Social Comparison and Stress Appraisal in Women with Chronic Illness
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Relationships and Structure: Social Comparison Orientation, Stress Appraisal and Social Comparison Strategies
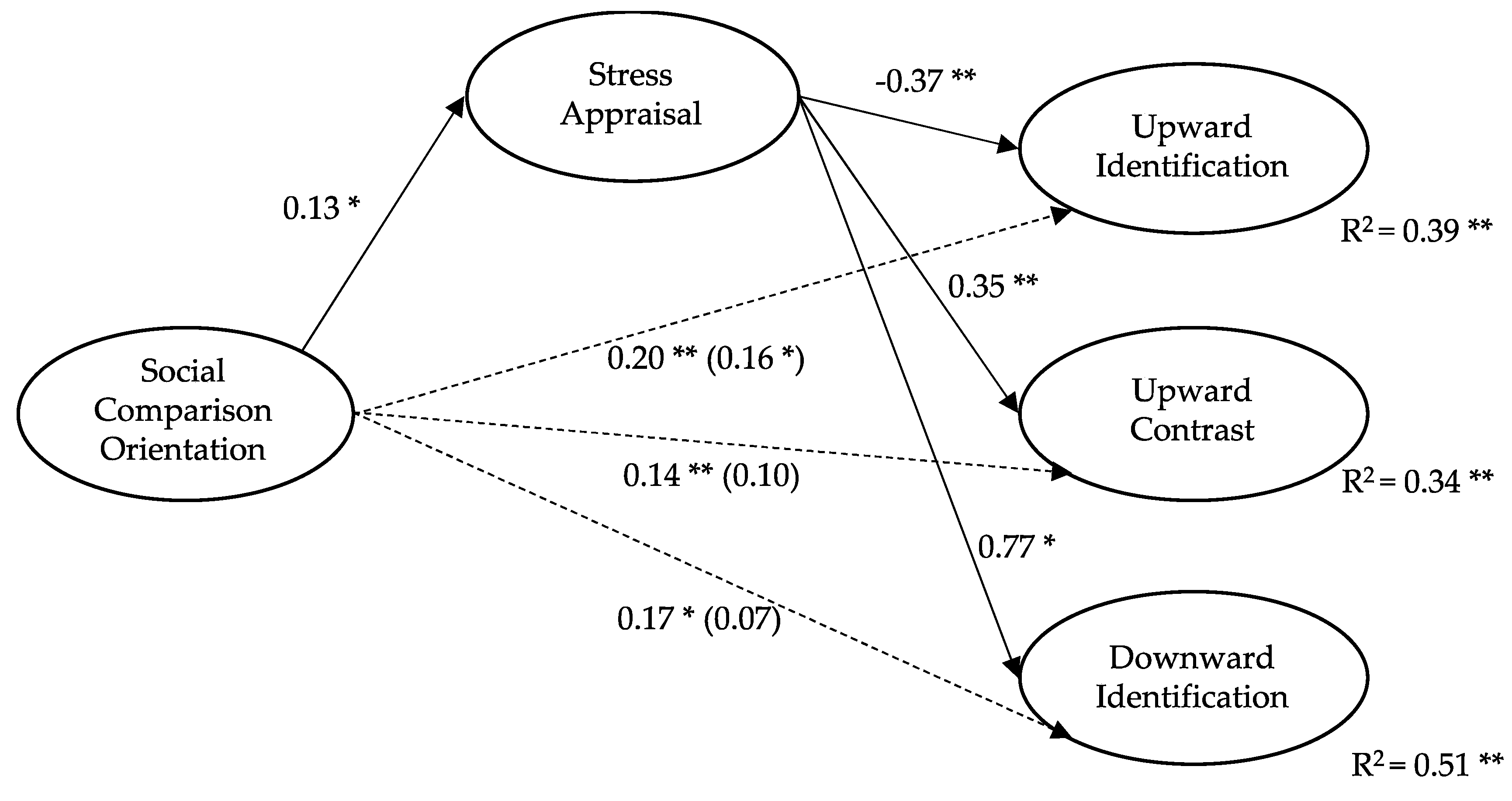
3.2. A Hypothetical Model: Stress Appraisal as a Mediator between SCO and SC Strategies
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Festinger, L.A. Theory of Social Comparison Processes. Hum. Relat. 1954, 7, 117–140. [Google Scholar] [CrossRef]
- Arigo, D.; Suls, J.; Smyth, J.M. Social Comparisons and Chronic Illness: Research Synthesis and Clinical Implications. Health Psychol. Rev. 2012, 8, 154–214. [Google Scholar] [CrossRef]
- Stiegelis, H.E.; Hagedoorn, M.; Sanderman, R.; Bennenbroek, F.T.; Buunk, A.P.; Van den Bergh, A.C.; Botke, G.; Ranchor, A.V. The Impact of an Informational Self-Management Intervention on the Association between Control and Illness Uncertainty before and Psychological Distress after Radiotherapy. PsychoOncology 2004, 13, 248–259. [Google Scholar] [CrossRef]
- Terol, M.C.; Neipp, M.C.; Lledó, A.; Pons, N.; Bernabé, M. Comparación Social y Variables Psicosociales Relacionadas: Una Revisión de Cáncer y Dolor Crónico. An. Psicol. 2012, 28, 327–337. [Google Scholar] [CrossRef]
- Umstead, K.L.; Kalia, S.S.; Madeo, A.C.; Erby, L.H.; Blank, T.O.; Visvanathan, K.; Roter, D.L. Social Comparisons and Quality of Life Following a Prostate Cancer Diagnosis. J. Psychosoc. Oncol. 2018, 36, 350–363. [Google Scholar] [CrossRef]
- Buunk, A.P.; Bennenbroek, F.; Stiegelis, H.E.; Van den Bergh, A.C.; Sanderman, R.; Hagedoorn, M. Follow-up Effects of Social Comparison Information on the Quality of Life of Cancer Patients: The Moderating Role of Social Comparison Orientation. Psychol. Health 2011, 27, 641–654. [Google Scholar] [CrossRef]
- Buunk, A.P.; Belmonte, J.; Peiró, J.M.; Zurriaga, R.; Gibbons, F.X. Diferencias Individuales En La Comparación Social: Propiedades de La Escala Española de Orientación Hacia La Comparación Social. Rev. Latinoam. Psicol. 2005, 37, 561–579. [Google Scholar]
