Preconception Care Program for Women with Inflammatory Bowel Disease Using Intervention Mapping: A Protocol for Program Development
Abstract
1. Introduction
2. Materials and Methods
2.1. IM Step 1: Logic Model of the Problem (Needs Assessment)
2.1.1. In-Depth Individual Interviews
2.1.2. Literature Review
2.2. IM Step 2: Program Outcomes and Objectives, Logic Model of Change
2.3. IM Step 3: Program Design
2.4. IM Step 4: Program Production
3. Results
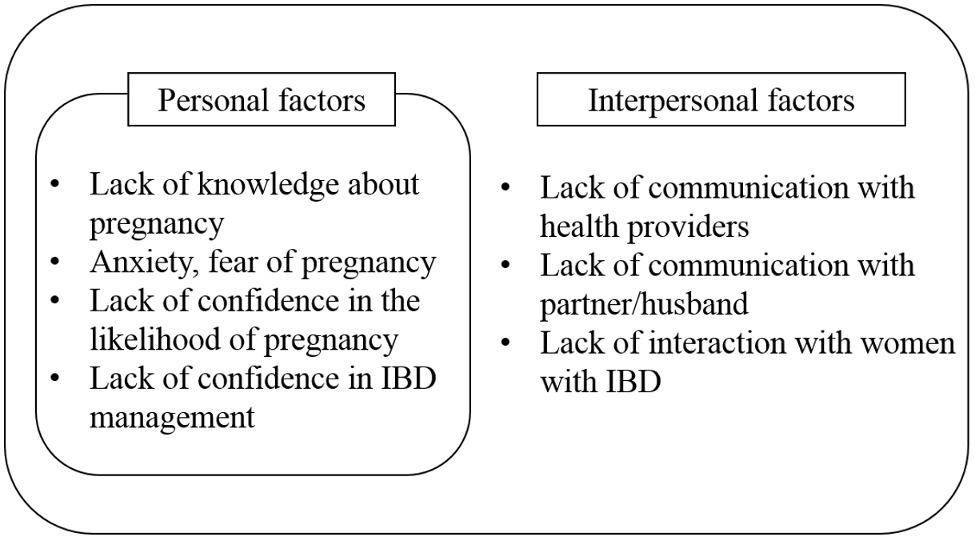
3.1. IM Step 1: Logic Model of the Problem (Needs Assessment)
3.1.1. In-Depth Individual Interviews
3.1.2. Literature Review
3.2. IM Step 2: Program Outcomes and Objectives: Logic Model of Change
3.3. IM Step 3: Program Design
3.4. IM Step 4: Program Production
3.4.1. Development of the Program
Preliminary Program Development
Program Validation
Pilot Testing
Final Program
3.4.2. Development of Materials
Workbook
Preconception Care Diaries
Video Clips
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Zhang, Y.-Z. Inflammatory bowel disease: Pathogenesis. World J. Gastroenterol. 2014, 20, 91–99. [Google Scholar] [CrossRef]
- Patel, N.; Yarur, A.J. Inflammatory Bowel Disease and Pregnancy. In Gastrointestinal and Liver Disorders in Women’s Health; Beniwal-Patel, P., Shaker, R., Eds.; Springer Nature: Cham, Switzerland, 2019; pp. 313–329. [Google Scholar]
- O’Toole, A.; Nwanne, O.; Tomlinson, T. Inflammatory Bowel Disease Increases Risk of Adverse Pregnancy Outcomes: A Meta-Analysis. Dig. Dis. Sci. 2015, 60, 2750–2761. [Google Scholar] [CrossRef]
- Lee, H.H.; Bae, J.; Lee, B.-I.; Lee, K.-M.; Wie, J.H.; Kim, J.S.; Cho, Y.-S.; Jung, S.-A.; Kim, S.W.; Choi, H.; et al. Pregnancy outcomes in women with inflammatory bowel disease: A 10-year nationwide population-based cohort study. Aliment. Pharmacol. Ther. 2020, 51, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Hendy, P.; Chadwick, G.; Hart, A. IBD: Reproductive health, pregnancy and lactation. Front. Gastroenterol. 2014, 6, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Ng, W.K.; Wong, S.H.; Ng, S.C. Changing epidemiological trends of inflammatory bowel disease in Asia. Intestig. Res. 2016, 14, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Yun, S.; Kim, J.-H.; Park, J.Y.; Kim, H.Y.; Kim, Y.-H.; Chang, D.K.; Kim, J.S.; Song, I.S.; Park, J.B.; et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986–2005: A KASID study. Inflamm. Bowel Dis. 2008, 14, 542–549. [Google Scholar] [CrossRef]
- Jung, Y.S.; Han, M.; Kim, W.H.; Park, S.; Cheon, J.H. Incidence and Clinical Outcomes of Inflammatory Bowel Disease in South Korea, 2011–2014: A Nationwide Population-Based Study. Dig. Dis. Sci. 2017, 62, 2102–2112. [Google Scholar] [CrossRef]
