Relations between Stress and Depressive Symptoms in Psychiatric Nurses: The Mediating Effects of Sleep Quality and Occupational Burnout
Abstract
:1. Introduction
2. Methods
2.1. Design and Setting
2.2. Participants
2.3. Data Collection and Ethical Considerations
2.4. Instruments
2.4.1. Chinese Pittsburgh Sleep Quality Index
2.4.2. Stress
2.4.3. The Center for Epidemiologic Studies Depression
2.4.4. Occupational Burnout Inventory
2.5. Data Analysis
3. Results
3.1. Participant Characteristics
3.2. Preliminary Analysis
3.3. Structural Equation Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vasconcelos, E.M.; Martino, M.M.F.; França, S.P.S. Burnout and depressive symptoms in intensive care nurses: Relationship analysis. Rev. Bras. Enferm. 2018, 71, 135–141. [Google Scholar] [CrossRef] [Green Version]
- Maharaj, S.; Lees, T.; Lal, S. Prevalence and Risk Factors of Depression, Anxiety, and Stress in a Cohort of Australian Nurses. Int. J. Environ. Res. Public Health 2018, 16, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Nursing the Nurses. 2019. Available online: https://www.upaged.com/blog/nursing-and-depression-on-r-u-ok-day (accessed on 5 March 2021).
- Gao, Y.Q.; Pan, B.C.; Sun, W.; Wu, H.; Wang, J.N.; Wang, L. Depressive symptoms among Chinese nurses: Prevalence and the associated factors. J. Adv. Nurs. 2012, 68, 1166–1175. [Google Scholar] [CrossRef]
- Tsaras, K.; Papathanasiou, I.V.; Vus, V.; Panagiotopoulou, A.; Katsou, M.A.; Kelesi, M.; Fradelos, E.C. Predicting Factors of Depression and Anxiety in Mental Health Nurses: A Quantitative Cross-Sectional Study. Med. Arch. 2018, 72, 62–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moustaka, L.; Constantinidis, T. Sources and effects of Work-related stress in nursing. Health Sci. J. 2010, 4, 210–216. [Google Scholar]
- Welsh, D. Predictors of depressive symptoms in female medical-surgical hospital nurses. Issues Ment. Health Nurs. 2009, 30, 320–326. [Google Scholar] [CrossRef]
- Stetz, M.C.; Thomas, M.L.; Russo, M.B.; Stetz, T.A.; Wildzunas, R.M.; McDonald, J.J.; Wiederhold, B.K.; Romano, J.A., Jr. Stress, mental health, and cognition: A brief review of relationships and countermeasures. Aviat. Space Environ. Med. 2007, 78, B252–B260. [Google Scholar]
- Lee, C.Y.; Chen, H.C.; Meg Tseng, M.C.; Lee, H.C.; Huang, L.H. The Relationships Among Sleep Quality and Chronotype, Emotional Disturbance, and Insomnia Vulnerability in Shift Nurses. J. Nurs. Res. JNR 2015, 23, 225–235. [Google Scholar] [CrossRef]
- Griep, R.H.; Bastos, L.S.; Fonseca Mde, J.; Silva-Costa, A.; Portela, L.F.; Toivanen, S.; Rotenberg, L. Years worked at night and body mass index among registered nurses from eighteen public hospitals in Rio de Janeiro, Brazil. BMC Health Serv. Res. 2014, 14, 603. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.L.; Howard, M.E.; Horrey, W.J.; Liang, Y.; Anderson, C.; Shreeve, M.S.; O’Brien, C.S.; Czeisler, C.A. High risk of near-crash driving events following night-shift work. Proc. Natl. Acad. Sci. USA 2016, 113, 176–181. [Google Scholar] [CrossRef] [Green Version]
