Beneficial Effects of Mindfulness-Based Stress Reduction Training on the Well-Being of a Female Sample during the First Total Lockdown Due to COVID-19 Pandemic in Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
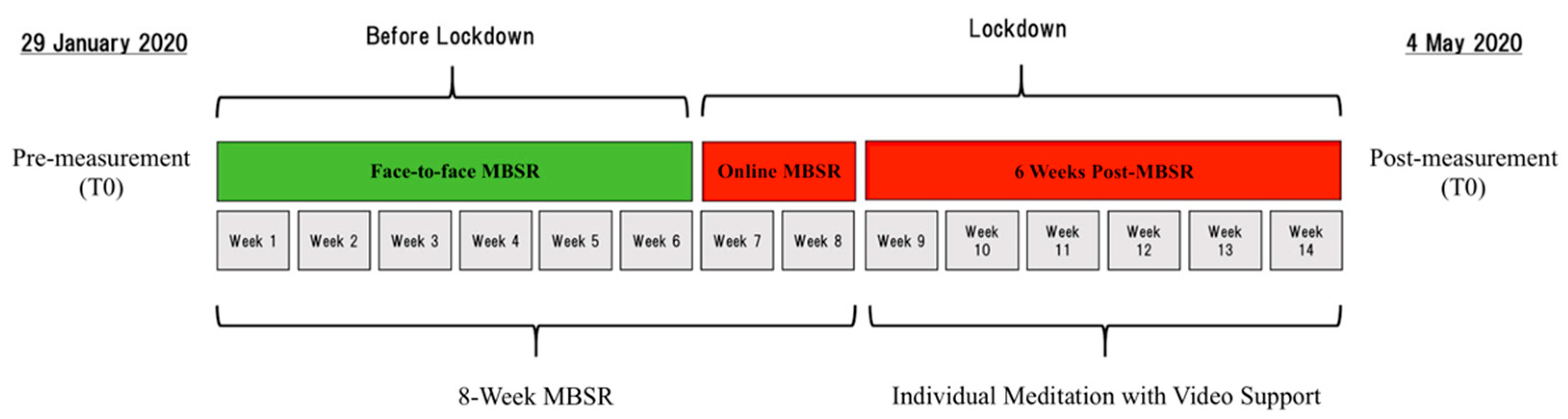
2.3. Procedure
2.4. Statistical Analyses
3. Results
3.1. Preliminary Analyses: The Between-Group Difference at Baseline
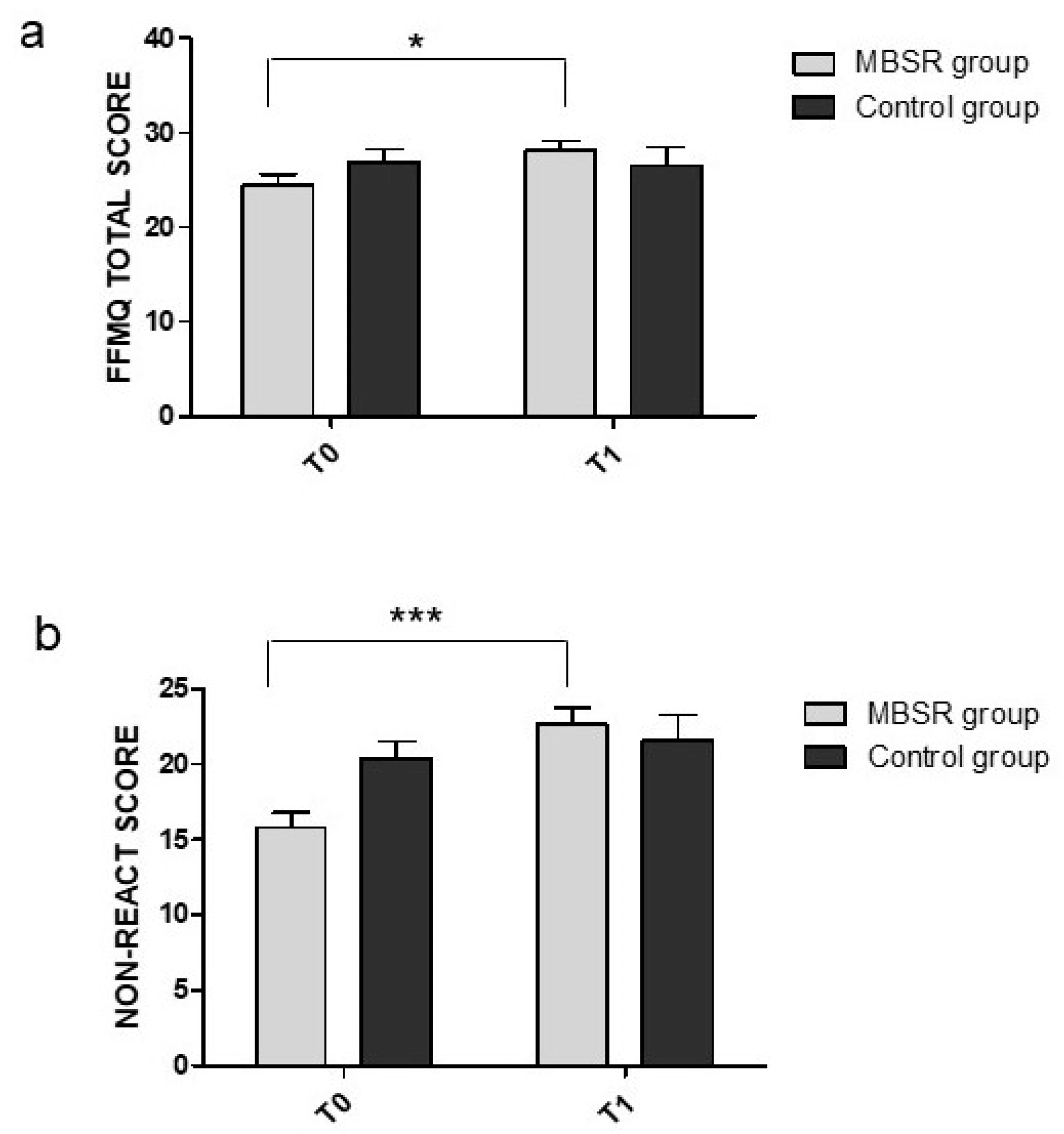
3.2. Effects of MBSR on Mindfulness Variables Measured Using the FFMQ Questionnaire
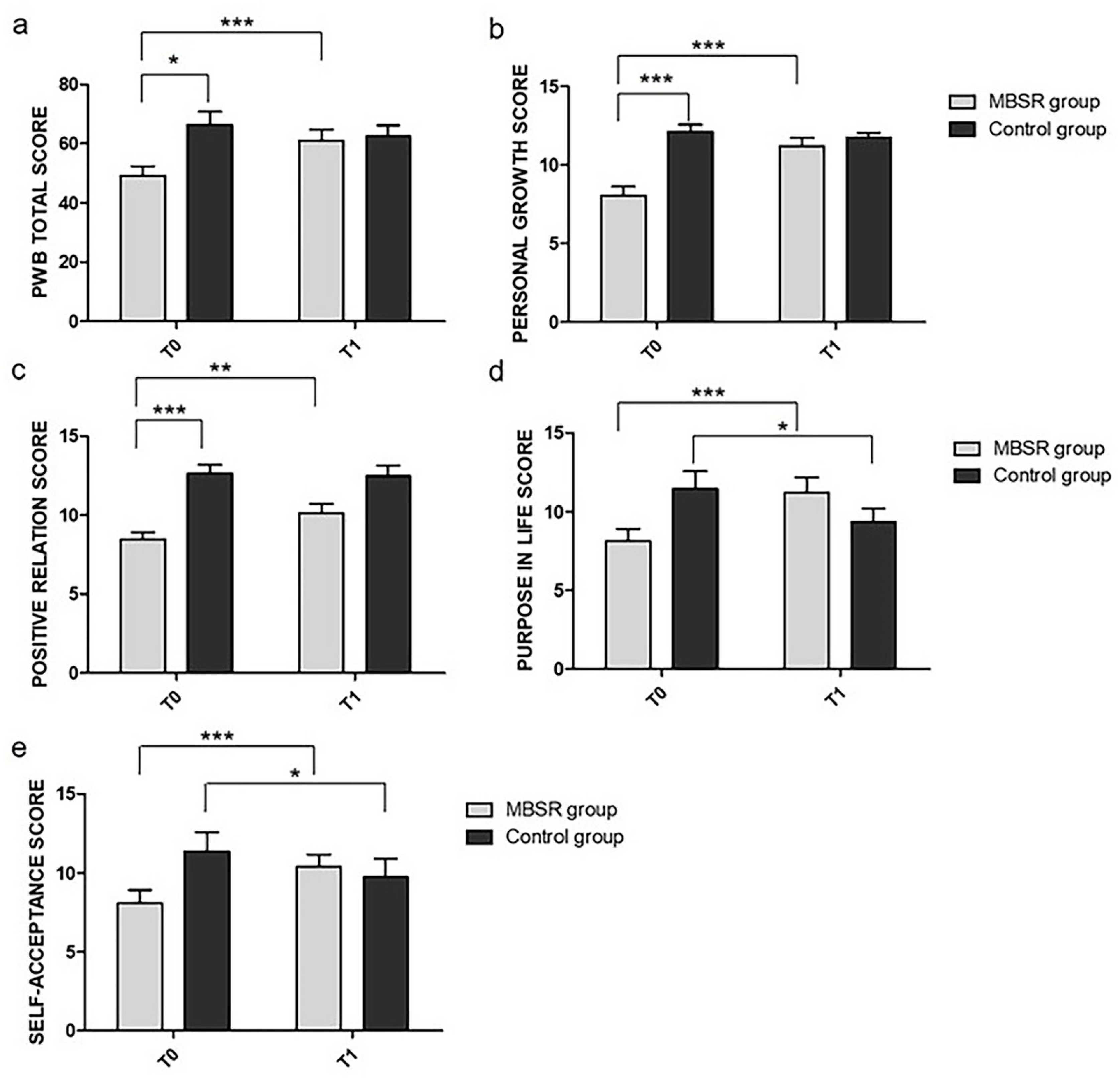
3.3. Effects of MBSR on Psychological Well-Being Variables as Measured Using the PWB Questionnaire
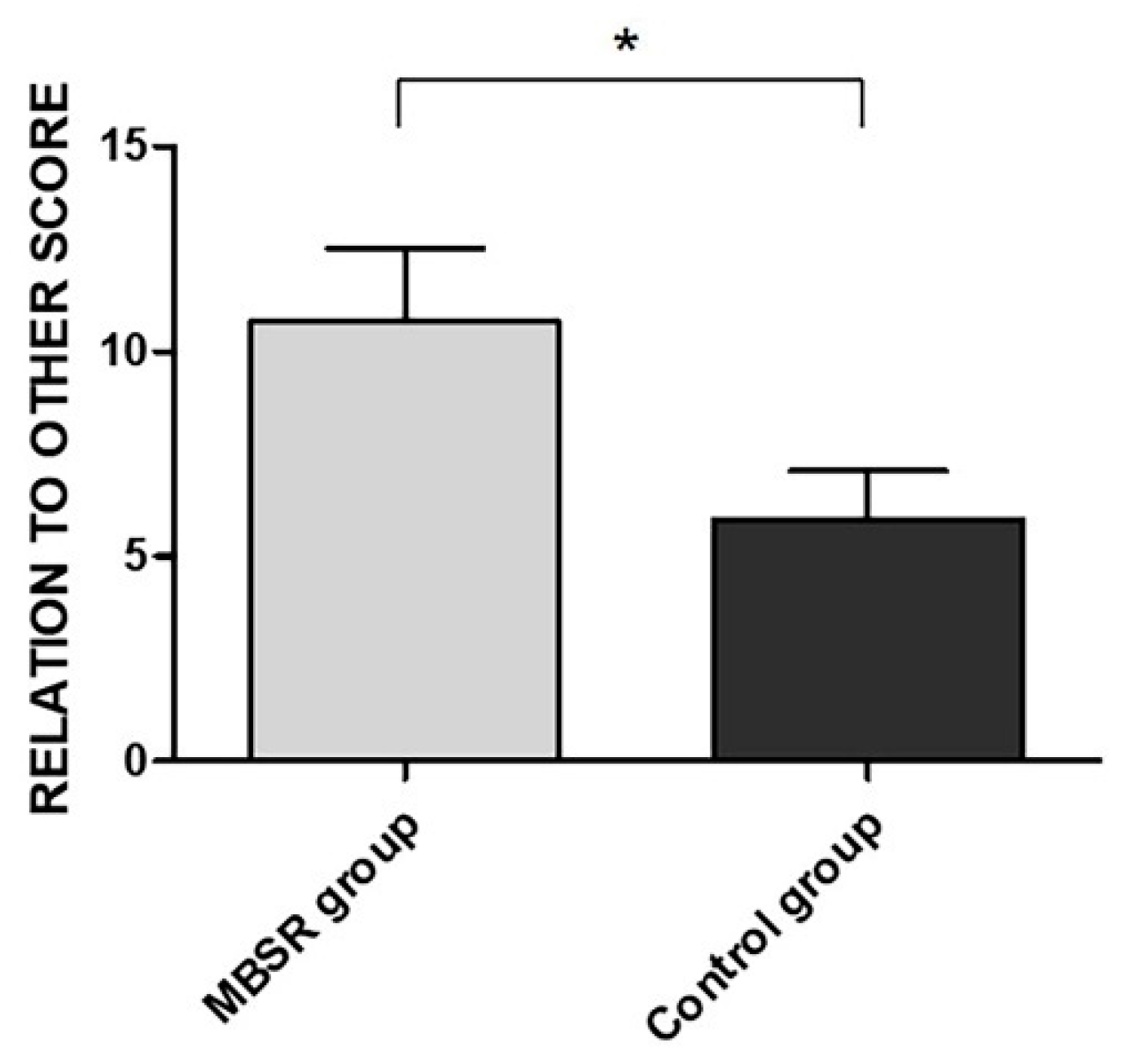
3.4. Effects of MBSR on Post-Traumatic Growth Variables Measured Using the PTGI Questionnaire
3.5. Effects of MBSR on Flexibility as Measured Using the AAQ-II Questionnaire
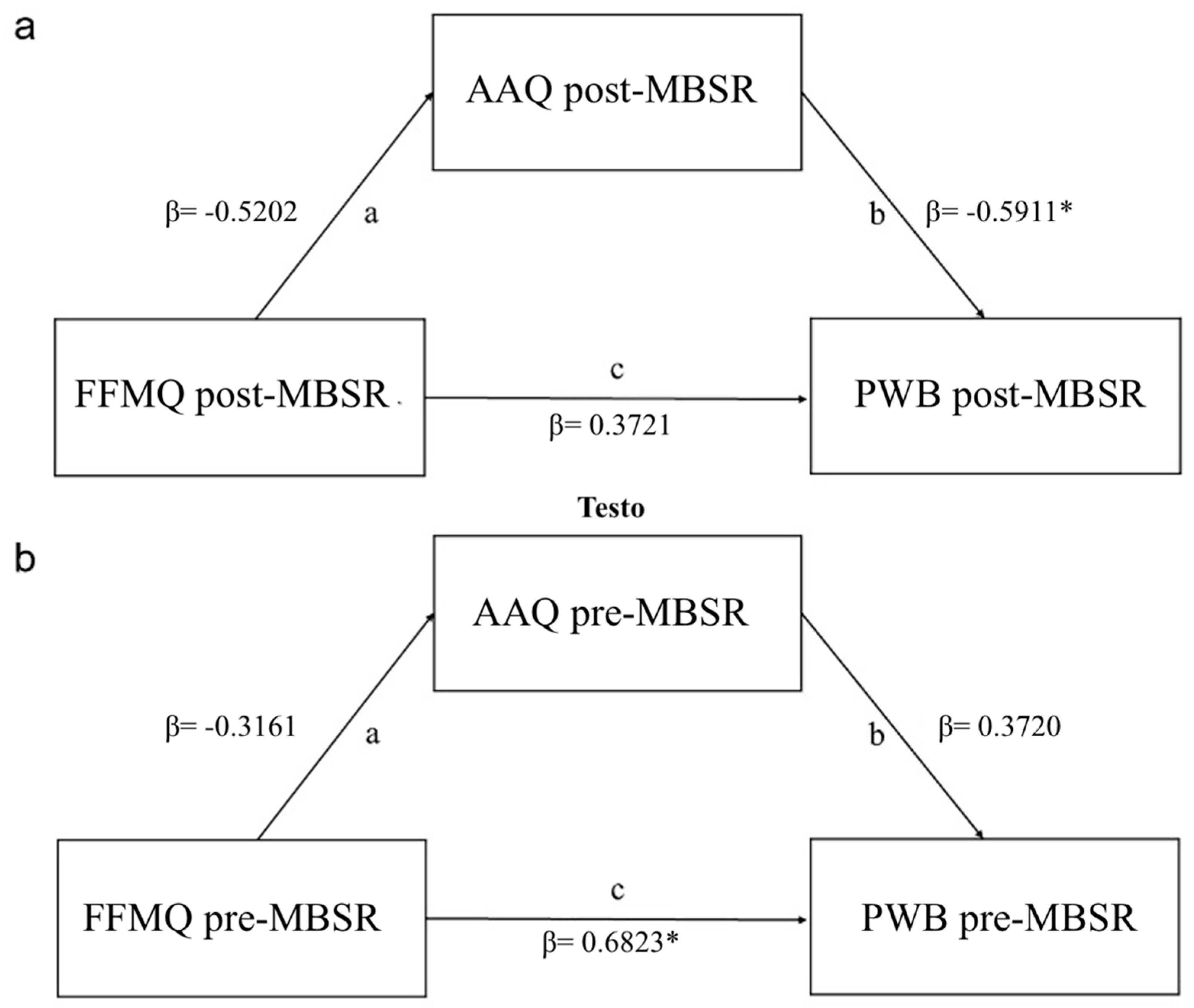
3.6. Mindfulness Predictor of Psychopathological Outcomes during the Pandemic in MBSR Group
4. Discussion
4.1. Objective 1: Effects of MBSR Training on Mindfulness Skills
4.2. Objective 2: Effects of MBSR Training on Psychological Well-Being
4.3. Objective 3: Post-Traumatic Growth
4.4. Objective 4: The Role of Psychological Flexibility as Mediator Variable
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef]
- Fauci, A.S.; Lane, H.C.; Redfield, R.R. Covid-19—Navigating the uncharted. N. Engl. J. Med. 2020, 382, 1268–1269. [Google Scholar] [CrossRef] [PubMed]
- Mahase, E. Covid-19: UK starts social distancing after new model points to 260,000 potential deaths. BMJ 2020, 368, m1089. [Google Scholar] [CrossRef] [Green Version]
- Spina, S.; Marrazzo, F.; Migliari, M.; Stucchi, R.; Sforza, A.; Fumagalli, R. The response of Milan’s emergency medical system to the COVID-19 outbreak in Italy. Lancet 2020, 395, e49–e50. [Google Scholar] [CrossRef] [Green Version]
- Distante, C.; Piscitelli, P.; Miani, A. Covid-19 outbreak progression in Italian regions: Approaching the peak by the end of march in Northern Italy and first week of april in Southern Italy. Int. J. Environ. Res. Public Health 2020, 17, 3025. [Google Scholar] [CrossRef] [PubMed]
- Bao, C.; Liu, X.; Zhang, H.; Li, Y.; Liu, J. Coronavirus disease 2019 (COVID-19) CT findings: A systematic review and meta-analysis. J. Am. Coll. Radiol. 2020, 17, 701–709. [Google Scholar] [CrossRef] [PubMed]
- Capuano, R.; Altieri, M.; Bisecco, A.; d’Ambrosio, A.; Docimo, R.; Buonanno, D.; Matrone, F.; Giuliano, F.; Tedeschi, G.; Santangelo, G.; et al. Psychological consequences of COVID-19 pandemic in Italian MS patients: Signs of resilience? J. Neurol. 2021, 268, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Orrù, G.; Ciacchini, R.; Gemignani, A.; Conversano, C. Psychological intervention measures during the Covid-19 pandemic. Clin. Neuropsychiatry 2020, 17, 76–79. [Google Scholar]
- Poli, A.; Gemignani, A.; Conversano, C. The psychological impact of SARS-CoV-2 quarantine: Observations through the lens of the polyvagal theory. Clin. Neuropsychiatry 2020, 17, 112–114. [Google Scholar]
- Nelson, B.; Pettitt, A.; Flannery, J.; Allen, N. Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample. PLoS ONE 2020, 15, e0241990. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marazziti, D.; Pozza, A.; Di Giuseppe, M.; Conversano, C. The psychosocial impact of COVID-19 pandemic in Italy: A lesson for mental health prevention in the first severely hit European country. Psychol. Trauma 2020, 12, 531–533. [Google Scholar] [CrossRef]
