Impact on Health-Related Quality of Life after Different Aerobic Exercise Programs in Physically Inactive Adults with Overweight/Obesity and Primary Hypertension: Data from the EXERDIET-HTA Study
Abstract
1. Introduction
2. Methods
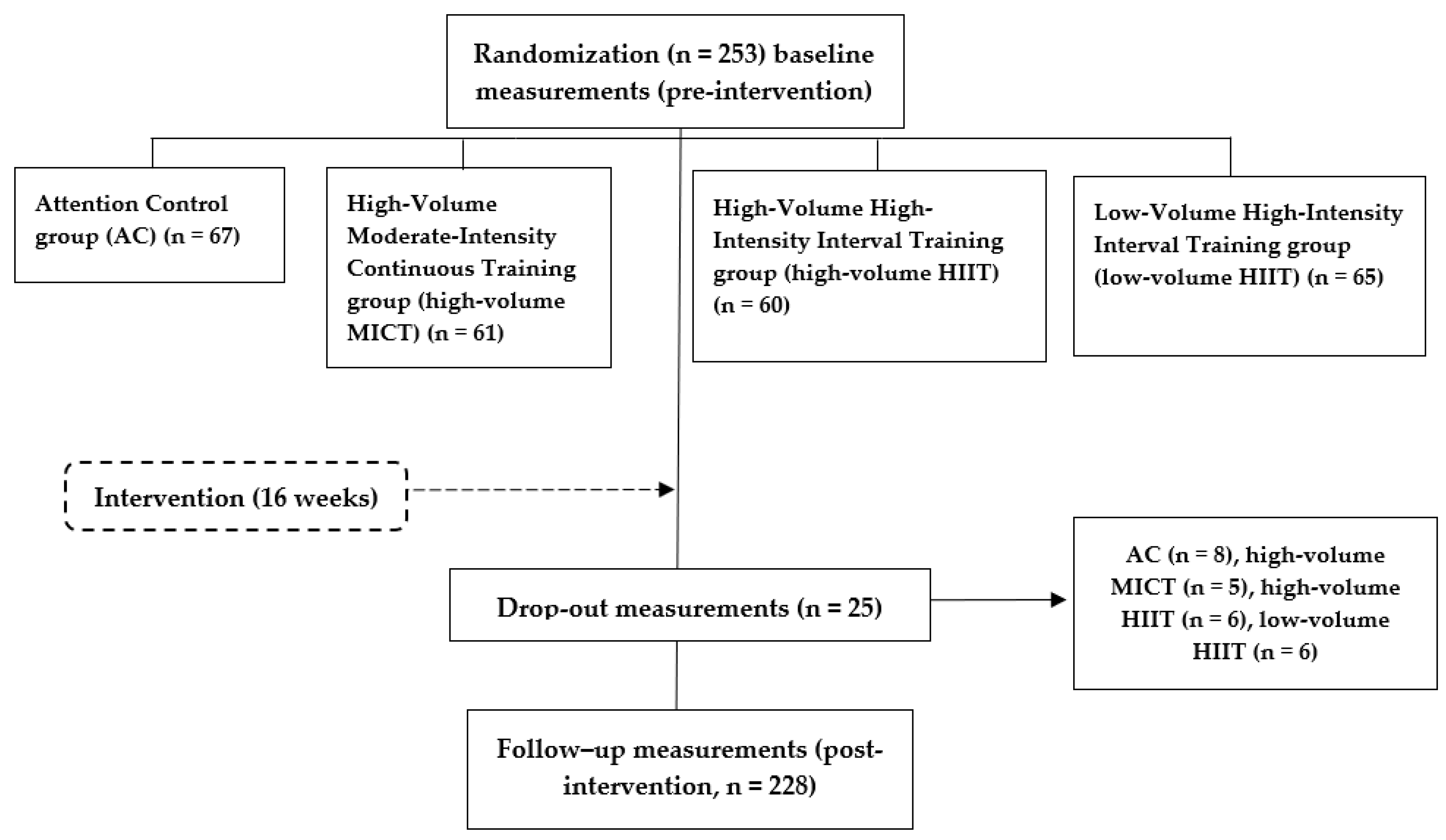
2.1. Study Design
2.2. Participants
2.3. Measurements
2.4. Intervention
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension. Kardiol. Pol. 2019, 77, 71–159. [Google Scholar] [CrossRef]
- Trevisol, D.J.; Moreira, L.B.; Fuchs, F.D.; Fuchs, S.C. Health-Related Quality of Life is Worse in Individuals with Hypertension Under Drug Treatment: Results of Population-Based Study. J. Hum. Hypertens. 2012, 26, 374–380. [Google Scholar] [CrossRef]
- Kitaoka, M.; Mitoma, J.; Asakura, H.; Anyenda, O.E.; Nguyen, T.T.; Hamagishi, T.; Hori, D.; Suzuki, F.; Shibata, A.; Horii, M.; et al. The Relationship between Hypertension and Health-Related Quality of Life: Adjusted by Chronic Pain, Chronic Diseases, and Life Habits in the General Middle-Aged Population in Japan. Environ. Health Prev. Med. 2016, 21, 193–214. [Google Scholar] [CrossRef]
- Pariente Rodrigo, E.; Garcia-Garrido, A.B.; Lara Torres, M.; Garcia Martinez, A.; Montes Perez, M.; Andino Lopez, J.; Otero Cabanillas, N.; Ramos Barron, M.C. Health-Related Quality of Life in Hypertension: A Gender-Differentiated Analysis in Population of Cantabria. Rev. Esp. Salud Publica 2020, 94, e202010139. [Google Scholar]
- Cuspidi, C.; Tadic, M.; Grassi, G.; Mancia, G. Treatment of Hypertension: The ESH/ESC Guidelines Recommendations. Pharmacol. Res. 2018, 128, 315–321. [Google Scholar] [CrossRef]
- Leal, J.M.; Galliano, L.M.; Del Vecchio, F.B. Effectiveness of High-Intensity Interval Training Versus Moderate-Intensity Continuous Training in Hypertensive Patients: A Systematic Review and Meta-Analysis. Curr. Hypertens. Rep. 2020, 22, 26. [Google Scholar] [CrossRef]
- Gorostegi-Anduaga, I.; Corres, P.; MartinezAguirre-Betolaza, A.; Perez-Asenjo, J.; Aispuru, G.R.; Fryer, S.M.; Maldonado-Martin, S. Effects of Different Aerobic Exercise Programmes with Nutritional Intervention in Sedentary Adults with Overweight/Obesity and Hypertension: EXERDIET-HTA Study. Eur. J. Prev. Cardiol. 