Digital Impressions in Implant Dentistry: A Literature Review
Abstract
1. Introduction
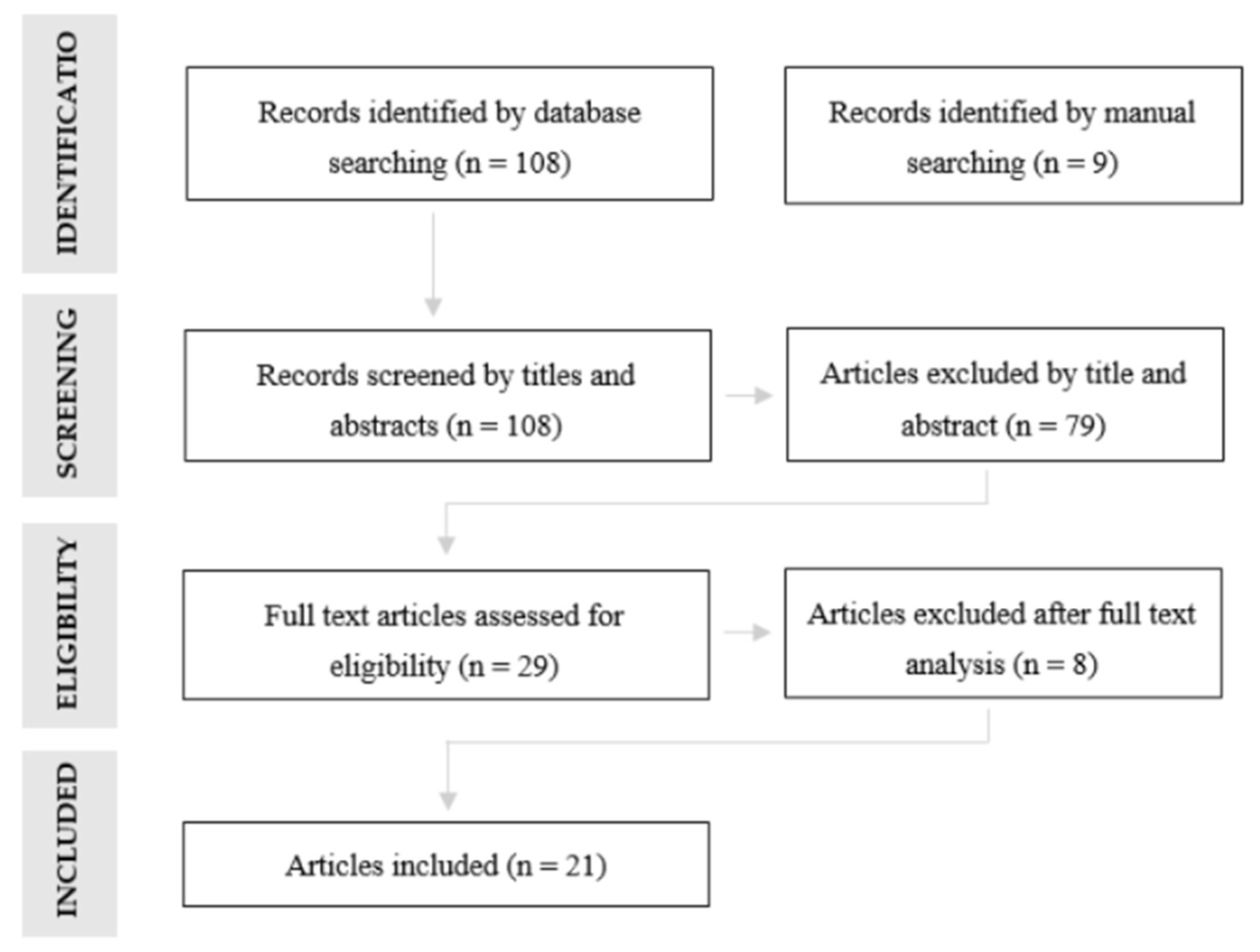
2. Materials and Methods
- From each study, the following data were extracted:
- Study design—randomized/nonrandomized controlled study, experimental study;
- Study setting—in vivo/in vitro;
- Type of impressions—digital/conventional;
- Type of arch—single-unit case, partially edentulous, completely edentulous;
- Type and number of implants placed;
- Implant depth and angulation;
- Type and design of the ISBs;
- IOS used;
- Scanning technique;
- Outcomes.
