Injury in Children with Developmental Disorders: A 1:1 Nested Case–Control Study Using Multiple Datasets in Taiwan
Abstract
:1. Introduction
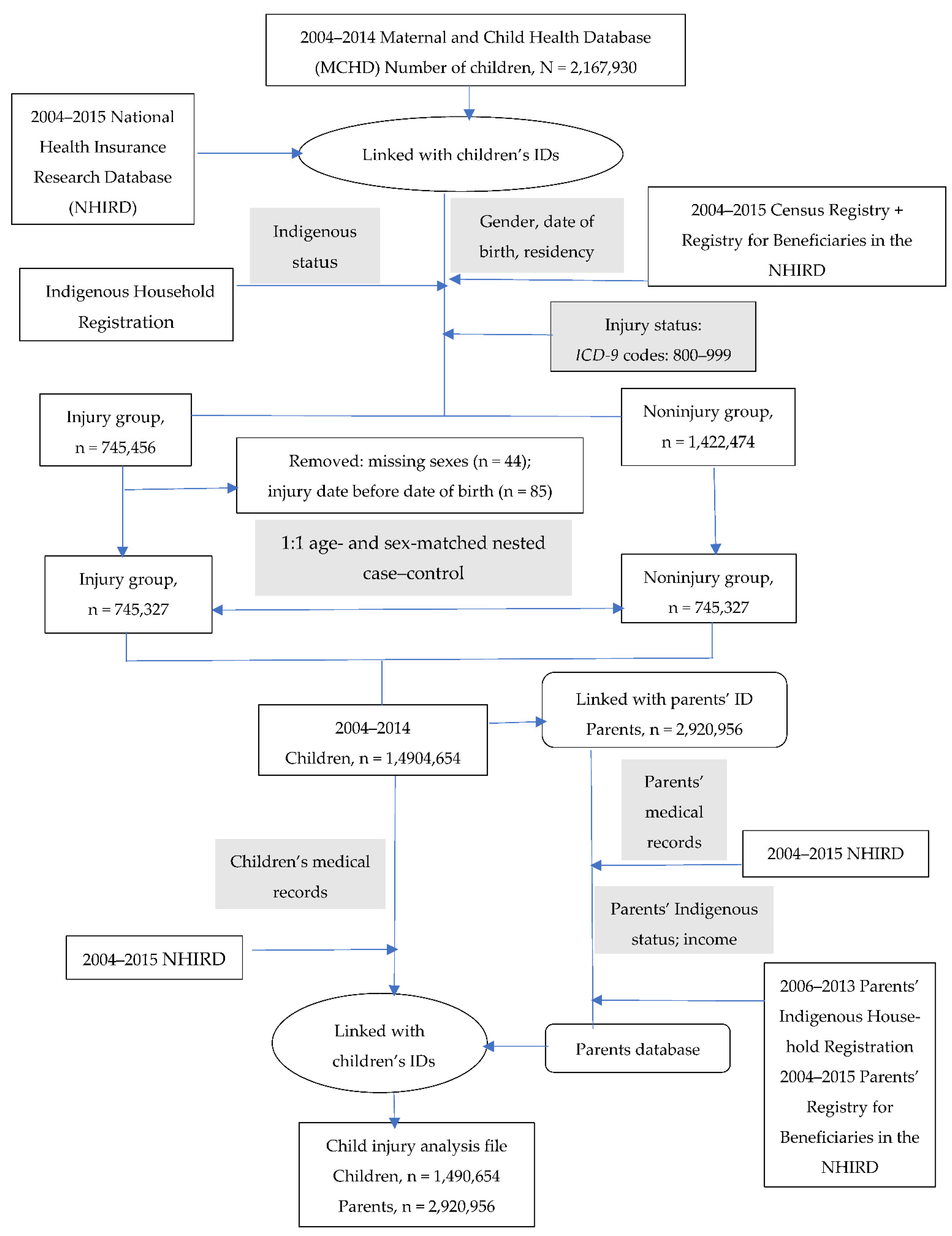
2. Materials and Methods
2.1. Study Design and Setting
2.2. Variable Definitions
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- James, S.L.; Castle, C.D.; Dingels, Z.V.; Fox, J.T.; Hamilton, E.B.; Liu, Z.; Roberts, N.L.S.; Sylte, D.O.; Henry, N.J.; LeGrand, K.E.; et al. Global injury morbidity and mortality from 1990 to 2017: Results from the Global Burden of Disease Study 2017. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2020, 26, i96–i114. [Google Scholar] [CrossRef] [PubMed]
- Adeloye, D.; Bowman, K.; Chan, K.Y.; Patel, S.; Campbell, H.; Rudan, I. Global and regional child deaths due to injuries: An assessment of the evidence. J. Glob. Health 2018, 8, 021104. [Google Scholar] [CrossRef]
- Alonge, O.; Khan, U.R.; Hyder, A.A. Our Shrinking Globe: Implications for Child Unintentional Injuries. Pediatr. Clin. N. Am. 2016, 63, 167–181. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-J.; Ko, M.H.-J.; Li, S.-T.; Chiu, N.-C.; Hung, K.-L. Prevalence of preschool children developmental disabilities in northeastern Taiwan—Screening with Taipei City Developmental Screening Checklist for Preschoolers, 2nd Version. J. Formos. Med. Assoc. Taiwan Yi Zhi 2020, 119, 1174–1179. [Google Scholar] [CrossRef] [PubMed]
- Zablotsky, B.; Black, L.I.; Maenner, M.J.; Schieve, L.A.; Danielson, M.L.; Bitsko, R.H.; Blumberg, S.J.; Kogan, M.D.; Boyle, C.A. Prevalence and Trends of Developmental Disabilities among Children in the United States: 2009–2017. Pediatrics 2019, 144, e20190811. [Google Scholar] [CrossRef]
- Leland, N.L.; Garrard, J.; Smith, D.K. Comparison of injuries to children with and without disabilities in a day-care center. J. Dev. Behav. Pediatr. 1994, 15, 402–408. [Google Scholar] [CrossRef]
- Sinclair, S.A.; Xiang, H. Injuries among US children with different types of disabilities. Am. J. Public Health 2008, 98, 1510–1516. [Google Scholar] [CrossRef]
- Xiang, H.; Stallones, L.; Chen, G.; Hostetler, S.G.; Kelleher, K. Nonfatal injuries among US children with disabling conditions. Am. J. Public Health 2005, 95, 1970–1975. [Google Scholar] [CrossRef]
- Van Den Broek, M.; Beghi, E.; Epilepsia, R.G.J. Accidents in patients with epilepsy: Types, circumstances, and complications: A European cohort study. Epilepsia 2004, 45, 667–672. [Google Scholar] [CrossRef]
- Jain, A.; Spencer, D.; Yang, W.; Kelly, J.P.; Newschaffer, C.J.; Johnson, J.; Marshall, J.; Azocar, F.; Tabb, L.P.; Dennen, T. Injuries among children with autism spectrum disorder. Acad. Pediatr. 2014, 14, 390–397. [Google Scholar] [CrossRef]