2018, 25, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Vagetti, G.C.; Barbosa Filho, V.C.; Moreira, N.B.; Oliveira, V.; Mazzardo, O.; Campos, W. Association between Physical Activity and Quality of Life in the Elderly: A Systematic Review, 2000–2012. Braz. J. Psychiatry 2014, 36, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Dechamps, A.; Diolez, P.; Thiaudiere, E.; Tulon, A.; Onifade, C.; Vuong, T.; Helmer, C.; Bourdel-Marchasson, I. Effects of Exercise Programs to Prevent Decline in Health-Related Quality of Life in Highly Deconditioned Institutionalized Elderly Persons: A Randomized Controlled Trial. Arch. Intern. Med. 2010, 170, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Atan, T.; Karavelioglu, Y. Effectiveness of High-Intensity Interval Training Vs Moderate-Intensity Continuous Training in Patients with Fibromyalgia: A Pilot Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2020, 101, 1865–1876. [Google Scholar] [CrossRef] [PubMed]
- Hunt, S.M.; McEwen, J.; McKenna, S.P. Measuring Health Status: A New Tool for Clinicians and Epidemiologists. J. R. Coll. Gen. Pract. 1985, 35, 185–188. [Google Scholar] [PubMed]
- Kind, P.; Carr-Hill, R. The Nottingham Health Profile: A Useful Tool for Epidemiologists? Soc. Sci. Med. 1987, 25, 905–910. [Google Scholar] [CrossRef]
- De Oliveira Paes Leme, M.; Yuan, S.L.K.; Oliveira Magalhaes, M.; Ferreira de Meneses, S.R.; Marques, A.P. Pain and Quality of Life in Knee Osteoarthritis, Chronic Low Back Pain and Fibromyalgia: A Comparative Cross-Sectional Study. Reumatismo 2019, 71, 68–74. [Google Scholar] [CrossRef] [PubMed]
- George, S.M.; Alfano, C.M.; Groves, J.; Karabulut, Z.; Haman, K.L.; Murphy, B.A.; Matthews, C.E. Objectively Measured Sedentary Time is Related to Quality of Life among Cancer Survivors. PLoS ONE 2014, 9, e87937. [Google Scholar] [CrossRef]
- Sanchez-Carazo, J.L.; Lopez-Estebaranz, J.L.; Guisado, C. Comorbidities and Health-Related Quality of Life in Spanish Patients with Moderate to Severe Psoriasis: A Cross-Sectional Study (Arizona Study). J. Dermatol. 2014, 41, 673–678. [Google Scholar] [CrossRef]
- Rebollo-Rubio, A.; Morales-Asencio, J.M.; Pons-Raventos, M.E.; Mansilla-Francisco, J.J. Review of Studies on Health Related Quality of Life in Patients with Advanced Chronic Kidney Disease in Spain. Nefrologia 2015, 35, 92–109. [Google Scholar]
- Tsai, J.C.; Yang, H.Y.; Wang, W.H.; Hsieh, M.H.; Chen, P.T.; Kao, C.C.; Kao, P.F.; Wang, C.H.; Chan, P. The Beneficial Effect of Regular Endurance Exercise Training on Blood Pressure and Quality of Life in Patients with Hypertension. Clin. Exp. Hypertens. 2004, 26, 255–265. [Google Scholar] [CrossRef]
- Arija, V.; Villalobos, F.; Pedret, R.; Vinuesa, A.; Jovani, D.; Pascual, G.; Basora, J. Physical Activity, Cardiovascular Health, Quality of Life and Blood Pressure Control in Hypertensive Subjects: Randomized Clinical Trial. Health Qual. Life Outcomes 2018, 16, 184. [Google Scholar] [CrossRef]
