Simulation and Improvement of Patients’ Workflow in Heart Clinics during COVID-19 Pandemic Using Timed Coloured Petri Nets
Abstract
1. Introduction
2. Literature Review
3. Research Methodology
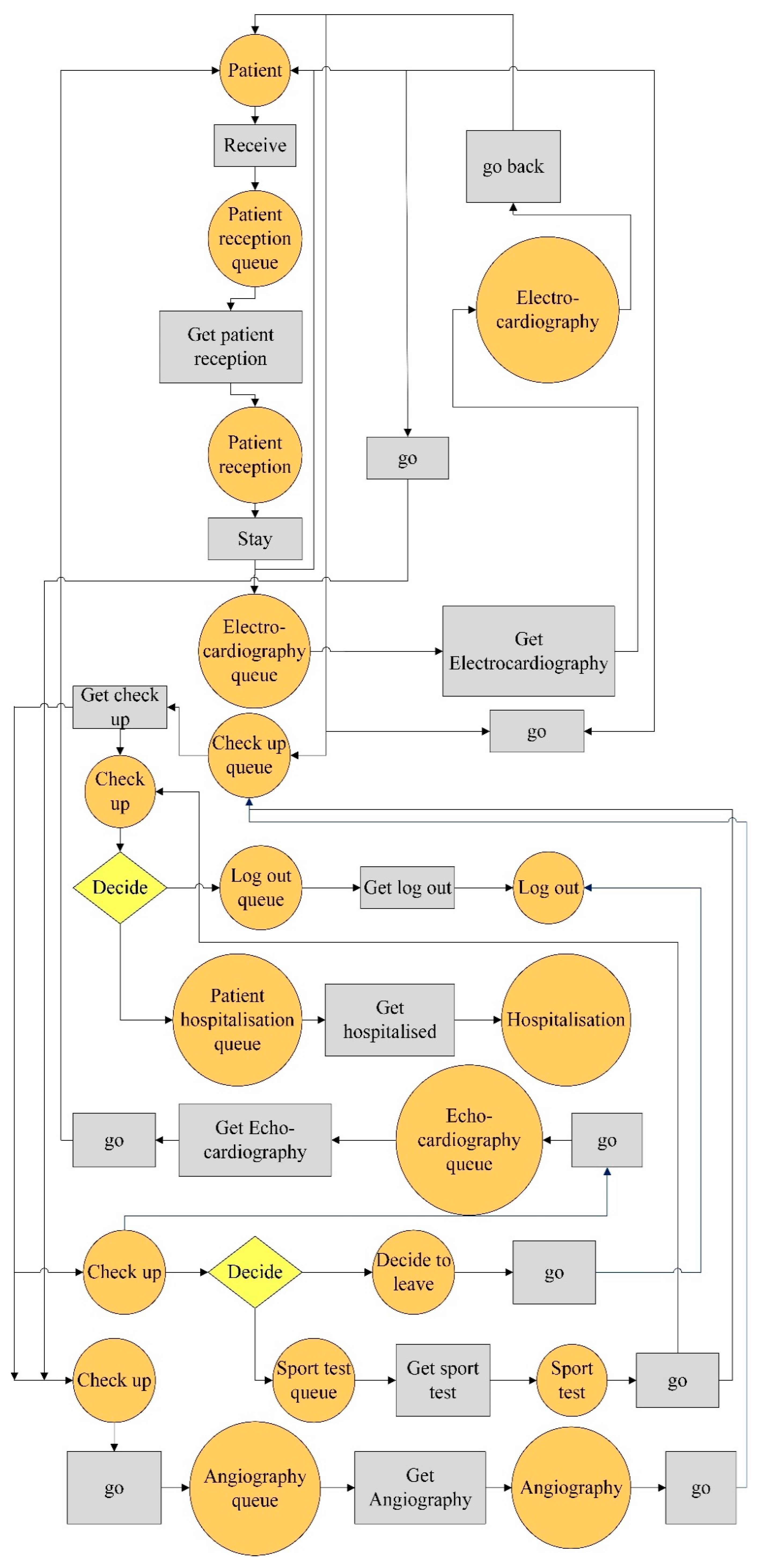