- Lee, L.C.; Harrington, R.A.; Chang, J.J.; Connors, S.L. Increased risk of injury in children with developmental disabilities. Res. Dev. Disabil. 2008, 29, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Schwebel, D.C.; Speltz, M.L.; Jones, K.; Bardina, P. Unintentional injury in preschool boys with and without early onset of disruptive behavior. J. Pediatr. Psychol. 2002, 27, 727–737. [Google Scholar] [CrossRef] [PubMed]
- Petridou, E.; Zervos, I.; Christopoulos, G.; Revinthi, K.; Papoutsakis, G.; Trichopoulos, D. Biosocial variables and auditory acuity as risk factors for non-fatal childhood injuries in Greece. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 1995, 1, 92–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raman, S.R.; Boyce, W.; Pickett, W. Injury among 1107 Canadian students with self-identified disabilities. Disabil. Rehabil. 2007, 29, 1727–1735. [Google Scholar] [CrossRef] [PubMed]
- White, D.; McPherson, L.; Lennox, N.; Ware, R.S. Injury among adolescents with intellectual disability: A prospective cohort study. Injury 2018, 49, 1091–1096. [Google Scholar] [CrossRef] [Green Version]
- De Lourdes Drachler, M.; de Carvalho Leite, J.C.; Marshall, T.; Anselmo Hess Almaleh, C.M.; Feldens, C.A.; Vitolo, M.R. Effects of the home environment on unintentional domestic injuries and related health care attendance in infants. Acta Paediatr. 2007, 96, 1169–1173. [Google Scholar] [CrossRef]
- Faelker, T.; Pickett, W.; Brison, R.J. Socioeconomic differences in childhood injury: A population based epidemiologic study in Ontario, Canada. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2000, 6, 203–208. [Google Scholar] [CrossRef]
- Hjern, A.; Ringbäck-Weitoft, G.; Andersson, R. Socio-demographic risk factors for home-type injuries in Swedish infants and toddlers. Acta Paediatr. 2001, 90, 61–68. [Google Scholar] [CrossRef]
- Laursen, B.; Nielsen, J.W. Influence of sociodemographic factors on the risk of unintentional childhood home injuries. Eur. J. Public Health 2008, 18, 366–370. [Google Scholar] [CrossRef] [Green Version]
- Nathens, A.B.; Neff, M.J.; Goss, C.H.; Maier, R.V.; Rivara, F.P. Effect of an older sibling and birth interval on the risk of childhood injury. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2000, 6, 219–222. [Google Scholar] [CrossRef] [Green Version]
- Petridou, E.; Anastasiou, A.; Katsiardanis, K.; Dessypris, N.; Spyridopoulos, T.; Trichopoulos, D. A prospective population based study of childhood injuries: The Velestino town study. Eur. J. Public Health 2005, 15, 9–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sato, N.; Hagiwara, Y.; Ishikawa, J.; Akazawa, K. Association of socioeconomic factors and the risk for unintentional injuries among children in Japan: A cross-sectional study. BMJ Open 2018, 8, e021621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weitoft, G.R.; Hjern, A.; Haglund, B.; Rosén, M. Mortality, severe morbidity, and injury in children living with single parents in Sweden: A population-based study. Lancet 2003, 361, 289–295. [Google Scholar] [CrossRef]