3. Results
3.1. Accuracy of Digital Impressions in Implant Dentistry
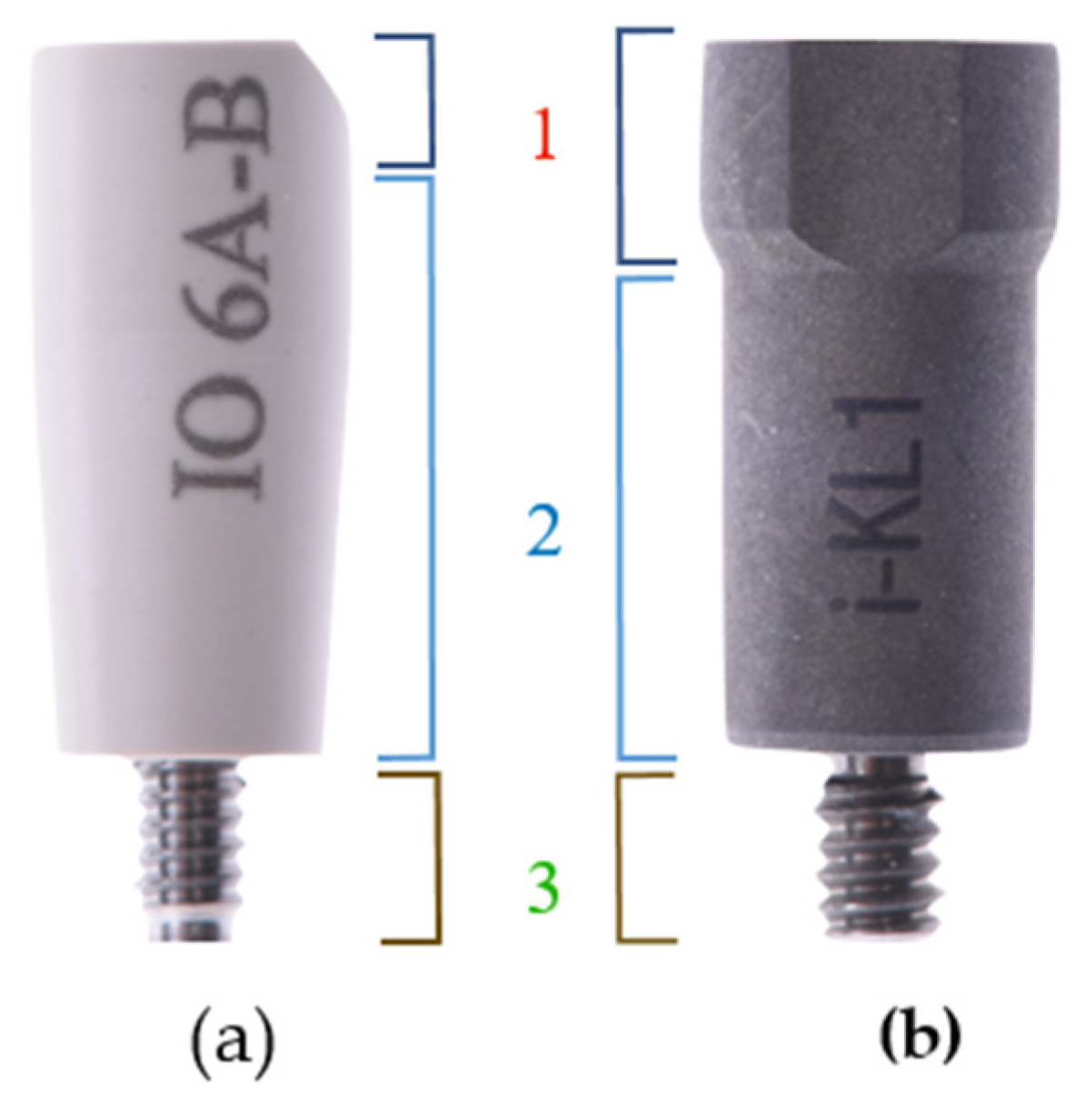
3.2. Design/Material of ISBs
3.3. Scanning Technique
3.4. Implants Angulation/Depth
3.5. Accuracy of Different IOS Devices
4. Discussion
5. Conclusions
- Evidence suggests that digital impressions are an accurate procedure in implant dentistry.
- Regardless of the IOS device used, the scanning protocol can influence the accuracy of the digital impressions.
- Implant angulation seems to have no effect on the accuracy of the digital impressions. On the other hand, implant depth may affect the accuracy of the procedure. However, clinical guidelines cannot be drawn based on the presented data.
- ISBs are implant position transfer devices that are commercialized in multiple shapes, geometries and materials.
- The design and material of ISBs may influence the accuracy of digital impressions.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Joda, T.; Wittneben, J.G.; Bragger, U. Digital implant impressions with the “Individualized Scanbody Technique” for emergence profile support. Clin. Oral Implants Res. 2014, 25, 395–397. [Google Scholar] [CrossRef]
- Stimmelmayr, M.; Guth, J.F.; Erdelt, K. Digital evaluation of the reproducibility of implant scanbody fit-an in vitro study. Clin. Oral Investig. 2012, 16, 851–856. [Google Scholar] [CrossRef]
- Logozzo, S.; Zanetti, E.M.; Franceschini, G.; Kilpela, A.; Makynen, A. Recent advances in dental optics—Part I: 3D intraoral scanners for restorative dentistry. Opt. Lasers Eng. 2014, 54, 203–221. [Google Scholar] [CrossRef]
- Zimmermann, M.; Mehl, A.; Mormann, W.H.; Reich, S. Intraoral scanning systems—A current overview. Int. J. Comput Dent. 2015, 18, 101–129. [Google Scholar] [PubMed]
- Gjelvold, B.; Chrcanovic, B.R.; Korduner, E.K.; Collin-Bagewitz, I.; Kisch, J. Intraoral Digital Impression Technique Compared to Conventional Impression Technique. A Randomized Clinical Trial. J. Prosthodont. 2016, 25, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Goracci, C.; Franchi, L.; Vichi, A.; Ferrari, M. Accuracy, reliability, and efficiency of intraoral scanners for full-arch impressions: A systematic review of the clinical evidence. Eur. J. Orthod. 2016, 38, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Guth, J.F.; Edheloff, D.; Schweiger, J.; Keul, C. A new method for the evaluation of the accuracy of full-arch digital impressions in vitro. Clin. Oral Investig. 2016, 20, 1487–1494. [Google Scholar] [CrossRef]
- Andriessen, F.S.; Rijkens, D.R.; van der Meer, W.J.; Wismeijer, D.W. Applicability and accuracy of an intraoral scanner for scanning multiple implants in edentulous mandibles: A pilot study. J. Prosthet. Dent. 2014, 111, 186–194. [Google Scholar] [CrossRef]
- Ng, J.; Ruse, D.; Wyatt, C. A comparison of the marginal fit of crowns fabricated with digital and conventional methods. J. Prosthet. Dent. 2014, 112, 555–560. [Google Scholar] [CrossRef]
- Ueda, K.; Beuer, F.; Stimmelmayr, M.; Erdelt, K.; Keul, C.; Guth, J.F. Fit of 4-unit FDPs from CoCr and zirconia after conventional and digital impressions. Clin. Oral Investig. 2016, 20, 283–289. [Google Scholar] [CrossRef]
- Abdel-Azim, T.; Rogers, K.; Elathamna, E.; Zandinejad, A.; Metz, M.; Morton, D. Comparison of the marginal fit of lithium disilicate crowns fabricated with CAD/CAM technology by using conventional impressions and two intraoral digital scanners. J. Prosthet. Dent. 2015, 114, 554–559. [Google Scholar] [CrossRef] [PubMed]
- Ahrberg, D.; Lauer, H.C.; Ahrberg, M.; Weigl, P. Evaluation of fit and efficiency of CAD/CAM fabricated all-ceramic restorations based on direct and indirect digitalization: A double-blinded, randomized clinical trial. Clin. Oral Investig. 2016, 20, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Pradies, G.; Zarauz, C.; Valverde, A.; Ferreiroa, A.; Martinez-Rus, F. Clinical evaluation comparing the fit of all-ceramic crowns obtained from silicone and digital intraoral impressions based on wavefront sampling technology. J. Dent. 2015, 43, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Zarauz, C.; Valverde, A.; Martinez-Rus, F.; Hassan, B.; Pradies, G. Clinical evaluation comparing the fit of all-ceramic crowns obtained from silicone and digital intraoral impressions. Clin. Oral Investig. 2016, 20, 799–806. [Google Scholar] [CrossRef]
- Joda, T.; Bragger, U. Digital vs. conventional implant prosthetic workflows: A cost/time analysis. Clin. Oral Implants Res. 2015, 26, 1430–1435. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Bragger, U. Complete digital workflow for the production of implant-supported single-unit monolithic crowns. Clin. Oral Implants Res. 2014, 25, 1304–1306. [Google Scholar] [CrossRef]
- Schaefer, O.; Decker, M.; Wittstock, F.; Kuepper, H.; Guentsch, A. Impact of digital impression techniques on the adaption of ceramic partial crowns in vitro. J. Dent. 2014, 42, 677–683. [Google Scholar] [CrossRef]
- Giménez, B.; Özcan, M.; Martínez-Rus, F.; Pradíes, G. Accuracy of a digital impression system based on active wavefront sampling technology for implants considering operator experience, implant angulation, and depth. Clin. Implant. Dent. Relat. Res. 2015, 17, 54–64. [Google Scholar] [CrossRef]