3.1. Timed Coloured Petri Net
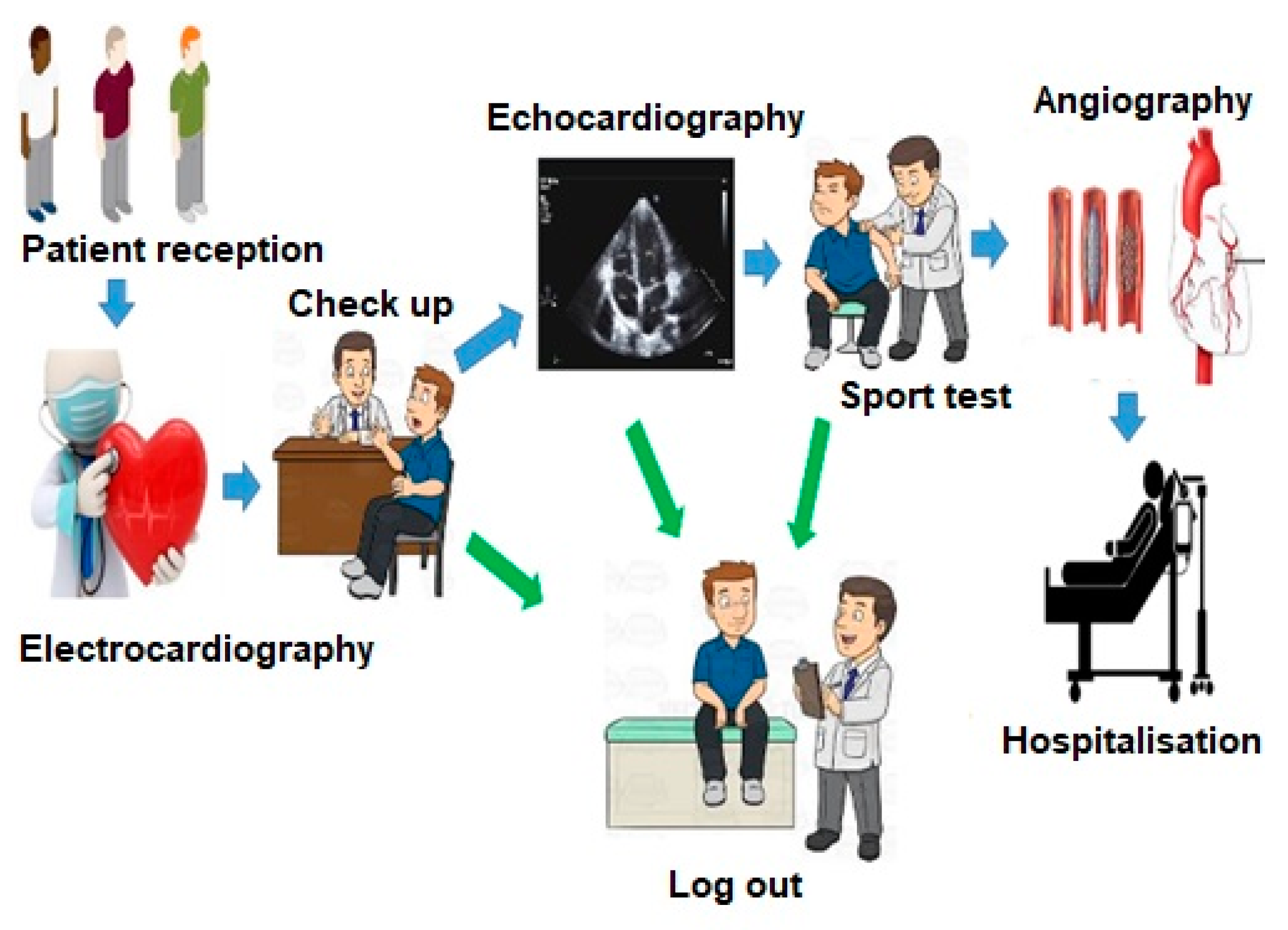
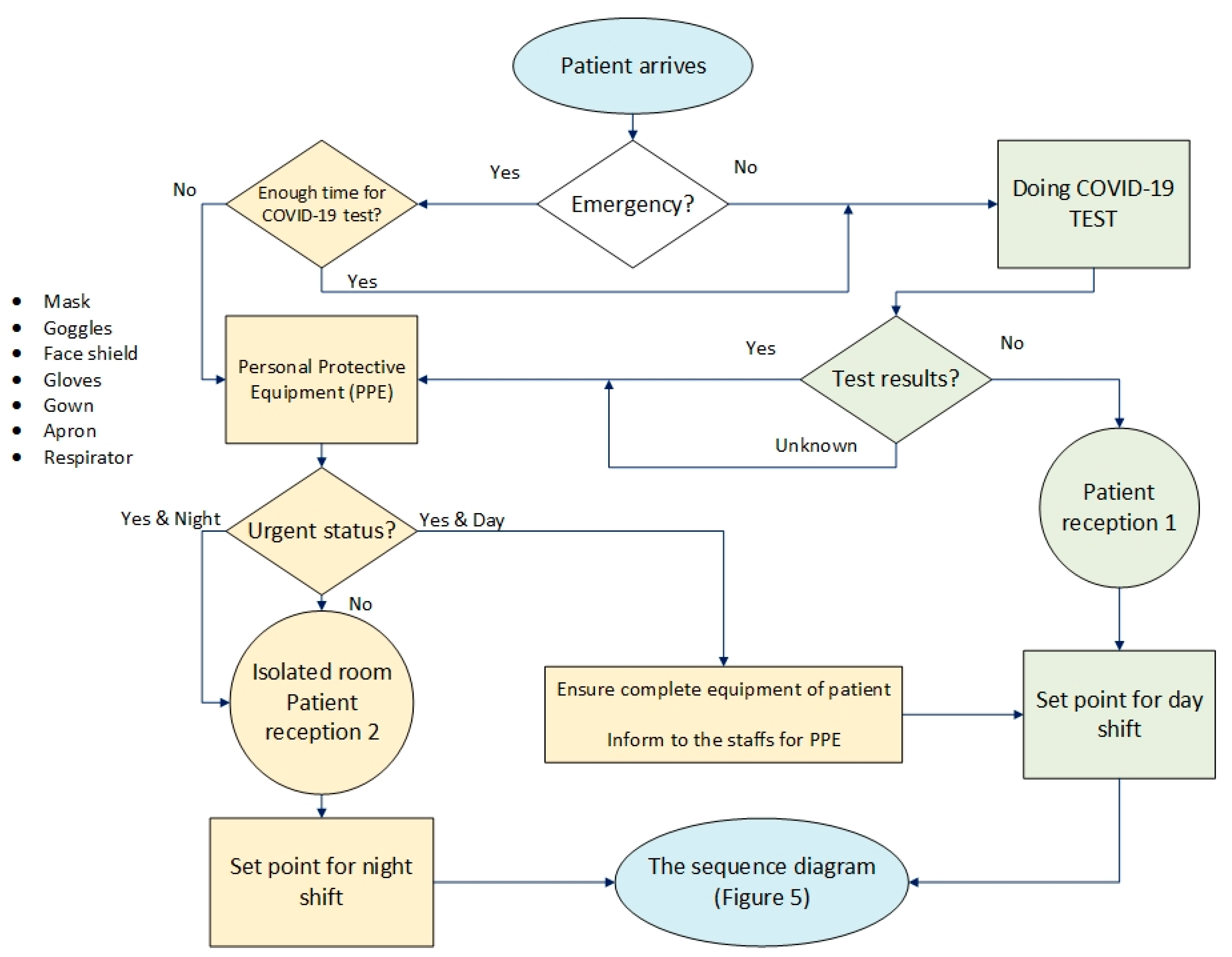
3.2. Workflow Modelling
3.3. Sequence Diagram Evaluation
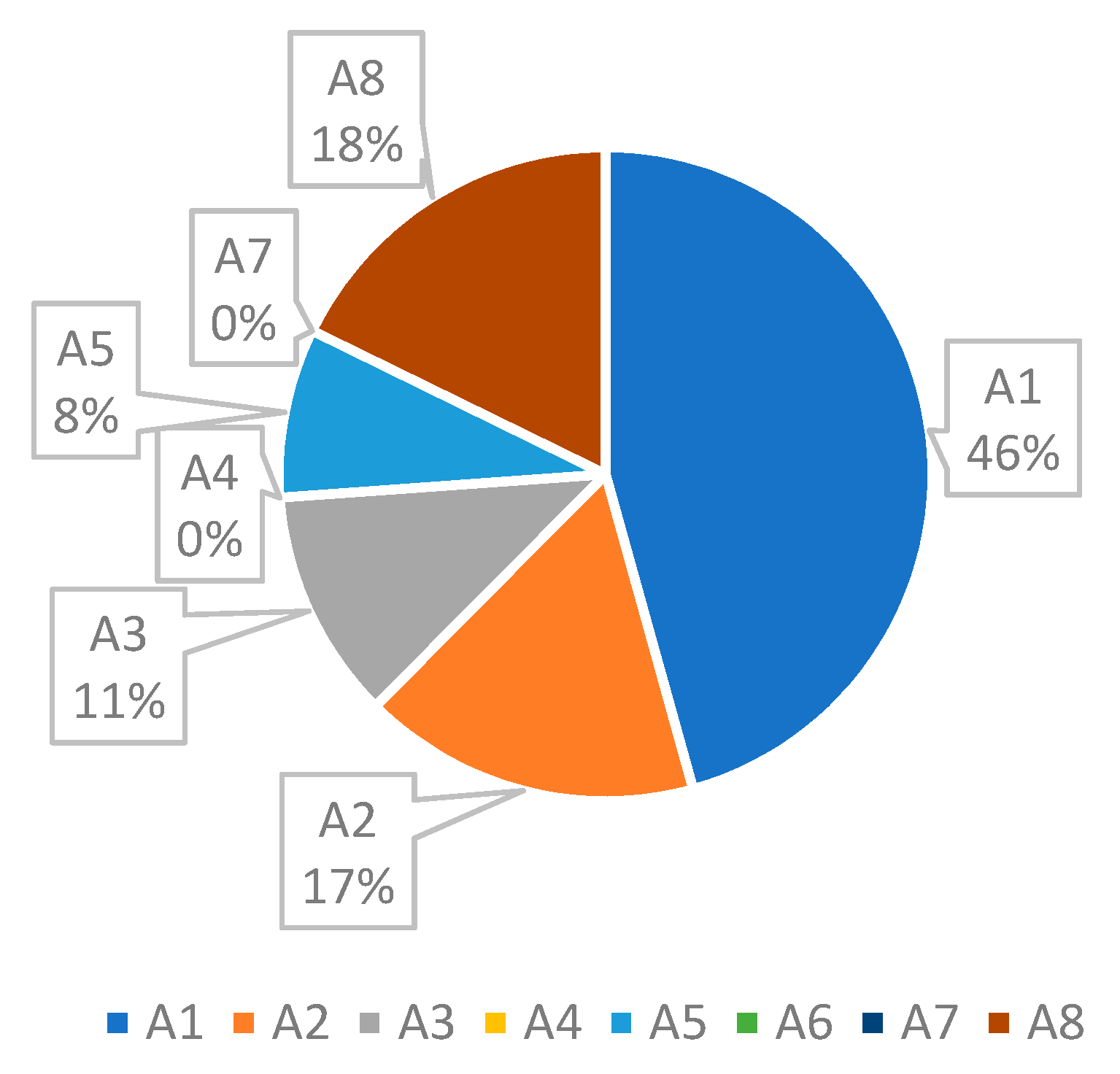
3.4. Data Collection
4. Results
4.1. Initial Simulation
4.2. Scenario Planning and Simulation
- changing the patient’s workflow,
- increasing the number of staff
- temporary usage of free human resources of other wards (sharing), and
- buying new equipment.