- Davico, C.; Ghiggia, A.; Marcotulli, D.; Ricci, F.; Amianto, F.; Vitiello, B. Psychological impact of the COVID-19 pandemic on adults and their children in Italy. SSRN Electron. J. 2020, 12, 239. [Google Scholar]
- Baiano, C.; Zappullo, I.; Conson, M.; The LabNPEE Group. Tendency to worry and fear of mental health during Italy’s COVID-19 lockdown. Int. J. Environ. Res. Public Health 2020, 17, 5928. [Google Scholar] [CrossRef]
- Liu, N.; Zhang, F.; Wei, C.; Jia, Y.; Shang, Z.; Sun, L.; Wu, L.; Sun, Z.; Zhou, Y.; Wang, Y.; et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020, 287, 112921. [Google Scholar] [CrossRef]
- Ravaldi, C.; Wilson, A.; Ricca, V.; Homer, C.; Vannacci, A. Pregnant women voice their concerns and birth Expectations during the COVID-19 pandemic in Italy. Women Birth 2020. [Google Scholar] [CrossRef]
- Favieri, F.; Forte, G.; Tambelli, R.; Casagrande, M. The Italians in the time of coronavirus: Psychosocial aspects of unexpected COVID-19 pandemic. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Meredith, L.S.; Eisenman, D.P.; Tanielian, T.; Taylor, S.L.; Basurto-Davila, R.; Zazzali, J.; Diamond, D.; Cienfuegos, B.; Shields, S. Prioritizing “psychological” consequences for disaster preparedness and response: A framework for addressing the emotional, behavioral, and cognitive effects of patient surge in large-scale disasters. Disaster Med. Public Health Prep. 2011, 5, 73–80. [Google Scholar] [CrossRef]
- Lanciano, T.; Graziano, G.; Curci, A.; Costadura, S.; Monaco, A. Risk perceptions and psychological effects during the Italian COVID-19 emergency. Front. Psychol. 2020, 11, 580053. [Google Scholar] [CrossRef]
- Flesia, L.; Monaro, M.; Mazza, C.; Fietta, V.; Colicino, E.; Segatto, B.; Roma, P. Predicting perceived stress related to the covid-19 outbreak through stable psychological traits and machine learning models. J. Clin. Med. 2020, 9, 3350. [Google Scholar] [CrossRef]
- Anisman, H.; Merali, Z. Understanding stress: Characteristics and caveats. Alcohol Res. Health 1999, 23, 241–249. [Google Scholar]
- Koolhaas, J.M.; Bartolomucci, A.; Buwalda, B.; de Boer, S.F.; Flügge, G.; Korte, S.M.; Meerlo, P.; Murison, R.; Olivier, B.; Palanza, P.; et al. Stress revisited: A critical evaluation of the stress concept. Neurosci. Biobehav. Rev. 2011, 35, 1291–1301. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.A. How much “thinking” about COVID-19 is clinically dysfunctional? Brain Behav. Immun. 2020, 87, 97–98. [Google Scholar] [CrossRef] [PubMed]
- Nowak, B.; Brzóska, P.; Piotrowski, J.; Sedikides, C.; Żemojtel-Piotrowska, M.; Jonason, P.K. Adaptive and maladaptive behavior during the COVID-19 pandemic: The roles of dark triad traits, collective narcissism, and health beliefs. Pers. Individ. Dif. 2020, 167, 110232. [Google Scholar] [CrossRef]
- Brailovskaia, J.; Margraf, J. Predicting adaptive and maladaptive responses to the coronavirus (COVID-19) outbreak: A prospective longitudinal study. Int. J. Clin. Health Psychol. 2020, 20, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Arslan, G.; Yıldırım, M.; Aytaç, M. Subjective vitality and loneliness explain how coronavirus anxiety increases rumination among college students. Death Stud. 2020, 1–10. [Google Scholar] [CrossRef]