- Stephansson, O.; Larsson, H.; Pedersen, L.; Kieler, H.; Granath, F.; Ludvigsson, J.F.; Falconer, H.; Ekbom, A.; Sørensen, H.T.; Nørgaard, M. Crohn’s Disease Is a Risk Factor for Preterm Birth. Clin. Gastroenterol. Hepatol. 2010, 8, 509–515. [Google Scholar] [CrossRef]
- Gawron, L.M.; Sanders, J.; Steele, K.P.; Flynn, A.D. Reproductive Planning and Contraception for Women with Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2016, 22, 459–464. [Google Scholar] [CrossRef]
- Johnson, K.; Posner, S.F.; Biermann, J.; Cordero, J.F.; Atrash, H.K.; Parker, C.S.; Boulet, S.; Curtis, M.G. Recommendations to Improve Preconception Health and Health Care--United States: A Report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm. Rep. 2006, 55, 1–23. [Google Scholar] [CrossRef]
- Dunlop, A.L.; Jack, B.W.; Bottalico, J.N.; Lu, M.C.; James, A.; Shellhaas, C.S.; Hallstrom, L.H.-K.; Solomon, B.D.; Feero, W.G.; Menard, M.K.; et al. The clinical content of preconception care: Women with chronic medical conditions. Am. J. Obstet. Gynecol. 2008, 199, S310–S327. [Google Scholar] [CrossRef] [PubMed]
- Selinger, C.P.; Lal, S.; Eaden, J.; Jones, D.B.; Katelaris, P.; Chapman, G.; McDonald, C.; Leong, R.W.; McLaughlin, J.T. Better disease specific patient knowledge is associated with greater anxiety in inflammatory bowel disease. J. Crohns Colitis. 2013, 7, e214–e218. [Google Scholar] [CrossRef] [PubMed]
- Rottenstreich, A.; Shitrit, A.B.-G. Preconception counseling of females with inflammatory bowel disease. Best Pract. Res. Clin. Gastroenterol. 2020, 44, 101666. [Google Scholar] [CrossRef] [PubMed]
- Hauser, G.; Plavšić, I.; Štimac, T. Crohn’s disease in women. Int. J. Women’s Health 2013, 5, 681–688. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kamp, K.; West, P.; Holmstrom, A.; Luo, Z.; Wyatt, G.; Given, B. Systematic Review of Social Support on Psychological Symptoms and Self-Management Behaviors Among Adults with Inflammatory Bowel Disease. J. Nurs. Sch. 2019, 51, 380–389. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Jung, S.-A.; Lee, K.-M.; Park, S.J.; Kim, T.O.; Choi, C.H.; Kim, H.G.; Moon, W.; Moon, C.M.; Song, H.K.; et al. Impact of inflammatory bowel disease on daily life: An online survey by the Korean Association for the Study of Intestinal Diseases. Intestig. Res. 2017, 15, 338–344. [Google Scholar] [CrossRef][Green Version]
- Lee, Y.N. Illness Perception, Disease-Related Knowledge and Self-Care Behavior in Patients with Crohn’s Disease. Master’s Thesis, Yonsei University, Seoul, Korea, February 2018. Available online: https://ir.ymlib.yonsei.ac.kr/handle/22282913/160040 (accessed on 23 October 2020).
