The Role of Facebook® in Promoting a Physically Active Lifestyle: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
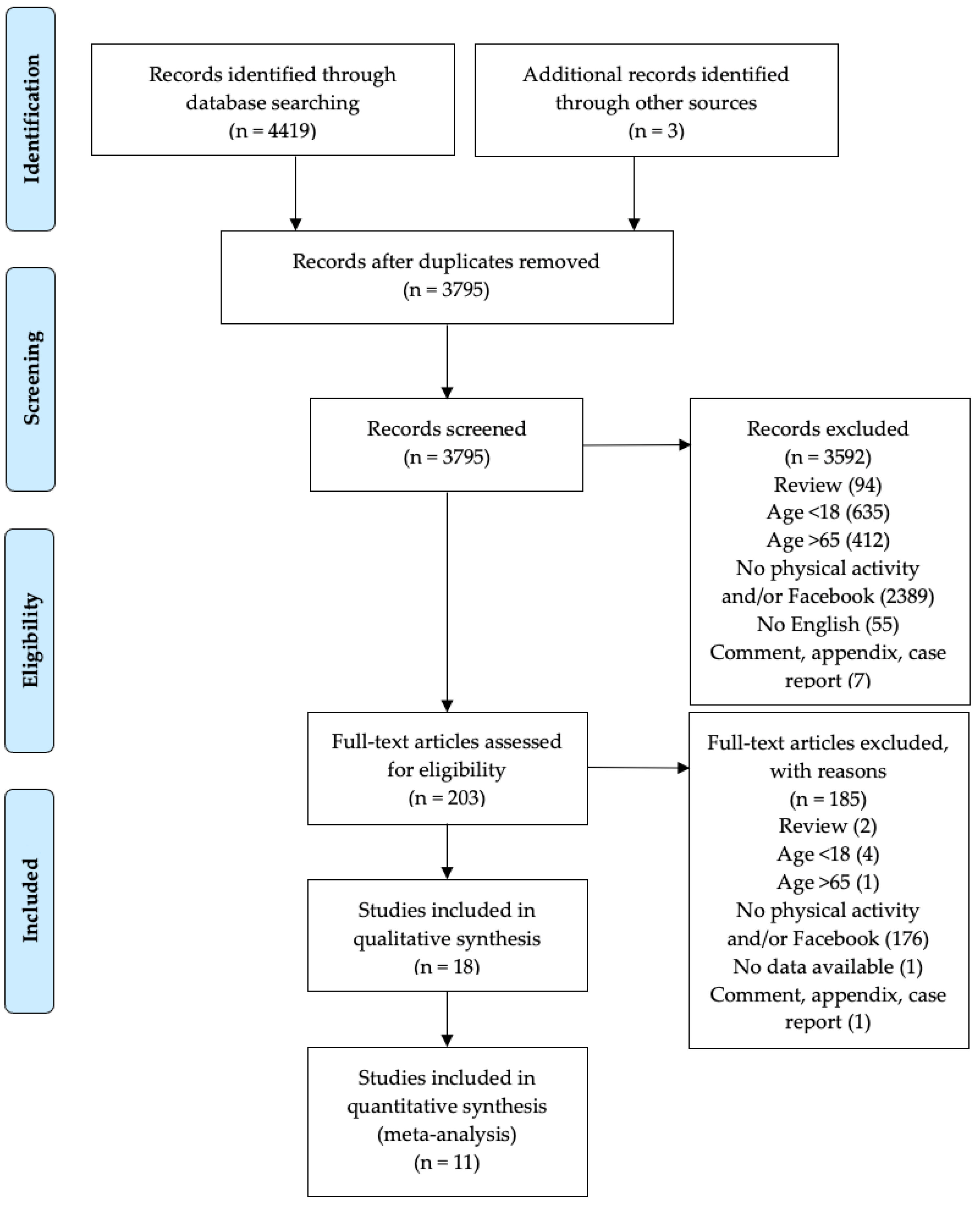
2. Materials and Methods
2.1. Study Design
2.2. Literature Research
2.3. Eligibility Criteria
2.4. Study Quality Assessment
2.5. Data Extraction and Synthesis
2.6. Data Analysis
3. Results
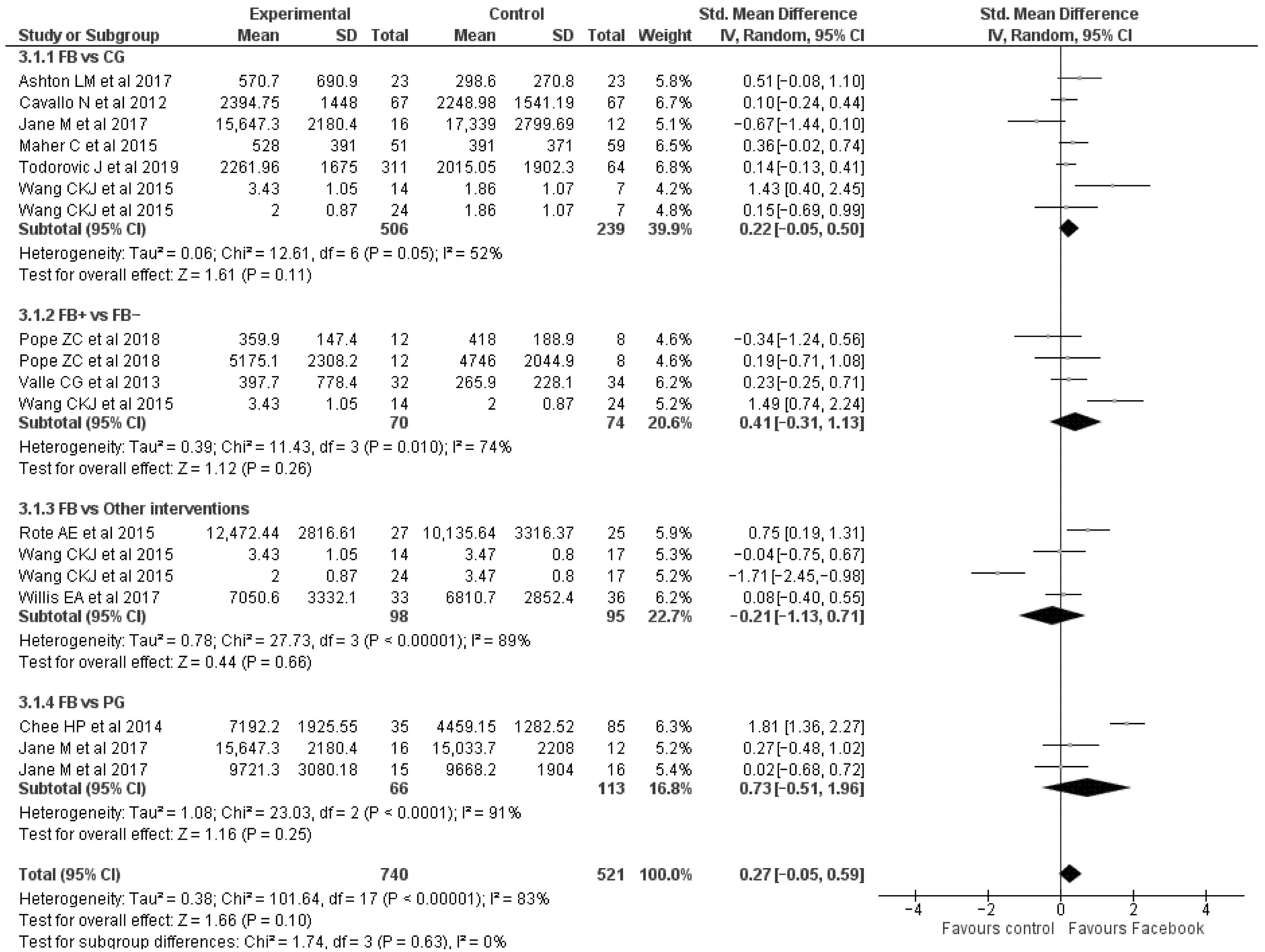
3.1. Physical Activity Parameters
3.2. Anthropometric Parameters
3.3. Cardiovascular Parameters
3.4. Diet Parameters
3.5. Body Composition
3.6. Lipid Profile and Glucose Tolerance
3.7. Psychosocial Parameters
| Study | Groups (n) | Results |
|---|---|---|
| Todorovic J et al. (2019) [22] | FB-G (311) vs. CG (64) | PA parameters ^ IPAQ (met/min/week) ↑: FB-G (+14.4); CG (−22.4) |
| Pope ZC et al. (2019) [41] | FBS-G (19) vs. FB-G (19) | PA parameters ^ SB (min/day) ↓: FBS-G (+2.9); FB-G (−2.1) LPA (min/day) ↑: FBS-G (−6.9); FB-G (+16.3) MVPA (min/day) ↑: FBS-G (+110.7); FB-G (+44.6) Diet parameters ^ Daily Kcaloric consumption (cals) ↓: FBS-G (−0.9); FB-G (−4.6) Daily Fruit intake (cups) ↑: FBS-G (+36.7); FB-G (−7.0) Daily Vegetable intake ↑: FBS-G (+14.5); FB-G (−0.7) Daily Whole Grain intake (oz. equivalents) ↑: FBS-G (+9.8); FB-G (+93.0) Daily SSB Consumption calories ↓: FBS-G (+47.1); FB-G (−7.5) Psychosocial parameters ^ Self-efficacy (sc) ↑: FBS-G (+33.7); FB-G (+28.7) Social-support (sc) ↑: FBS-G (+36.5); FB-G (+19.0) Enjoyment (sc) ↑: FBS-G (+9.3); FB-G (+5.7) Barriers (sc) ↓: FBS-G (−1.7); FB-G (−4.5) Outcome expectancy (sc) ↑: FBS-G (+8.3); FB-G (+7.7) Intrinsic motivation (sc) ↑: FBS-G (+13.7); FB-G (+12.3) Anthropometric parameters ^ Weight (kg) ↓: FBS-G (−0.2); FB-G (−0.5) Body composition ^ BFM (%) ↓: FBS-G (+11.1); FB-G (+1.7) Cardiovascular parameters ^ Cardiorespiratory fitness (heart rate) ↑: FBS-G (+2.6); FB-G (−2.0) |
| Torquati L et al. (2018) [24] | FB-G (47), 6-Mo F-Up (27) | PA parameters Steps (n/d) ↑: FB-G (−4.2) *, 6-Mo F-up (−6.2) SB (%) ↓: FB-G (−0.9), 6-Mo F-up (+2.1) SB (min) ↓: FB-G (−4.6), 6-Mo F-up (0.0) LPA (%) ↑: FB-G (+2.1), 6-Mo F-up (−1.5) LPA (min) ↑: FB-G (−2.4), 6-Mo F-up (−5.0) MVPA (%) ↑: FB-G (−16.7) *, 6-Mo F-up (0.0) Anthropometric parameters Weight (kg) ↓: FB-G (−0.1), 6-Mo F-up (−7.6) BMI (kg/m2) ↓: FB-G (−0.4), 6-Mo F-up (−7.4) WC (cm) ↓: FB-G (0.0), 6-Mo F-up (−6.6) Cardiovascular parameters SBP (mmHg) ↓: FB-G (−0.4), 6-Mo F-up (−1.6) DBP (mmHg) ↓: FB-G (−1.5), 6-Mo F-up (−3.5) Diet parameters Energy intake (kJ/d) ↓: FB-G (+2.3), 6-Mo F-up (−8.6) ARF score (diet quality) ↑: FB-G (+0.6), 6-Mo F-up (−1.2) Fruits and vegetables (%) ↑: FB-G (+26.5) *, 6-Mo F-up (−9.7) Discretionary food (% energy) ↓: FB-G (−2.9), 6-Mo F-up (−13.7) |
| Looyestyn J et al. (2018) [25] | FB-G (41) vs. PG (48); FB-G 5-Mo F-Up (29) vs. PG 5-Mo F-Up (29) | PA parameters MVPA (min/week) ↑: FB-G (+52.2) *,**; PG (+25.4) * FB-G 5-Mo F-Up (−2.7); PG 5-Mo F-Up (−31.3) Psychosocial parameters SE of BEM (sc) ↑: FB-G (−7.3); PG (+4.0) FB-G 5-Mo F-Up (+7.2); PG 5-Mo F-Up (−4.7) Exercise attitude (sc) ↑: FB-G (+2.2); PG (+3.0) FB-G 5-Mo F-Up (−1.7); PG 5-Mo F-Up (0.3) Social support and exercise survey (sc) ↑: FB-G (+18.6) *; PG (+2.8) * FB-G 5-Mo F-Up (−12.4); PG 5-Mo F-Up (−4.6) Cardiovascular parameters HR (bpm) ↓: FB-G (−4.5); PG (−6.6) FB-G 5-Mo F-Up (−0.8); PG 5-Mo F-Up (+3.9) |
| Pope ZC et al. (2018) [26] | FB-G (8) | PA parameters ^ Steps (n/d) ↑: FB-G (+33.6) SB (min/day) ↓: FB-G (−22.8) LPA (min/day) ↑: FB-G (−8.6) MVPA (min/day) ↑: FB-G (+9.7) EE ↑: FB-G (+20.6) Psychosocial parameters ^ Self-efficacy (sc) ↑: FB-G (+3.3) Social-support (sc) ↑: FB-G (+19.9) Enjoyment (sc) ↑: FB-G (+4.7) Barriers (sc) ↓: FB-G (−1.0) Outcome expectancy (sc) ↑: FB-G (−0.3) Anthropometric parameters ^ Weight (kg) ↓: FB-G (−2.9) Body composition ^ BFM (%) ↓: FB-G (−6.2) Cardiovascular parameters ^ Cardiorespiratory fitness (heart rate) ↑: FB-G (0.0) |
| Pope ZC et al. (2018) [26] | FBS-G (12) vs. FB-G (8) | PA parameters Steps (n/d) ↑: FBS-G (+7.1); FB-G (+7.6) SB (min/day) ↓: FBS-G (+0.5); FB-G (+0.1) LPA (min/day) ↑: FBS-G (+8.2); FB-G (+8.1) MVPA (min/day) ↑: FBS-G (+11.4); FB-G (+25.2) EE ↑: FBS-G (+8); FB-G (+5.7) Psychosocial parameters Self-efficacy (sc) ↑: FBS-G (−10.2); FB-G (−8.2) Social-support (sc) ↑: FBS-G (−10) **; FB-G (+25) Enjoyment (sc) ↑: FBS-G (−3); FB-G (+3.1) Barriers (sc) ↓: FBS-G (0.0) **; FB-G (−14.3) Outcome expectancy (sc) ↑: FBS-G (−4.9); FB-G (0.0) Anthropometric parameters Weight (kg) ↓: FBS-G (+0.4); FB-G (0.0) Body composition BFM (%) ↓: FBS-G (+1.0); FB-G (−2.8) Cardiovascular parameters Cardiorespiratory fitness (heart rate) ↑: FBS-G (−4.3); FB-G (−4.3) |
| Naslund JA et al. (2018) [27] | FB-G (19) | PA parameters Improved Fitness (>50 m on 6-MWT) ↑: Yes: 4 No: 14 Anthropometric parameters Weight loss (>5%) ↓: Yes: 7 No: 12 |
| Krishnamohan S et al. (2017) [28] | FB-G (22) vs. CG (23) | PA parameters SB (min/day) ↓: FB-G (+7.4); CG (−6.5) Academic MA (min/week) ↑: FB-G (+32.3); CG (−100) Leisure MA (min/week) ↑: FB-G (+0.9); CG (+35.5) Walking/cycling (min/week) ↑: FB-G (+66.5); CG (+36.1) Academic VA (min/week) ↑: FB-G (0.0); CG (0.0) Leisure VA (min/week) ↑: FB-G (−58.4) *; CG (−47.2) Anthropometric parameters BMI (kg/m2) ↓: FB-G (+0.3); CG (−1.6) * Diet parameters Intake of fruit (d/w) ↑: FB-G (−2.3); CG (+33.3) Intake of fruit (s/d) ↑: FB-G (+28.3); CG (+11.1) Intake of vegetables (d/w) ↑: FB-G (+8.5); CG (−10.5) Intake of vegetables (s/d) ↑: FB-G (0.0); CG (+9.1) Outside meals/week ↓: FB-G (−30.9); CG (+10.5) Intake of junk food (d/w) ↓: FB-G (−39.4) *; CG (−6.9) Intake of junk food (t/d) ↓: FB-G (−33.3) *; CG (0.0) |