- Simione, L.; Gnagnarella, C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. Front. Psychol. 2020, 11, 2166. [Google Scholar] [CrossRef]
- Casagrande, M.; Favieri, F.; Tambelli, R.; Forte, G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020, 75, 12–20. [Google Scholar] [CrossRef]
- Zhang, J.; Lu, H.; Zeng, H.; Zhang, S.; Du, Q.; Jiang, T.; Du, B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020, 87, 49–50. [Google Scholar] [CrossRef] [PubMed]
- Merow, C.; Urban, M.C. Seasonality and uncertainty in global COVID-19 growth rates. Proc. Natl. Acad. Sci. USA 2020, 117, 27456–27464. [Google Scholar] [CrossRef] [PubMed]
- Zhong, B.-L.; Luo, W.; Li, H.-M.; Zhang, Q.-Q.; Liu, X.-G.; Li, W.-T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Full Catastrophe Living; Delacorte Press: New York, NY, USA, 1990. [Google Scholar]
- Grossman, P.; Niemann, L.; Schmidt, S.; Walach, H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Focus Altern. Complement. Ther. 2010, 8, 500. [Google Scholar] [CrossRef]
- Goldin, P.R.; Gross, J.J. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion 2010, 10, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Raffone, A.; Srinivasan, N. Mindfulness and cognitive functions: Toward a unifying neurocognitive framework. Mindfulness 2017, 8, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Brown, K.W.; Goodman, R.J.; Inzlicht, M. Dispositional mindfulness and the attenuation of neural responses to emotional stimuli. Soc. Cogn. Affect. Neurosci. 2013, 8, 93–99. [Google Scholar] [CrossRef] [Green Version]
- Bishop, S.R.; Lau, M.; Shapiro, S.; Carlson, L.; Anderson, N.D.; Carmody, J.; Segal, Z.V.; Abbey, S.; Speca, M.; Velting, D.; et al. Mindfulness: A proposed operational definition. Clin. Psychol. 2006, 11, 230–241. [Google Scholar] [CrossRef]
- Buddharakkhita, A. Metta: Philosophy & Practice of Universal Love; Buddhist Publication Society: Kandy, Sri Lanka, 2007. [Google Scholar]
- Friese, M.; Messner, C.; Schaffner, Y. Mindfulness meditation counteracts self-control depletion. Conscious. Cogn. 2012, 21, 1016–1022. [Google Scholar] [CrossRef]
- Moore, A.; Malinowski, P. Meditation, mindfulness and cognitive flexibility. Conscious. Cogn. 2009, 18, 176–186. [Google Scholar] [CrossRef]
- Jones, D.R.; Lehman, B.J.; Noriega, A.; Dinnel, D.L. The effects of a short-term mindfulness meditation intervention on coping flexibility. Anxiety Stress Cop. 2019, 32, 347–361. [Google Scholar] [CrossRef] [PubMed]
- Juneau, C.; Shankland, R.; Dambrun, M. Trait and state equanimity: The effect of mindfulness-based meditation practice. Mindfulness 2020, 11, 1802–1812. [Google Scholar] [CrossRef]
- Guillaume, N.; Jean, M.; Marcaurelle, R.; Dupuis, G. Mindfulness meditation versus training in tranquil abiding: Theoretical comparison and relevance for developing concentration. Psychol. Conscious. 2020, 7, 151–172. [Google Scholar] [CrossRef]
- Bostanov, V.; Keune, P.M.; Kotchoubey, B.; Hautzinger, M. Event-related brain potentials reflect increased concentration ability after mindfulness-based cognitive therapy for depression: A randomized clinical trial. Psychiatry Res. 2012, 199, 174–180. [Google Scholar] [CrossRef]