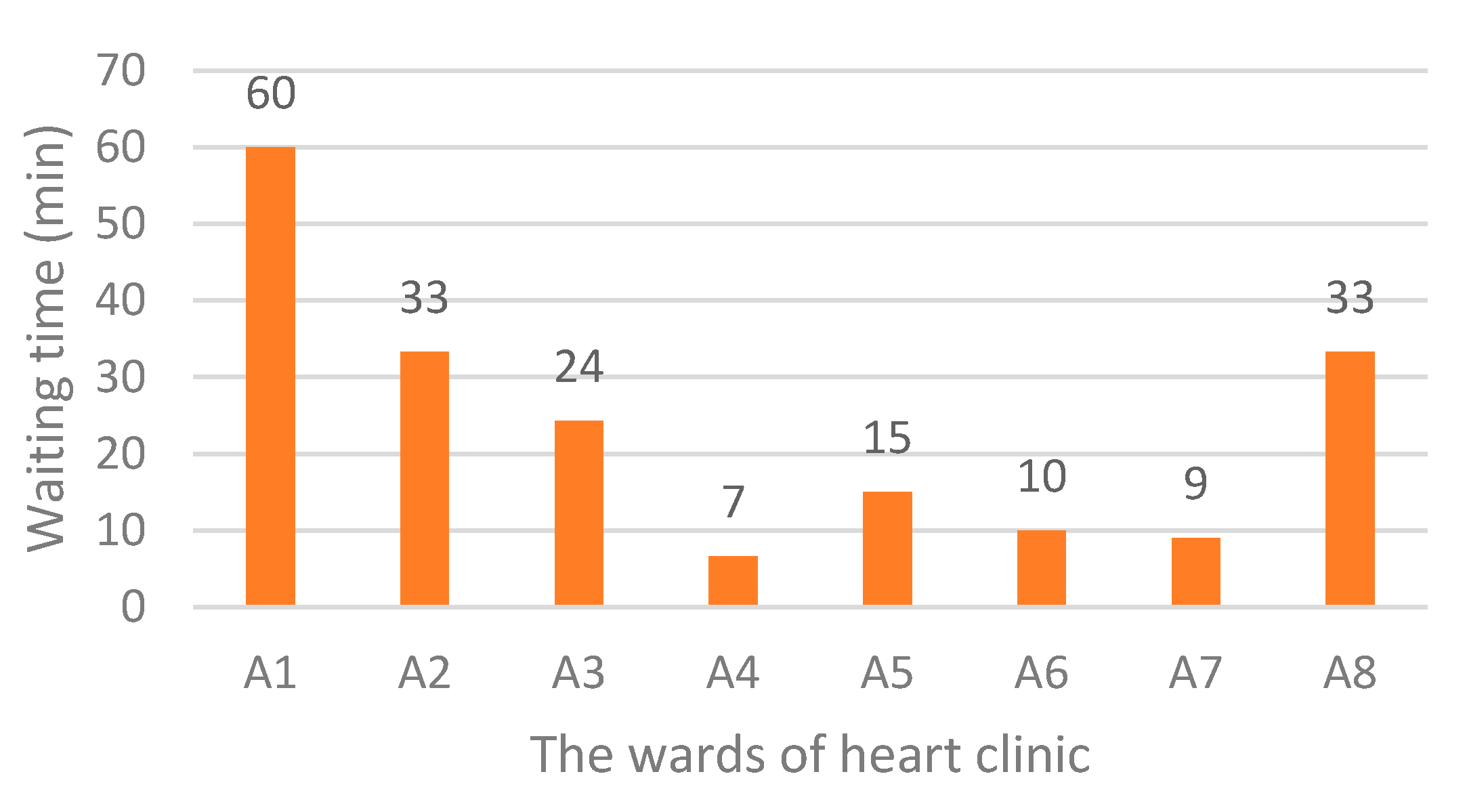
4.2.1. The Results of Scenario 1
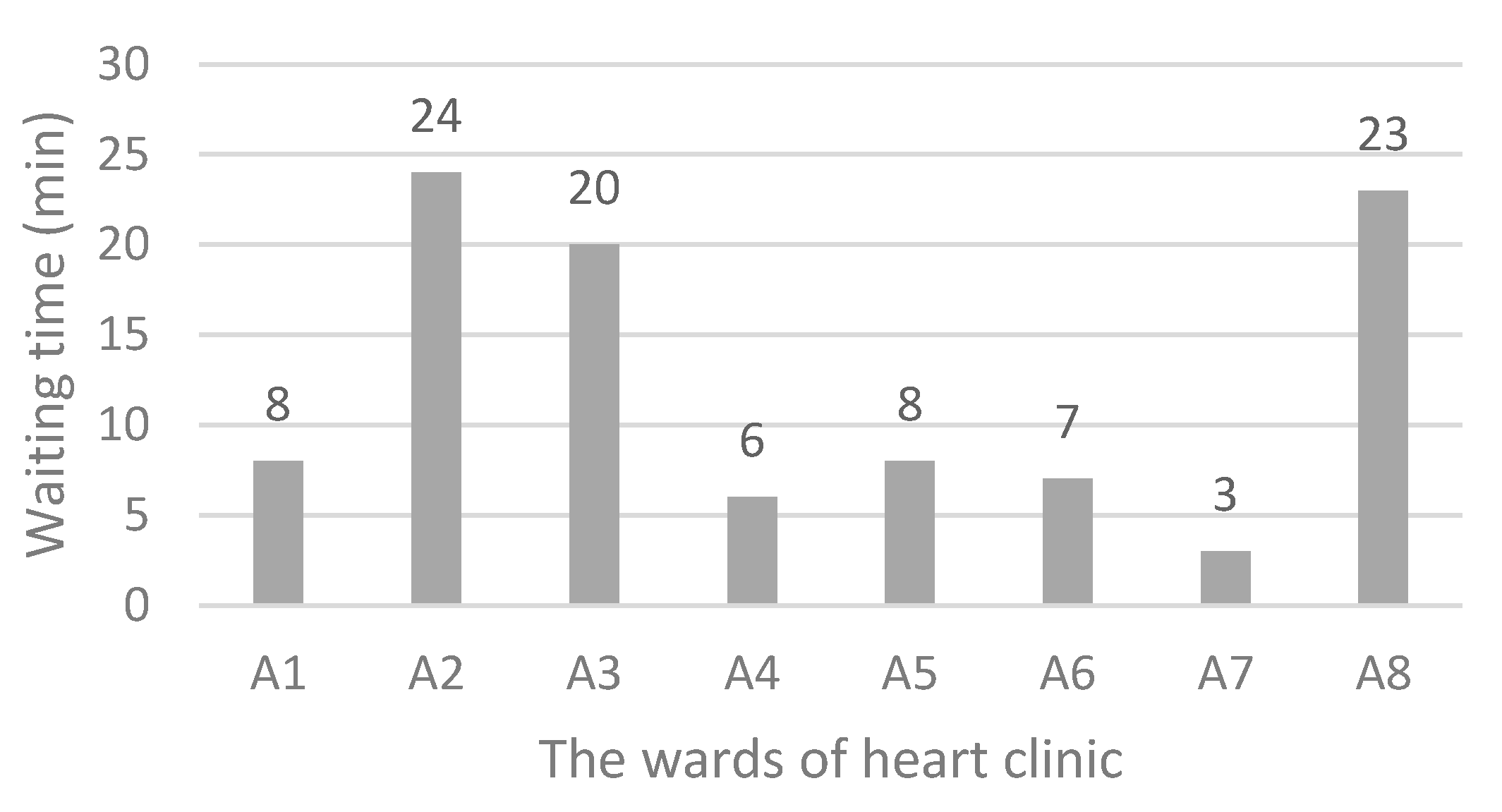
4.2.2. The Results of Scenario 2
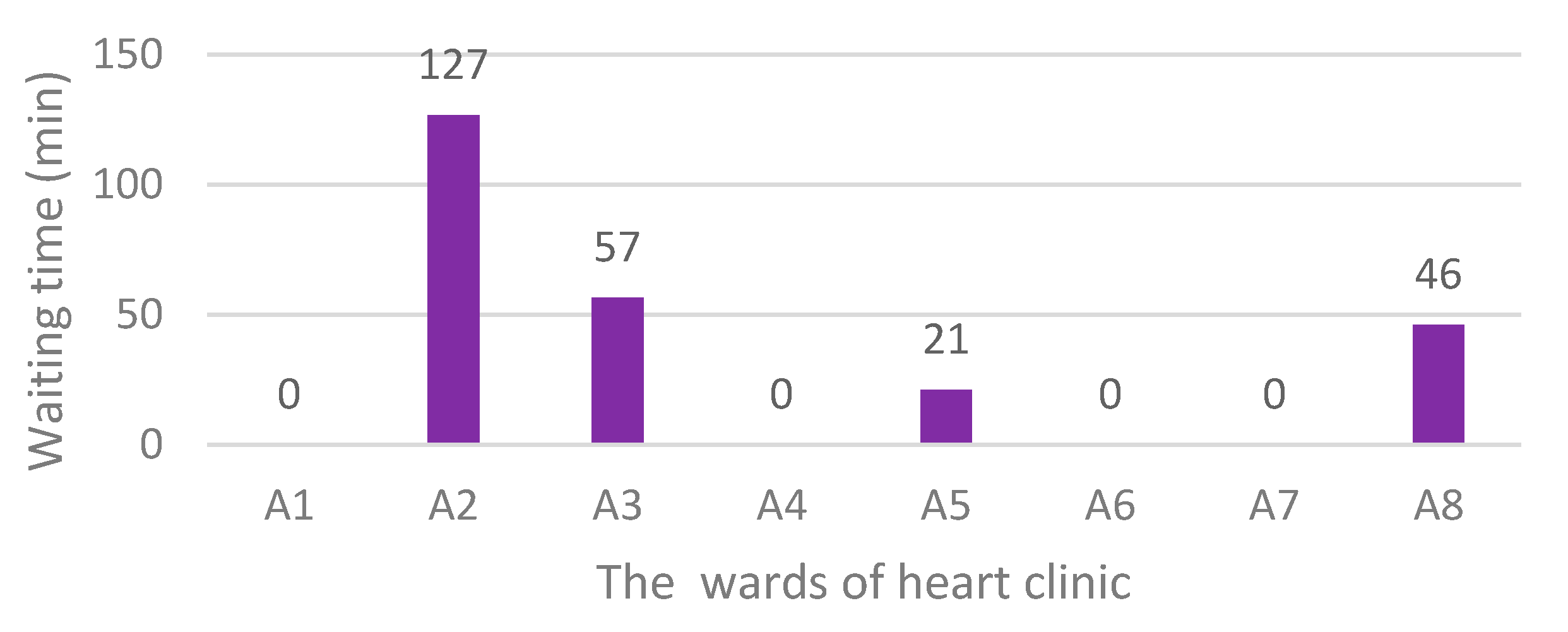
4.2.3. The Results of Scenario 3
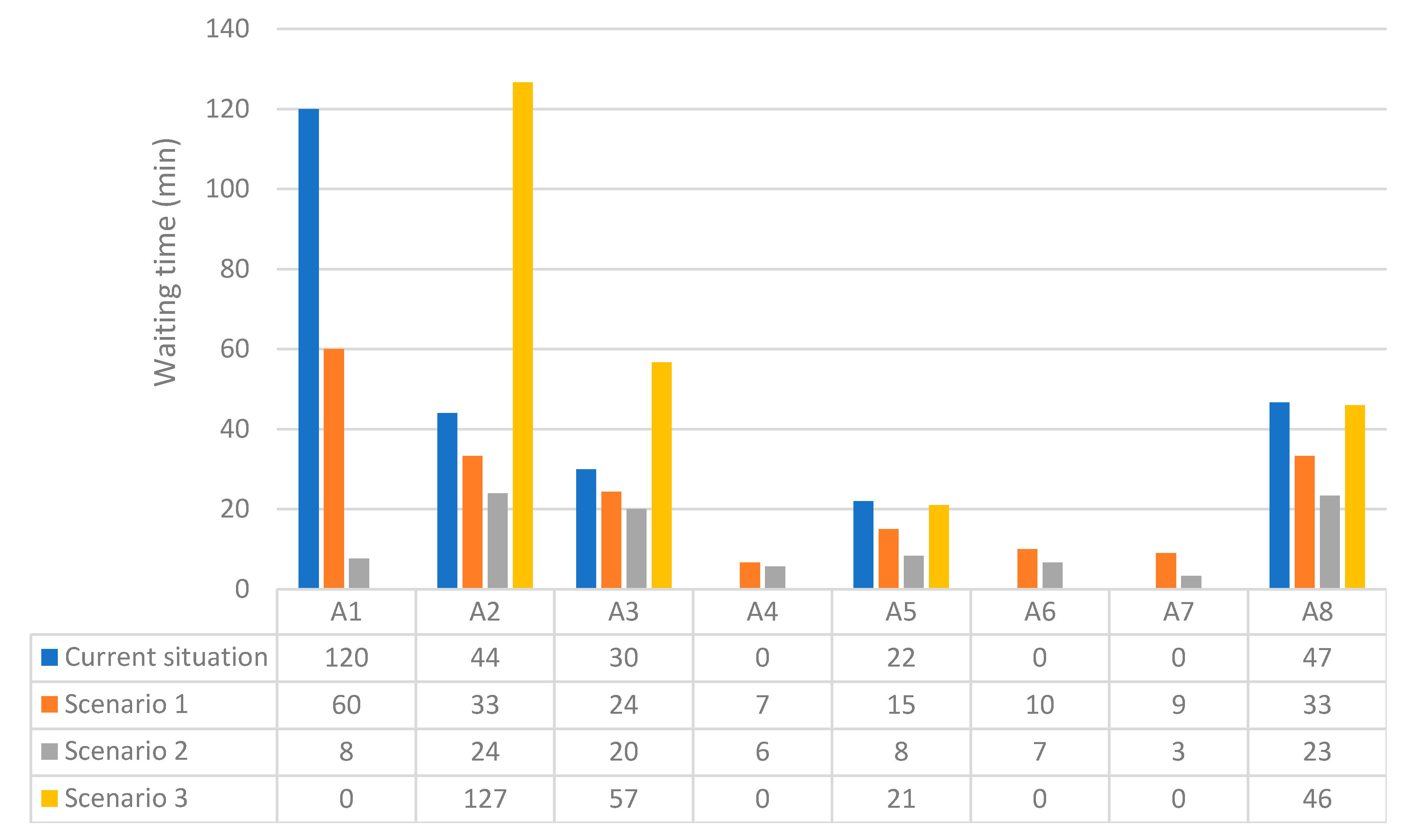
4.3. Comparing the Simulation Results
4.4. Framework Development
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Klemeš, J.J.; Fan, X.Y.; Tan, R.R.; Jiang, P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sustain. Energy Rev. 2020, 127, 109883. [Google Scholar] [CrossRef]
- Bettinelli, G.; Delmastro, E.; Salvato, D.; Salini, V.; Placella, G. Orthopaedic patient workflow in CoViD-19 pandemic in Italy. J. Orthop. 2020, 22, 158–159. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.A.; Clarke, B.; Ducharme, A.; Ezekowitz, J.A.; Heckman, G.A.; McDonald, M.; Mielniczuk, L.M.; Swiggum, E.; Van Spall, H.G.C.; Zieroth, S. Optimizing Access to Heart Failure Care in Canada During the COVID-19 Pandemic. Can. J. Cardiol. 2020, 36, 1148–1151. [Google Scholar] [CrossRef] [PubMed]
- Chofreh, A.G.; Goni, F.A.; Shaharoun, A.M.; Ismail, S. Review on Enterprise Resource Planning Implementation Roadmap: Project Management Perspective. J. Teknol. 2014, 2, 135–138. [Google Scholar]
- Klemeš, J.J.; Van Fan, Y.; Jiang, P. The Energy and Environmental Footprints of COVID-19 Fighting Measures–PPE, Disinfection, Supply Chains. Energy 2020, 211, 118701. [Google Scholar]
- Shan, Z.h.; Lin, C.H.; Ren, F.; Wei, Y. Modeling and Performance Analysis of a Multi-Server Multi-Queue System on the Grid. In Proceedings of the Ninth IEEE Workshop on Future Trends of Distributed Computing Systems 12, San Juan, PR, USA, 30 May 2003. [Google Scholar]
- Brenner, S.Z.Z.; Liu, Y.; Li, J.; Howard, P.K. Modelling and analysis of the emergency department at University of Kentucky Chandler Hospital using simulations. J. Emerg. Nurs. 2010, 36, 303–310. [Google Scholar] [CrossRef]
- Kabir, S.; Papadopoulos, Y. Applications of Bayesian networks and Petri nets in safety, reliability, and risk assessments: A review. Saf. Sci. 2019, 115, 154–175. [Google Scholar] [CrossRef]
- Aeenparast, A.; Tabibi, S.J.; Shahanagi, K.; Aryanejhad, M. Estimating outpatient waiting time: A simulation approach. Payesh 2009, 8, 315–320. [Google Scholar]
- Creemers, S.; Beliën, J.; Lambrecht, M. The optimal allocation of server time slots over different classes of patients. Eur. J. Oper. Res. 2012, 219, 508–521. [Google Scholar] [CrossRef]
