Long-Term Changes in Older Adults’ Independence Levels for Performing Activities of Daily Living in Care Settings: A Nine-Year Follow-Up Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population, Design
2.2. Measurements
2.3. Statistical Analysis
2.4. Ethical Considerations
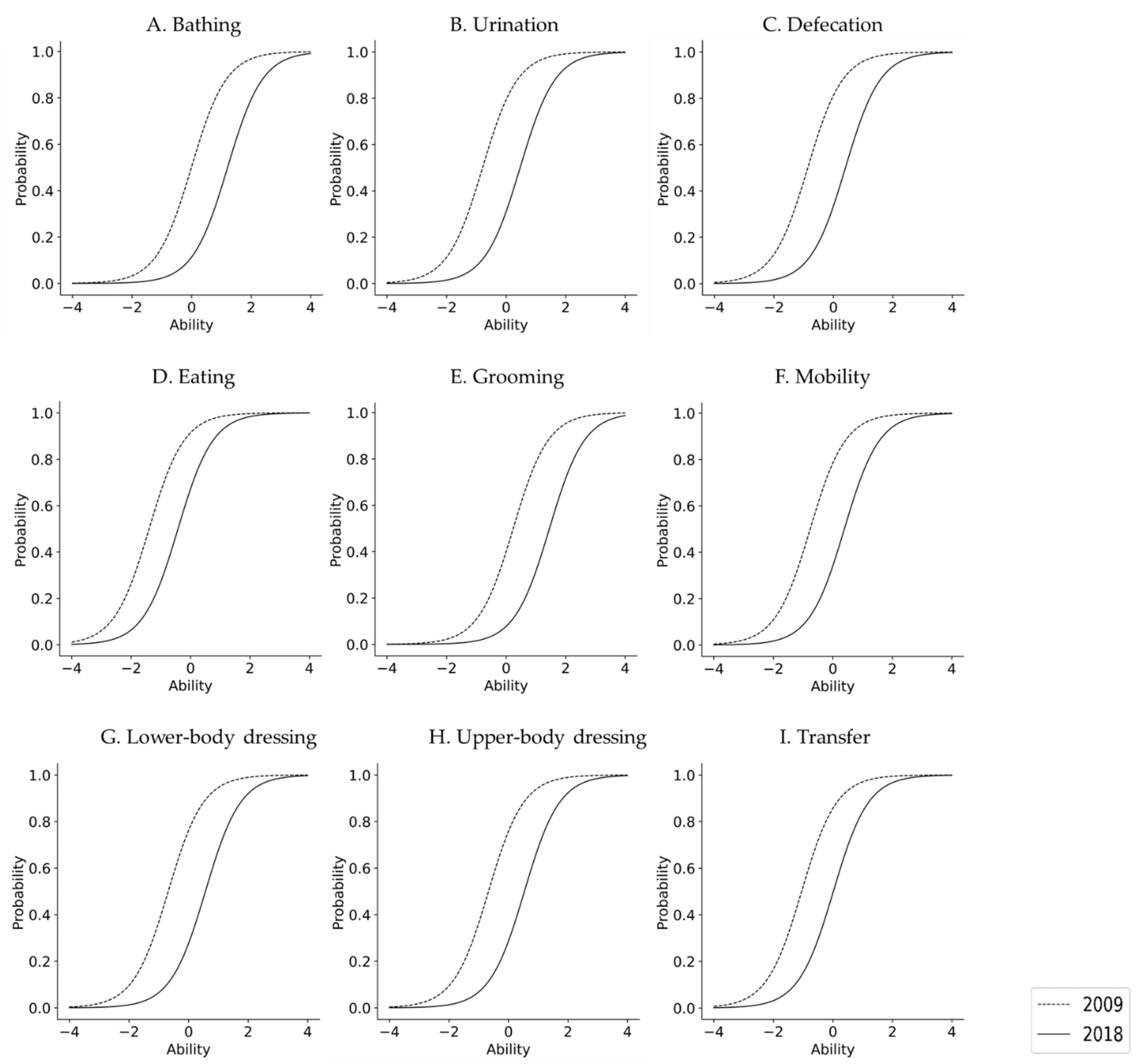
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Cabinet Office, Government of Japan. Labour and Welfare, 2019. Long-Term Care, Health and Welfare Services for the Elderly. Available online: https://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/index.html (accessed on 12 September 2021). (In Japanese)
- Cabinet Office, Government of Japan. Survey on the Senior Citizens’ Attitude toward Daily Living. 2017. Available online: https://www8.cao.go.jp/kourei/ishiki/h29/zentai/pdf/sec_2_1.pdf (accessed on 12 September 2021). (In Japanese)
- Di Bari, M.; Virgillo, A.; Matteuzzi, D.; Inzitari, M.; Mazzaglia, G.; Pozzi, C.; Geppetti, P.; Masotti, G.; Marchionni, N.; Pini, R. Predictive validity of measures of comorbidity in older community dwellers: The Insufficienza Cardiaca negli Anziani Residenti a Dicomano Study. J. Am. Geriatr. Soc. 2006, 54, 210–216. [Google Scholar] [CrossRef]
- Shinkai, S.; Kumagai, S.; Fujiwara, Y.; Amano, H.; Yoshida, Y.; Watanabe, S.; Ishizaki, T.; Suzuki, T.; Shibata, H. Predictors for the onset of functional decline among initially non-disabled older people living in a community during a 6-year follow-up. Geriatr. Gerontol. Int. 2003, 3, S31–S39. [Google Scholar] [CrossRef]
- Okabe, T.; Abe, Y.; Tomita, Y.; Mizukami, S.; Kanagae, M.; Arima, K.; Nishimura, T.; Tsujimoto, R.; Tanaka, N.; Goto, H.; et al. Age-specific risk factors for incident disability in activities of daily living among middle-aged and elderly community-dwelling Japanese women during an 8-9-year follow up: The Hizen-Oshima study. Geriatr. Gerontol. Int. 2017, 17, 1096–1101. [Google Scholar] [CrossRef] [PubMed]
- Andrews, J.S.; Cenzer, I.S.; Yelin, E.; Covinsky, K.E. Pain as a risk factor for disability or death. J. Am. Geriatr. Soc. 2013, 61, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. Healthy Japan 21. Jpn. Med Assoc. J. 2003, 46, 47–49. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/kenkounippon21.html (accessed on 12 September 2021). (In Japanese).
- Vaupel, J.W. Biodemography of human ageing. Nature 2010, 464, 536–542. [Google Scholar] [CrossRef] [Green Version]
- Luy, M.; Minagawa, Y. Gender gaps-Life expectancy and proportion of life in poor health. Health Rep. 2014, 25, 12–19. [Google Scholar]
- Sauvaget, C.; Tsuji, I.; Aonuma, T.; Hisamichi, S. Health-life expectancy according to various functional levels. J. Am. Geriatr. Soc. 1999, 47, 1326–1331. [Google Scholar] [CrossRef]
- Shi, Z.; Lin, J.; Xiao, J.; Fang, Y. Sex differences in the association between latent class of lifestyle and disability among older adults in China. BMC Geriatr. 2021, 21, 188. [Google Scholar] [CrossRef]