- Norra, C.; Kummer, J.; Boecker, M.; Skobel, E.; Schauerte, P.; Wirtz, M.; Gauggel, S.; Forkmann, T. Poor sleep quality is associated with depressive symptoms in patients with heart disease. Int. J. Behav. Med. 2012, 19, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Peltz, J.S.; Rogge, R.D. The indirect effects of sleep hygiene and environmental factors on depressive symptoms in college students. Sleep Health 2016, 2, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Ghavidel, F.; Fallahi-Khoshknab, M.; Molavynejad, S.; Zarea, K. The role of organizational factors in nurse burnout: Experiences from Iranian nurses working in psychiatric wards. J. Fam. Med. Prim. Care 2019, 8, 3893–3899. [Google Scholar] [CrossRef]
- MacCallum, R.C.; Browne, M.W.; Sugawara, H.M. Power analysis and determination of sample size for covariance structure modeling. Psychol. Methods 1996, 1, 15. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Tsai, P.S.; Wang, S.Y.; Wang, M.Y.; Su, C.T.; Yang, T.T.; Huang, C.J.; Fang, S.C. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual. Life Res. An Int. J. Qual. Life Asp. Treat. Care Rehabil. 2005, 14, 1943–1952. [Google Scholar] [CrossRef]
- Mental Health Foundation. Brief Stress Scale. 2008. Available online: http://www.brainlohas.org/%E7%B2%BE%E7%A5%9E%E5%81%A85%E85%BA%B87%E89%A82%A88%E85%90%91%E87%90%83/ (accessed on 5 March 2021).
- Radloff, L.S. The ces-d scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Chien, C.P.; Cheng, T.A. Depression in Taiwan: Epidemiological survey utilizing CES-D. Seishin Shinkeigaku Zasshi Psychiatr. Neurol. Jpn. 1985, 87, 335–338. [Google Scholar]
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Siegrist, J.; Starke, D.; Chandola, T.; Godin, I.; Marmot, M.; Niedhammer, I.; Peter, R. The measurement of effort-reward imbalance at work: European comparisons. Soc. Sci. Med. 2004, 58, 1483–1499. [Google Scholar] [CrossRef]
- Yeh, W.Y.; Cheng, Y.; Chen, C.J.; Hu, P.Y.; Kristensen, T.S. Psychometric properties of the Chinese version of Copenhagen burnout inventory among employees in two companies in Taiwan. Int. J. Behav. Med. 2007, 14, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Sobel, M.E. Asymptotic intervals for indirect effects in structural equations models. In Sociological Methodology; Leinhart, S., Ed.; Jossey-Bass: San Francisco, CA, USA, 1982; pp. 1290–1312. [Google Scholar]
- Hall, R.J.; Snell, A.F.; Foust, M.S. Item Parceling Strategies in SEM: Investigating the Subtle Effects of Unmodeled Secondary Constructs. Organ. Res. Methods 1999, 2, 233–256. [Google Scholar] [CrossRef]
- Whittaker, T.A. Using the Modification Index and Standardized Expected Parameter Change for Model Modification. J. Exp. Educ. 2012, 80, 26–44. [Google Scholar] [CrossRef]
- Hasan, A.A.; Elsayed, S.; Tumah, H. Occupational stress, coping strategies, and psychological-related outcomes of nurses working in psychiatric hospitals. Perspect. Psychiatr. Care 2018, 54, 514–522. [Google Scholar] [CrossRef]
- Lin, S.H.; Liao, W.C.; Chen, M.Y.; Fan, J.Y. The impact of shift work on nurses’ job stress, sleep quality and self-perceived health status. J. Nurs. Manag. 2014, 22, 604–612. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Family Caregivers Report in Taiwan. 2018. Available online: https://www.mohw.gov.tw/sp-GS-1.html?Query=%E4%B8%BB%E8%A6%81%E7%85%A7%E9%A1%A7%E8%80%85#gsc.tab=0&gsc.q=%E4%B8%BB%E8%A6%81%E7%85%A7%E9%A1%A7%E8%80%85&gsc.sort= (accessed on 5 March 2021).