- Maldonado-Martín, S.; Gorostegi-Anduaga, I.; Aispuru, R.; Illera-Villas, M.; Jurio-Iriarte, B.; Francisco-Terreros, S.; Pérez-Asenjo, J. Effects of Different Aerobic Exercise Programs with Nutritional Intervention in Primary Hypertensive and Overweight/Obese Adults: EXERDIET-HTA Controlled Trial. J. Clin. Trials 2016, 6, 1–10. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Bohm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 2013, 31, 1281–1357. [Google Scholar] [CrossRef] [PubMed]
- Mezzani, A.; Hamm, L.F.; Jones, A.M.; McBride, P.E.; Moholdt, T.; Stone, J.A.; Urhausen, A.; Williams, M.A.; European Association for Cardiovascular Prevention and Rehabilitation; American Association of Cardiovascular and Pulmonary Rehabilitation; et al. Aerobic Exercise Intensity Assessment and Prescription in Cardiac Rehabilitation: A Joint Position Statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation, and the Canadian Association of Cardiac Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2012, 32, 327–350. [Google Scholar] [PubMed]
- Task Force of the Italian Working Group on Cardiac Rehabilitation Prevention; Working Group on Cardiac Rehabilitation and Exercise Physiology of the European Society of Cardiology; Piepoli, M.F.; Corra, U.; Agostoni, P.G.; Belardinelli, R.; Cohen-Solal, A.; Hambrecht, R.; Vanhees, L. Statement on Cardiopulmonary Exercise Testing in Chronic Heart Failure due to Left Ventricular Dysfunction: Recommendations for Performance and Interpretation. Part I: Definition of Cardiopulmonary Exercise Testing Parameters for Appropriate use in Chronic Heart Failure. Eur. J. Cardiovasc. Prev. Rehabil. 2006, 13, 150–164. [Google Scholar] [PubMed]
- Alonso, J.; Prieto, L.; Antó, J. La Versión Española Del SF-36 Health Survey (Cuestionario De Salud SF-36): Un Instrumento Para La Medida De Los Resultados Clínicos. Med. Clin. 1995, 104, 771–776. [Google Scholar]
- Ware, J.E.; Snow, K.; Kosinski, M.; Gandek, B. SF-36 Health Survey. Manual and Interpretation Guide; The Health Institute, New England Medical Center: Boston, MA, USA, 1993. [Google Scholar]
- LoMartire, R.; Ang, B.O.; Gerdle, B.; Vixner, L. Psychometric Properties of Short Form-36 Health Survey, EuroQol 5-Dimensions, and Hospital Anxiety and Depression Scale in Patients with Chronic Pain. Pain 2020, 161, 83–95. [Google Scholar] [CrossRef]