- Mountifield, R.; Andrews, J.M.; Bampton, P.A. It IS worth the effort: Patient knowledge of reproductive aspects of inflammatory bowel disease improves dramatically after a single group education session. J. Crohns Colitis 2014, 8, 796–801. [Google Scholar] [CrossRef]
- Wierstra, K.; Sutton, R.T.; Bal, J.; Ismond, K.; Dieleman, L.; Halloran, B.P.; Kroeker, K.; Fedorak, R.N.; Berga, K.-A.; Huang, V.M. Innovative Online Educational Portal Improves Disease-Specific Reproductive Knowledge among Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2018, 24, 2483–2493. [Google Scholar] [CrossRef]
- Bartholomew, L.K.; Parcel, G.S.; Kok, G. Intervention Mapping: A Process for Developing Theory and Evidence-Based Health Education Programs. Health Educ. Behav. 1998, 25, 545–563. [Google Scholar] [CrossRef]
- Brendryen, H.; Kraft, P.; Schaalma, H. Looking Inside the Black Box: Using Intervention Mapping to Describe the Development of the Automated Smoking Cessation Intervention ‘Happy Ending’. J. Smok. Cessat. 2010, 5, 29–56. [Google Scholar] [CrossRef]
- Highfield, L.; Bartholomew, L.K.; Hartman, M.; Ford, M.M.; Balihe, P. Grounding Evidence-Based Approaches to Cancer Prevention in the Community. Health Promot. Pract. 2014, 15, 904–914. [Google Scholar] [CrossRef]
- Kim, S.; Ko, Y.H.; Song, Y.; Kang, M.J.; Lee, H.; Kim, S.H.; Jeon, J.Y.; Cho, Y.U.; Yi, G.; Han, J. Development of an exercise adherence program for breast cancer survivors with cancer-related fatigue—An intervention mapping approach. Support. Care Cancer 2019, 27, 4745–4752. [Google Scholar] [CrossRef] [PubMed]
- Springvloet, L.; Lechner, L.; Oenema, A. Planned development and evaluation protocol of two versions of a web-based computer-tailored nutrition education intervention aimed at adults, including cognitive and environmental feedback. BMC Public Health 2014, 14, 47. [Google Scholar] [CrossRef] [PubMed]
- Ahn, Y.H. Using Intervention Mapping to Develop a Community-based Disease Self-management Support Program for Patients with Osteoarthritis. J. Muscle Jt. Health 2015, 22, 245–257. [Google Scholar] [CrossRef]
- Sakakibara, B.M.; Lear, S.A.; Barr, S.I.; Benavente, O.; Goldsmith, C.H.; Silverberg, N.D.; Yao, J.; Eng, J. Development of a Chronic Disease Management Program for Stroke Survivors Using Intervention Mapping: The Stroke Coach. Arch. Phys. Med. Rehabil. 2017, 98, 1195–1202. [Google Scholar] [CrossRef] [PubMed]
- Decat, P.; Nelson, E.; De Meyer, S.; Jaruseviciene, L.; Orozco, M.; Segura, Z.; Gorter, A.; Vega, B.; Cordova-Pozo, K.L.; Maes, L.; et al. Community embedded reproductive health interventions for adolescents in Latin America: Development and evaluation of a complex multi-centre intervention. BMC Public Health 2013, 13, 31. [Google Scholar] [CrossRef]
- Draper, C.E.; Micklesfield, L.K.; Kahn, K.; Tollman, S.; Pettifor, J.M.; Dunger, D.B.; A Norris, S. Application of Intervention Mapping to develop a community-based health promotion pre-pregnancy intervention for adolescent girls in rural South Africa: Project Ntshembo (Hope). BMC Public Health 2014, 14, S5. [Google Scholar] [CrossRef]
- Hicking-Woodison, L. Planning Health Promotion Programs: An Intervention Mapping Approach. Nurs. Stand. 2017, 32, 33. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Marri, S.R.; Ahn, C.; Buchman, A.L. Voluntary childlessness is increased in women with inflammatory bowel disease. Inflamm. Bowel Dis. 2007, 13, 591–599. [Google Scholar] [CrossRef]
- Purewal, S.; Chapman, S.; Czuber-Dochan, W.; Selinger, C.P.; Steed, H.; Brookes, M.J. Systematic review: The consequences of psychosocial effects of inflammatory bowel disease on patients′ reproductive health. Aliment. Pharmacol. Ther. 2018, 48, 1202–1212. [Google Scholar] [CrossRef] [PubMed]