- Palacios-Ceña, D.; Jiménez-García, R.; Hernández-Barrera, V.; Alonso-Blanco, C.; Carrasco-Garrido, P.; Fernández-de-Las-Peñas, C. Has the prevalence of disability increased over the past decade (2000–2007) in elderly people? A Spanish population-based survey. J. Am. Med. Dir. Assoc. 2012, 13, 136–142. [Google Scholar] [CrossRef]
- Auais, M.; Ahmed, T.; Alvarado, B.; Phillips, S.P.; Rosendaal, N.; Curcio, C.L.; Fernandes, J.; Guralnik, J.; Zunzunegui, M.V. Gender differences in four-year incidence of self-reported and performance-based functional disability: The International Mobility in Aging Study. Arch. Gerontol. Geriatr. 2019, 82, 266–272. [Google Scholar] [CrossRef]
- Sato, S.; Demura, S.; Kobayashi, H.; Nagasawa, Y. The relationship and its change with aging between ADL and daily life satisfaction characteristics in independent Japanese elderly living at home. J. Physiol. Anthropol. Appl. Hum. Sci. 2002, 21, 195–204. [Google Scholar] [CrossRef] [Green Version]
- Sato, S.; Demura, S.; Tanaka, K.; Kasuga, K.; Kobayashi, H. ADL ability characteristics of partially dependent older people: Gender and age differences in ADL ability. Environ. Health Prev. Med. 2001, 6, 92–96. [Google Scholar] [CrossRef]
- Dunlop, D.D.; Hughes, S.L.; Manheim, L.M. Disability in activities of daily living: Patterns of change and a hierarchy of disability. Am. J. Public Health 1997, 87, 378–383. [Google Scholar] [CrossRef] [Green Version]
- Jagger, C.; Arthur, A.J.; Spiers, N.A.; Clarke, M. Patterns of onset of disability in activities of daily living with age. J. Am. Geriatr. Soc. 2001, 49, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Fong, J.H.; Feng, J. Patterns of Functional Disability in the Oldest Adults in China. J. Am. Geriatr. Soc. 2016, 64, 1890–1894. [Google Scholar] [CrossRef] [PubMed]
- Kingston, A.; Collerton, J.; Davies, K.; Bond, J.; Robinson, L.; Jagger, C. Losing the ability in activities of daily living in the oldest old: A hierarchic disability scale from the Newcastle 85+ study. PLoS ONE 2012, 7, e31665. [Google Scholar] [CrossRef]
- Kishimoto, M.; Ojima, T.; Nakamura, Y.; Yanagawa, H.; Fujita, Y.; Kasagi, F.; Kodama, K.; Ueda, K.; Suzuki, S.; Kagamimori, S. Relationship between the level of activities of daily living and chronic medical conditions among the elderly. J. Epidemiol. 1998, 8, 272–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spector, W.D.; Fleishman, J.A. Combining activities of daily living with instrumental activities of daily living to measure functional disability. J. Gerontol. B Psychol. Sci. Soc. Sci. 1998, 53, S46–S57. [Google Scholar] [CrossRef] [Green Version]
- Morris, J.N.; Berg, K.; Fries, B.E.; Steel, K.; Howard, E.P. Scaling functional status within the interRAI suite of assessment instruments. BMC Geriatr. 2013, 13, 128. [Google Scholar] [CrossRef] [Green Version]