- van der Meer, W.J.; Andriessen, F.S.; Wismeijer, D.; Ren, Y. Application of intra-oral dental scanners in the digital workflow of implantology. PLoS ONE 2012, 7, 4331–4332. [Google Scholar] [CrossRef]
- Ender, A.; Attin, T.; Mehl, A. In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J. Prosthet. Dent. 2016, 115, 313–320. [Google Scholar] [CrossRef]
- Ender, A.; Zimmermann, M.; Attin, T.; Mehl, A. In vivo precision of conventional and digital methods for obtaining quadrant dental impressions. Clin. Oral Investig. 2016, 20, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Guth, J.F.; Keul, C.; Stimmelmayr, M.; Beuer, F.; Edelhoff, D. Accuracy of digital models obtained by direct and indirect data capturing. Clin. Oral Investig. 2013, 17, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Gimenez-Gonzalez, B.; Hassan, B.; Özcan, M.; Pradíes, G. An In Vitro Study of Factors Influencing the Performance of Digital Intraoral Impressions Operating on Active Wavefront Sampling Technology with Multiple Implants in the Edentulous Maxilla. J. Prosthodont. 2016, 26, 650–655. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Veronesi, G. Digital versus Analog Procedures for the Prosthetic Restoration of Single Implants: A Randomized Controlled Trial with 1 Year of Follow-Up. Biomed Res Int. 2018, 2018, 5325032. [Google Scholar] [CrossRef] [PubMed]
- Imburgia, M.; Logozzo, S.; Hauschild, U.; Veronesi, G.; Mangano, C.; Mangano, F.G. Accuracy of four intraoral scanners in oral implantology: A comparative in vitro study. BMC Oral Health 2017, 17, 92. [Google Scholar] [CrossRef] [PubMed]
- Marti, A.M.; Harris, B.T.; Metz, M.J.; Morton, D.; Scarfe, W.C.; Metz, C.J. Comparison of digital scanning and polyvinyl siloxane impression techniques by dental students: Instructional efficiency and attitudes towards technology. Eur. J. Dent. Educ. 2017, 21, 200–205. [Google Scholar] [CrossRef]
- Mandelli, F.; Ferrini, F.; Gastaldi, G.; Gherlone, E.; Ferrari, M. Improvement of a Digital Impression with Conventional Materials: Overcoming Intraoral Scanner Limitations. Int. J. Prosthodont. 2017, 30, 373–376. [Google Scholar] [CrossRef]
- Martin, C.B.; Chalmers, E.V.; McIntyre, G.T.; Cochrane, H.; Mossey, P.A. Orthodontic scanners: What’s available? J. Orthod. 2015, 42, 136–143. [Google Scholar] [CrossRef]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral scanners in dentistry: A review of the current literature. BMC Oral Health 2017, 17, 149. [Google Scholar] [CrossRef]
- Abduo, J.; Elseyoufi, M. Accuracy of Intraoral Scanners: A Systematic Review of Influencing Factors. Eur. J. Prost. Rest. Dent. 2018, 26, 101–121. [Google Scholar]
- Flügge, T.; Att, W.; Metzger, M.; Nelson, K. Precision of Dental Implant Digitization Using Intraoral Scanners. Int. J. Prosthodont. 2016, 29, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Papaspyridakos, P.; Gallucci, G.O.; Chen, C.J.; Hanssen, S.; Naert, I.; Vandenberghe, B. Digital versus conventional implant impressions for edentulous patients: Accuracy outcomes. Clin. Oral Implants Res. 2016, 27, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Gherlone, E.; Capparè, P.; Vinci, R.; Ferrini, F.; Gastaldi, G.; Crespi, R. Conventional Versus Digital Impressions for “All-on-Four” Restorations. Int. J. Oral Maxillofac. Implants 2016, 31, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, R.; Yilmaz, B. Intraoral scan bodies in implant dentistry: A systematic review. J. Prost. Dent. 2018, 120, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Del Corso, M.; Abà, G.; Vasquez, L.; Dargaud, J.; Ehrenfest, D.M.D. Optical Three-Dimensional Scanning Acquisition of the Position of Osseointegrated Implants: An in vitro Study to Determine Method Accuracy and Operational Feasibility. Clin. Implant Dent. Relat. Res. 2009, 11, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Papaspyridakos, P.; Benic, G.I.; Hogsett, V.L.; White, G.S.; Lal, K.; Galucci, G.O. Accuracy of implant casts generated with splinted and non-splinted impression techniques for edentulous patients: An optical scanning study. Clin. Oral Implants Res. 2012, 23, 676–681. [Google Scholar] [CrossRef]
- Patzelt, S.; Vonau, S.; Stampf, S.; Att, W. Assessing the feasibility and accuracy of digitizing edentulous jaws. J. Am. Dent. Assoc. 2013, 144, 914–920. [Google Scholar] [CrossRef]
- Lee, S.J.; Betensky, R.A.; Gianneschi, G.E.; Galucci, G.O. Accuracy of digital versus conventional implant impressions. Clin. Oral Implants Res. 2015, 26, 715–719. [Google Scholar] [CrossRef]
- Amin, S.; Weber, H.P.; Finkelman, M.; El Rafie, K.; Kudara, Y.; Papaspyridakos, P. Digital vs. conventional full-arch implant impressions: A comparative study. Clin. Oral Implants Res. 2016, 28, 1360–1367. [Google Scholar] [CrossRef]
- Fluegge, T.; Att, W.; Metzger, M.; Nelson, K. A Novel Method to Evaluate Precision of Optical Implant Impressions with Commercial Scan Bodies—An Experimental Approach. J. Prosthodont. 2017, 26, 34–41. [Google Scholar] [CrossRef]