- Bevilacqua, M.; Ciarapica, F.E.; Giovanni, M. Timed colored Petri nets for modeling and managing processes and projects. In Proceedings of the 11th CIRP Conference on Intelligent Computation in Manufacturing Engineering, Gulf of Naples, Italy, 19–21 July 2017. [Google Scholar]
- Chofreh, A.G.; Goni, F.A.; Zeinalnezhad, M.; Vavidar, S.; Shayestehzadeh, H.; Klemeš, J.J. Value chain mapping of the water and sewage treatment to contribute to sustainability. J. Environ. Manag. 2019, 239, 38–47. [Google Scholar] [CrossRef]
- Chofreh, A.; Goni, F.; Klemeš, J.J. A Master Plan for the Implementation of Sustainable Enterprise Resource Planning Systems (Part III): Evaluation of a Roadmap. Chem. Eng. Trans. 2016, 52, 1105–1110. [Google Scholar]
- Chofreh, A.; Goni, F.; Malik, M.N.; Khan, H.H.; Klemeš, J.J. The imperative and research directions of sustainable project management. J. Clean. Prod. 2019, 238, 117810. [Google Scholar] [CrossRef]
- Klemeš, J.J.; Van Fan, Y.; Jiang, P. COVID-19 pandemic facilitating energy transition opportunities. Int. J. Energy Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Harjai, K.J.; Agarwal, S.; Bauch, T.; Bernardi, M.; Casale, A.S.; Green, S.; Harostock, M.; Ierovante, N.; Mascarenhas, V.; Matsumura, M.; et al. Coronary and structural heart disease interventions during COVID-19 pandemic: A road map for clinicians and health care delivery systems. Cardiovasc. Revasc. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Asdaghpour, E.; Baghaei, R.; Jalilifar, N.; Radmehr, H.; Shirzad, M.; Mirzaaghayan, M.R.; Yousefnia, M.A.; Austin, N.; Alizadeh Ghavidel, A.; Hossein Ahmadi, Z.; et al. Iranian society of cardiac surgeons position statement for the treatment of patients in need of cardiac surgery in the COVID-19 pandemic period (Version I). Multidiscip. Cardiovasc. Ann. 2020, 11, e104296. [Google Scholar] [CrossRef]
- Fersia, O.; Bryant, S.; Nicholson, R.; McMeeken, K.; Brown, C.; Donaldson, B.; Jardine, A.; Grierson, V.; Whalen, V.; Mackay, A. The impact of the COVID-19 pandemic on cardiology services. Open Heart 2020, 7, e001359. [Google Scholar] [CrossRef]
- Wei, W.; Zheng, D.; Lei, Y.; Wu, S.; Verma, V.; Liu, Y.; Wei, X.; Bi, J.; Hu, D.; Han, G. Radiotherapy workflow and protection procedures during the Coronavirus Disease 2019 (COVID-19) outbreak: Experience of the Hubei Cancer Hospital in Wuhan, China. Radiother. Oncol. 2020, 148, 203–210. [Google Scholar] [CrossRef]
