–4604. [Google Scholar] [CrossRef] [PubMed]
- Allemann, Y.; Sartori, C.; Lepori, M.; Pierre, S.; Mélot, C.; Naeije, R.; Scherrer, U.; Maggiorini, M. Echocardiographic and invasive measurements of pulmonary artery pressure correlate closely at high altitude. Am. J. Physiol. Circ. Physiol. 2000, 279, H2013–H2016. [Google Scholar] [CrossRef] [PubMed]
- Sartori, C.; Allemann, Y.; Duplain, H.; Lepori, M.; Egli, M.; Lipp, E.; Hutter, D.; Turini, P.; Hugli, O.; Cook, S.; et al. Salmeterol for the Prevention of High-Altitude Pulmonary Edema. N. Engl. J. Med. 2002, 346, 1631–1636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sartori, C.; Vollenweider, L.; Löffler, B.-M.; Delabays, A.; Nicod, P.; Bärtsch, P.; Scherrer, U. Exaggerated Endothelin Release in High-Altitude Pulmonary Edema. Circulation 1999, 99, 2665–2668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scherrer, U.; Vollenweider, L.; Delabays, A.; Savcic, M.; Eichenberger, U.; Kleger, G.R.; Fikrle, A.; Ballmer, P.E.; Nicod, P.; Bärtsch, P. Inhaled nitric oxide for high-altitude pulmonary edema. N. Engl. J. Med. 1996, 334, 624–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winkler, K.; Brehm, H.P.; Haltmeier, J. Bergsport Winter; SAC-Verlag: Bern, Switzerland, 2008. [Google Scholar]
- Winkler, K.; Brehm, H.P.; Haltmeier, J. Bergsport Sommer; SAC-Verlag: Bern, Switzerland, 2008. [Google Scholar]
- Schlechtriemen, T.; Burghofer, K.; Lackner, C.K.; Altemeyer, K.H. Validierung des NACA-Score anhand objektivierbarer Parameter. Untersuchung an 104.962 Primäreinsätzen der Jahre 1999–2003 aus der Luftrettung. Notf. Rett. 2005, 8, 96–108. [Google Scholar]
- Weiss, M.; Bernoulli, L.; Zollinger, A. Der NACA-Index. Der Anaesthesist 2001, 50, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Schendera, C.F.G. Datenmanagement und Datenanalyse mit dem SAS-System; Oldenburg: München, Germany, 2004. [Google Scholar]
- Schendera, C.F.G. Datenqualität mit SPSS; Oldenburg: München, Germany, 2007. [Google Scholar]
- Stier, W. Empirische Forschungsmethoden; Springer: Berlin, Germany, 1996. [Google Scholar]
- Bera, A.K.; Jarque, C.M. Efficent tests for normality, homoscedasticity and serial independence of regression residuals. Econ. Lett. 1980, 6, 255–259. [Google Scholar] [CrossRef]
- Bärtsch, P.; Milledge, J. Blood and haemostasis. In High Altitude: Human Adaptation to Hypoxia; Swenson, E.R., Bärtsch, P., Eds.; Springer: New York, NY, USA, 2014; pp. 203–216. [Google Scholar]
- Swenson, E.R.; Bärtsch, P. High Altitude: Human Adaption to Hypoxia; Springer: New York, NY, USA, 2014. [Google Scholar]
- Schweizer Alpen-Club. Bergnotfallstatistik 2020. Schweizer Alpen-Club SAC. Available online: https://www.sac-cas.ch/de/ausbildung-und-sicherheit/bergnotfaelle-2020-trotz-corona-lockdown-mehr-notfaelle-32341 (accessed on 1 June 2021).
- Swissmedic. Seltene Erkrankungen. Available online: www.swissmedic.ch (accessed on 10 March 2021).
| NACA 0 | No injury or disease. |
| NACA I | Minor disturbance. No medical intervention is required. e.g., slight abrasion. |
| NACA II | Slight to moderate disturbance. Outpatient medical investigation, but usually no emergency medical measures necessary. e.g., fracture of a finger bone, moderate cuts, dehydration. |
| NACA III | Moderate to severe but not life-threatening disorder. Stationary treatment required, often emergency medical measures on the site. e.g., femur fracture, milder stroke, smoke inhalation. |
| NACA IV | Serious incident where rapid development into a life-threatening condition can not be excluded. In the majority of cases, emergency medical care is required. e.g., vertebral injury with neurological deficit, severe asthma attack; drug poisoning. |
| NACA V | Acute danger. e.g., third grade skull or brain trauma, severe heart attack. |
| NACA VI | Respiratory and or cardiac arrest |
| NACA VII | Death |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gasser, B.; Stouder, J. Rescue Emergencies Due to High-Altitude Illnesses Are Rare in Switzerland. Int. J. Environ. Res. Public Health 2022, 19, 865. https://doi.org/10.3390/ijerph19020865
Gasser B, Stouder J. Rescue Emergencies Due to High-Altitude Illnesses Are Rare in Switzerland. International Journal of Environmental Research and Public Health. 2022; 19(2):865. https://doi.org/10.3390/ijerph19020865
Chicago/Turabian StyleGasser, Benedikt, and Joel Stouder. 2022. "Rescue Emergencies Due to High-Altitude Illnesses Are Rare in Switzerland" International Journal of Environmental Research and Public Health 19, no. 2: 865. https://doi.org/10.3390/ijerph19020865
APA StyleGasser, B., & Stouder, J. (2022). Rescue Emergencies Due to High-Altitude Illnesses Are Rare in Switzerland. International Journal of Environmental Research and Public Health, 19(2), 865. https://doi.org/10.3390/ijerph19020865