- Menini, M.; Setti, P.; Pera, F.; Pera, P.; Pesce, P. Accuracy of multi-unit implant impression: Traditional techniques versus a digital procedure. Clin. Oral Investig. 2017, 22, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Vandeweghe, S.; Vervack, V.; Dierens, M.; De Bruyn, H. Accuracy of digital impressions of multiple dental implants: An in vitro study. Clin. Oral Implants Res. 2017, 28, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Ciocca, L.; Meneghello, R.; Monaco, C.; Savio, G.; Scheda, L.; Gatto, M.R.; Baldissara, P. In vitro assessment of the accuracy of digital impressions prepared using a single system for full-arch restorations on implants. Int. J. Comput. Assist. Radiol. Surg. 2018, 13, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, P.; Herrero-Climent, M.; Díaz-Castro, C.; Ríos-Santos, J.V.; Padrós, R.; Mur, J.G.; Falcão, C. Accuracy of Implant Casts Generated with Conventional and Digital Impressions—An In Vitro Study. Int. J. Environ. Res. Public Health 2018, 15, 1599. [Google Scholar] [CrossRef] [PubMed]
- Gedrimiene, A.; Adaskevicius, R.; Rutkunas, V. Accuracy of digital and conventional dental implant impressions for fixed partial dentures: A comparative clinical study. J. Adv. Prosthodont. 2019, 11, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Arcuri, L.; Pozzi, A.; Lio, F.; Rompen, E.; Zechner, W.; Nardi, A. Influence of implant scanbody material, position and operator on the accuracy of digital impression for complete-arch: A randomized in vitro trial. J. Prosthodont. Res. 2020, 64, 128–136. [Google Scholar] [CrossRef]
- Mizumoto, R.M.; Yilmaz, B.; McGlumphy, E.A.; Seidt, J.; Johnston, W.M. Accuracy of different digital scanning techniques and scan bodies for complete-arch implant-supported prostheses. J. Prosthet. Dent. 2020, 123, 96–104. [Google Scholar] [CrossRef]
- Motel, C.; Kirchner, E.; Adler, W.; Whichman, M.; Matta, R.E. Impact of Different Scan Bodies and Scan Strategies on the Accuracy of Digital Implant Impressions Assessed with an Intraoral Scanner: An In Vitro Study. J. Prosthodont. 2020, 29, 309–314. [Google Scholar] [CrossRef]
- Revilla-León, M.; Fogarty, R.; Barrington, J.J.; Zandinejad, A.; Özcan, M. Influence of scan body design and digital implant analogs on implant replica position in additively manufactured casts. J. Prosthet. Dent. 2020, 124, 202–210. [Google Scholar] [CrossRef]
| Study Design | Number of Studies |
|---|---|
| Nonrandomized clinical trial | 2 |
| Randomized experimental study | 1 |
| Experimental study | 18 |
| Study Design | Number of Studies |
|---|---|
| In vivo | 2 |
| In vitro | 19 |
| Author/Year | Accuracy of Digital Impressions in Implant Dentistry | Design/Material of the ISBs | Scanning Technique | Implants Angulation/Depth | Accuracy of Different IOS Devices |
|---|---|---|---|---|---|
| Del Corso et al., 2009 [35] | X | ||||
| Papaspyridakos et al., 2012 [36] | X | X | |||
| Van der Meer et al., 2012 [19] | X | X | X | ||
| Patzelt et al., 2013 [37] | X | X | |||
| Andriessen et al., 2014 [8] | X | ||||
| Lee et al., 2015 [38] | X | ||||
| Amin et al., 2016 [39] | X | X | X | ||
| Flugge et al., 2016 [31] | X | X | X | ||
| Giménez-González et al., 2016 [23] | X | X | X | ||
| Papaspyridakos et al., 2016 [32] | X | X | |||
| Fluegge et al., 2017 [40] | X | X | |||
| Imburgia et al., 2017 [25] | X | X | |||
| Menini et al., 2017 [41] | X | ||||
| Vandweghe et al., 2017 [42] | X | X | |||
| Ciocca et al., 2018 [43] | X | ||||
| Ribeiro et al., 2018 [44] | X | X | |||
| Gedrimieni et al., 2019 [45] | X | X | |||
| Arcuri et al., 2020 [46] | X | X | X | ||
| Mizumoto et al., 2020 [47] | X | X | X | ||
| Motel et al., 2020 [48] | X | X | X | X | |
| Revilla-León et al., 2020 [49] | X | X |
| Author/Year | Study Setting | Type of Arch | Number of Implants | Implant System | Angulation of Implants | Depth of Implants | IOS Device |
|---|---|---|---|---|---|---|---|
| Del Corso et al., 2009 [35] | In vitro | Edentulous | 5 | 3i Implant Innovations | Not reported | Not reported | Comet VZ250 (Steinbichler Optotechnik GmbH, Germany) |
| Papaspyridakos et al., 2012 [36] | In vitro | Edentulous | 6 | Not reported | Not reported | Not reported | - |
| Van der Meer et al., 2012 [19] | In vitro | Partially Edentulous | 3 | Not reported | Not reported | Not reported | -CEREC Bluecam (Sirona, Germany) -iTero (Cadent, CA, USA)-Lava COS (3M, USA) |
| Patzelt et al., 2013 [37] | In vitro | Edentulous | 0 | - | - | - | -CEREC Bluecam (Sirona, Germany)-LavaCOS (3M, USA) -iTero (Cadent, CA, USA) -ZFX Intrascan (Zimmer, Dachau, Germany) |
| Andriessen et al., 2014 [8] | In vivo | Edentulous | 2 | Strauman Standard SLA-active | Not reported | Not reported | iTero (Cadent, CA, USA |
| Lee et al., 2015 [38] | In vitro | Partially Edentulous | 1 | Strauman BL | Not reported | Not reported | iTero (Cadent, CA, USA |
| Amin et al., 2016 [39] | In vitro | Edentulous | 5 | Strauman BL | Median 3 implants; 0° Distal left implant:10° distal Distal right implant: 15° | Not reported | -CEREC Omnicam (Sirona, Germany) -True Definition (3M, USA) |
| Flugge et al., 2016 [31] | In vitro | Partially Edentulous | 2 and 5 | BL and TL | Not reported | Not reported | -iTero (Cadent, CA, USA)-Trios (3Shape, Denmark)-True Definition (3M, USA) |
| Giménez-González et al., 2016 [23] | In vitro | Edentulous | 6 | Certain implants Biomet 3i | #2 #4 #7 #15: 0° #4 #13: 30° | #2 #4 #13 #15: 0 mm #7: 4 mm #10: 2 mm | True Definition (3M, USA) |