- Selinger, C.P.; Ghorayeb, J.; Madill, A. What Factors Might Drive Voluntary Childlessness (VC) in Women with IBD? Does IBD-specific Pregnancy-related Knowledge Matter? J. Crohns Colitis 2016, 10, 1151–1158. [Google Scholar] [CrossRef] [PubMed]
- Ellul, P.; Zammita, S.C.; Katsanos, K.H.; Cesarini, M.; Allocca, M.; Danese, S.; Karatzas, P.; Moreno, S.C.; Kopylov, U.; Fiorino, G.; et al. Perception of Reproductive Health in Women with Inflammatory Bowel Disease. J. Crohns Colitis 2016, 10, 886–891. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.D.; Fisher, W.A. Changing AIDS-risk behavior. Psychol. Bull. 1992, 111, 455–474. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Hupcey, J.E. Clarifying the social support theory-research linkage. J. Adv. Nurs. 1998, 27, 1231–1241. [Google Scholar] [CrossRef]
- Fisher, J.D.; Fisher, W.A.; Bryan, A.D.; Misovich, S.J. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002, 21, 177–186. [Google Scholar] [CrossRef]
- Mahadevan, U.; Robinson, C.; Bernasko, N.; Boland, B.; Chambers, C.; Dubinsky, M.; Friedman, S.; Kane, S.; Manthey, J.; Sauberan, J.; et al. Inflammatory Bowel Disease in Pregnancy Clinical Care Pathway: A Report From the American Gastroenterological Association IBD Parenthood Project Working Group. Inflamm. Bowel Dis. 2019, 25, 627–641. [Google Scholar] [CrossRef]
- Van Der Woude, C.J.; Ardizzone, S.; Bengtson, M.; Fiorino, G.; Fraser, G.; Katsanos, K.H.; Kolacek, S.; Juillerat, P.; Mulders, A.; Pedersen, N.; et al. The Second European Evidenced-Based Consensus on Reproduction and Pregnancy in Inflammatory Bowel Disease. J. Crohns Colitis 2015, 9, 107–124. [Google Scholar] [CrossRef]
- Sung, N.J.; Lee, D.U.; Park, K.H. Suitability Assessment of Patients’ Education Materials Made by Korean Academy of Family Medicine. Korean J. Fam. Med. 2004, 25, 669–677. [Google Scholar]
- Tu, W.; Du, S.; Xu, G. Structure and content components of self-management interventions that improve health-related quality of life in people with inflammatory bowel disease: A systematic review, meta-analysis and meta-regression. J. Clin. Nurs. 2015, 24, 2695–2709. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.E.; Jung, S.-A.; Yoon, H.; Park, S.H.; Moon, C.M.; Kim, E.S.; Kim, S.-E.; Yang, S. Factors associated with pregnancy-related knowledge in women of reproductive age with inflammatory bowel disease. Scand. J. Gastroenterol. 2017, 52, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.D. Effects of the Self-Management Program Based on IMB Model for Inflammatory Bowel Disease Patients. Ph.D. Thesis, Kyungpook National University, Daegu, Korea, February 2018. [Google Scholar]
- Magharei, M.; Jaafari, S.; Mansouri, P.; Safarpour, A.; Taghavi, S.A. Effects of Self-Management Education on Self-Efficacy and Quality of Life in Patients with Ulcerative Colitis: A Randomized Controlled Clinical Trial. Int. J. Community Based Nurs. Midwifery 2019, 7, 32–42. [Google Scholar] [PubMed]
- Reusch, A.; Weiland, R.; Gerlich, C.; Dreger, K.; Derra, C.; Mainos, D.; Tuschhoff, T.; Berding, A.; Witte, C.; Kaltz, B.; et al. Self-management education for rehabilitation inpatients suffering from inflammatory bowel disease: A cluster-randomized controlled trial. Health Educ. Res. 2016, 31, 782–791. [Google Scholar] [CrossRef]
- Trachter, A.B.; Rogers, A.I.; Leiblum, S.R. Inflammatory bowel disease in women: Impact on relationship and sexual health. Inflamm. Bowel Dis. 2002, 8, 413–421. [Google Scholar] [CrossRef]
- Miki, Y.; Hohashi, N. Actual conditions of sexuality and sexual perceptions among IBD patients in Japan. J. Med. Care Res. Rev. 2018, 1, 1–7. [Google Scholar]