- Corcoran, K.; Cruisius, J.; Mussweiler, T. Social Comparison: Motives, standards and mechanisms. In Theories in Social Psychology; Chadee, D., Ed.; Wiley-Blackwell: Oxford, UK, 2011; pp. 119–139. [Google Scholar]
- Tennen, H.; McKee, T.E.; Affleck, G.; Suls, J.M.; Wheeler, L. Social comparison processes in health and illness. In Handbook of Social Comparison: Theory and Research; The Plenum Series in Social/Clinical Psychology; Kluwer Academic Publishers: Boston, MA, USA, 2000; pp. 443–483. [Google Scholar]
- Terol, M.C.; Buunk, A.P.; Cabrera, V.; Bernabé, M.; Martin-Aragón, M. Profiles of Women with Fibromyalgia and Social Comparison Processes. Front. Psychol. 2020, 11. [Google Scholar] [CrossRef]
- Cabrera, V.; Buunk, A.P.; Terol, M.C.; Quiles, Y.; Martin-Aragón, M. Social Comparison Processes and Catastrophising in Fibromyalgia: A Path Analysis. Psychol. Health 2017, 32, 745–764. [Google Scholar] [CrossRef]
- Butzer, B.; Kuiper, N.A. Relationships between the Frequency of Social Comparisons and Self-Concept Clarity, Intolerance of Uncertainty, Anxiety, and Depression. Personal. Individ. Differ. 2006, 41, 167–176. [Google Scholar] [CrossRef]
- Buunk, A.P.; Zurriaga, R.; González, P.; Terol, M.C.; López-Roig, S. Targets and Dimensions of Social Comparison among People with Spinal Cord Injury and Other Health Problems. Br. J. Health Psychol. 2006, 11, 677–693. [Google Scholar] [CrossRef]
- Taylor, S.E.; Lobel, M. Social Comparison Activity under Threat: Downward Evaluation and Upward Contacts. Psychol. Rev. 1989, 96, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Buunk, A.P.; Ybema, J.F. Social comparisons and occupational stress: The identification-contrast model. In Health, Coping, and Well-Being: Perspectives from Social Comparison Theory; Buunk, B.P., Gibbons, F.X., Eds.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 1997; pp. 359–388. [Google Scholar]
- Wood, J.V.; VanderZee, K. Social comparisons among cancer patients: Under what conditions are comparisons upward and downward? In Health, Coping, and Well-Being: Perspectives from Social Comparison Theory; Buunk, B.P., Gibbons, F.X., Eds.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 1997; pp. 299–328. [Google Scholar]