- Gargallo Fernandez, M.; Quiles Izquierdo, J.; Basulto Marset, J.; Breton Lesmes, I.; Formiguera Sala, X.; Salas-Salvado, J.; FESNAD-SEEDO Consensus Group. Evidence-Based Nutritional Recommendations for the Prevention and Treatment of Overweight and Obesity in Adults (FESNAD-SEEDO Consensus Document). the Role of Diet in Obesity Prevention (II/III). Nutr. Hosp. 2012, 27, 800–832. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Corres, P.; Fryer, S.M.; Aguirre-Betolaza, A.M.; Gorostegi-Anduaga, I.; Arratibel-Imaz, I.; Perez-Asenjo, J.; Francisco-Terreros, S.; Saracho, R.; Maldonado-Martin, S. A Metabolically Healthy Profile is a Transient Stage when Exercise and Diet are Not Supervised: Long-Term Effects in the EXERDIET-HTA Study. Int. J. Environ. Res. Public. Health 2020, 17, 2830. [Google Scholar] [CrossRef]
- Alonso, J.; Ferrer, M.; Gandek, B.; Ware, J.E., Jr.; Aaronson, N.K.; Mosconi, P.; Rasmussen, N.K.; Bullinger, M.; Fukuhara, S.; Kaasa, S.; et al. Health-Related Quality of Life Associated with Chronic Conditions in Eight Countries: Results from the International Quality of Life Assessment (IQOLA) Project. Qual. Life Res. 2004, 13, 283–298. [Google Scholar] [CrossRef]
- Di Liegro, C.M.; Schiera, G.; Proia, P.; Di Liegro, I. Physical Activity and Brain Health. Genes 2019, 10, 720. [Google Scholar] [CrossRef]
- Matta Mello Portugal, E.; Cevada, T.; Sobral Monteiro-Junior, R.; Teixeira Guimaraes, T.; da Cruz Rubini, E.; Lattari, E.; Blois, C.; Camaz Deslandes, A. Neuroscience of Exercise: From Neurobiology Mechanisms to Mental Health. Neuropsychobiology 2013, 68, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Gorostegi-Anduaga, I.; Maldonado-Martin, S.; MartinezAguirre-Betolaza, A.; Corres, P.; Romaratezabala, E.; Whittaker, A.C.; Francisco-Terreros, S.; Perez-Asenjo, J. Effects on Cardiovascular Risk Scores and Vascular Age After Aerobic Exercise and Nutritional Intervention in Sedentary and Overweight/Obese Adults with Primary Hypertension: The EXERDIET-HTA Randomized Trial Study. High. Blood Press Cardiovasc. Prev. 2018, 25, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Moreira, J.B.N.; Wohlwend, M.; Wisloff, U. Exercise and Cardiac Health: Physiological and Molecular Insights. Nat. Metab. 2020, 2, 829–839. [Google Scholar] [CrossRef] [PubMed]
- Karlsen, T.; Aamot, I.L.; Haykowsky, M.; Rognmo, O. High-Intensity Interval Training for Maximizing Health Outcomes. Prog. Cardiovasc. Dis. 2017, 60, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Battaglia, G.; Bellafiore, M.; Alesi, M.; Paoli, A.; Bianco, A.; Palma, A. Effects of an Adapted Physical Activity Program on Psychophysical Health in Elderly Women. Clin. Interv. Aging 2016, 11, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Pescatello, L.S.; MacDonald, H.V.; Ash, G.I.; Lamberti, L.M.; Farquhar, W.B.; Arena, R.; Johnson, B.T. Assessing the Existing Professional Exercise Recommendations for Hypertension: A Review and Recommendations for Future Research Priorities. Mayo Clin. Proc. 2015, 90, 801–812. [Google Scholar] [CrossRef]