| Ashton LM et al. (2017) [29] | FB-G (23) vs. CG (23) | PA parameters Steps (n/d) ↑ #: FB-G (+20.6) *; CG (+9.3) MVPA (min/week) ↑: FB-G (+39.4) **; CG (+24) Anthropometric parameters Weight (kg) ↓: FB-G (−0.7) **; CG (+1.2) BMI (kg/m2) ↓: FB-G (−0.8) **; CG (+1.2) WC (cm) ↓: FB-G (−1.3) **; CG (+2.2) Body composition BFM (kg) ↓: FB-G (−2.5) **; CG (+5.3) SMM (kg) ↑: FB-G (0); CG (+0.3) Cardiovascular parameters SBP (mmHg) ↓: FB-G (−2); CG (−2.1) DBP (mmHg) ↓: FB-G (−2.3); CG (−1.4) HRrest (bpm) ↓: FB-G (−0.1); CG (−2.8) AI (%) ↓: FB-G (−11.9); CG (−2) Diet parameters Diet quality (ARF total score) ↑: FB-G (+19.2) *; CG (+8.2) Fruit (serves/day) ↑: FB-G (+33.3); CG (+23.1) Vegetables (serves/day) ↑: FB-G (+28.6) **; CG (−2.9) Energy intake (kJ/day) ↓: FB-G (−4.3); CG (−0.7) Proportion of energy from ED-NP foods (%) ↓: FB-G (−24.4) **; CG (−6.2) Proportion of energy from alcohol (%) ↓: FB-G (+11.8); CG (−19.2) Lipid profile and Glucose tolerance Chol-tot (mmol/L) ↓: FB-G (−10.3) **; CG (0) LDL (mmol/L) ↓: FB-G (−18.2) **; CG (+5) HDL (mmol/L) ↑: FB-G (0); CG (0) Chol-tot/HDL-C ratio↓: FB-G (−9.1) **; CG (0) TG (mmol/L) ↓: FB-G (0); CG (0) |
| Jane M et al. (2017) [30] | FB-G (19) vs. CG (17) | PA parameters Steps (n/d) ↑: FB-G (+28.5) Energy expenditure (kJ/die) ↑: FB-G (−1.7); CG (+1.5) Anthropometrics parameters Weight (kg) ↓: FB-G (−4.8) **; CG (−1.6) BMI (kg/m2) ↓: FB-G (−4.6) **; CG (−1.5) WC (cm) ↓: FB-G (−4.7) **; CG (−1.8) HC (cm) ↓: FB-G (−2.9); CG (−1.3) Body composition BFM (%) ↓: FB-G (−2.6) **; CG (−0.6) Lean Mass (%) ↑: FB-G (+1.1) **; CG (+0.2) Cardiovascular parameters SBP (mmHg) ↓: FB-G (−2.3); CG (+2.8) DBP (mmHg) ↓: FB-G (−0.7); CG (+1.6) Lipid profile and Glucose tolerance Chol-tot (mmol/L) ↓: FB-G (−3.4); CG (+1.8) LDL (mmol/L) ↓: FB-G (−5.3); CG (0) HDL (mmol/L) ↑: FB-G (0); CG (+6.7) TG (mmol/L) ↓: FB-G (−15.4); CG (+8.3) Fasting glucose (mmol/L) ↓: FB-G (−7.3); CG (+6.9) Insulin (mU/L) ↓: FB-G (−1); CG (+1.2) Diet parameters Energy Intake (kJ/day) ↓: FB-G (−18.3); CG (−13.7) Carbohydrate (%): FB-G (−3); CG (+0.1) Protein (%): FB-G (+4.8); CG (+1.3) Fat (%): FB-G (−2); CG (−0.9) Alcohol (%) ↓: FB-G (−0.5); CG (−0.6) Fibre (g): FB-G (−1.7); CG (−1.8) |
| FB-G (19) vs. PG (18) | PA parameters Steps (n/d) ↑: FB-G (+28.5); PG (+10.7) Energy expenditure (kJ/die) ↑: FB-G (−1.7); PG (−9.8) Anthropometrics parameters Weight (kg) ↓: FB-G (−4.8); PG (−4.2) BMI (kg/m2) ↓: FB-G (−4.6); PG (−4) WC (cm) ↓: FB-G (−4.7); PG (−3.1) HC (cm) ↓: FB-G (−2.9); PG (−2.8) Body composition BFM (%) ↓: FB-G (−2.6); PG (−1.4) Lean Mass (%) ↑: FB-G (+1.1); PG (+0.6) Cardiovascular parameters SBP (mmHg) ↓: FB-G (−2.3); PG (−0.2) DBP (mmHg) ↓: FB-G (−0.7); PG (−0.1) Lipid profile and Glucose tolerance Chol-tot (mmol/L) ↓: FB-G (−3.4); PG (−1.7) LDL (mmol/L) ↓: FB-G (−5.3); PG (−2.7) HDL (mmol/L) ↑: FB-G (0); PG (0) TG (mmol/L) ↓: FB-G (−15.4); PG (+36.4) Fasting glucose (mmol/L) ↓: FB-G (−7.3) **; PG (−6.5) Insulin (mU/L) ↓: FB-G (−1); PG (+11.4) Diet parameters Energy Intake (kJ/day) ↓: FB-G (−18.3); PG (−13) Carbohydrate (%): FB-G (−3); PG (−3.2) Protein (%): FB-G (+4.8); PG (+3.2) Fat (%): FB-G (−2); PG (0) Alcohol (%) ↓: FB-G (−0.5); PG (−0.3) Fibre (g): FB-G (−1.7); PG (+2.4) | |
| PG (18) vs. CG (17) | PA parameters Steps (n/d) ↑: PG (+10.7); Energy expenditure (kJ/die) ↑: PG (−9.8); CG (+1.5) Anthropometrics parameters Weight (kg) ↓: PG (−4.2) **; CG (−1.6) BMI (kg/m2) ↓: PG (−4); CG (−1.5) WC (cm) ↓: PG (−3.1); CG (−1.8) HC (cm) ↓: PG (−2.8); CG (−1.3) Body composition BFM (%) ↓: PG (−1.4); CG (−0.6) Lean Mass (%) ↑: PG (+0.6); CG (+0.2) Cardiovascular parameters SBP (mmHg) ↓: PG (−0.2); CG (+2.8) DBP (mmHg) ↓: PG (−0.1); CG (+1.6) Lipid profile and Glucose tolerance Chol-tot (mmol/L) ↓: PG (−1.7); CG (+1.8) LDL (mmol/L) ↓: PG (−2.7); CG (0) HDL (mmol/L) ↑: PG (0); CG (+6.7) TG (mmol/L) ↓: PG (+36.4); CG (+8.3) Fasting glucose (mmol/L) ↓: PG (−6.5) **; CG (+6.9) Insulin (mU/L) ↓: PG (+11.4); CG (+1.2) Diet parameters Energy Intake (kJ/day) ↓: PG (−13); CG (−13.7) Carbohydrate (%): PG (−3.2); CG (+0.1) Protein (%): PG (+3.2); CG (+1.3) Fat (%): PG (0); CG (−0.9) Alcohol (%) ↓: PG (−0.3); CG (−0.6) Fibre (g): PG (+2.4) **; CG (−1.8) | |
| Willis EA et al. (2017) [31] | FB-G (34) vs. PhC-G (36) | PA parameters Steps per day (num)(a) ↑: FB-G (7050.6 ± 3332.1); PhC-G (6810.7 ± 2852.4) PA (min)(a) ↑: FB-G (103.1 ± 149.7); PhC-G (118.8 ± 91.1) Accelerometer (counts/min) ↑: FB-G (+7.6); PhC-G (+6.9) Met calorie goal (%) ↑: FB-G (22 ± 21.2); PhC-G (44 ± 26.2) ** Complete weekly reports (%) ↑: FB-G (34.7 ± 28.9); PhC-G (37.6 ± 27.4) Anthropometric parameters Weight (kg) ↓: FB-G (−5.8); PhC-G (−6.3) BMI (kg/m2) ↓: FB-G (−6); PhC-G (−5.9) WC (cm) ↓: FB-G (−9.7); PhC-G (−3.5) Categories of weight change (%) Gained: FB-G (11.8); PhC-G (11.1) Lost 0 to 4.9%: FB-G (38.2); PhC-G (30.6) Lost 5 to 9.9%: FB-G (17.7); PhC-G (33.3) Lost >10%: FB-G (14.7); PhC-G (13.9) Diet parameters Kcal/die ↓: FB-G (−24.9); PhC-G (−22.9) Carbohydrate (g): FB-G (−16.1); PhC-G (−23.1) Protein (g): FB-G (−15.8); PhC-G (−10.8) Fat (g): FB-G (−36.2); PhC-G (−22.5) |
| Joseph RP et al. (2015) [32] | FB-G (14) vs. PG (15) | PA parameters Weekly steps (num) ↑: FB-G (−16); PG (−18.9) Sedentary (0–99 ctm) ↓: FB-G (−0.9) **; PG (+1.5) Light activity (100–759 ctm) ↑: FB-G (+7.8) **; PG (+5) Moderate-lifestyle (760–1951 ctm) ↑: FB-G (+6.1) **; PG (−7.3) Moderate activity (1952–5725 ctm) ↑: FB-G (−7.4); PG (+2.3) Vigorous activity (>5725 ctm) ↑: FB-G (+500); PG (−50) Total moderate-to-vigorous activity (>1951 ctm) ↑: FB-G (−5.7); PG (−0.7) Moderate-to-vigorous activity in 10 min bouts or greater (>1951 ctm) ↑: FB-G (+18.2); PG (+9.1) Exercise vital sign (minutes/week) ↑: FB-G (+68.1) *,**; PG (+6.9) Psychosocial parameters Outcome expectations (sc) ↑: FB-G (+3.5); PG (+6.6) ** Self-regulation (sc) ↑: FB-G (+89.9) *,**; PG (+55.1) * Self-efficacy (sc) ↑: FB-G (+4.2); PG (+6.5) Social support from friends (sc) ↑: FB-G (+28.1); PG (+11.4) Social support from family (sc) ↑: FB-G (+30.8) *,**; PG (+14.6) Anthropometric parameters BMI (kg/m2) ↓: FB-G (−0.2); PG (+1) |