- Charoensukmongkol, P. Benefits of mindfulness meditation on emotional intelligence, general self-efficacy, and perceived stress: Evidence from Thailand. J. Spiritual. Ment. Health 2014, 16, 171–192. [Google Scholar] [CrossRef]
- Chu, L.-C. The benefits of meditation vis-à-vis emotional intelligence, perceived stress and negative mental health. Stress Health 2010, 26, 169–180. [Google Scholar] [CrossRef]
- Hofmann, S.G.; Grossman, P.; Hinton, D.E. Loving-kindness and compassion meditation: Potential for psychological interventions. Clin. Psychol. Rev. 2011, 31, 1126–1132. [Google Scholar] [CrossRef] [Green Version]
- Baer, R.A. Self-compassion as a mechanism of change in mindfulness-and acceptance-based treatments. In Assessing Mindfulness and Acceptance Processes in Clients: Illuminating the Theory and Practice of Change; New Harbinger: Oakland, CA, USA, 2010; pp. 135–153. [Google Scholar]
- Neff, K.D.; Dahm, K.A. Self-compassion: What it is, what it does, and how it relates to mindfulness. In Handbook of Mindfulness and Self-Regulation; Springer: New York, NY, USA, 2015; pp. 121–137. [Google Scholar]
- Kabat-Zinn, J. Mindfulness-based stress reduction (MBSR). Denton 2003, 8, 73–83. [Google Scholar]
- Bishop, S.R. What do we really know about mindfulness-based stress reduction? Psychosom. Med. 2002, 64, 71–83. [Google Scholar] [CrossRef]
- Baer, R.A.; Smith, G.T.; Hopkins, J.; Krietemeyer, J.; Toney, L. Using self-report assessment methods to explore facets of mindfulness. Assessment 2006, 13, 27–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindahl, J.R.; Fisher, N.E.; Cooper, D.J.; Rosen, R.K.; Britton, W.B. The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLoS ONE 2017, 12, e0176239. [Google Scholar] [CrossRef]
- Gu, J.; Strauss, C.; Bond, R.; Cavanagh, K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol. Rev. 2015, 37, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Chiesa, A.; Serretti, A. Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. J. Altern. Complement. Med. 2009, 15, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Carmody, J.; Baer, R.A. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J. Behav. Med. 2008, 31, 23–33. [Google Scholar] [CrossRef]
- Cohen-Katz, J.; Wiley, S.D.; Capuano, T.; Baker, D.M.; Kimmel, S.; Shapiro, S. The effects of mindfulness-based stress reduction on nurse stress and burnout, part II: A quantitative and qualitative study. Holist. Nurs. Pract. 2005, 19, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, S.L.; Schwartz, G.E.; Bonner, G. Effects of mindfulness-based stress reduction on medical and premedical students. J. Behav. Med. 1998, 21, 581–599. [Google Scholar] [CrossRef] [PubMed]
- Boyd, J.; Lanius, R.; McKinnon, M. Mindfulness-based treatments for post-traumatic stress disorder: A review of the treatment literature and neurobiological evidence. J. Psychiatry Neurosci. 2018, 43, 7–25. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Q.; Zhao, H.; Zheng, Y. Effectiveness of mindfulness-based stress reduction (MBSR) on symptom variables and health-related quality of life in breast cancer patients—A systematic review and meta-analysis. Support. Care Cancer 2019, 27, 771–781. [Google Scholar] [CrossRef]