| Papaspyridakos et al., 2016 [32] | In vitro | Edentulous | 5 | Strauman BL | Median 3 implants: 0° Distal left implant: 10° Distal right implant:15° | Not reported | Trios (3Shape, Denmark) |
| Fluegge et al., 2017 [40] | In vitro | Partially Edentulous | 2 | S1 Camlog | Not reported | Not reported | - |
| Imburgia et al., 2017 [25] | In vitro | Edentulous and Partially Edentulous | 3 and 6 | BT Safe Int ®, BTK- Biotec Implants | 0° | Not reported | -CS3600 (Carestream, USA)-Trios3 (3Shape, Denmark) -CEREC Omnicam (Sirona Germany) -True Definition (3M, USA) |
| Menini et al., 2017 [41] | In vitro | Edentulous | 4 | Biomet 3i | Not reported | Not reported | True Definition (3M, USA) |
| Vandweghe et al., 2017 [42] | In vitro | Edentulous | 6 | IBT, Southern Implants | #46-44: 0,57° ° #44-42: 1,65° #42-32: 4,62° #32-34: 4,79 #34-36: 4,22° | Not reported | -Lava COS (3M, USA) -True Definition (3M, USA) -CEREC Omnicam (Sirona, Germany) -Trios (3Shape, Denmark) |
| Ciocca et al., 2018 [43] | In vitro | Edentulous | 6 | Premium Kohno, Sweden and Martina | Not reported | Not reported | True Definition (3M, USA) |
| Ribeiro et al., 2018 [44] | In vitro | Edentulous | 4 | Klockner KL RP implants | Model 1: 0° Model 2: divergence angle of 15° between the more distal implants and convergence angle of 15° between the two central implants | Model 1: 0 mm Model 2: 0 mm | True Definition (3M, USA) |
| Gedrimieni et al., 2019 [45] | In vivo | Partially Edentulous | 2 | AnyOne Megagen | 10° | Not reported | Trios (3Shape, Denmark) |
| Arcuri et al., 2020 [46] | In vitro | Edentulous | 6 | Not reported | #16: 0° #14: 25° distal #12 #22: 0° #24: 20° distal #26: 20° distal 20° facial | #16: 6 mm #14: 3 mm #12 #22 #24: 0 mm #26: 2 0 mm | Trios (3Shape, Denmark) |
| Mizumoto et al., 2020 [47] | In vitro | Edentulous | 4 | TSV Zimmer Biomet | 0° | 3 mm | Trios (3Shape, Denmark) |
| Motel et al., 2020 [48] | In vitro | Edentulous | 3 | Nobelreplace Select implants, Nobel Biocare | Mesial Implant: 15° vestibular Central and Distal implant: 0° | Not reported | Trios (3Shape, Denmark) |
| Revilla-León et al., 2020 [49] | In vitro | Partially Edentulous | 3 | RP Branemark system; Nobel Biocare | 0° | Not reported | - |
| Author/Year | ISB Type | ISB Design | ISB Material | Reference Method | Superimposition Software |
|---|---|---|---|---|---|
| Del Corso et al., 2009 [35] | Prototypes | Reference markers were assembled on a stainless steel-type AISI-310 base referencing the implant position | Ceramic | CMM | - |
| Papaspyridakos et al., 2012 [36] | Not reported | Cylindrical with 5 mm diameter and 15 mm height | Metallic (inox) | Scan D101 (Imetric 3D Switzerland) | Imetric, Courgenay, Switzerland |
| Van der Meer et al., 2012 [19] | Createch Medical (Createch Medical, Spain) | Cylindrical | PEEK | Leitz PMM 12106 | Rapidform, INUS Technology Inc, Seoul, Korea |
| Patzelt et al., 2013 [37] | - | - | - | Activity 101 (Smart Optics, Germany) | (Geomagic Qualify 12, 3D Systems, Rock Hill, SC, USA) |
| Andriessen et al., 2014 [8] | Regular Neck scan abutment (Straumann, Switzerland) | Not reported | Not reported | Lava Scan ST (3M, Germany) | (Geomagic Qualify 12, 3D Systems, Rock Hill, SC, USA) |
| Lee et al., 2015 [38] | Regular Neck scan abutment (Straumann, Switzerland) | Not reported | Not reported | Lava Scan ST (3M, Germany) | (Geomagic Qualify 12, 3D Systems, Rock Hill, SC, USA) |
| Amin et al., 2016 [39] | RC (Straumann, Switzerland) | Flat and cylindrical with a partially beveled upper part | Polymer | Activity 880 (Smart Optics, Germany) | (Geomagic Qualify 12, 3D Systems, Rock Hill, SC, USA) |
| Flugge et al., 2016 [31] | Not reported | Model 1: 1 TL scanbody H: 10 mm, ∅: 5 mm and BL scanbody H: 9 mm, ∅: 4 mm Model 2: 5 TL scanbody H: 10 mm, ∅: 5 mm | Not reported | D250 (3Shape, Denmark) | Rapidform, INUS Technology Inc, Seoul, Korea |
| Giménez-González et al., 2016 [23] | Prototypes | Cylindrical with 8 mm height | PEEK | CMM | (Geomagic Qualify 12, 3D Systems, Rock Hill, SC, USA) |
| Papaspyridakos et al., 2016 [32] | RC (Straumann, Switzerland) | Flat and cylindrical with a partially beveled upper part | Polymer | IScan D103i (Imetric, Switzerland | Mimics (Materialise, Belgium) |
| Fluegge et al., 2017 [40] | -23: (REF K2600.3810) -25: (REF K2600.4310) -35: (REF 048.168)-36: (REF 025.4915) | -23/25: Height of 10 mm and a diameter of 4.3 mm (23/25) -35: Height of 10 mm and a diameter of 5 mm -36: Height of 9 mm and a diameter of 4 mm | Not reported | D250 (3Shape, Denmark) | Rapidform (Rapidform, Korea) |
| Imburgia et al., 2017 [25] | BT Scanbodies®, BTK-Biotec Implants, Italy | Cylindrical | PEEK | ScanRider (Italy) | (Geomagic Qualify 12, 3D Systems, Rock Hill, SC, USA) |
| Menini et al., 2017 [41] | Createch Medical (Createch Medical, Spain) | Height of 8 mm and a diameter of 4 mm | PEEK | CMM | Rapidform (Rapidform, Korea) |
| Vandweghe et al., 2017 [42] | Proscan, Zonhoven, Belgium | Cylindrical shape with an axial incision | PEEK | IScan D104i (Imetric, Switzerland) | (Geomagic Qualify 12, 3D Systems, Rock Hill, SC, USA) |
| Ciocca et al., 2018 [43] | Sweden and Martina | 8–10 mm height | Not reported | OCMM (SmartScope Flash CNC 300; Optical Gaging Products, Rochester, NY, USA)-error (MPE) < 3.5 μm | Rhinoceros (Rhinoceros 5.0; USA) |