- Tang, C.S.; Lim, M.S.M.; Koh, J.M.; Cheung, F.Y.L. Emotion Dysregulation Mediating Associations Among Work Stress, Burnout, and Problem Gambling: A Serial Multiple Mediation Model. J. Gambl. Stud. 2019, 35, 813–828. [Google Scholar] [CrossRef] [PubMed]
- Corfield, E.C.; Martin, N.G.; Nyholt, D.R. Co-occurrence and symptomatology of fatigue and depression. Compr. Psychiatry 2016, 71, 1–10. [Google Scholar] [CrossRef]
- Wang, S.M.; Lai, C.Y.; Chang, Y.Y.; Huang, C.Y.; Zauszniewski, J.A.; Yu, C.Y. The relationships among work stress, resourcefulness, and depression level in psychiatric nurses. Arch. Psychiatr. Nurs. 2015, 29, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.L. Folk Belief, Religious Therapy and Base on Religious Beliefs—Tsu Huei Temple’s Ritual of Asking to Gods; Lan Tai Press: Taipei, Taiwan, 2009. [Google Scholar]
 = latent variable;
= latent variable;  = measured variable; → = unidirectional path.
= measured variable; → = unidirectional path.
 = latent variable;
= latent variable;  = measured variable; → = unidirectional path.
= measured variable; → = unidirectional path.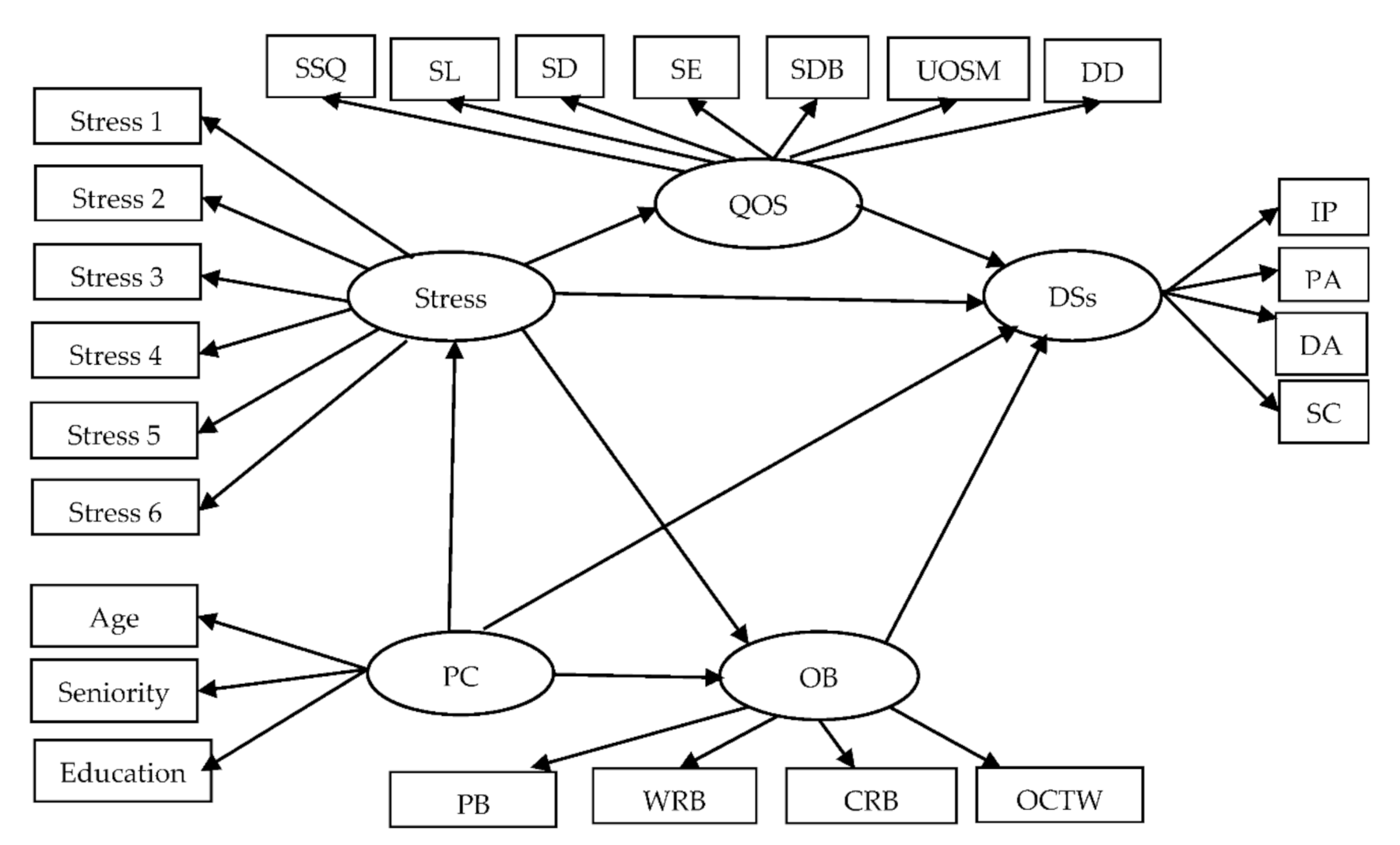
 = latent variable;
= latent variable;  = measured variable; → = unidirectional path; *** = p < 0.001.