- Zhang, J.-Y.; Zhou, Y.-Q.; Feng, Z.-W.; Fan, Y.-N.; Zeng, G.-C.; Wei, L. Randomized controlled trial of mindfulness-based stress reduction (MBSR) on posttraumatic growth of Chinese breast cancer survivors. Psychol. Health Med. 2017, 22, 94–109. [Google Scholar] [CrossRef]
- Ledesma, D.; Kumano, H. Mindfulness-based stress reduction and cancer: A meta-analysis: Mindfulness and cancer. Psychooncology 2009, 18, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Spijkerman, M.P.J.; Pots, W.T.M.; Bohlmeijer, E.T. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clin. Psychol. Rev. 2016, 45, 102–114. [Google Scholar] [CrossRef] [Green Version]
- Sevilla-Llewellyn-Jones, J.; Santesteban-Echarri, O.; Pryor, I.; McGorry, P.; Alvarez-Jimenez, M. Web-based mindfulness interventions for mental health treatment: Systematic review and meta-analysis. JMIR Ment. Health 2018, 5, e10278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmad, F.; Wang, J.J.; El Morr, C. Online mindfulness interventions: A systematic review. In Advances in Healthcare Information Systems and Administration; IGI Global: Hershey, PA, USA, 2018; pp. 1–27. [Google Scholar]
- Matiz, A.; Fabbro, F.; Paschetto, A.; Cantone, D.; Paolone, A.R.; Crescentini, C. Positive impact of mindfulness meditation on mental health of female teachers during the COVID-19 outbreak in Italy. Int. J. Environ. Res. Public Health 2020, 17, 6450. [Google Scholar] [CrossRef] [PubMed]
- Liu, L. Examining the usefulness of mindfulness practices in managing school leader stress during COVID-19 pandemic. J. Sch. Administ. Res. Dev. 2020, 5 (Suppl. S1), 15–20. [Google Scholar] [CrossRef]
- Bäuerle, A.; Graf, J.; Jansen, C.; Musche, V.; Schweda, A.; Hetkamp, M.; Weismüller, B.; Dörrie, N.; Junne, F.; Teufel, M.; et al. E-mental health mindfulness-based and skills-based “CoPE It” intervention to reduce psychological distress in times of COVID-19: Study protocol for a bicentre longitudinal study. BMJ Open 2020, 10, e039646. [Google Scholar] [CrossRef] [PubMed]
- Gutowski, E.; White, A.E.; Liang, B.; Diamonti, A.-J.; Berado, D. How stress influences purpose development: The importance of social support. J. Adolesc. Res. 2018, 33, 571–597. [Google Scholar] [CrossRef]
- Carver, C.S.; Scheier, M.F. On the Self-Regulation of Behavior; Cambridge University Press: Cambridge, UK, 1998. [Google Scholar]
- Mystakidou, K.; Parpa, E.; Tsilika, E.; Panagiotou, I.; Theodorakis, P.N.; Galanos, A.; Gouliamos, A. Self-efficacy and its relationship to posttraumatic stress symptoms and posttraumatic growth in cancer patients. J. Loss Trauma 2015, 20, 160–170. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. The posttraumatic growth inventory: Measuring the positive legacy of trauma. J. Trauma. Stress 1996, 9, 455–471. [Google Scholar] [CrossRef]
- Gu, J.; Strauss, C.; Crane, C.; Barnhofer, T.; Karl, A.; Cavanagh, K.; Kuyken, W. Examining the factor structure of the 39-item and 15-item versions of the five facet mindfulness questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychol. Assess. 2016, 28, 791–802. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biglan, A.; Hayes, S.C.; Pistorello, J. Acceptance and commitment: Implications for prevention science. Prev. Sci. 2008, 9, 139–152. [Google Scholar] [CrossRef] [Green Version]