- Diaz, M.C.G.; Dawson, K. Use of simulation to develop a COVID-19 resuscitation process in a pediatric emergency department. Am. J. Infect. Control 2020, 48, 1244–1247. [Google Scholar] [CrossRef] [PubMed]
- Das, A. Impact of the COVID-19 pandemic on the workflow of an ambulatory endoscopy center: An assessment by discrete event simulation. Gastrointest. Endosc. 2020, 92, 914–924. [Google Scholar] [CrossRef] [PubMed]
- Quraishi, M.I.; Rizvi, A.A.; Heidel, R.E. Off-site radiology workflow changes due to the coronavirus disease 2019 (COVID-19) pandemic. J. Am. College Radiol. 2020, 17, 878–881. [Google Scholar] [CrossRef] [PubMed]
- Dexter, F.; Elhakim, M.; Loftus, R.W.; Seering, M.S.; Epstein, R.H. Strategies for daily operating room management of ambulatory surgery centers following resolution of the acute phase of the COVID-19 pandemic. J. Clin. Anesth. 2020, 64, 109854. [Google Scholar] [CrossRef] [PubMed]
- Phua, J.; Weng, L.; Ling, L.; Egi, M.; Lim, C.M.; Divatia, J.V.; Shrestha, B.R.; Arabi, M.; Mel, J.N.M.; Gomersall, C.D.; et al. Intensive care management of coronavirus disease 2019 (COVID-19): Challenges and recommendations. Lancet Respir. Med. 2020, 8, 506–517. [Google Scholar] [CrossRef]
- Tey, J.; Ho, S.; Choo, B.A.; Ho, F.; Yap, S.P.; Tuan, J.K.L.; Leong, C.N.; Cheo, T.; Sommat, K.; Wang, M.L.C. Navigating the challenges of the COVID-19 outbreak: Perspectives from the radiation oncology service in Singapore. Radiother. Oncol. 2020, 148, 189–193. [Google Scholar] [CrossRef]
- Yan, C.; Lin, J.; Xu, Y. Recommendations for coronavirus disease 2019 (COVID-19) prevention and infection control in the radiology department: Chinese experience. Clin. Imaging 2020, 69, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Esmaili, H.; Matin, A. Principles and Basics of Petri Networks with an Industrial Engineering and Management Approach; Dibagaran Publication: Tehran, Iran, 2018. [Google Scholar]
- Najmuddin, A.; Ibrahim, I.; Ismail, S. A simulation approach: Improving patient waiting time for multiphase patient flow of obstetrics and gynecology department (O and G Department) in local specialist centre. WSEAS Trans. Math. 2010, 10, 778–790. [Google Scholar]
- Julia, S.; Oliveira, F.F.D.; Valette, R. Real time scheduling of workflow management systems based on a p-time Petri net model with hybrid resources. Simul. Model. Pract. Theory 2008, 16, 462–482. [Google Scholar] [CrossRef]