- Guallar-Castillón, P.; Santa-Olalla, P.; Ramón, J.; López, E.; Rodríguez-Artalejo, F. Actividad Física Y Calidad De Vida De La Población Adulta Mayor En España. Med. Clin. 2004, 123, 606–610. [Google Scholar] [CrossRef]
- Yorks, D.M.; Frothingham, C.A.; Schuenke, M.D. Effects of Group Fitness Classes on Stress and Quality of Life of Medical Students. J. Am. Osteopath. Assoc. 2017, 117, e17–e25. [Google Scholar] [CrossRef]
- Reljic, D.; Frenk, F.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Low-Volume High-Intensity Interval Training Improves Cardiometabolic Health, Work Ability and Well-being in Severely Obese Individuals: A Randomized-Controlled Trial Sub-Study. J. Transl. Med. 2020, 18, 419. [Google Scholar] [CrossRef]
- Jung, M.E.; Bourne, J.E.; Little, J.P. Where does HIT Fit? An Examination of the Affective Response to High-Intensity Intervals in Comparison to Continuous Moderate- and Continuous Vigorous-Intensity Exercise in the Exercise Intensity-Affect Continuum. PLoS ONE 2014, 9, e114541. [Google Scholar] [CrossRef]
| EXERDIET-HTA SUBGROUPS | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variables | HEALTHY (n = 30) | EXERDIET-HTA (n = 253) | p HEALTHYvs. EXERDIET-HTA | AC (n = 67) | High-Volume MICT (n = 61) | High-Volume HIIT (n = 60) | Low-Volume HIIT (n = 65) | p Value Subgroups |
| Sex (men/women) | 12/18 | 161/92 | <0.001 | 41/26 | 38/23 | 39/21 | 43/22 | 0.934 |
| Age (yrs) | 40.0 ± 9.0 | 53.7 ± 7.9 | <0.001 | 52.7 ± 8.4 | 54.2 ± 7.2 | 53.0 ± 8.6 | 54.7 ± 7.2 | 0.339 |
| Body mass (kg) | 66.1 ± 10.5 | 91.5 ± 15.2 | <0.001 | 91.3 ± 15.2 | 92.5 ± 16.8 | 90.1 ± 15.1 | 91.3 ± 14.0 | 0.826 |
| BMI (kg/m2) | 23.1 ± 2.6 | 32.1 ± 4.2 | <0.001 | 32.3 ± 4.4 | 32.3 ± 4.4 | 31.7 ± 3.7 | 32.0 ± 4.3 | 0.799 |
| Waist (cm) | 74.7 ± 8.1 | 103.2 ± 11.2 | <0.001 | 103.3 ± 11.1 | 104.1 ± 12.8 | 101.8± 11.0 | 103.1 ± 10,1 | 0.667 |
| SBP (mmHg) | 114.0 ± 6.6 | 135.8 ± 12.1 | <0.001 | 138.2 ± 13.4 | 133.9 ± 11.1 | 134.3 ± 10.0 | 136.5 ± 13.2 | 0.167 |
| DBP (mmHg) | 68.1 ± 7.2 | 78.0 ± 8.1 | <0.001 | 79.0 ± 8.3 | 75.8 ± 8.1 | 78.9 ± 7.6 | 78.5 ± 8.5 | 0.077 |
| V̇O2peak (mL·kg−1·min−1) | 48.1 ± 8.1 | 22.6 ± 5.5 | <0.001 | 23.3 ± 6.3 | 21.8 ± 5.2 | 22.7 ± 4.9 | 22.6 ± 5.5 | 0.451 |