- Nevriana, A.; Pierce, M.; Dalman, C.; Wicks, S.; Hasselberg, M.; Hope, H.; Abel, K.M.; Kosidou, K. Association between maternal and paternal mental illness and risk of injuries in children and adolescents: Nationwide register based cohort study in Sweden. BMJ (Clin. Res. Ed.) 2020, 369, m853. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.-W. Statistics of Health Promotion 2018; Health Promotion Administraton Ministry of Health and Welfare: Taipei, Taiwan, 2018. [Google Scholar]
- Liu, C.-Y.; Hung, Y.T.; Chuang, Y.L.; Chen, Y.J.; Weng, W.S.; Liu, J.S. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar] [CrossRef]
- Osborne, J.M.; Davey, T.M.; Spinks, A.B.; McClure, R.J.; Sipe, N.; Cameron, C.M. Child injury: Does home matter? Soc. Sci. Med. 2016, 153, 250–257. [Google Scholar] [CrossRef] [Green Version]
- DiScala, C.; Lescohier, I.; Barthel, M.; Li, G. Injuries to children with attention deficit hyperactivity disorder. Pediatrics 1998, 102, 1415–1421. [Google Scholar] [CrossRef]
- Farmer, J.E.; Peterson, L. Injury risk factors in children with attention deficit hyperactivity disorder. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 1995, 14, 325–332. [Google Scholar] [CrossRef]
- Limbos, M.A.; Ramirez, M.; Park, L.S.; Peek-Asa, C.; Kraus, J.F. Injuries to the head among children enrolled in special education. Arch. Pediatr. Adolesc. Med. 2004, 158, 1057–1061. [Google Scholar] [CrossRef] [Green Version]
- Petridou, E.; Kedikoglou, S.; Andrie, E.; Farmakakis, T.; Tsiga, A.; Angelopoulos, M.; Dessypris, N.; Trichopoulos, D. Injuries among disabled children: A study from Greece. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2003, 9, 226–230. [Google Scholar] [CrossRef] [Green Version]
- Ramirez, M.; Peek-Asa, C.; Kraus, J.F. Disability and risk of school related injury. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2004, 10, 21–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sherrard, J.; Ozanne-Smith, J.; Staines, C. Prevention of unintentional injury to people with intellectual disability: A review of the evidence. J. Intellect. Disabil. Res. 2004, 48, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Pan, S.W.; Chong, H.H.; Kao, H.C. Unintentional injury mortality among indigenous communities of Taiwan: Trends from 2002 to 2013 and evaluation of a community-based intervention. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2019, 25, 26–30. [Google Scholar] [CrossRef]
- Möller, H.; Falster, K.; Ivers, R.; Jorm, L. Inequalities in unintentional injuries between indigenous and non-indigenous children: A systematic review. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2015, 21, e144–e152. [Google Scholar] [CrossRef] [PubMed]