| Rote AE et al. (2015) [33] | FB-G (27) vs. SWI-G (26) | PA parameters Mean weekly steps per day (n) ↑: FB-G (+135.5) *,**; SWI-G (+81.2) * |
| Maher C et al. (2015) [18] | FB-G (51) vs. CG (59); FB-G 20-week F-Up (44) vs. CG 20-week F-Up (52) | PA parameters PA time (min/week) ↑: FB-G (+89.2) **; CG (+40.6) FB-G 20-week F-Up (−28.8); CG 20-week F-Up (−14.3) Walking time (min/week) ↑: FB-G (+161.4) **; CG (+45.5) FB-G 20-week F-Up (−50.3); CG 20-week F-Up (−16.9) Moderate PA (min/week) ↑: FB-G (+46); CG (+47.8) FB-G 20-week F-Up (−47.9); CG 20-week F-Up (−36.8) Vigorous PA (min/week) ↑: FB-G (+50); CG (+31.7) FB-G 20-week F-Up (+14.1); CG 20-week F-Up (−1.2) |
| Wang CKJ et al. (2015) [34] | FB3h-G (14) vs. FB1h-G (24) | PA parameters Short form IPAQ (met/min/week) ↑: FB3h-G (+33.5) *; FB1h-G (+4.2) Psychosocial parameters Autonomy (sc) ↑: FB3h-G (−4.9); FB1h-G (+4.8) Competence (sc) ↑: FB3h-G (+12) *; FB1h-G (+20.8) ** Relatedness (sc) ↑: FB3h-G (+8); FB1h-G (+4) Enjoyment (sc) ↑: FB3h-G (0); FB1h-G (+13.7) * Vitality (sc) ↑: FB3h-G (+9.9); FB1h-G (+8.9) |
| FB3h-G (14) vs. EG (17) | PA parameters Short form IPAQ (met/min/week) ↑: FB3h-G (+33.5) *; EG (+20.5) * Psychosocial parameters Autonomy (sc) ↑: FB3h-G (−4.9); EG (−3.5) Competence (sc) ↑: FB3h-G (+12) *.**; EG (+10.7) * Relatedness (sc) ↑: FB3h-G (+8); EG (−2) Enjoyment (sc) ↑: FB3h-G (0); EG (0) Vitality (sc) ↑: FB3h-G (+9.9); EG (+9.1) | |
| FB3h-G (14) vs. CG (7) | PA parameters Short form IPAQ (met/min/week) ↑: FB3h-G (+33.5) *; CG (+18.5) Psychosocial parameters Autonomy (sc) ↑: FB3h-G (−4.9); CG (+3.2) Competence (sc) ↑: FB3h-G (+12) *; CG (+5.5) Relatedness (sc) ↑: FB3h-G (+8); CG (−4.8) Enjoyment (sc) ↑: FB3h-G (0); CG (+14.1) Vitality (sc) ↑: FB3h-G (+9.9); CG (+9.1) | |
| FB1h-G (24) vs. EG (17) | PA parameters Short form IPAQ (met/min/week) ↑: FB1h-G (+4.2); EG (+20.5) * Psychosocial parameters Autonomy (sc) ↑: FB1h-G (−4.8); EG (−3.5) Competence (sc) ↑: FB1h-G (+20.8) **; EG (+10.7) * Relatedness (sc) ↑: FB1h-G (+4); EG (−2) Enjoyment (sc) ↑: FB1h-G (+13.7) *; EG (0) Vitality (sc) ↑: FB1h-G (+8.9); EG (+9.1) | |
| FB1h-G (24) vs. CG (7) | PA parameters Short form IPAQ (met/min/week) ↑: FB1h-G (+4.2); CG (+18.5) Psychosocial parameters Autonomy (sc) ↑: FB1h-G (−4.8); CG (+3.2) Competence (sc) ↑: FB1h-G (+20.8); CG (+5.5) Relatedness (sc) ↑: FB1h-G (+4); CG (−4.8) Enjoyment (sc) ↑: FB1h-G (+13.7) *,**; CG (+14.1) Vitality (sc) ↑: FB1h-G (+8.9); CG (+9.1) | |
| EG (17) vs. CG (7) | PA parameters Short form IPAQ (met/min/week) ↑: EG (+20.5) *; CG (+18.5) Psychosocial parameters Autonomy (sc) ↑: EG (−3.5); CG (+3.2) Competence (sc) ↑: EG (+10.7) *; CG (+5.5) Relatedness (sc) ↑: EG (−2); CG (−4.8) Enjoyment (sc) ↑: EG (0); CG (+14.1) Vitality (sc) ↑: EG (+9.1); CG (+9.1) | |
| Chee HP et al. (2014) [35] | FB-G (35) vs. PG (85); FB-G 2-month F-Up (35) vs. PG 2-month F-Up (85) | PA parameters Step per day (num) # ↑: FB-G (+84.5) *,**; PG (+13.2) * FB-G 2-month F-Up (+58.1) *,**; PG 2-month F-Up (+9.6) * Anthropometric parameters Weight (kg) # ↓: FB-G (−7.3) *; PG (−1.1) * FB-G 2-month F-Up (−4.4) *; PG 2-month F-Up (−0.5) * BMI (kg/m2) # ↓: FB-G (−7.4) *; PG (−1) * FB-G 2-month F-Up (−4.4); PG 2-month F-Up (−0.5) WC (cm) # ↓: FB-G (−4.5) *; PG (−0.7) * FB-G 2-month F-Up (−2.7) *; PG 2-month F-Up (−0.3) * HC (cm) # ↓: FB-G (−2.4) *; PG (−0.4) * FB-G 2-month F-Up (−1.4) *; PG 2-month F-Up (−0.2) * WHR (sc) # ↓: FB-G (−2.3) *; PG (−1.1) * FB-G 2-month F-Up (−1.1) *; PG 2-month F-Up (0.0) * Body composition BFM (kg) # ↓: FB-G (−22.7) *; PG (−3.9) * FB-G 2-month F-Up (−14.1); PG 2-month F-Up (−2.7) BFM (%) # ↓: FB-G (−17.1) *,**; PG (−3) * FB-G 2-month F-Up (−10.4) *,**; PG 2-month F-Up (−2.2) * Lipid profile and Glucose tolerance Chol.tot (mmol/L) # ↓: FB-G (−14.4) *; PG (−3.6) * FB-G 2-month F-Up (−9.6) *; PG 2-month F-Up (−1.7) * LDL (mmol/L) # ↓: FB-G (−21.4) *; PG (−4.9) * FB-G 2-month F-Up (−14.5) *; PG 2-month F-Up (−1.8) * HDL (mmol/L) # ↑: FB-G (+15.8) *; PG (+3.6) * FB-G 2-month F-Up (9.2) *; PG 2-month F-Up (1.8) * Triglycerides (mmol/L) # ↓: FB-G (−34.9) *; PG (−7) * FB-G 2-month F-Up (−19.7) *; PG 2-month F-Up (−4.8) * Fasting glucose (mmol/L) # ↓: FB-G (−18.1) *; PG (−3.2) * FB-G 2-month F-Up (−11.7) *; PG 2-month F-Up (−0.8) * Cardiovascular parameters SBP (mmHg) # ↓: FB-G (−5.1) *; PG (−0.9) * FB-G 2-month F-Up (−3.1) *; PG 2-month F-Up (−0.5) * DBP (mmHg) # ↓: FB-G (−6.2) *; PG (−1.2) * FB-G 2-month F-Up (−3.8) *; PG 2-month F-Up (−0.6) * |
| Valle CG et al. (2013) [36] | FB-G.fit (32) vs. FB-G.com (34) | PA parameters MVPA (min/week) ↑: FB-G.fit(+51.1) *; FB-G.com(+38.9) * LPA (min/week) ↑: FB-G.fit(+197.1) *,**; FB-G.com(+25.3) Total PA (min/week) ↑: FB-G.fit(+112) *; FB-G.com(+33.4) * Anthropometric parameters Weight (kg) ↓: FB-G.fit(−7.8) *; FB-G.com(−1.9) BMI (kg/m2) ↓: FB-G.fit(−6.3) *; FB-G.com(−1.4) |
| Cavallo N et al. (2012) [37] | FB-G (67) vs. CG (67) | PA parameters PA total (kcal) ↑: FB-G (+45.5) *; CG (+31.8) PA light (kcal) ↑: FB-G (+5.8); CG (+138.3) PA moderate (kcal) ↑: FB-G (+213.2) *; CG (+105.9) PA heavy (kcal) ↑: FB-G (+96.5) *; CG (+142.5) |
4. Discussion
4.1. Physical Activity Parameters
4.2. Anthropometric Parameters
4.3. Cardiovascular Parameters
4.4. Diet Parameters
4.5. Body Composition
4.6. Lipid Profile and Glucose Tolerance
4.7. Psychosocial Parameters
4.8. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- WHO. Physical Inactivity a Leading Cause of Disease and Disability, Warns WHO. 2020. Available online: https://www.Who.Int/Mediacentre/News/Releases/Release23/En/#:~:Text=Approximately%202%20million%20deaths%20per,And%20disability%20in%20the%20world (accessed on 14 June 2020).