- Kashdan, T.B.; Rottenberg, J. Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev. 2010, 30, 865–878. [Google Scholar] [CrossRef] [Green Version]
- Giovannini, C.; Giromini, L.; Bonalume, L.; Tagini, A.; Lang, M.; Amadei, G. The Italian five facet mindfulness questionnaire: A contribution to its validity and reliability. J. Psychopathol. Behav. Assess. 2014, 36, 415–423. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Pers. Soc. Psychol. 1989, 57, 1069–1081. [Google Scholar] [CrossRef]
- Sirigatti, S.; Stefanile, C.; Giannetti, E.; Iani, L.; Penzo, I.; Mazzeschi, A. Assessment of factor structure of Ryff’s psychological well-being scales in Italian adolescents. Boll. Psicol. Appl. 2009, 259, 30–50. [Google Scholar]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary psychometric properties of the acceptance and action questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef] [Green Version]
- Pennato, T.; Berrocal, C.; Bernini, O.; Rivas, T. Italian version of the acceptance and action questionnaire-II (AAQ-II): Dimensionality, reliability, convergent and criterion validity. J. Psychopathol. Behav. Assess. 2013, 35, 552–563. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Banerjee, M.; Cavanagh, K.; Strauss, C. A qualitative study with healthcare staff exploring the facilitators and barriers to engaging in a self-help mindfulness-based intervention. Mindfulness 2017, 8, 1653–1664. [Google Scholar] [CrossRef]
- Hunt, C.A.; Hoffman, M.A.; Mohr, J.J.; Williams, A.-L. Assessing perceived barriers to meditation: The determinants of meditation practice inventory-revised (DMPI-R). Mindfulness 2020, 11, 1139–1149. [Google Scholar] [CrossRef]
- Wenzel, M.; von Versen, C.; Hirschmüller, S.; Kubiak, T. Curb your neuroticism—Mindfulness mediates the link between neuroticism and subjective well-being. Pers. Individ. Dif. 2015, 80, 68–75. [Google Scholar] [CrossRef]
- Evans, S.; Ferrando, S.; Findler, M.; Stowell, C.; Smart, C.; Haglin, D. Mindfulness-based cognitive therapy for generalized anxiety disorder. J. Anxiety Disord. 2008, 22, 716–721. [Google Scholar] [CrossRef]
- Hazlett-Stevens, H. Mindfulness-based stress reduction for comorbid anxiety and depression: Case report and clinical considerations. J. Nerv. Ment. Dis. 2012, 200, 999–1003. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Lindquist, R. Effects of mindfulness-based stress reduction on depression, anxiety, stress and mindfulness in Korean nursing students. Nurs. Educ. Today 2015, 35, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Freligh, C.B.; Debb, S.M. Nonreactivity and resilience to stress: Gauging the mindfulness of African American college students. Mindfulness 2019, 10, 2302–2311. [Google Scholar] [CrossRef]
- McManus, F.; Surawy, C.; Muse, K.; Vazquez-Montes, M.; Williams, J.M.G. A randomized clinical trial of mindfulness-based cognitive therapy versus unrestricted services for health anxiety (Hypochondriasis). J. Consult. Clin. Psychol. 2012, 80, 817–828. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- Tran, B.X.; Ha, G.H.; Nguyen, L.H.; Vu, G.T.; Hoang, M.T.; Le, H.T.; Latkin, C.A.; Ho, C.S.H.; Ho, R.C.M. Studies of novel coronavirus disease 19 (COVID-19) pandemic: A global analysis of literature. Int. J. Environ. Res. Public Health 2020, 17, 4095. [Google Scholar] [CrossRef]