- Ferrucci, L.; Guralnik, J.M.; Cecchi, F.; Marchionni, N.; Salani, B.; Kasper, J.; Celli, R.; Giardini, S.; Heikkinen, E.; Jylhä, M.; et al. Constant hierarchic patterns of physical functioning across seven populations in five countries. Gerontologist 1998, 38, 286–294. [Google Scholar] [CrossRef] [Green Version]
- Tamiya, N.; Noguchi, H.; Nishi, A.; Reich, M.R.; Ikegami, N.; Hashimoto, H.; Shibuya, K.; Kawachi, I.; Campbell, J.C. Population ageing and wellbeing: Lessons from Japan's long-term care insurance policy. Lancet 2011, 378, 1183–1192. [Google Scholar] [CrossRef]
- Fukuda, Y.; Nakao, H.; Yahata, Y.; Imai, H. In-depth descriptive analysis of trends in prevalence of long-term care in Japan. Geriatr. Gerontol. Int. 2008, 8, 166–171. [Google Scholar] [CrossRef]
- Ikegami, N. Rationale, Design and Sustainability of Long-Term Care Insurance in Japan—In Retrospect. Soc. Policy Soc. 2007, 6, 423–434. [Google Scholar] [CrossRef]
- Maruta, M.; Tabira, T.; Makizako, H.; Sagari, A.; Miyata, H.; Yoshimitsu, K.; Han, G.; Yoshiura, K.; Kawagoe, M. Impact of Outpatient Rehabilitation Service in Preventing the Deterioration of the Care-Needs Level Among Japanese Older Adults Availing Long-Term Care Insurance: A Propensity Score Matched Retrospective Study. Int. J. Environ. Res. Public Health 2019, 16, 1292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finlayson, M.; Mallinson, T.; Barbosa, V.M. Activities of daily living (ADL) and instrumental activities of daily living (IADL) items were stable over time in a longitudinal study on aging. J. Clin. Epidemiol. 2005, 58, 338–349. [Google Scholar] [CrossRef]
- Oksuzyan, A.; Juel, K.; Vaupel, J.W.; Christensen, K. Men: Good health and high mortality. Sex differences in health and aging. Aging Clin. Exp. Res. 2008, 20, 91–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noël-Miller, C. Longitudinal changes in disabled husbands' and wives' receipt of care. Gerontologist 2010, 50, 681–693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuzuya, M.; Hasegawa, J.; Enoki, H.; Izawa, S.; Hirakawa, Y.; Hirose, T.; Iguchi, A. Gender difference characteristics in the sociodemographic background of care recipients. Nihon Ronen Igakkai Zasshi 2010, 47, 461–467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dubuc, N.; Dubois, M.-F.; Raîche, M.; Gueye, N.D.R.; Hébert, R. Meeting the home-care needs of disabled older persons living in the community: Does integrated services delivery make a difference? BMC Geriatr. 2011, 11, 67. [Google Scholar] [CrossRef] [Green Version]
- Bürge, E.; Berchtold, A.; von Gunten, A. Gender-related ADL performance of old people recently admitted to a Swiss nursing home. A cross-sectional study. Swiss. Med. Wkly. 2011, 141, w13183. [Google Scholar] [CrossRef]
- Nathanson, C.A. Sex differences in mortality. Annu. Rev. Sociol. 1984, 10, 191–213. [Google Scholar] [CrossRef]
- Rogers, R.G.; Everett, B.G.; Onge, J.M.S.; Krueger, P.M. Social, behavioral, and biological factors, and sex differences in mortality. Demography 2010, 47, 555–578. [Google Scholar] [CrossRef] [PubMed]