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.-M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef] [Green Version]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.; Martin, B.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Kavussanu, M.; Roberts, G.C. Motivation in Physical Activity Contexts: The Relationship of Perceived Motivational Climate to Intrinsic Motivation and Self-Efficacy. J. Sport Exerc. Psychol. 1996, 18, 264–280. [Google Scholar] [CrossRef]
- Knittle, K.; Nurmi, J.; Crutzen, R.; Hankonen, N.; Beattie, M.; Dombrowski, S.U. How can interventions increase motivation for physical activity? A systematic review and meta-analysis. Health Psychol. Rev. 2018, 12, 211–230. [Google Scholar] [CrossRef]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [Green Version]
- Rhodes, R.E.; Gray, S.M.; Husband, C. Experimental manipulation of affective judgments about physical activity: A systematic review and meta-analysis of adults. Health Psychol. Rev. 2019, 13, 18–34. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, P.D.; Joyner, C. Source and Size of Emotional and Financial-Related Social Support Network on Physical Activity Behavior Among Older Adults. J. Phys. Act. Health 2016, 13, 776–779. [Google Scholar] [CrossRef]
- Berkman, L.F.; Glass, T.; Brissette, I.; Seeman, T.E. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med. 2000, 51, 843–857. [Google Scholar] [CrossRef]
- King, A.C.; Whitt-Glover, M.C.; Marquez, D.X.; Buman, M.P.; Napolitano, M.A.; Jakicic, J.; Fulton, J.E.; Tennant, B.L. Physical Activity Promotion: Highlights from the 2018 Physical Activity Guidelines Advisory Committee Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1340–1353. [Google Scholar] [CrossRef]
- Schwartz, J.; Rhodes, R.; Bredin, S.; Oh, P.; Warburton, D. Effectiveness of Approaches to Increase Physical Activity Behavior to Prevent Chronic Disease in Adults: A Brief Commentary. J. Clin. Med. 2019, 8, 295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Physical Activity Strategy for the WHO European Region; Europe W.H.O.: Copenhagen, Denmark, 2016; pp. 2016–2025. Available online: https://www.Euro.Who.Int/__data/Assets/Pdf_file/0014/311360/Physical-Activity-Strategy-2016-2025.Pdf (accessed on 21 July 2020).
- Greene, J.A.; Choudhry, N.K.; Kilabuk, E.; Shrank, W.H. Online Social Networking by Patients with Diabetes: A Qualitative Evaluation of Communication with Facebook. J. Gen. Intern. Med. 2011, 26, 287–292. [Google Scholar] [CrossRef] [Green Version]
- Cobb, N.K.; Graham, A.L.; Abrams, D.B. Social Network Structure of a Large Online Community for Smoking Cessation. Am. J. Public Health 2010, 100, 1282–1289. [Google Scholar] [CrossRef] [PubMed]
- Hamari, J.; Koivisto, J. “Working out for likes”: An empirical study on social influence in exercise gamification. Comput. Hum. Behav. 2015, 50, 333–347. [Google Scholar] [CrossRef]
- Laranjo, L.; Arguel, A.; Neves, A.L.; Gallagher, A.M.; Kaplan, R.; Mortimer, N.; Mendes, G.A.; Lau, A.Y.S. The influence of social networking sites on health behavior change: A systematic review and meta-analysis. J. Am. Med. Inform. Assoc. 2015, 22, 243–256. [Google Scholar] [CrossRef]
- Maher, C.; Ferguson, M.; Vandelanotte, C.; Plotnikoff, R.; de Bourdeaudhuij, I.; Thomas, S.; Nelson-Field, K.; Olds, T. A Web-Based, Social Networking Physical Activity Intervention for Insufficiently Active Adults Delivered via Facebook App: Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e174. [Google Scholar] [CrossRef] [Green Version]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- van Tulder, M.W.; Assendelft, W.J.J.; Koes, B.W.; Bouter, L.M. Method Guidelines for Systematic Reviews in the Cochrane Collaboration Back Review Group for Spinal Disorders. Spine 1997, 22, 2323–2330. [Google Scholar] [CrossRef] [Green Version]
- Todorovic, J.; Terzic-Supic, Z.; Djikanovic, B.; Nesic, D.; Piperac, P.; Stamenkovic, Z. Can social media intervention improve physical activity of medical students? Public Health 2019, 174, 69–73. [Google Scholar] [CrossRef]
- Pope, Z.; Barr-Anderson, D.; Lewis, B.; Pereira, M.; Gao, Z. Use of Wearable Technology and Social Media to Improve Physical Activity and Dietary Behaviors among College Students: A 12-Week Randomized Pilot Study. Int. J. Environ. Res. Public Health 2019, 16, 3579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torquati, L.; Kolbe-Alexander, T.; Pavey, T.; Leveritt, M. Changing Diet and Physical Activity in Nurses: A Pilot Study and Process Evaluation Highlighting Challenges in Workplace Health Promotion. J. Nutr. Educ. Behav. 2018, 50, 1015–1025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Looyestyn, J.; Kernot, J.; Boshoff, K.; Maher, C. A Web-Based, Social Networking Beginners’ Running Intervention for Adults Aged 18 to 50 Years Delivered via a Facebook Group: Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, e67. [Google Scholar] [CrossRef]
- Pope, Z.; Zeng, N.; Zhang, R.; Lee, H.; Gao, Z. Effectiveness of Combined Smartwatch and Social Media Intervention on Breast Cancer Survivor Health Outcomes: A 10-Week Pilot Randomized Trial. J. Clin. Med. 2018, 7, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naslund, J.A.; Aschbrenner, K.A.; Marsch, L.A.; McHugo, G.J.; Bartels, S.J. Facebook for Supporting a Lifestyle Intervention for People with Major Depressive Disorder, Bipolar Disorder, and Schizophrenia: An Exploratory Study. Psychiatr. Q. 2018, 89, 81–94. [Google Scholar] [CrossRef]
- Krishnamohan, S. Efficacy of Health Education using Facebook to Promote Healthy Lifestyle among Medical Students in Puducherry, India: A Non-Randomized Controlled Trial. J. Clin. Diagn. Res. 2017, 11, LC07–LC10. [Google Scholar] [CrossRef] [PubMed]
- Ashton, L.M.; Morgan, P.J.; Hutchesson, M.J.; Rollo, M.E.; Collins, C.E. Feasibility and preliminary efficacy of the ‘HEYMAN’ healthy lifestyle program for young men: A pilot randomised controlled trial. Nutr. J. 2017, 16, 2. [Google Scholar] [CrossRef] [Green Version]