| Ribeiro et al., 2018 [44] | Not reported | Not reported | Titanium | IScan D104i (Imetric, Switzerland) | (Geomagic Qualify 12, 3D Systems, Rock Hill, SC, USA) |
| Gedrimieni et al., 2019 [45] | 3 shape | Flat and cylindrical with a partially beveled upper part | Not reported | D800 (3Shape, Denmark) | Rapidform (Rapidform, Korea) |
| Arcuri et al., 2020 [46] | Prototypes | Cylindrical shape with an axial Incision; 4.1mm diameter, height 9 mm; ± 0.01mm tolerance | PEEK Titanium Hybrids (PEEK body and Ti base) | ATOS Compact Scan 5M (GOM GmbH, Germany) | Parametric measurement software (Gom Inspect Professional, GOM GmbH, Germany) |
| Mizumoto et al., 2020 [47] | 1. AF (IO-Flo; Dentsply Sirona) 2. NT (Nt-Trading GmbH & CoKG 3. DE (DESS-USA) 4. C3D (Core3Dcentres) 5. ZI (Zimmer Biomet Dental) | 1. Flat cylinder with ball top. 2. Rectangular 3. Cylinder with triangular region. 4. Tapered flat cylinder 5. Flat cylinder | 1. PEEK/Metal (base) 2. PEEK/Metal 3. PEEK/PEEK 4. PEEK/Ti 5. PEEK/PEEK | COMET L3D (Carl Zeiss Optotechnik GmbH) | Industrial metrology software program (Polyworks; InnovMetric Software Inc) |
| Motel et al., 2020 [48] | 1. Elos A/S 2. NT-trading, GmbH 3.TeamZiereis, GmbH. | 1. The body of the ISB presents a flat and cylindrical shape. The scan region presents a partially beveled segment. 2. The ISB presents an asymmetrical shape with bulges and indentations. The body of the ISB is cylindrical and the scan region is light. 3. The ISB presents a cylindrical shape with one retraction each and a slightly enlarged diameter in the scan region. ISB 3 presents an intermediate shape between ISB 1 and ISB 2. | 1. Titanium / PEEK 2. PEEK/Metal 3. PEEK | ATOS So4 II (GOM GmbH, Germany) | ATOS Professional Software (V7.5 SR2, GOM GmbH, Germany) |
| Revilla-León et al., 2020 [49] | 1. Elos Medtech 2. Nt-Trading 3. Dynamic Abutment | 1. Cylinder with angled flat surface, one-piece screw-retained ISB geometry 2. One-piece screw-retained ISB geometry 3. Two-piece screw-retained/ magnet-retained ISB geometry | 1. Titanium base, PEEK 2. Titanium base, PEEK 3. PEEK | E3 scanner (3 Shape, Denmark) and CMM | Geomagic Qualify 12.0 (Geomagic, USA) |
| Author/Year | Scanning Technique | Outcomes |
|---|---|---|
| Del Corso et al., 2009 [35] | Not reported | Regarding the accuracy, it appears that 3D scanning technologies are valid options for conventional impressions techniques. Nevertheless, the bias levels presented in this study need confirmation in a clinical trial. |
| Papaspyridakos et al., 2012 [36] | - | When comparing splinted and non-splinted impression techniques in edentulous patients, the first one shows better accuracy results. The positioning of the implant in the dental arch affected the accuracy of the impressions. Considering the implant system used (external connection), a 3D misfit ranging from 59 to 72 mm is considered as the highest discrepancy in order to obtain an acceptable clinical fit with one-piece implant fixed complete dental prosthesis. |
| Van der Meer et al., 2012 [19] | Attending to the scanning of implant locators, the IOS manufacturers were asked about the high-accuracy scanning protocol, as well as special recommendations or technique modifications, considering the clinical situation on the stand. iTero and CEREC had only one recommended scanning technique for all cases and did not make a distinction between normal scanning and high-accuracy scanning. Lava COS presented a high-accuracy scanning protocol and subsequent calibration protocol. When scanning implant abutments, the LAVA COS high-accuracy scanning technique consists of a calibration with a small calibration block before beginning the intraoral scan, followed by a slow zig-zag scanning of the dental arch. Then, the calibration block is once again performed. The calibration measurements are used to calculate and compensate for deviations that might occur during the scanning procedure. | Lava COS performance with a high-accuracy scanning technique obtained the lowest and most consistent errors of all 3 IOS devices when considering the mean distance errors in full arch impressions. The increased distance and/or angular errors over the length of the dental arch can be explained by the accumulation of errors of the patched tridimensional areas, but the rebounds were not statistically significant. |
| Patzelt et al., 2013 [37] | The scanning protocol started at the distobuccal surfaces, following the crest to the opposite surface and finally completing the palatal gaps by rolling the scanner tip in a zig-zag trajectory over the palate. On the mandibular area, the scanner tip was used in a zig-zag trajectory, initiating at the distal area of one surface and following the jaw crest to the antagonist surface. | The digitization of edentulous mandible models was feasible with the use of four IOS devices. The high levels of inaccuracy lead to the conclusion that enhancements are needed before the clinical recommendation of the use of these scanners for the digitization of edentulous jaws in vivo. |