- Friedman, H.S.; Tucker, J.S.; Schwartz, J.E.; Tomlinson-Keasey, C.; Martin, L.R.; Wingard, D.L.; Criqui, M.H. Psychosocial and behavioral predictors of longevity. The aging and death of the “termites”. Am. Psychol. 1995, 50, 69–78. [Google Scholar] [CrossRef]
- Case, A.; Paxson, C. Sex differences in morbidity and mortality. Demography 2005, 42, 189–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crimmins, E.M.; Kim, J.K.; Solé-Auró, A. Gender differences in health: Results from SHARE, ELSA and HRS. Eur. J. Public Health 2011, 21, 81–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verbrugge, L.M.; Wingard, D.L. Sex differentials in health and mortality. Women Health 1987, 12, 103–145. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L. Gender differences in the reporting of physical and somatoform symptoms. Psychosom. Med. 1998, 60, 150–155. [Google Scholar] [CrossRef]
- Naik, A.D.; Concato, J.; Gill, T.M. Bathing disability in community-living older persons: Common, consequential, and complex. J. Am. Geriatr. Soc. 2004, 52, 1805–1810. [Google Scholar] [CrossRef]
- Gill, T.M.; Guo, Z.; Allore, H.G. The epidemiology of bathing disability in older persons. J. Am. Geriatr. Soc. 2006, 54, 1524–1530. [Google Scholar] [CrossRef] [PubMed]
- Gill, T.M.; Allore, H.G.; Han, L. Bathing disability and the risk of long-term admission to a nursing home. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 821–825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LaPlante, M.P.; Harrington, C.; Kang, T. Estimating paid and unpaid hours of personal assistance services in activities of daily living provided to adults living at home. Health Serv. Res. 2002, 37, 397–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yagi, A.; Hayasaka, S.; Ojima, T.; Sasaki, Y.; Tsuji, T.; Miyaguni, Y.; Nagamine, Y.; Namiki, T.; Kondo, K. Bathing Frequency and Onset of Functional Disability Among Japanese Older Adults: A Prospective 3-Year Cohort Study From the JAGES. J. Epidemiol. 2019, 29, 451–456. [Google Scholar] [CrossRef] [Green Version]
- Shida, J.; Sugawara, K.; Goto, J.; Sekito, Y. Relationship between self-esteem and living conditions among stroke survivors at home. Jpn. J. Nurs. Sci. 2014, 11, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Fong, J.H.; Feng, J. Comparing the loss of functional independence of older adults in the U.S. and China. Arch. Gerontol. Geriatr. 2018, 74, 123–127. [Google Scholar] [CrossRef] [PubMed]


| 2009 | 2018 | |
|---|---|---|
| Mean ± SD, n (%) | ||
| Sex | Men 1143 (19.5) | |
| Women 4729 (80.5) | ||
| Age (years) | 79.2 ± 6.4 | 88.2 ± 6.4 |
| Men 76.2 ± 6.3 | Men 85.2 ± 6.3 | |
| Women 80.0 ± 6.2 | Women 89.0± 6.2 | |
| Lived at home | 5451 (92.8) | 4542 (77.4) |
| Living alone | 2497 (42.5) | 2829 (48.2) |
| Living together | 2954 (50.3) | 1713 (29.2) |
| In an institution | 421 (7.2) | 1330 (22.6) |
| Care-need level | ||