- Jane, M.; Hagger, M.; Foster, J.; Ho, S.; Kane, R.; Pal, S. Effects of a weight management program delivered by social media on weight and metabolic syndrome risk factors in overweight and obese adults: A randomised controlled trial. PLoS ONE 2017, 12, e0178326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willis, E.A.; Szabo-Reed, A.N.; Ptomey, L.T.; Steger, F.L.; Honas, J.J.; Al-Hihi, E.M.; Lee, R.; Lee, J.; Oh, Y.; Washburn, R.A.; et al. Distance learning strategies for weight management utilizing online social networks versus group phone conference call. Obes. Sci. Pract. 2017, 3, 134–142. [Google Scholar] [CrossRef] [Green Version]
- Joseph, R.P.; Keller, C.; Adams, M.A.; Ainsworth, B.E. Print versus a culturally-relevant Facebook and text message delivered intervention to promote physical activity in African American women: A randomized pilot trial. BMC Women’s Health 2015, 15, 30. [Google Scholar] [CrossRef] [Green Version]
- Rote, A.E.; Klos, L.A.; Brondino, M.J.; Harley, A.E.; Swartz, A.M. The Efficacy of a Walking Intervention Using Social Media to Increase Physical Activity: A Randomized Trial. J. Phys. Act. Health 2015, 12, S18–S25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.C.K.; Leng, H.K.; Kee, Y.H. Use of Facebook in physical activity intervention programme: Test of self-determination theory. Int. J. Sport Psychol. 2015, 46, 210–224. [Google Scholar]
- Chee, H.P.; Hazizi, A.S.; Mohd Nasir, M.T. A randomised controlled trial of a Facebook-based physical activity intervention for government employees with metabolic syndrome. Malays. J. Nutr. 2014, 20, 165–181. [Google Scholar]
- Valle, C.G.; Tate, D.F.; Mayer, D.K.; Allicock, M.; Cai, J. A randomized trial of a Facebook-based physical activity intervention for young adult cancer survivors. J. Cancer Surviv. 2013, 7, 355–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavallo, D.N.; Tate, D.F.; Ries, A.V.; Brown, J.D.; DeVellis, R.F.; Ammerman, A.S. A Social Media–Based Physical Activity Intervention. Am. J. Prev. Med. 2012, 43, 527–532. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Sawilowsky, S. New effect size rules of thumb. Theor. Behav. Found. 2009, 8, 597–599. [Google Scholar] [CrossRef]
- Napolitano, M.A.; Hayes, S.; Bennett, G.G.; Ives, A.K.; Foster, G.D. Using facebook and text messaging to deliver a weight loss program to college students. Obesity 2013, 21, 25–31. [Google Scholar] [CrossRef]
- Pope, Z.; Lee, J.E.; Zeng, N.; Lee, H.Y.; Gao, Z. Feasibility of smartphone application and social media intervention on breast cancer survivors’ health outcomes. Transl. Behav. Med. 2019, 9, 11–22. [Google Scholar] [CrossRef] [Green Version]
- Lee, I.-M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Edney, S.; Plotnikoff, R.; Vandelanotte, C.; Olds, T.; de Bourdeaudhuij, I.; Ryan, J.; Maher, C. “Active Team” a social and gamified app-based physical activity intervention: Randomised controlled trial study protocol. BMC Public Health 2017, 17, 859. [Google Scholar] [CrossRef] [Green Version]
- Arietaleanizbeaskoa, M.S.; Sancho, A.; Olazabal, I.; Moreno, C.; Gil, E.; Garcia-Alvarez, A.; Mendizabal, N.; de la Fuente, I.; Dominguez, S.; Pablo, S.; et al. Effectiveness of physical exercise for people with chronic diseases: The EFIKRONIK study protocol for a hybrid, clinical and implementation randomized trial. BMC Fam. Pract. 2020, 21, 227. [Google Scholar] [CrossRef] [PubMed]
- Curioni, C.C.; Lourenço, P.M. Long-term weight loss after diet and exercise: A systematic review. Int. J. Obes. 2005, 29, 1168–1174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pedersen, B.K.; Saltin, B. Exercise as medicine-evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miele, E.M.; Headley, S.A.E. The Effects of Chronic Aerobic Exercise on Cardiovascular Risk Factors in Persons with Diabetes Mellitus. Curr. Diabetes Rep. 2017, 17, 97. [Google Scholar] [CrossRef]
- Schoeppe, S.; Alley, S.; van Lippevelde, W.; Bray, N.A.; Williams, S.L.; Duncan, M.J.; Vandelanotte, C. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 127. [Google Scholar] [CrossRef] [Green Version]
- Vaughan, C.A.; Ghosh-Dastidar, M.; Dubowitz, T. Attitudes and Barriers to Healthy Diet and Physical Activity: A Latent Profile Analysis. Health Educ. Behav. 2018, 45, 381–393. [Google Scholar] [CrossRef]
- Liberman, K.; Forti, L.N.; Beyer, I.; Bautmans, I. The effects of exercise on muscle strength, body composition, physical functioning and the inflammatory profile of older adults. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 30–53. [Google Scholar] [CrossRef]
- Kelley, G.A.; Kelley, K.S. Effects of aerobic exercise on C-reactive protein, body composition, and maximum oxygen consumption in adults: A meta-analysis of randomized controlled trials. Metabolism 2006, 55, 1500–1507. [Google Scholar] [CrossRef] [PubMed]
- Burrup, R.; Tucker, L.A.; le Cheminant, J.D.; Bailey, B.W. Strength training and body composition in middle-age women. J. Sports Med. Phys. Fit. 2017, 58, 82–91. [Google Scholar] [CrossRef]
- Finucane, F.M.; Sharp, S.J.; Purslow, L.R.; Horton, K.; Horton, J.; Savage, D.B.; Brage, S.; Besson, H.; de Lucia Rolfe, E.; Sleigh, A.; et al. The effects of aerobic exercise on metabolic risk, insulin sensitivity and intrahepatic lipid in healthy older people from the Hertfordshire Cohort Study: A randomised controlled trial. Diabetologia 2010, 53, 624–631. [Google Scholar] [CrossRef] [Green Version]
- Barazzoni, R.; Gortan Cappellari, G.; Ragni, M.; Nisoli, E. Insulin resistance in obesity: An overview of fundamental alterations. Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2018, 23, 149–157. [Google Scholar] [CrossRef] [PubMed]