| Andriessen et al., 2014 [8] | Not reported | Considering the intra-oral scans obtained of the edentulous mandibles, it was not possible to produce well-fitting frameworks on implants, because the distance and angulation errors were too significant. The lack of anatomic landmarks for scanning seem to be the reason for these unreliable results. |
| Lee et al., 2015 [38] | Not reported | Milled models obtained from the digital impression with IOS can be compared to gypsum models obtained from the conventional impression in most anatomical areas. However, in areas such as grooves and fossae, conventional models presented a more thorough and detailed anatomy. Vertical displacements of implant position from both groups were statistically significantly different from the reference model. |
| Amin et al., 2016 [39] | The scanning protocol was initiated at the right retromolar pad, performing a continuous scanning movement through the occlusal surface until the left retromolar pad. The IOS tip was placed again at the right retromolar pad, performing a continuous scanning movement through the buccal surface until the left retromolar pad. The same procedure was used to capture the lingual surface. Voids and gap areas were re-scanned in the end by using the right retromolar pad as reference. | True Definition and Omnicam provided significantly more accurate impressions than the conventional techniques, on full arch implant impressions. True Definition presented significantly less tridimensional deviations than Omnicam. |
| Flugge et al., 2016 [31] | Following the manufacturer’s recommendation. | The scanning precision of IOSs is significantly different among the different tested devices. The precision of the IOS systems decreased with an increasing distance between ISBs, whereas the precision of the extraoral reference scanner was not influenced by the distance between ISBs. |
| Giménez-González et al., 2016 [23] | The scanning protocol was performed according to the manufacturer, using the IOS camera parallel to the gum. Scanning protocol started at mesial #15, describing a circular movement around ISB #15, and kept on scanning the gingiva surrounding all the ISB (using the same circular trajectory), until digitizing the full anterior span between #10 and #7. The IOS camera was then moved back to the previous scan data near ISB #10, performing a 180° turn of the IOS tip toward the other quadrant. The same scan technique around the contralateral ISB was used. At the end, each of the ISB was captured through tilting the camera and designing a circle around the ISB body region. | The portion of visible ISB influences the final accuracy of the digital impression, so when the implants are placed more deeply, longer ISBs are recommended. The experience of the operator may influence the accuracy of the digital impression, as well as the individual ability to follow a specific scan protocol. Since the distance and angular deviations were increased throughout the arch, it is advisable to start scanning the area of the arch where the restoration is needed, in the case of partial restorations. The angulation of the implants did not influence the accuracy of the digital impressions. |
| Papaspyridakos et al., 2016 [32] | Following the manufacturer’s recommendation. | On edentulous patients, the accuracy of digital impressions and conventional impressions using splinted technique was similar, and both achieved better results than conventional impressions using the non-splinted technique. The accuracy of implant impressions is not influenced by the implant angulation up to 15° for completely edentulous patients. |
| Fluegge et al., 2017 [40] | Not reported | The precision of extraoral scanning of ISBs is influenced by the ISB surface design and geometry and by the distance between ISBs, but not by the detachment and repositioning of the ISBs. |
| Imburgia et al., 2017 [25] | For every IOS device, the scanning protocol comprised a zig-zag trajectory: starting from the first quadrant, the tip of the IOS draws an arch movement, from vestibular to palatal and back, slowly moving forward, passing over the occlusal surface. | Significant differences in trueness were found among different IOSs, but no significant differences in precision were found. CS3600 had the best trueness results. Nevertheless, Trios 3 had better results in the transition from the partially to the fully edentulous model. Scanning a fully edentulous jaw remains more difficult than scanning an area of more limited extent. |
| Menini et al., 2017 [41] | The scanning protocol started from #26 and a first overall scan was performed in a continuous movement around all the ISBs, reaching #16. Then, another scan of each ISB was accomplished, making a circular movement. Voids and gap areas were re-scanned in the end. The entire scanning process had to be concluded in less than seven minutes. | IOS is a reliable alternative to conventional impression materials for the fabrication of full-arch implant-support prosthesis, providing an acceptable passive fit. |
| Vandweghe et al., 2017 [42] | Following the manufacturer’s recommendation | There was a significant difference in accuracy between the different IOS devices. Lava COS demonstrated the highest deviations for trueness and precision and performed significantly worse compared to the other IOS. |