| Requiring support 1 | 1050 (17.9) | 247 (4.2) |
| Requiring support 2 | 1816 (30.9) | 624 (10.6) |
| Requiring long-term care 1 | 1285 (21.9) | 718 (12.2) |
| Requiring long-term care 2 | 807 (13.7) | 1024 (17.4) |
| Requiring long-term care 3 | 452 (7.7) | 1039 (17.7) |
| Requiring long-term care 4 | 304 (5.2) | 1211 (20.6) |
| Requiring long-term care 5 | 158 (2.7) | 1009 (17.2) |
| n = 5872 | |||||
|---|---|---|---|---|---|
| ADL Items | All | Men | Women | ||
| % (n) | % (n) | % (n) | p † | ||
| 2009 y | Grooming | 58.6 (3443) | 63.8 (729) | 57.4 (2714) | <0.001 |
| Bathing | 49.7 (2921) | 57.1 (653) | 48.0 (2268) | <0.001 | |
| Upper-body dressing | 29.4 (1724) | 43.2 (494) | 26.0 (1230) | <0.001 | |
| Lower-body dressing | 28.6 (1680) | 40.8 (466) | 25.7 (1214) | <0.001 | |
| Mobility | 25.4 (1490) | 32.7 (374) | 23.6 (1116) | <0.001 | |
| Urination | 25.1 (1476) | 34.6 (395) | 22.9 (1081) | <0.001 | |
| Defecation | 23.3 (1366) | 31.9 (365) | 21.2 (1001) | <0.001 | |
| Transfer | 18.6 (1094) | 25.5 (291) | 17.0 (803) | <0.001 | |
| Eating | 12.0 (703) | 17.4 (199) | 10.7 (504) | <0.001 | |
| 2018 y | Grooming | 89.8 (5275) | 90.6 (1035) | 89.7 (4240) | 0.383 |
| Bathing | 85.1 (5000) | 86.8 (992) | 84.8 (4008) | <0.086 | |
| Upper-body dressing | 68.4 (4017) | 72.9 (833) | 67.3 (3184) | <0.001 | |
| Lower-body dressing | 62.9 (4064) | 73.4 (839) | 68.2 (3225) | <0.001 | |
| Mobility | 62.2 (3654) | 60.0 (686) | 62.8 (2968) | 0.089 | |
| Urination | 66.2 (3885) | 69.6 (796) | 65.3 (3089) | 0.006 | |
| Defecation | 64.0 (3757) | 66.6 (761) | 63.4 (2996) | 0.043 | |
| Transfer | 49.9 (2933) | 48.1 (550) | 50.4 (2383) | 0.177 | |
| Eating | 34.9 (2051) | 32.9 (376) | 35.4 (1675) | 0.112 | |
| χ2 test |
| 2009 y | 2018 y | β | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADL Items | β2009 | SE | χ2 | p | R | β2018 | SE | χ2 | p | R | ||
| All | Grooming | 0.263 | 0.018 | 398.5 | <0.001 | 1 | 1.476 | 0.025 | 376.3 | <0.001 | 1 | 1.213 |
| Bathing | 0.025 | 0.016 | 207.2 | <0.001 | 2 | 1.231 | 0.025 | 393.2 | <0.001 | 2 | 1.206 | |
| Upper-body dressing | −0.578 | 0.018 | 86.8 | <0.001 | 3 | 0.568 | 0.020 | 205.8 | <0.001 | 4 | 1.146 | |
| Lower-body dressing | −0.604 | 0.018 | 153.9 | <0.001 | 4 | 0.595 | 0.021 | 220.2 | <0.001 | 3 | 1.199 | |
| Mobility | −0.721 | 0.018 | 77.9 | <0.001 | 5 | 0.365 | 0.020 | 1112.8 | <0.001 | 7 | 1.086 | |
| Urination | −0.73 | 0.018 | 188.1 | <0.001 | 6 | 0.493 | 0.020 | 116.1 | <0.001 | 5 | 1.223 | |
| Defecation | −0.802 | 0.019 | 216.8 | <0.001 | 7 | 0.421 | 0.020 | 141.8 | <0.001 | 6 | 1.223 | |
| Transfer | −0.998 | 0.020 | 49.3 | <0.001 | 8 | 0.0 | 0.019 | 1746.2 | <0.001 | 8 | 0.998 | |
| Eating | −1.338 | 0.022 | 189.8 | <0.001 | 9 | −0.436 | 0.022 | 1493.2 | <0.001 | 9 | 0.902 | |
| Men | Grooming | 0.376 | 0.046 | 16.6 | <0.001 | 1 | 1.564 | 0.059 | 61.2 | <0.001 | 1 | 1.188 |
| Bathing | 0.177 | 0.044 | 25.7 | <0.001 | 2 | 1.335 | 0.054 | 68.6 | <0.001 | 2 | 1.158 | |