- Ivers, R.; Clapham, K.; Senserrick, T.; Lyford, M.; Stevenson, M. Injury prevention in Australian Indigenous communities. Injury 2008, 39 (Suppl. 5), S61–S67. [Google Scholar] [CrossRef]
- Clapham, K.; Senserrick, T.; Ivers, R.; Lyford, M.; Stevenson, M. Understanding the extent and impact of Indigenous road trauma. Injury 2008, 39 (Suppl. 5), S19–S23. [Google Scholar] [CrossRef]
- Mistry, R.M.; Pasisi, L.; Chong, S.; Stewart, J.; She, R.B. Socioeconomic deprivation and burns. Burns 2010, 36, 403–408. [Google Scholar] [CrossRef]
- Saylor, K. Injuries in Aboriginal children. Paediatr. Child Health 2004, 9, 312–314. [Google Scholar] [CrossRef] [Green Version]
- Campos-Outcalt, D.; Bay, C.; Dellapena, A.; Cota, M.K. Motor vehicle crash fatalities by race/ethnicity in Arizona, 1990–1996. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2003, 9, 251–256. [Google Scholar] [CrossRef] [Green Version]
- Cercarelli, L.R.; Knuiman, M.W. Trends in road injury hospitalisation rates for Aboriginal and non-Aboriginal people in Western Australia, 1971–1997. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2002, 8, 211–215. [Google Scholar] [CrossRef] [Green Version]
- Day, G.E.; Lanier, A.P. Alaska native mortality, 1979–1998. Public Health Rep. 2003, 118, 518–530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlberg, M.M.; Shapiro-Mendoza, C.K.; Goodman, M. Maternal and infant characteristics associated with accidental suffocation and strangulation in bed in US infants. Matern. Child Health J. 2012, 16, 1594–1601. [Google Scholar] [CrossRef] [PubMed]
- Voas, R.B.; Fisher, D.A.; Tippetts, A.S. Children in fatal crashes: Driver blood alcohol concentration and demographics of child passengers and their drivers. Addiction 2002, 97, 1439–1448. [Google Scholar] [CrossRef] [PubMed]
- Arria, A.M.; Mericle, A.A.; Meyers, K.; Winters, K.C. Parental substance use impairment, parenting and substance use disorder risk. J. Subst. Abus. Treat. 2012, 43, 114–122. [Google Scholar] [CrossRef] [Green Version]
- Neger, E.N.; Prinz, R.J. Interventions to address parenting and parental substance abuse: Conceptual and methodological considerations. Clin. Psychol. Rev. 2015, 39, 71–82. [Google Scholar] [CrossRef] [Green Version]
- Wan, M.W.; Warren, K.; Salmon, M.P.; Abel, K.M. Patterns of maternal responding in postpartum mothers with schizophrenia. Infant Behav. Dev. 2008, 31, 532–538. [Google Scholar] [CrossRef]
- Paranjothy, S.; Evans, A.; Bandyopadhyay, A.; Fone, D.; Schofield, B.; John, A.; Bellis, M.A.; Lyons, R.A.; Farewell, D.; Long, S.J. Risk of emergency hospital admission in children associated with mental disorders and alcohol misuse in the household: An electronic birth cohort study. Lancet Public Health 2018, 3, e279–e288. [Google Scholar] [CrossRef]