- amanouchi, K.; Shinozaki, T.; Chikada, K.; Nishikawa, T.; Ito, K.; Shimizu, S.; Ozawa, N.; Suzuki, Y.; Maeno, H.; Kato, K.; et al. Daily Walking Combined with Diet Therapy Is a Useful Means for Obese NIDDM Patients Not Only to Reduce Body Weight But Also to Improve Insulin Sensitivity. Diabetes Care 1995, 18, 775–778. [Google Scholar] [CrossRef] [PubMed]
| Participants, Interventions, Comparators, Outcomes, Study (PICOS) Designs | |
|---|---|
| PICOS | Details |
| Participants | Male and female aged from 18 to 65 years old |
| Interventions | Supervised or no supervised exercise protocol with Facebook group support |
| Comparative factors | Facebook-support intervention compared with other type of support |
| Outcomes | Primary outcomes: evaluation of PA before and after the intervention Secondary outcomes: changes on weight, BMI, body circumferences, body composition, diet parameters, cardiovascular parameters |
| Study designs | Pilot study, RCT, no-RCT, exploratory study, Randomized pilot trial |
| Citation | Randomization Procedure | Similarity of Study Groups | Inclusion or Exclusion Criteria | Dropouts | Blinding | Compliance | Intention-to-Treat Analysis | Timing of Outcomes Assessment | Follow-Up | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Todorovic J et al. (2019) [22] | − | + | − | + | − | − | − | + | − | 3/9 |
| Pope ZC et al. (2019) [23] | + | + | + | + | − | + | − | + | − | 6/9 |
| Torquati L et al. (2018) [24] | − | − | + | + | − | + | + | + | + | 6/9 |
| Looyestyn J et al. (2018) [25] | + | − | + | + | − | + | + | + | + | 7/9 |
| Pope ZC et al. (2018) [26] | − | − | + | + | − | − | − | + | − | 3/9 |
| Pope ZC et al. (2018) [26] | + | + | + | + | − | + | − | + | − | 6/9 |
| Naslund JA et al. (2018) [27] | − | − | + | + | − | + | − | − | − | 3/9 |
| Krishnamohan S et al. (2017) [28] | − | + | + | + | − | − | − | − | − | 3/9 |
| Ashton LM et al. (2017) [29] | + | − | + | + | + | + | + | − | − | 6/9 |
| Jane M et al. (2017) [30] | + | − | + | + | − | − | − | + | − | 4/9 |
| Willis EA et al. (2016) [31] | + | + | + | + | − | + | + | − | − | 6/9 |
| Joseph RP et al. (2015) [32] | + | + | + | + | − | + | − | + | − | 6/9 |
| Rote AE et al. (2015) [33] | + | + | + | − | − | + | − | + | − | 5/9 |
| Maher C et al. (2015) [18] | + | − | + | + | + | + | + | + | + | 8/9 |
| Wang CKJ et al. (2015) [34] | − | − | − | − | − | − | − | − | − | 0/9 |
| Chee HP et al. (2014) [35] | + | − | + | + | − | + | − | + | + | 6/9 |
| Valle CG et al. (2013) [36] | + | − | + | + | − | + | + | − | − | 5/9 |
| Cavallo N et al. (2012) [37] | + | − | + | + | − | − | + | + | − | 5/9 |
| Study | Subjects and Grouping (n) | Protocol Duration and Frequency; Training Modality, Program and Intensity |
|---|---|---|
| Todorovic J et al. (2019) [22] | 375 medical students FB-G (311) CG (64) | Duration: 4 weeks Facebook group Students were free to practice any kind of physical activity if and when they wanted to. Facebook group was managed by the research team, that used a participatory approach. All members were allowed to post motivational messages or questions for their peers; the reports and photos from organized events were also posted regularly, so all participants could follow the level of participation of other students. Control group In this group, students were free to practice any kind of physical activity if and when they wanted to, but they did not join the facebook group. |
| Pope ZC et al. (2019) [41] | 38 college students, men age 21.5 FB+S-G (19; 15F, 4M) FB-G (19; 13F, 6M)) | Duration: 12 weeks Facebook group1 1. Smartwatch to recorded daily step; 2. FB group: Social Cognitive Theory-related health education tips 2 twice-weekly. The aim was to integrate PA into their daily routine improving PA-related self-efficacy, outcome expectancy, social support and enjoyment. Facebook group2 FB group: Social Cognitive Theory-related health education tips 2 twice-weekly. The aim was to integrate PA into their daily routine improving PA-related self-efficacy, outcome expectancy, social support and enjoyment. |
| Torquati L et al. (2018) [24] | 47 healthy nurses, mean age 41.4 FB-G (47; 6M, 41F) | Duration: 12 weeks, with a 6-month follow up. Mobile app to set diet; accelerometers to monitor physical activity behavior; FB group where people share experiences and motivate others. Moreover, diet and PA suggestion was given by FB group. |
| Looyestyn J et al. (2018) [25] | 89 healthy adults, mean age 35.2 FB-G (41; 4M, 37F) PG (48; 29M, 34F) | Duration: 8 weeks, 30 min 3 d/w, with a 5-month follow up. Facebook group Warm-up: 5 min Main part: week 1 (5 sets run/walk 1:1 min; 6 sets run/walk 1:1 min; 5 sets run/walk 1.5:1.5 min); week 2 (6 sets run/walk 1.5:1.5 min; 5 sets run/walk 2:2 min; 3 sets run/walk 3:3 min); week 3 (6 sets run/walk 2:2 min; 6 sets run/walk 2:1 min; 6 sets run/walk 3:1.5 min); week 4 (5 sets run/walk 4:2 min; 7 sets run/walk 3:1 min; 12 min run); week 5 (6 sets run/walk 4:2 min; 10 sets run/walk 3:1 min; 4 sets run/walk 6:2 min); week 6 (15 min run; 3 sets run/walk 8:3 min; 18 min run); week 7 (5 sets run/walk 6:2 min; run 22 min; 3 sets run/walk 10:2 min); week 8 (26 min run; 16 min run, 2 min walk, 16 min run; 30 min run) Cool-down: 5 min Each day the group facilitator posted a message to the closed FB group. These posts were informative and encouraged social interaction including asking participants to post photos, providing information with lonks, motivational quotes, opinion polls, and posts prompting participants to answer questions and interest. Paper group Self-directed running program only to follow individually. |
| Pope ZC et al. (2018) [26] | 8 female breast cancer survivor, mean age 45.8 | Duration: 10 weeks: 1. Mobile application to recorded daily step 2. FB group: Social Cognitive Theory-related health education tips 2 twice-weekly. The aim was to integrate PA into their daily routine improving PA-related self-efficacy, outcome expectancy, social support and enjoyment while reducing physical activity-related barriers. |