| Upper-body dressing | −0.226 | 0.042 | 22.3 | <0.001 | 3 | 0.72 | 0.046 | 27.9 | <0.001 | 4 | 0.946 | |
| Lower-body dressing | −0.299 | 0.043 | 44.4 | <0.001 | 4 | 0.739 | 0.046 | 56.2 | <0.001 | 3 | 1.038 | |
| Mobility | −0.552 | 0.044 | 19.0 | <0.001 | 6 | 0.293 | 0.043 | 50.2 | <0.001 | 7 | 0.845 | |
| Urination | −0.493 | 0.044 | 62.6 | <0.001 | 5 | 0.605 | 0.045 | 35.2 | <0.001 | 5 | 1.098 | |
| Defecation | −0.578 | 0.045 | 69.3 | <0.001 | 7 | 0.501 | 0.044 | 34.8 | <0.001 | 6 | 1.079 | |
| Transfer | −0.803 | 0.047 | 20.3 | <0.001 | 8 | −0.049 | 0.043 | 21.7 | <0.001 | 8 | 0.754 | |
| Eating | −1.131 | 0.052 | 37.7 | <0.001 | 9 | −0.49 | 0.046 | 89.7 | <0.001 | 9 | 0.641 | |
| Women | Grooming | 0.241 | 0.019 | 447.4 | <0.001 | 1 | 1.458 | 0.027 | 433.1 | <0.001 | 1 | 1.217 |
| Bathing | −0.005 | 0.017 | 214.0 | <0.001 | 2 | 1.21 | 0.027 | 433.9 | <0.001 | 2 | 1.215 | |
| Upper-body dressing | −0.669 | 0.021 | 68.6 | <0.001 | 3 | 0.538 | 0.022 | 248.5 | <0.001 | 4 | 1.207 | |
| Lower-body dressing | −0.681 | 0.021 | 108.9 | <0.001 | 4 | 0.567 | 0.022 | 221.3 | <0.001 | 3 | 1.248 | |
| Mobility | −0.76 | 0.021 | 133.4 | <0.001 | 5 | 0.388 | 0.021 | 780.1 | <0.001 | 7 | 1.148 | |
| Urination | −0.789 | 0.021 | 138.4 | <0.001 | 6 | 0.472 | 0.022 | 131.0 | <0.001 | 5 | 1.261 | |
| Defecation | −0.859 | 0.022 | 160.1 | <0.001 | 7 | 0.407 | 0.021 | 166.6 | <0.001 | 6 | 1.266 | |
| Transfer | −1.049 | 0.024 | 112.7 | <0.001 | 8 | 0.017 | 0.021 | 1564.1 | <0.001 | 8 | 1.066 | |
| Eating | −1.394 | 0.026 | 188.6 | <0.001 | 9 | −0.421 | 0.024 | 1270.7 | <0.001 | 9 | 0.973 | |
| Men median (quartile) | Women median (quartile) | p† | ||||||||||
| Total of β | 1.038 (0.845, 1.098) | 1.215 (1.148, 1.248) | 0.008 | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okabe, T.; Suzuki, M.; Iso, N.; Tanaka, K.; Sagari, A.; Miyata, H.; Han, G.; Maruta, M.; Tabira, T.; Kawagoe, M. Long-Term Changes in Older Adults’ Independence Levels for Performing Activities of Daily Living in Care Settings: A Nine-Year Follow-Up Study. Int. J. Environ. Res. Public Health 2021, 18, 9641. https://doi.org/10.3390/ijerph18189641
Okabe T, Suzuki M, Iso N, Tanaka K, Sagari A, Miyata H, Han G, Maruta M, Tabira T, Kawagoe M. Long-Term Changes in Older Adults’ Independence Levels for Performing Activities of Daily Living in Care Settings: A Nine-Year Follow-Up Study. International Journal of Environmental Research and Public Health. 2021; 18(18):9641. https://doi.org/10.3390/ijerph18189641
Chicago/Turabian StyleOkabe, Takuhiro, Makoto Suzuki, Naoki Iso, Koji Tanaka, Akira Sagari, Hironori Miyata, Gwanghee Han, Michio Maruta, Takayuki Tabira, and Masahiro Kawagoe. 2021. "Long-Term Changes in Older Adults’ Independence Levels for Performing Activities of Daily Living in Care Settings: A Nine-Year Follow-Up Study" International Journal of Environmental Research and Public Health 18, no. 18: 9641. https://doi.org/10.3390/ijerph18189641