- Buunk, A.P.; Gibbons, F.X. Health, Coping, and Well-Being: Perspectives from Social Comparison Theory; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 1997. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Van der Zee, K.; Buunk, B.; Sanderman, R.; Botke, G.; Van den Bergh, F. Social Comparison and Coping with Cancer Treatment. Personal. Individ. Differ. 2000, 28, 17–34. [Google Scholar] [CrossRef]
- Suls, J.; Martin, R.; Wheeler, L. Social comparison: Why, with whom, and with what effect? Curr. Dir. Psychol. Sci. 2002, 11, 159–163. [Google Scholar] [CrossRef]
- Brakel, T.M.; Dijkstra, A.; Buunk, A.P. Targeting Cancer Patients’ Quality of Life through Social Comparison: A Randomised Trial. Psychol. Health 2014, 29, 950–966. [Google Scholar] [CrossRef]
- Vitaliano, P.P.; Russo, J.; Weber, L.; Celum, C. The Dimensions of Stress Scale: Psychometric Properties1. J. Appl. Soc. Psychol. 1993, 23, 1847–1878. [Google Scholar] [CrossRef]
- Gibbons, F.X.; Gerrard, M. Downward comparison and coping with threat. In Social Comparison: Contemporary Theory and Research; Suls, J., Wills, T.A., Eds.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 1991; pp. 317–345. [Google Scholar]
- Gerber, J.P.; Wheeler, L.; Suls, J. A Social Comparison Theory Meta-Analysis 60+ Years On. Psychol. Bull. 2018, 144, 177–197. [Google Scholar] [CrossRef]
- Croyle, R.T. Appraisal of health threats: Cognition, motivation, and social comparison. Cogn. Ther. Res. 1992, 16, 165–182. [Google Scholar] [CrossRef]
- Osterman, L.M.R. Stress Appraisal: The Role of Social Comparison; Dissertations Publishing 9621761; University of California: Riverside, CA, USA, 1996. [Google Scholar]
- Katz, J.D.; Mamyrova, G.; Guzhva, O.; Furmark, L. Gender bias in diagnosing fibromyalgia. Gender Med. 2010, 7, 19–27. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. World Health Organization. Global Cancer Observatory. Available online: https://gco.iarc.fr/ (accessed on 8 April 2020).