- Trzebiński, J.; Cabański, M.; Czarnecka, J.Z. Reaction to the COVID-19 pandemic: The influence of meaning in life, life satisfaction, and assumptions on world orderliness and positivity. J. Loss Trauma 2020, 25, 544–557. [Google Scholar] [CrossRef]
- Lima, C.K.T.; de Carvalho, P.M.M.; de Lima, I.A.A.S.; de Nunes, J.V.A.O.; Saraiva, J.S.; de Souza, R.I.; da Silva, C.G.L.; Neto, M.L.R. The emotional impact of coronavirus 2019-NCoV (new coronavirus disease). Psychiatry Res. 2020, 287, 112915. [Google Scholar] [CrossRef]
- Shi, W.; Hall, B.J. What can we do for people exposed to multiple traumatic events during the coronavirus pandemic? Asian J. Psychiatry 2020, 51, 102065. [Google Scholar] [CrossRef]
- Mukhtar, S. Psychological health during the coronavirus disease 2019 pandemic outbreak. Int. J. Soc. Psychiatry 2020, 66, 512–516. [Google Scholar] [CrossRef]
- Mukhtar, S. Mental health and psychosocial aspects of coronavirus outbreak in Pakistan: Psychological intervention for public mental health crisis. Asian J. Psychiatry 2020, 51, 102069. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, A.L.; Faulkner, B.; Wekerle, C. The relationship among internal resilience, smoking, alcohol use, and depression symptoms in emerging adults transitioning out of child welfare. Child Abuse Negl. 2013, 37, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Richardson, G.E. The metatheory of resilience and resiliency. J. Clin. Psychol. 2002, 58, 307–321. [Google Scholar] [CrossRef] [PubMed]
- Tedeschi, R.G.; Calhoun, L.G. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychol. Inq. 2004, 15, 1–18. [Google Scholar] [CrossRef]
- Colzato, L.S.; Zech, H.; Hommel, B.; Verdonschot, R.; van den Wildenberg, W.P.; Hsieh, S. Loving-kindness bringsloving-kindness: The impact of Buddhism on cognitive self–other integration. Psychonom. Bull. Rev. 2020, 19, 541–545. [Google Scholar] [CrossRef] [Green Version]
- Trautwein, F.M.; Naranjo, J.R.; Schmidt, S. Meditation effects in the social domain: Self-other connectedness as a general mechanism? In Meditation—Neuroscientific Approaches and Philosophical Implications; Schmidt, S., Walach, H., Eds.; Springer: Cham, Switzerland, 2014; pp. 175–198. [Google Scholar]
- Chiarella, S.G.; Makwana, M.; Simione, L.; Hartkamp, M.; Calabrese, L.; Raffone, A.; Srinivasan, N. Mindfulness meditation weakens attachment to self: Evidence from a self vs other binding task. Mindfulness 2020, 11, 2411–2422. [Google Scholar] [CrossRef]
- Luberto, C.M.; Shinday, N.; Song, R.; Philpotts, L.L.; Park, E.R.; Fricchione, G.L.; Yeh, G.Y. A systematic review and meta-analysis of the effects of meditation on empathy, compassion, and prosocial behaviors. Mindfulness 2018, 9, 708–724. [Google Scholar] [CrossRef]
- Işık Ulusoy, S.; Kal, Ö. Relationship among coping strategies, quality of life, and anxiety and depressive disorders in hemodialysis patients: Coping strategies and mood in hemodialysis. Ther. Apher. Dial. 2020, 24, 189–196. [Google Scholar] [CrossRef]
- Gloster, A.T.; Meyer, A.H.; Lieb, R. Psychological flexibility as a malleable public health target: Evidence from a representative sample. J. Contextual Behav. Sci. 2017, 6, 166–171. [Google Scholar] [CrossRef] [Green Version]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stabbe, O.K.; Rolffs, J.L.; Rogge, R.D. Flexibly and/or inflexibly embracing life: Identifying fundamental approaches to life with latent profile analyses on the dimensions of the hexaflex model. J. Contextual Behav. Sci. 2019, 12, 106–118. [Google Scholar] [CrossRef]