- Gawron, L.M.; Hammond, C.; Keefer, L. Documentation of reproductive health counseling and contraception in women with inflammatory bowel diseases. Patient Educ. Couns. 2013, 94, 134–137. [Google Scholar] [CrossRef]
- Con, D.; De Cruz, P.; Van Mierlo, T.; Aramaki, E. Mobile Phone Apps for Inflammatory Bowel Disease Self-Management: A Systematic Assessment of Content and Tools. JMIR mHealth uHealth 2016, 4, e13. [Google Scholar] [CrossRef]
- Ali, T.; Madhoun, M.F.; Orr, W.C.; Rubin, D.T. Assessment of the Relationship Between Quality of Sleep and Disease Activity in Inflammatory Bowel Disease Patients. Inflamm. Bowel Dis. 2013, 19, 2440–2443. [Google Scholar] [CrossRef]
- Cosnes, J. Smoking, Physical Activity, Nutrition and Lifestyle: Environmental Factors and Their Impact on IBD. Dig. Dis. 2010, 28, 411–417. [Google Scholar] [CrossRef]
- Halmos, E.P.; Gibson, P.R. Dietary management of IBD—Insights and advice. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 133–146. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, A.; Korzenik, J. Environmental Triggers for IBD. Curr. Gastroenterol. Rep. 2014, 16, 396. [Google Scholar] [CrossRef]
- Czeizel, A.E.; Czeizel, B.; Vereczkey, A. The Participation of Prospective Fathers in Preconception Care. Clin. Med. Insights Reprod. Health 2013, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
| No | Age | Diagnosis | Age at Last Childbirth | Number of Children | Gestation (Weeks) | Childbirth Method | Interview Time (min) |
|---|---|---|---|---|---|---|---|
| 1 | 37 | CD | 35 | 2 | 37, 34 | NSVD | 67 |
| 2 | 39 | CD | 32 | 1 | 39 | C/sec | 75 |
| 3 | 40 | CD | 37 | 1 | 37 | C/sec | 60 |
| 4 | 39 | CD | 35 | 2 | 33 * | NSVD | 56 |
| 5 | 39 | CD | 35 | 1 | 37 | NSVD | 74 |
| 6 | 39 | CD | 37 | 1 | 39 | C/sec | 90 |
| 7 | 41 | UC | 40 | 2 | 38, 37 | NSVD | 60 |
| 8 | 45 | CD | 36 | 2 | 39, 35 | NSVD | 90 |
| 9 | 41 | UC | 39 | 1 | 38 | C/sec | 50 |
| 10 | 41 | UC | 35 | 2 | 41, 38 | C/sec | 80 |
| Program Goal: Women with IBD Should be Prepared before Pregnancy | ||||
|---|---|---|---|---|
| Program Objective: Women with IBD Should Be Prepared for Pregnancy While Maintaining Remission for at Least 3 Months. | ||||
| Performance Objectives | Personal Determinants | Interpersonal Determinant | ||
| Knowledge (K) | Attitude/Motivation (AM) | Self-Efficacy (SE) | Social Interaction (SI) | |
| PO1. Practice pregnancy planning | K. 1a. Understand and explain fertility and pregnancy outcomes of women with IBD. K. 1b. Understand and explain the importance of planned pregnancy. K. 1c. Understand and explain types of contraception. | AM. 1a. Express positive feelings about pregnancy with IBD. AM. 1b. State an increased motivation for planning pregnancy. AM. 1c. State an increased motivation for contraception to avoid unwanted pregnancy. | SE. 1a. Express confidence in staying healthy for pregnancy. SE. 1b. Express confidence in the ability to practice pregnancy planning. SE. 1c. Express confidence in the ability to practice contraception to avoid unwanted pregnancy. | SI. 1a. Communicate with husband/partner about the appropriate time for pregnancy SI. 1b. Communicate with husband/partner about preconception behavior. SI. 1c. Communicate with husband/partner about the contraceptive method to avoid unwanted pregnancy. |
| PO2. Take medicine as prescribed | K. 2. Understand and explain what types of IBD medications can be taken before pregnancy. | AM. 2a. Express positive feelings about taking IBD medicine before pregnancy. AM. 2b. State an increased motivation to take medicine as prescribed. | SE. 2. Express confidence in taking medicine as prescribed. | SI. 2a. Communicate with peers about their experience of medication. SI. 2b. Communicate with a healthcare provider about medication. |