| Ciocca et al., 2018 [43] | During the entire scanning procedure, the camera tip was placed parallel to the gingiva, following the dental arch. The scanning protocol started from position #46, performing circular movements around each ISB towards position #36. All the gaps were improved, making a scan back to the position #46. | Operator skill and experience did not affect the accuracy of digital impressions. The mean 3D position error of the digital impression was 0.041 ± 0.023 mm to 0.082 ± 0.030 mm, suggesting an acceptable accuracy result. Regardless of the scanning technique, the distance between ISBs influenced the magnitude of the error. Errors increased with an increasing length of scan within the arch. |
| Ribeiro et al., 2018 [44] | Following the manufacturer’s recommendation. | The deviations found in the digital impressions group were smaller than those related to conventional impressions, when using parallel implants. The same cannot be stated for angled implants, where the results between groups were similar. |
| Gedrimieni et al., 2019 [45] | On the maxilla, the scanning protocol initiated on the occlusal surface, moving then towards the buccal and palatal surfaces. On the mandible, the occlusal surfaces were scanned first. Thereafter, scanning of the lingual and buccal surfaces was performed. | The angulation between implants affected the positioning of the ISBs and the accuracy of digital impressions. |
| Arcuri et al., 2020 [46] | Followed manufacturer recommendations. From #26 to #16, the scanning protocol had as its starting point the occlusal–palatal ISB surface, maintaining an approximate 45° inclination of the IOS tip and performing a wave movement in the anterior area, in order to avoid image splitting. The buccal area and any other gaps were re-scanned thereafter. | Considering the ISB material, the accuracy performed better as follows: PEEK > Ti > PEEK + Ti. Angulation of the implants decreases the accuracy of digital impressions. Depth of the implant seems to have no influence on the accuracy of digital impressions. |
| Mizumoto et al., 2020 [47] | A standardized scan path was used according to the manufacturer’s recommendation, which consisted of scanning the occlusal surface, then the buccal surface, and then the palatal surface. 1. Unmodified master model (NO). 2. Glass fiduciary markers placed on the edentulous ridge (GB). 3. Pressure-indicating paste brushed over the ridge and palate (PP). 4. Floss tied between the scan bodies (FL). | The accuracy of full-arch digital implant impressions using ISBs was affected by both the ISB and scan protocol when using one specific IOS system. The ZI scan body had significantly less distance deviation, whereas splinting ISBs with floss led to significantly more distance deviation. Scan techniques with different surface modifications resulted in similar distance deviations to the technique without any modifications. The use of different ISBs led to significant differences in scan time. |
| Motel et al., 2020 [48] | Strategy A was a one-step procedure that included both the titanium master model and the integrated scan bodies. Strategy B comprised two steps. First, a digital overlay was performed with a scan of the titanium master model without integrated scan bodies. A second scan was performed with the titanium master model and integrated scan bodies. | The quality of digital intraoral impressions seems to be influenced by both the geometry of the scan body and the scan strategy. For clinical practice, the one-step scan strategy seems beneficial. The high accuracy in the use of 3Shape’s ISB leads to a corresponding clinical recommendation. |
| Revilla-León et al., 2020 [49] | - | The lower overall tridimensional discrepancy was registered in the Elos Medtech < Dynamic Abutment < NtTrading < CNV. The 3 scan bodies and digital implant replica systems evaluated obtained better accuracy in the 3D implant position transference than conventional procedures. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marques, S.; Ribeiro, P.; Falcão, C.; Lemos, B.F.; Ríos-Carrasco, B.; Ríos-Santos, J.V.; Herrero-Climent, M. Digital Impressions in Implant Dentistry: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 1020. https://doi.org/10.3390/ijerph18031020
Marques S, Ribeiro P, Falcão C, Lemos BF, Ríos-Carrasco B, Ríos-Santos JV, Herrero-Climent M. Digital Impressions in Implant Dentistry: A Literature Review. International Journal of Environmental Research and Public Health. 2021; 18(3):1020. https://doi.org/10.3390/ijerph18031020
Chicago/Turabian StyleMarques, Simone, Paulo Ribeiro, Carlos Falcão, Bernardo Ferreira Lemos, Blanca Ríos-Carrasco, José Vicente Ríos-Santos, and Mariano Herrero-Climent. 2021. "Digital Impressions in Implant Dentistry: A Literature Review" International Journal of Environmental Research and Public Health 18, no. 3: 1020. https://doi.org/10.3390/ijerph18031020
APA StyleMarques, S., Ribeiro, P., Falcão, C., Lemos, B. F., Ríos-Carrasco, B., Ríos-Santos, J. V., & Herrero-Climent, M. (2021). Digital Impressions in Implant Dentistry: A Literature Review. International Journal of Environmental Research and Public Health, 18(3), 1020. https://doi.org/10.3390/ijerph18031020