- Roemer, L.; Orsillo, S.M.; Salters-Pedneault, K. Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: Evaluation in a randomized controlled trial. J. Consult. Clin. Psychol. 2008, 76, 1083–1089. [Google Scholar] [CrossRef] [Green Version]
- Dahl, J.; Wilson, K.G.; Nilsson, A. Acceptance and commitment therapy and the treatment of persons at risk for long-term disability resulting from stress and pain symptoms: A preliminary randomized trial. Behav. Ther. 2004, 35, 785–801. [Google Scholar] [CrossRef] [Green Version]
- Trindade, I.A.; Mendes, A.L.; Ferreira, N.B. The moderating effect of psychological flexibility on the link between learned helplessness and depression symptomatology: A preliminary study. J. Contextual Behav. Sci. 2020, 15, 68–72. [Google Scholar] [CrossRef]
- Creswell, J.D.; Pacilio, L.E.; Lindsay, E.K.; Brown, K.W. Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology 2014, 44, 1–12. [Google Scholar] [CrossRef]
- Schonert-Reichl, K.A.; Oberle, E.; Lawlor, M.S.; Abbott, D.; Thomson, K.; Oberlander, T.F.; Diamond, A. Enhancing cognitive and social-emotional development through a simple-to-administer mindfulness-based school program for elementary school children: A randomized controlled trial. Dev. Psychol. 2015, 51, 52. [Google Scholar] [CrossRef] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Accoto, A.; Chiarella, S.G.; Raffone, A.; Montano, A.; de Marco, A.; Mainiero, F.; Rubbino, R.; Valzania, A.; Conversi, D. Beneficial Effects of Mindfulness-Based Stress Reduction Training on the Well-Being of a Female Sample during the First Total Lockdown Due to COVID-19 Pandemic in Italy. Int. J. Environ. Res. Public Health 2021, 18, 5512. https://doi.org/10.3390/ijerph18115512
Accoto A, Chiarella SG, Raffone A, Montano A, de Marco A, Mainiero F, Rubbino R, Valzania A, Conversi D. Beneficial Effects of Mindfulness-Based Stress Reduction Training on the Well-Being of a Female Sample during the First Total Lockdown Due to COVID-19 Pandemic in Italy. International Journal of Environmental Research and Public Health. 2021; 18(11):5512. https://doi.org/10.3390/ijerph18115512
Chicago/Turabian StyleAccoto, Alessandra, Salvatore Gaetano Chiarella, Antonino Raffone, Antonella Montano, Adriano de Marco, Francesco Mainiero, Roberta Rubbino, Alessandro Valzania, and David Conversi. 2021. "Beneficial Effects of Mindfulness-Based Stress Reduction Training on the Well-Being of a Female Sample during the First Total Lockdown Due to COVID-19 Pandemic in Italy" International Journal of Environmental Research and Public Health 18, no. 11: 5512. https://doi.org/10.3390/ijerph18115512
APA StyleAccoto, A., Chiarella, S. G., Raffone, A., Montano, A., de Marco, A., Mainiero, F., Rubbino, R., Valzania, A., & Conversi, D. (2021). Beneficial Effects of Mindfulness-Based Stress Reduction Training on the Well-Being of a Female Sample during the First Total Lockdown Due to COVID-19 Pandemic in Italy. International Journal of Environmental Research and Public Health, 18(11), 5512. https://doi.org/10.3390/ijerph18115512