- Gibbons, F.X.; Buunk, A.P. Individual Differences in Social Comparison: Development of a Scale of Social Comparison Orientation. J. Pers. Soc. Psychol. 1999, 76, 129–142. [Google Scholar] [CrossRef]
- Buunk, A.P.; Dijkstra, P.; Bosch, Z.A.; Dijkstra, A.; Barelds, D.P.H. Social Comparison Orientation as Related to Two Types of Closeness. J. Res. Personal. 2012, 46, 279–285. [Google Scholar] [CrossRef]
- Buunk, B.P.; Oldersma, F.L.; de Dreu, C.K.W. Enhancing Satisfaction through Downward Comparison: The Role of Relational Discontent and Individual Differences in Social Comparison Orientation. J. Exp. Soc. Psychol. 2001, 37, 452–467. [Google Scholar] [CrossRef]
- Galvin, L.R.; Godfrey, H.P. The Impact of Coping on Emotional Adjustment to Spinal Cord Injury (SCI): Review of the Literature and Application of a Stress Appraisal and Coping Formulation. Spinal Cord 2001, 39, 615–627. [Google Scholar] [CrossRef] [PubMed]
- Buunk, B.P.; Brenninkmeijer, V. When Individuals Dislike Exposure to an Actively Coping Role Model: Mood Change as Related to Depression and Social Comparison Orientation. Eur. J. Soc. Psychol. 2001, 31, 537–548. [Google Scholar] [CrossRef]
- Terol, M.C.; Quiles, Y.; Pérez, V. Manual de Evaluación Psicosocial en Contextos de Salud; Pirámide: Madrid, Spain, 2012. [Google Scholar]
- Terol, C.; Lledó, A.; Quiles, Y.; Martín-Aragón, M. Adaptation and Validation of the Spanish Version of the Social Comparison Scale in Chronic Illness Patients. J. Health Psychol. 2015, 20, 1474–1482. [Google Scholar] [CrossRef]
- Nunnally, J.C.; Bernstein, I.H. The Assessment of Reliability; Psychometric Theory; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Frias-Navarro, D. Apuntes de Consistencia Interna de las Puntuaciones de un Instrumento de Medida; Universidad de Valencia: Valencia, Spain, 2020; Available online: https://www.uv.es/friasnav/AlfaCronbach.pdf (accessed on 4 May 2021).
- Jaimeson, S. Likert Scales: How to (ab) Use Them. Med. Educ. 2005, 38, 1217–1218. [Google Scholar] [CrossRef]
- Clatworthy, J.; Buick, D.; Hankins, M.; Weinman, J.; Horne, R. The Use and Reporting of Cluster Analysis in Health Psychology: A Review. Br. J. Health Psychol. 2005, 10, 329–358. [Google Scholar] [CrossRef] [PubMed]
- Kutner, M.H.; Nachstheim, C.J.; Neter, J. Applied Linear Regression Models; McGraw Hill: New York, NY, USA, 2004. [Google Scholar]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS Procedures for Estimating Indirect Effects in Simple Mediation Models. Behav. Res. Methods Instrum. Comput. 2004, 36, 185–227. [Google Scholar] [CrossRef]
- Preacher, K.J.; Rucker, D.D.; Hayes, A.F. Addressing Moderated Mediation Hypotheses: Theory, Methods, and Prescriptions. Multivar. Behav. Res. 2007, 42, 185–227. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The Moderator–Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Dibb, B.; Yardley, L. Factors Important for the Measurement of Social Comparison in Chronic Illness: A Mixed-Methods Study. Chronic Illn. 2006, 2, 219–230. [Google Scholar] [CrossRef]
- Bouchard, L.C.; Fisher, H.M.; Carver, C.S.; Kim, Y.; Antoni, M.H. Social Comparisons Predict Health-Related Quality of Life and Depressive Symptoms across the First Year of Breast Cancer Treatment. Psychooncology 2019, 28, 386–393. [Google Scholar] [CrossRef]