- Chofreh, A.G.; Goni, F.A.; Klemeš, J.J. Development of a Framework for the Implementation of Sustainable Enterprise Resource Planning. Chem. Eng. Trans. 2017, 61, 1543–1548. [Google Scholar] [CrossRef]
- Giua, A.; Silva, M. Modeling, analysis and control of discrete event systems: A Petri net perspective. Int. Fed. Autom. Control 2017, 12, 1772–1783. [Google Scholar] [CrossRef]
- Chofreh, A.; Goni, F.; Klemeš, J.J. A Master Plan for the Implementation of Sustainable Enterprise Resource Planning Systems (Part II): Development of a roadmap. Chem. Eng. Trans. 2016, 52, 1099–1104. [Google Scholar]
- Kontogiannis, T. A Petri Net-based approach for ergonomic task analysis and modeling with emphasis on adaptation to system changes. Saf. Sci. 2003, 41, 803–835. [Google Scholar] [CrossRef]
- Zeinalnezhad, M.; Sepehri, F.; Molana, M.H.; Pourrostam, T.; Chofreh, A.G.; Klemeš, J.J.; Goni, F.A. Identification of performance evaluation indicators for health, safety, environment, and ergonomics management systems. Chem. Eng. Trans. 2018, 67, 451–456. [Google Scholar]
- Zeinalnezhad, M.; Mukhtar, M.; Sahran, S. An investigation of lead benchmarking implementation: A comparison of small/medium enterprises and large companies. Benchmarking Int. J. 2014, 21, 121–145. [Google Scholar] [CrossRef]
- Zeinalnezhad, M.; Chofreh, A.G.; Goni, F.A.; Klemeš, J.J. Critical success factors of the reliability-centred maintenance implementation in the oil and gas industry. Symmetry 2020, 12, 1585. [Google Scholar] [CrossRef]
- Zeinalnezhad, M.; Chofreh, A.G.; Goni, F.A.; Klemeš, J.J. Air pollution prediction using semi-experimental regression model and Adaptive Neuro-Fuzzy Inference System. J. Clean. Prod. 2020, 261, 121218. [Google Scholar] [CrossRef]



| Author | Objective | Specialised Clinic | Research Method | Research Highlights |
|---|---|---|---|---|
| Virani et al. [3] | Optimising access to heart failure care during the COVID-19 outbreak | Heart | Review of the activities performed, and the experiences gained | The study provided viewpoints from leadership within the Canadian Heart Failure Society. |
| Quraishi et al. [22] | Study of the changes related to the off-site radiology workflow due to the COVID-19 pandemic | Radiology | A survey of 174 radiologists used frequency and descriptive statistics to perform χ2 analyses and nonparametric Mann–Whitney U tests. | The bulk of radiology practices have leveraged internal teleradiology for regular workday shifts and found an adequate benefit to consider continuing internal teleradiology after the epidemic passes. |