| PO3. Perform regular exercise | K. 3a. Understand and explain the effects of exercise for symptom relief of IBD. K. 3b. Understand and explain whether exercise is important when preparing for pregnancy. | AM. 3a. Express positive feelings about regular exercise. AM. 3b. State an increased motivation to exercise regularly. | SE. 3. Express confidence in exercising regularly. | SI. 3. Communicate with peers about experiences of exercising. |
| PO4. Consume healthy foods | K. 4a. Understand and explain what foods make IBD symptoms worse. K. 4b. Understand and explain the importance and dosage of folic acid to take appropriately depending on the IBD condition. | AM. 4a. State an increased motivation to avoid foods that make IBD symptoms worse. AM. 4b. State an increased motivation to take folic acid. | SE. 4a. Express confidence in avoiding foods that make IBD symptoms worse. SE. 4c. Express confidence in taking folic acid. | SI. 4a. Communicate with peers about experiences of dietary management for IBD. SI 4b. Communicate with a healthcare provider about the appropriate folic acid dosage for pregnancy. |
| PO5. Stop smoking and drinking alcohol | K. 5. Understand and explain the need to stop drinking alcohol and quit smoking before pregnancy. | AM. 5. State an increased motivation to stop drinking alcohol and quit smoking. | SE. 5. Express confidence in stopping alcohol and quitting smoking. | SI. 5. Communicate with the peers about experiences of stopping drinking alcohol and quitting smoking. |
| PO6. Receivecounseling aboutpregnancy with a healthcare provider. | K. 6. Understand and explain the importance of counseling with a healthcare provider before pregnancy for women with chronic conditions. | AM. 6a. Express positive feelings about counseling about pregnancy with a healthcare AM. 6b. State an increased motivation for gastroenterological and gynecological examinations before pregnancy. | SE. 6a. Express confidence in communicating with a healthcare provider SE. 6b. Express confidence in gastroenterological and gynecological examinations | SI.6. Communicate with a healthcare provider about the appropriate time for pregnancy. |
| Theoretical Basis for Determinant | Determinant | Change Objective | Methods (Theory) | Strategies and Practical Applications |
|---|---|---|---|---|
| Information–motivation–behavioral skills (IMB) model | Knowledge | Increased knowledge of pregnancy and preconception care for women with IBD | ∙ Providing information (IMB model) | ∙ Providing information: small group lectures, social networking service messages, workbook |
| Attitude/motivation | Positive attitude toward pregnancy and pre-pregnancy preparation, and promotion of motivation to prepare for pregnancy | ∙ Emotional arousal (self-efficacy theory) ∙ Verbal persuasion (self-efficacy theory) ∙ Vicarious experience (self-efficacy theory) | ∙ Writing a letter to their child to be born: workbook ∙ Supporting and motivating: individual tele-coaching ∙ Sharing the experience of women with IBD who have experienced pregnancy and childbirth: video clip | |
| Self-efficacy theory | Self-efficacy | Confidence in preconception management and improvement in IBD disease management in women with IBD | ∙ Performance accomplishments (self-efficacy theory) ∙ Vicarious experience (self-efficacy theory) ∙ Verbal persuasion (self-efficacy theory) | ∙ Participants keep records and monitor preconception behavior : Preconception diary. ∙ Sharing positive and negative experiences of others: small group discussion ∙ Identifying difficulties of disease management in everyday life and finding solutions: individual tele-coaching |