| Pope ZC et al. (2018) [26] | 20 breast cancer survivor, mean age 52.8 FB+S-G (12F) FB-G (8F) | Duration: 10 weeks Facebook group1 1. Smartwatch to recorded daily step; 2. FB group: Social Cognitive Theory-related health education tips 2 twice-weekly. The aim was to integrate PA into their daily routine improving PA-related self-efficacy, outcome expectancy, social support and enjoyment. Facebook group2 FB group: Social Cognitive Theory-related health education tips 2 twice-weekly. The aim was to integrate PA into their daily routine improving PA-related self-efficacy, outcome expectancy, social support and enjoyment. |
| Naslund JA et al. (2018) [27] | 25 obese people with depressive disorder, bipolar disorder, and schizophrenia, mean age 49.2 FB-G (19; 7M, 12F) CG_not join the Facebook Group (6; 5M, 1F) | Duration: 24 weeks, 1 + 2 d/w Facebook group One weight management session facilitated by two lifestyle coaches and two optional exercise sessions led by a certified fitness trainer. Weight management: interactive focused on healthy eating and exercise, with group discussion and teamwork exercise when participants worked together to plan healthy meals and overcome challenges to adopting healthier lifestyle. Exercise sessions: stretching, resistance and cardio exercise tailored to the needs of obese sedentary adults. These sessions were intended to help participants work towards reaching 150 min of exercise each week. The program also included a secret Facebook group to allow participants to connect and support each other towards achieving their healthy eating and exercise goals. |
| Krishnamohan S et al. (2017) [28] | 45 college students, age: 18–23 FB-G (22; 12M, 10F) CG (23; 12M, 11F) | Duration: 6 weeks Facebook group Inclusion in a private Facebook group in which the health education messages were posted thrice a week in the form of pictures, videos, quotes. Content was decided by a team of dietician, physical education trainer and public health specialist. Control group No such intervention was done for the control group. |
| Ashton LM et al. (2017) [29] | 47 men, age 18–25 FB-G (24M) CG (23M) | Duration: 12 weeks Facebook group 1. Responsive website with relevant information and resources including guidelines, support video and recommended mobile application for improving eating habits, PA, reducing alcohol intake or coping with stress. 2. Wearable PA tracker with associated mobile phone application. 3. 1 h of weekly supervised PA: 40 min of aerobic and strength exercise, 10 min of healthy eating education, 10 min of stress and well-being management 4. An individualized session (week 3) in which personal tailored goals for dietary improvements were set. 5. A private FB group to facilitate social support. 6. Gymstick resistance band for home-based strength training (preferably 2 d/w). 7. A TEMPlate dinner disc to guide main meal portion size form main meal components. Control group Control participants were asked to continue their usual lifestyle for 3 months and offered the program once follow-up assessments were completed. |
| Jane M et al. (2017) [30] | 67 obese or overweight; subjects, mean age: 21–65 FB-G (23; 4M, 19F) PG (23; 2M, 21F) CG (21; 4M, 17F) | Duration: 24 weeks Facebook group Participants were instructed to follow the Total Wellbeing Diet: an energy-reduced, low fat, lower carbohydrate, and higher protein diet. In addition, they were issued with a pedometer and instructed to achieve 10,000 steps per day. The information was received into a secret FB group. Paper group The same instructions and information of the FG, but in written form. Control group Participants were instructed to follow the Australian Government dietary guidelines as well as the National Physical Activity Guidelines for Adults as standard care. |
| Willis EA et al. (2016) [31] | 70 obese people, age: 21–70 FB-G (34; 5M, 29F) PhC-G (36; 6M, 30F) | Duration: 24 weeks Facebook group 24 weekly online modules (1 health lesson post, 1 audio recordings of the phone conference group, 4 comments to highlight the major points of the lesson). Participants were instructed to post a minimum of 4 comments on the message boards per week. Phone conference group 24 meeting (1 evening per week) of group phone conference of 60 min. Participants were encouraged to actively participate and interact with the other. |
| Joseph RP et al. (2015) [32] | 29 healthy women, mean age 35 FB-G (14F) PG (15F) | Duration: 8 weeks Facebook group 1. Weekly PA promotion materials posted on the FB group wall; 2. Discussion topics and participants engagement on the group FB wall: week 1 (overview of the national PA recommendations, health benefits of PA, and PA statistics among African American women); week 2 (developing a PA plan that works for you); week 3 (barriers to PA among African American women and strategies to overcoming barriers); week 4 (developing a social support network to promote PA); week 5 (strategies for incorporating short bouts of PA into your daily routine to achieve national PA recommendations); week 6 (testimonials from African American Women on how they successfully incorporate PA into their daily lives); week 7 (National PA recommendations, barriers to PA among African American Women and strategies to overcoming barriers and incorporate more PA into your life); week 8 (strategies for maintaining a physical active lifestyle after the intervention); 3. Motivational text messages promoting PA: 3 text messages every each week (a. tips on strategies to increase PA throughout the day; b. information on how to overcome barriers to PA; c. reminders of the health benefits of PA; d. motivational/inspirational tips and quotes to participants); 4. Adaptive pedometer-based self-monitoring and goal-setting program: weekly individualized step goals and social reinforcement via email. Printed group 1. Mailed print-based component: booklets mailed every two weeks at home with general information on risk factors for cardiovascular disease, the benefits of PA, tips and strategies to increase daily PA, and encouraged participants to perform a minimum of 150 min of MVPA per week; 2. Static pedometer-based self-monitoring program: participants were instructed to achieve a static goal of 8000–10,000 steps each day. |