- Kaplan, L.M.; Nayak, M.B.; Greenfield, T.K.; Karriker-Jaffe, K.J. Alcohol’s Harm to Children: Findings from the 2015 United States National Alcohol’s Harm to Others Survey. J. Pediatr. 2017, 184, 186–192. [Google Scholar] [CrossRef] [Green Version]
- Phelan, K.J.; Morrongiello, B.A.; Khoury, J.C.; Xu, Y.; Liddy, S.; Lanphear, B. Maternal supervision of children during their first 3 years of life: The influence of maternal depression and child gender. J. Pediatr. Psychol. 2014, 39, 349–357. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.; Ozegovic, D.; Voaklander, D.C. Differences in incidence of injury between rural and urban children in Canada and the USA: A systematic review. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2012, 18, 264–271. [Google Scholar] [CrossRef]
- Sharpe, A.; Hardt, J. Five Deaths a Day: Workplace Fatalities in Canada, 1993–2005; Centre for the Study of Living Standards: Ottawa, ON, Canada, 2006. [Google Scholar]
- Sleet, D.A. The Global Challenge of Child Injury Prevention. Int. J. Environ. Res. Public Health 2018, 15, 1921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Noninjury Group | Injury Group | p Value | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Variable for children | |||||
| Indigenous status | <0.0001 | ||||
| No | 721,874 | 96.9 | 713,749 | 95.8 | |
| Yes | 23,453 | 3.1 | 31,578 | 4.2 | |
| Area of residence | <0.0001 | ||||
| Highly urbanized | 148,507 | 21.1 | 142,424 | 20.3 | |
| Moderately urbanized | 209,572 | 29.8 | 208,726 | 29.7 | |
| Boomtown a | 160,377 | 22.8 | 153,078 | 21.8 | |
| Rural | 184,281 | 26.3 | 198,164 | 28.3 | |
| Development disorder b | <0.0001 | ||||
| No | 693,243 | 93.0 | 669,608 | 89.8 | |
| Yes | 52,084 | 7.0 | 75,719 | 10.2 | |
| Parental variable | |||||
| Age | <0.0001 | ||||
| 0–17 | 1455 | 0.1 | 937 | 0.0 | |
| 18–34 | 833,157 | 54.1 | 821,309 | 56.6 | |
| 35+ | 616,082 | 45.8 | 629,450 | 43.4 | |
| Income | <0.0001 | ||||
| Low | 306,804 | 21.8 | 320,093 | 22.8 | |
| Medium | 694,803 | 49.5 | 696,968 | 49.7 | |
| High | 399,755 | 28.5 | 383,161 | 27.3 | |
| Illicit drug use | <0.0001 | ||||
| No | 1,449,716 | 99.2 | 1,442,928 | 98.9 | |
| Yes | 12,103 | 0.8 | 16,209 | 1.1 | |
| Alcohol addiction | <0.0001 | ||||
| No | 1,452,832 | 99.4 | 1,446,975 | 99.2 | |
| Yes | 8987 | 0.6 | 12,162 | 0.8 | |
| Mental disorder c | <0.0001 | ||||
| No | 1,307,371 | 89.4 | 1,268,599 | 86.7 | |
| Yes | 154,448 | 10.6 | 190,538 | 13.3 | |
| AOR | 95% CI | |
|---|---|---|
| Variable for children | ||
| Indigenous status | ||
| No | ref. | |
| Yes | 1.29 * | 1.26–1.32 |
| Area of residence | ||
| Highly urbanized area | ref. | |
| Moderately urbanized area | 1.04 * | 1.03–1.05 |
| Boomtown a | 0.99 | 0.98–1.00 |
| Rural area | 1.10 * | 1.08–1.11 |
| Development disorder b | ||
| No | ref. | |
| Yes | 1.49 * | 1.47–1.51 |
| Parental variable | ||
| Age | ||
| 0–17 | 0.67 * | 0.58–0.78 |
| 18–34 | ref. | |