- Jager, J.; Putnick, D.L.; Bornstein, M.H. More than Just Convenient: The Scientific Merits of Homogeneous Convenience Samples. Monogr. Soc. Res. Child Dev. 2017, 82, 13–30. [Google Scholar] [CrossRef]
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. Social comparison orientation | 3.03 | 0.73 | 0.25 ** | 0.13 | 0.19 * | 0.18 * | 0.14 | |
| 2. Stress appraisal | 4.07 | 1.03 | −0.32 ** | 0.32 ** | 0.47 ** | −0.10 | ||
| 3. Upward identification strategy | 3.29 | 1.54 | −0.14 | −0.14 | 0.40 ** | |||
| 4. Upward contrast strategy | 2.98 | 1.48 | 0.34 ** | 0.13 | ||||
| 5. Downward identification strategy | 2.31 | 1.31 | 0.02 | |||||
| 6. Downward contrast strategy | 3.03 | 1.35 |
| Cluster 1 | Cluster 2 | F-Fisher | p-Value | |
|---|---|---|---|---|
| (n = 89) | (n = 86) | |||
| 1. Social comparison orientation | 2.87 (0.81) | 3.20 (0.62) | 9.02 | ** |
| 2. Stress appraisal | 3.37 (0.87) | 4.76 (0.63) | 145.79 | *** |
| 3. Upward identification strategy | 3.99 (1.31) | 2.57(1.40) | 48.24 | *** |
| 4. Upward contrast strategy | 1.71 (1.01) | 2.93 (1.31) | 47.87 | *** |
| 5. Downward identification strategy | 1.96 (1.10) | 4.07 (0.94) | 182.53 | *** |
| 6. Downward contrast strategy | 3.12 (1.38) | 2.93 (1.29) | 0.92 | n.s. |
| SCO− (n = 83) | SCO+ (n = 92) | SA− (n = 77) | SA+ (n = 98) | |
|---|---|---|---|---|
| Cluster 1. (n = 89) | 57.8% | 44.57% | 89.61% | 20.41% |
| Cluster 2. (n = 86) | 42.2% | 55.43% | 10.39% | 79.59% |
| 100% | 100% | 100% | 100% | |
| χ2 = 0.054 (n.s.) | χ2 = 82.62 *** | |||
| β | SE | p-Value | t | R2 | ΔR2 | F | |
|---|---|---|---|---|---|---|---|
| Total Effects | |||||||
| Upward identification strategy | 0.20 | 0.15 | 0.002 | 2.27 | 0.31 | 9.08 * | |
| Upward contrast strategy | 0.14 | 0.13 | 0.024 | 2.27 | 0.23 | 4.68 * | |
| Downward identification strategy | 0.17 | 0.15 | 0.039 | 2.07 | 0.23 | 4.88 * | |
| Direct Effects | |||||||
| Upward identification strategy | 0.16 | 0.15 | 0.003 | 2.97 | 0.39 | 0.08 | 10.47 * |
| Upward contrast strategy | 0.10 | 0.13 | 0.122 | 1.55 | 0.34 | 0.11 | 7.94 * |
| Downward identification strategy | 0.07 | 0.13 | 0.368 | 0.90 | 0.51 | 0.28 | 19.78 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Terol Cantero, M.C.; Bernabé, M.; Martín-Aragón, M.; Vázquez, C.; Buunk, A.P. Social Comparison and Stress Appraisal in Women with Chronic Illness. Int. J. Environ. Res. Public Health 2021, 18, 5483. https://doi.org/10.3390/ijerph18105483
Terol Cantero MC, Bernabé M, Martín-Aragón M, Vázquez C, Buunk AP. Social Comparison and Stress Appraisal in Women with Chronic Illness. International Journal of Environmental Research and Public Health. 2021; 18(10):5483. https://doi.org/10.3390/ijerph18105483
Chicago/Turabian StyleTerol Cantero, M. Carmen, Miguel Bernabé, Maite Martín-Aragón, Carolina Vázquez, and Abraham P. Buunk. 2021. "Social Comparison and Stress Appraisal in Women with Chronic Illness" International Journal of Environmental Research and Public Health 18, no. 10: 5483. https://doi.org/10.3390/ijerph18105483
APA StyleTerol Cantero, M. C., Bernabé, M., Martín-Aragón, M., Vázquez, C., & Buunk, A. P. (2021). Social Comparison and Stress Appraisal in Women with Chronic Illness. International Journal of Environmental Research and Public Health, 18(10), 5483. https://doi.org/10.3390/ijerph18105483