| Rote AE et al. (2015) [33] | 53 university students, mean age 18 FB-G (27F) SWI-G (26F) | Duration: 8 weeks Facebook group Each week: personal FB message from the intervention leader requesting a report of their steps/day for the previous week. New step goal each week in according to the previous week steps (10% more steps than the previous mean). Weekly post in the FB page and group with educational information. Standard Walking Intervention group Weekly e-mails with the new step goal in according to the previous week steps (10% more steps than the previous mean), and educational information (the same of FB group). |
| Maher C et al. (2015) [18] | 110 adults, mean age 35.6 FB-G (51; 14M, 37F) CG (59; 18M, 41F) | Duration: 50-day, with a 20-week follow up Facebook group Team challenge: participants are provided with a pedometer and encourage achieving 10,000 steps per day, working in teams of 3 to 8 FB friends. Control group Waiting list, with health monitoring over the ensuing 5 months. |
| Wang CKJ et al. (2015) [34] | 62 university students, mean age 22.3 FB3h-G (14) FB1h-G (24) EG (17) CG (7) | Duration: 8 weeks Facebook1 group 3 h of physical fitness class taught by university lecturer each week + FB group. Facebook2 group Voluntary 1 h of exercise programme taught by experienced university lecturer each week + FB group. Exercise group 3 h of physical fitness class each week. Control group This group did not receive any intervention. |
| Chee HP et al. (2014) [35] | 120 government employees, mean age: 18–59 FB-G (35; 11M, 24F) PG (85, 23M, 62F) | Duration: 16 weeks, with a 2-month follow up Facebook group The participants received a card to log the number of steps taken per day and a pamphlet on PA information that summarized the information provided on FB. Moreover, participants can view and comment the content of the posts, in addition to logging their daily steps counts, through the FB group page. The content of the FB posts were the subsequent: Week 1: healthy every day with 10,000 steps per day Week 2: PA recommendation (10,000 steps per day, or 150 min of moderate intensity PA per week, or 75 min of vigorous PA per week) Week 3–5: benefits of walking Week 6–8: walking as the PA Week 9: PA level based on number of steps per day Week 10–15: strategies to increase number of steps per day (e.g., to park the vehicle far away from the office; to use the stairs instead of the elevator; to take 10-min walks for every 2-h worked) Week 16: PA pyramid Printed group The printed group did not receive a weekly physical activity-related intervention, but the participants obtained a card to log the number of steps taken per day and a pamphlet on PA information. |
| Valle CG et al. (2013) [36] | 86 cancer survivors, mean age 31.7 FB-G.fit (45; 4M, 41F) FB-G.com (41; 4M, 37F) | Duration: 12 weeks Facebook group—fitnet Participants received a pedometer. Each week was posted a Fb message, with expanded behavioral lesson with specific guidance on PA and behavioral strategies, such as enlisting social support, incorporating PA into daily routine, self-monitoring and maintaining PA. The administrator posted various prompts including discussion question, links to videos, exercise- or cancer-related news articles, or electronic PA resources, and a weekly reminder to set an exercise goal, log daily PA. Facebook group—comparison The same intervention but without administration moderation that encourage the interaction. |
| Cavallo N et al. (2012) [37] | 134 university students, aged <25 years FB-G (67F) CG (67F) | Duration: 12 weeks Facebook group INSHAPE website, which provided educational information related to PA and a self-monitoring tool that allowed participants to set goals, track their daily PA, and view a chart depicting their progress relative to their goal and to national recommendations for PA. Control group Control group participants received access to a limited version of the INSHAPE website, which excluded self-monitoring. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duregon, F.; Bullo, V.; Di Blasio, A.; Cugusi, L.; Pizzichemi, M.; Sciusco, S.; Viscioni, G.; Cruz-Diaz, D.; Bocalini, D.S.; Bortoletto, A.; et al. The Role of Facebook® in Promoting a Physically Active Lifestyle: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 9794. https://doi.org/10.3390/ijerph19169794
Duregon F, Bullo V, Di Blasio A, Cugusi L, Pizzichemi M, Sciusco S, Viscioni G, Cruz-Diaz D, Bocalini DS, Bortoletto A, et al. The Role of Facebook® in Promoting a Physically Active Lifestyle: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(16):9794. https://doi.org/10.3390/ijerph19169794
Chicago/Turabian StyleDuregon, Federica, Valentina Bullo, Andrea Di Blasio, Lucia Cugusi, Martina Pizzichemi, Salvatore Sciusco, Gianluca Viscioni, David Cruz-Diaz, Danilo Sales Bocalini, Alessandro Bortoletto, and et al. 2022. "The Role of Facebook® in Promoting a Physically Active Lifestyle: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 16: 9794. https://doi.org/10.3390/ijerph19169794
APA StyleDuregon, F., Bullo, V., Di Blasio, A., Cugusi, L., Pizzichemi, M., Sciusco, S., Viscioni, G., Cruz-Diaz, D., Bocalini, D. S., Bortoletto, A., Favro, F., Alberton, C. L., Gobbo, S., & Bergamin, M. (2022). The Role of Facebook® in Promoting a Physically Active Lifestyle: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(16), 9794. https://doi.org/10.3390/ijerph19169794