| 35+ | 1.06 * | 1.05–1.08 |
| Income | ||
| Low | 1.06 * | 1.05–1.07 |
| Medium | ref. | |
| High | 0.93 * | 0.92–0.94 |
| Illicit drug use | ||
| No | ref. | |
| Yes | 1.24 * | 1.16–1.32 |
| Alcohol addiction | ||
| No | ref. | |
| Yes | 1.11 * | 1.03–1.20 |
| Mental disorder c | ||
| No | ref. | |
| Yes | 1.26 * | 1.25–1.28 |
| Once (n = 988,774) | More than Once (n = 501,880) | |||
|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | |
| Variable for children | ||||
| Indigenous status | ||||
| No | ref. | ref. | ||
| Yes | 1.19 * | 1.16–1.22 | 1.51 * | 1.45–1.57 |
| Area of residence | ||||
| Highly urbanized area | ref. | ref. | ||
| Moderately urbanized area | 1.04 * | 1.02–1.05 | 1.04 * | 1.02–1.06 |
| Boomtown a | 1.00 | 0.99–1.02 | 0.96 * | 0.94–0.98 |
| Rural area | 1.08 * | 1.06–1.10 | 1.14 * | 1.11–1.17 |
| Development disorder b | ||||
| No | ref. | ref. | ||
| Yes | 1.34 * | 1.32–1.37 | 1.74 * | 1.70–1.78 |
| Parental variable | ||||
| Age | ||||
| 0–17 | 0.61 * | 0.50–0.75 | 0.73 * | 0.58–0.91 |
| 18–34 | ref. | ref. | ||
| 35+ | 1.08 * | 1.06–1.09 | 1.04 * | 1.02–1.06 |
| Income | ||||
| Low | 1.05 * | 1.03–1.06 | 1.09 * | 1.06–1.11 |
| Medium | ref. | ref. | ||
| High | 0.93 * | 0.91–0.94 | 0.95 * | 0.93–0.97 |
| Illicit drug use | ||||
| No | ref. | ref. | ||
| Yes | 1.12 * | 1.03–1.22 | 1.48 * | 1.32–1.66 |
| Alcohol addiction | ||||
| No | ref. | ref. | ||
| Yes | 1.06 | 0.97–1.17 | 1.21 * | 1.06–1.37 |
| Mental disorder c | ||||
| No | ref. | ref. | ||
| Yes | 1.18 * | 1.17–1.20 | 1.43 * | 1.41–1.46 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.-K.; Hsu, L.-M.; Chiu, N.-C.; Saleh, W.; Pai, C.-W.; Chen, P.-L. Injury in Children with Developmental Disorders: A 1:1 Nested Case–Control Study Using Multiple Datasets in Taiwan. Int. J. Environ. Res. Public Health 2022, 19, 9814. https://doi.org/10.3390/ijerph19169814
Chen S-K, Hsu L-M, Chiu N-C, Saleh W, Pai C-W, Chen P-L. Injury in Children with Developmental Disorders: A 1:1 Nested Case–Control Study Using Multiple Datasets in Taiwan. International Journal of Environmental Research and Public Health. 2022; 19(16):9814. https://doi.org/10.3390/ijerph19169814
Chicago/Turabian StyleChen, Shang-Ku, Li-Min Hsu, Nan-Chang Chiu, Wafaa Saleh, Chih-Wei Pai, and Ping-Ling Chen. 2022. "Injury in Children with Developmental Disorders: A 1:1 Nested Case–Control Study Using Multiple Datasets in Taiwan" International Journal of Environmental Research and Public Health 19, no. 16: 9814. https://doi.org/10.3390/ijerph19169814
APA StyleChen, S.-K., Hsu, L.-M., Chiu, N.-C., Saleh, W., Pai, C.-W., & Chen, P.-L. (2022). Injury in Children with Developmental Disorders: A 1:1 Nested Case–Control Study Using Multiple Datasets in Taiwan. International Journal of Environmental Research and Public Health, 19(16), 9814. https://doi.org/10.3390/ijerph19169814