= measured variable; → = unidirectional path; *** = p < 0.001.
 = latent variable;
= latent variable;  = measured variable; → = unidirectional path; *** = p < 0.001.
= measured variable; → = unidirectional path; *** = p < 0.001.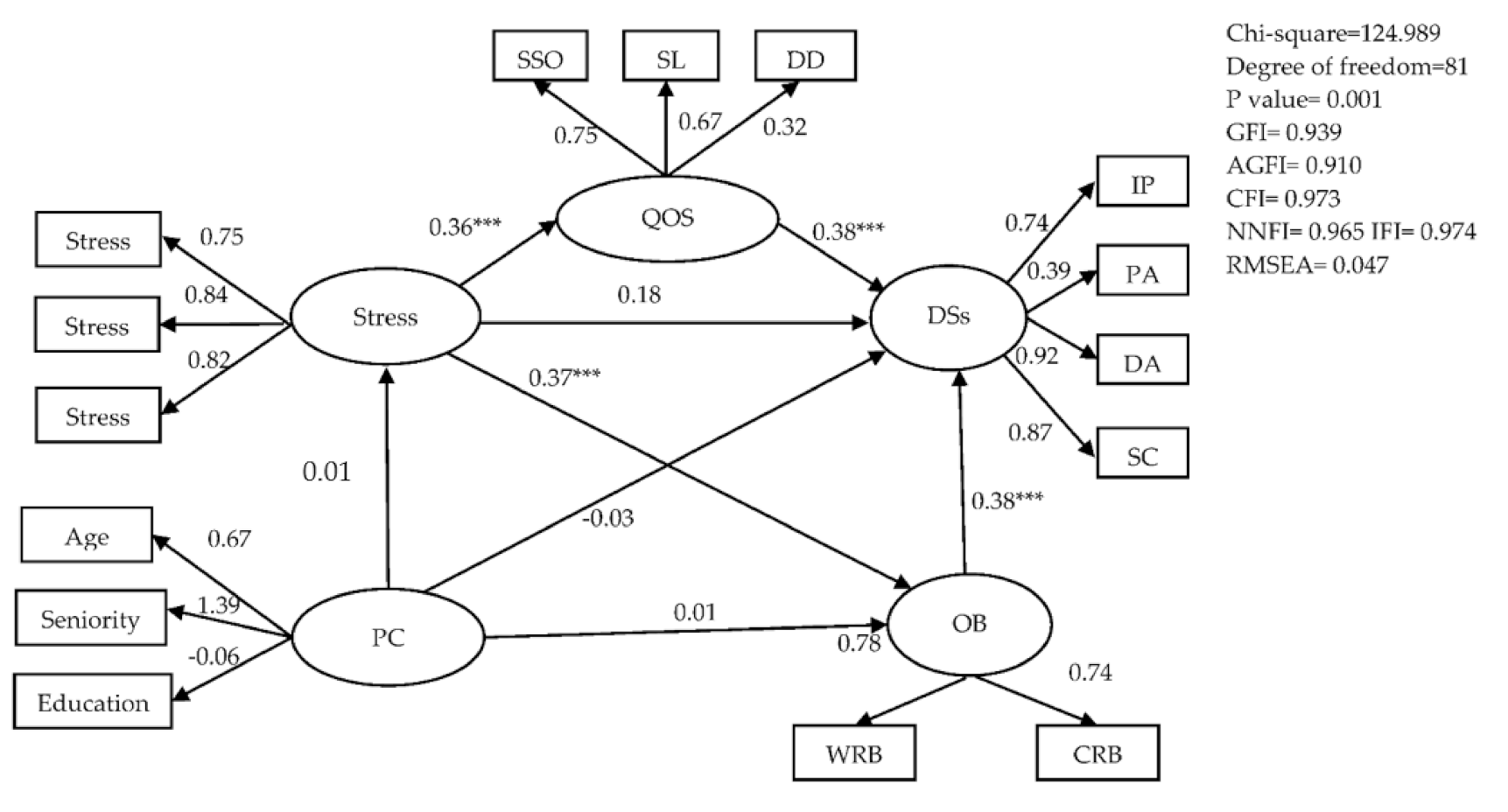
| Relationship | Point Estimate | Product of Coefficients | Percentile | Bootstrapping | ||||
|---|---|---|---|---|---|---|---|---|
| 95% CI | BC 95% CI | |||||||
| SE | Z | Lower | Upper | Lower | Upper | p | ||
| Indirect Effects | ||||||||
| S to QOS to D | 0. 449 | 0.192 | 2.931 | 0.145 | 0.881 | 0.167 | 0.931 | <0.001 *** |
| S to OB to D | 0.448 | 0.189 | 3.285 | 0.141 | 0.876 | 0.179 | 0.963 | <0.001 *** |
| Direct Effects | ||||||||
| S to D direct | 0.567 | 0.323 | 1.755 | −0.081 | 1.213 | −0.087 | 1.210 | 0.081 |
| Total Effects | ||||||||
| S to D total | 0.897 | 0.287 | 3.125 | 0.412 | 1.572 | 0.453 | 1.633 | <0.001 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, H.-F.; Liu, Y.; Hsu, H.-T.; Ma, S.-C.; Wang, H.-H.; Ko, C.-H. Relations between Stress and Depressive Symptoms in Psychiatric Nurses: The Mediating Effects of Sleep Quality and Occupational Burnout. Int. J. Environ. Res. Public Health 2021, 18, 7327. https://doi.org/10.3390/ijerph18147327
Hsieh H-F, Liu Y, Hsu H-T, Ma S-C, Wang H-H, Ko C-H. Relations between Stress and Depressive Symptoms in Psychiatric Nurses: The Mediating Effects of Sleep Quality and Occupational Burnout. International Journal of Environmental Research and Public Health. 2021; 18(14):7327. https://doi.org/10.3390/ijerph18147327
Chicago/Turabian StyleHsieh, Hsiu-Fen, Yi Liu, Hsin-Tien Hsu, Shu-Ching Ma, Hsiu-Hung Wang, and Chih-Hung Ko. 2021. "Relations between Stress and Depressive Symptoms in Psychiatric Nurses: The Mediating Effects of Sleep Quality and Occupational Burnout" International Journal of Environmental Research and Public Health 18, no. 14: 7327. https://doi.org/10.3390/ijerph18147327
APA StyleHsieh, H.-F., Liu, Y., Hsu, H.-T., Ma, S.-C., Wang, H.-H., & Ko, C.-H. (2021). Relations between Stress and Depressive Symptoms in Psychiatric Nurses: The Mediating Effects of Sleep Quality and Occupational Burnout. International Journal of Environmental Research and Public Health, 18(14), 7327. https://doi.org/10.3390/ijerph18147327