| Physical Functioning | 99.2 ± 2.3 | 88.6 ± 12.2 | <0.001 | 89.2 ± 11.8 | 88.6 ± 12.5 | 89.3 ± 11.2 | 87.2 ± 13.3 | 0.757 |
| Role-Physical | 96.0 ± 18.4 | 90.8 ± 25.0 | 0.165 | 92.5 ± 21.8 | 86.5 ± 28.7 | 94.6 ± 21.6 | 89.6 ± 27.2 | 0.228 |
| Bodily Pain | 81.3 ± 11.2 | 78.2 ± 19.7 | 0.189 | 75.3 ± 19.2 | 78.5 ± 18.7 | 80.9 ± 18.5 | 78.4 ± 22.3 | 0.482 |
| General Health | 82.4 ± 13.0 | 63.3 ± 16.6 | <0.001 | 65.0 ± 18.1 | 63.9 ± 15.2 | 62.4 ± 15.1 | 62.1 ± 17.9 | 0.735 |
| Vitality | 68.7 ± 9.9 | 58.2 ± 15.0 | <0.001 | 58.1 ± 15.6 | 57.6 ± 14.8 | 60.1 ± 14.4 | 56.9± 15.2 | 0.704 |
| Social Functioning | 95.2 ± 10.0 | 88.5 ± 17.2 | 0.002 | 88.8 ± 17.3 | 87.9 ± 16.8 | 89.0 ± 17.1 | 88.3 ± 17.8 | 0.991 |
| Role-Emotional | 91.4 ± 21.0 | 89.5 ± 27.4 | 0.704 | 92.0 ± 24.7 | 85.8 ± 30.7 | 91.7 ± 24.3 | 88.2 ± 29.7 | 0.576 |
| Mental Health | 81.8 ± 7.3 | 76.1 ± 14.2 | <0.001 | 75.0 ± 14.1 | 78.2 ± 12.9 | 76.1 ± 15 | 75.5 ± 14.7 | 0.592 |
| Physical Component Summary | 54.9 ± 4.2 | 50.3 ± 6.6 | <0.001 | 50.4 ± 6.2 | 50.0 ± 7.1 | 51.0 ± 5.8 | 50.0 ± 7.3 | 0.698 |
| Mental Component Summary | 53.1 ± 5.0 | 50.9 ± 8.3 | 0.036 | 50.9± 7.6 | 50.9 ± 8.7 | 51.1 ± 8.5 | 50.5 ± 8.8 | 0.970 |
| Variables | ALL (n = 253) | AC (n = 67) | High-Volume MICT (n = 61) | High-Volume HIIT (n = 60) | Low-VolumeHIIT (n = 65) | pAC vs. ExT | p Value Intergroups |
|---|---|---|---|---|---|---|---|
| Physical Functioning | |||||||
| T0 | 88.9 ± 11.8 | 90.0 ± 10.3 | 88.5 ± 12.6 | 90.0 ± 10.8 | 87.3 ± 13.5 | 0.011 | 0.057 |
| T1 | 93.3 ± 7.9 *× | 91.4 ± 9.9 | 94.1 ± 6.9 * | 94.4 ± 7.5 * | 93.8 ± 6.6 * | ||
| Role-Physical | |||||||
| T0 | 91.8 ± 23.2 | 93.6 ± 20.5 | 89.1 ± 25.8 | 95.4 ± 18.1 | 90.2 ± 25.8 | 0.145 | 0.292 |
| T1 | 93.6 ± 22.2 | 90.2 ± 28.6 | 95.0 ± 18.2 | 94.5 ± 17.8 | 94.5 ± 22.3 | ||
| Bodily Pain | |||||||
| T0 | 78.8 ± 19.1 | 75.4 ± 19.8 | 79.2 ± 17.9 | 82.4 ± 16.4 | 77.8 ± 21.4 | 0.984 | 0.312 |
| T1 | 81.4 ± 20.1 | 78.1 ± 23.5 | 85.5 ± 19.9 | 79.8 ± 19.2 | 82.2 ± 18.4 | ||
| General Health | |||||||
| T0 | 64.1 ± 16.6 | 65.9 ± 18.3 | 64.4 ± 15.1 | 63.5 ± 14.7 | 62.4 ± 17.9 | 0.001 | 0.003 |
| T1 | 71.0 ±17.1 *× | 66.8 ± 21.3 | 70.6 ± 14.6 * | 74.3 ± 15.5 *× | 72.5 ± 15.5 *× | ||
| Vitality | |||||||
| T0 | 59.0 ± 14.9 | 58.5 ± 15.8 | 57.9 ± 15.1 | 61.8 ± 13.5 | 58.0 ± 15.2 | 0.101 | 0.043 |
| T1 | 66.2 ± 13.8 *× | 63.0 ± 15.9 * | 66.3 ± 13.4 * | 66.5 ± 13.5 * | 69.1 ± 11.8 * | ||
| Social Functioning | |||||||
| T0 | 88.9 ± 17.0 | 89.2 ± 17.0 | 88.6 ± 16.7 | 90.0 ± 16.4 | 87.7 ± 18.0 | 0.951 | 0.769 |
| T1 | 92.8 ± 14.6 * | 93.0 ± 13.2 | 91.8 ± 19.6 | 92.5 ± 11.7 | 93.8 ± 13.2 * | ||