| Social support theory | Social interaction | Improvement in communication skills with peers, husband/partner, and health providers | ∙ Enhancing communication (social support theory) | ∙ Support from peers during small group discussions ∙ Talking to husband/partner or health provider about preconception care: home activity |
| Session | Theme | Methods | Topics and Activities | Tools/Materials |
|---|---|---|---|---|
| 1 | Managing myself for IBD | Lecture | - IBD and current treatment trends - Reproductive health in women with IBD - Fertility of women with IBD - Birth outcomes of women with IBD - 10 commandments of IBD management in daily life - Guideline for reproductive health diary | ·PowerPoint ·Workbook |
| Group work | - Sharing disease management experiences - Checking disease-related knowledge | ·Workbook | ||
| 2 | Smart preparation for healthy pregnancy | Lecture | - Preconception behavior of women with IBD - Medication before pregnancy - Laboratory and imaging exams before pregnancy - Importance of pregnancy planning, contraception - Men’s preconception care | ·PowerPoint ·Workbook ·Video clip |
| Group work | - Sharing experiences of symptom management - Sharing impressions | ·Workbook ·Preconceptiondiary | ||
| Tele-coaching | - Identifying difficulties of disease management in everyday life and finding solutions | ·Coaching guide ·Preconception diary | ||
| 3 | Smart preparation for healthychildbirth | Lecture | - Management during pregnancy - Laboratory and imaging exams during pregnancy - Childbirth methods for women with IBD - Postpartum care - Breastfeeding and medication - Immunization of the newborn | ·PowerPoint ·Workbook |
| Group work | - Talking about reproductive health management and current pre-pregnancy health behavior practiced by participants - Sharing thoughts about care during pregnancy - Checking delivery knowledge related to IBD - Sharing impressions | ·Workbook ·Preconceptiondiary | ||
| 4 | Get ready to have my baby! | Lecture | - Sharing the experience of women with IBD who have experienced pregnancy and childbirth | ·PowerPoint ·Workbook ·Video clip |
| Group work | - Talking to each other about changes in thoughts about pregnancy - Writing a letter to my child to be born - Sharing own feelings about the whole program | ·Workbook ·Preconception diary | ||
| Tele-coaching | - Identifying difficulties of disease management in everyday life and finding solutions | ·Coaching guide ·Preconception diary |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.J.; Kim, Y.H.; Kim, H.W. Preconception Care Program for Women with Inflammatory Bowel Disease Using Intervention Mapping: A Protocol for Program Development. Int. J. Environ. Res. Public Health 2020, 17, 9365. https://doi.org/10.3390/ijerph17249365
Lee YJ, Kim YH, Kim HW. Preconception Care Program for Women with Inflammatory Bowel Disease Using Intervention Mapping: A Protocol for Program Development. International Journal of Environmental Research and Public Health. 2020; 17(24):9365. https://doi.org/10.3390/ijerph17249365
Chicago/Turabian StyleLee, Young Jin, Yeon Hee Kim, and Hae Won Kim. 2020. "Preconception Care Program for Women with Inflammatory Bowel Disease Using Intervention Mapping: A Protocol for Program Development" International Journal of Environmental Research and Public Health 17, no. 24: 9365. https://doi.org/10.3390/ijerph17249365
APA StyleLee, Y. J., Kim, Y. H., & Kim, H. W. (2020). Preconception Care Program for Women with Inflammatory Bowel Disease Using Intervention Mapping: A Protocol for Program Development. International Journal of Environmental Research and Public Health, 17(24), 9365. https://doi.org/10.3390/ijerph17249365