| Role-Emotional | |||||||
| T0 | 90.5 ± 26.7 | 93.2 ± 23.8 | 87.3 ± 29.0 | 93.3 ± 23.5 | 88.1 ± 30.2 | 0.100 | 0.157 |
| T1 | 92.0 ± 23.5 | 89.8 ± 26.4 | 92.7 ± 21.9 | 92.1 ± 24.0 | 94.9 ± 18.4 | ||
| Mental Health | |||||||
| T0 | 76.8 ± 14.1 | 76.1 ± 13.7 | 78.6 ± 13.3 | 76.6 ± 15.4 | 76.0 ± 14.2 | 0.287 | 0.509 |
| T1 | 79.5 ± 12.9 * | 77.1 ± 13.5 | 81.3 ± 12.7 | 78.8 ± 14.1 | 80.9 ± 11.3 * | ||
| Physical Component Summary | |||||||
| T0 | 50.6 ± 6.4 | 50.6 ± 6.1 | 50.3 ± 6.8 | 51.4 ± 5.5 | 50.0 ± 7.2 | 0.098 | 0.309 |
| T1 | 52.3 ± 6.1 | 51.1 ± 7.4 | 52.9 ± 5.6* | 53.0 ±5.0 | 52.6 ± 5.8 * | ||
| Mental Component Summary | |||||||
| T0 | 51.2 ± 8.3 | 51.3 ± 7.4 | 51.2 ± 8.8 | 51.6 ± 8.5 | 50.7 ± 8.7 | 0.329 | 0.396 |
| T1 | 52.8 ± 7.3 | 52.0 ± 8.2 | 53.0 ± 8.1 | 52.5 ± 7.2 | 53.9 ± 5.3 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tous-Espelosín, M.; Gorostegi-Anduaga, I.; Corres, P.; MartinezAguirre-Betolaza, A.; Maldonado-Martín, S. Impact on Health-Related Quality of Life after Different Aerobic Exercise Programs in Physically Inactive Adults with Overweight/Obesity and Primary Hypertension: Data from the EXERDIET-HTA Study. Int. J. Environ. Res. Public Health 2020, 17, 9349. https://doi.org/10.3390/ijerph17249349
Tous-Espelosín M, Gorostegi-Anduaga I, Corres P, MartinezAguirre-Betolaza A, Maldonado-Martín S. Impact on Health-Related Quality of Life after Different Aerobic Exercise Programs in Physically Inactive Adults with Overweight/Obesity and Primary Hypertension: Data from the EXERDIET-HTA Study. International Journal of Environmental Research and Public Health. 2020; 17(24):9349. https://doi.org/10.3390/ijerph17249349
Chicago/Turabian StyleTous-Espelosín, Mikel, Ilargi Gorostegi-Anduaga, Pablo Corres, Aitor MartinezAguirre-Betolaza, and Sara Maldonado-Martín. 2020. "Impact on Health-Related Quality of Life after Different Aerobic Exercise Programs in Physically Inactive Adults with Overweight/Obesity and Primary Hypertension: Data from the EXERDIET-HTA Study" International Journal of Environmental Research and Public Health 17, no. 24: 9349. https://doi.org/10.3390/ijerph17249349
APA StyleTous-Espelosín, M., Gorostegi-Anduaga, I., Corres, P., MartinezAguirre-Betolaza, A., & Maldonado-Martín, S. (2020). Impact on Health-Related Quality of Life after Different Aerobic Exercise Programs in Physically Inactive Adults with Overweight/Obesity and Primary Hypertension: Data from the EXERDIET-HTA Study. International Journal of Environmental Research and Public Health, 17(24), 9349. https://doi.org/10.3390/ijerph17249349