| Dexter et al. [23] | Proposing strategies for daily operating room management following resolution of the critical phase of the coronavirus pandemic | Ambulatory surgery | A narrative review | The economic costs of the COVID-19 pandemic for ambulatory surgery centres were identified. |
| Harjai et al. [16] | Providing a road map for clinicians and healthcare delivery systems | Heart | Surveyed 16 physicians across three hospitals. | Most follow-up visits can be done via telemedicine rather than in-person visits. |
| Phua et al. [24] | Providing recommendations for serious care management of COVID-19 outbreak | Intensive care unit (ICU) | Review of the activities performed, and the experiences gained | National and international cooperation offers the best opportunity for survival for the critically ill. |
| Diaz and Dawson [20] | Development of a COVID-19 resuscitation procedure in the emergency department of paediatrics | Paediatric emergency | Discrete-event simulation | Simulation can be applied to enhance infection prevention and control initiatives, to assist developing of COVID-19 procedures, workflows, and spaces, as well as to support education teams about COVID-19 nuances. |
| Das [19] | Studying the influence of the COVID-19 outbreak on the current workflow | Endoscopy centre | Discrete-event simulation and Monte-Carlo analysis | Post-COVID-19 proposed workflow changes meaningfully impact productivity and operational metrics and, in turn, adversely impact financial indicators. |
| Tey et al. [25] | Studying the challenges of the COVID-19 pandemic | Radiation oncology | Using a modified workflow from a few cancer centres | Applied steps in the treatment of oncology patients during an infectious eruption were introduced. |
| Wei et al. [19] | Navigation of radiotherapy workflow and safety procedures during the COVID-19 outbreak | Radiotherapy in the cancer hospital | Review of the activities performed, and the experiences gained | Particular measures were taken to battle COVID-19 though maintaining radiotherapy care. |
| Yan et al. [26] | Providing recommendations for coronavirus disease 2019 prevention and infection control | Radiology | Review of the activities performed, and the experiences gained | Typical transmission-based provision, computed tomography workflow for the check-up of fever patients, as well as cleansing management of a radiology section were described. |
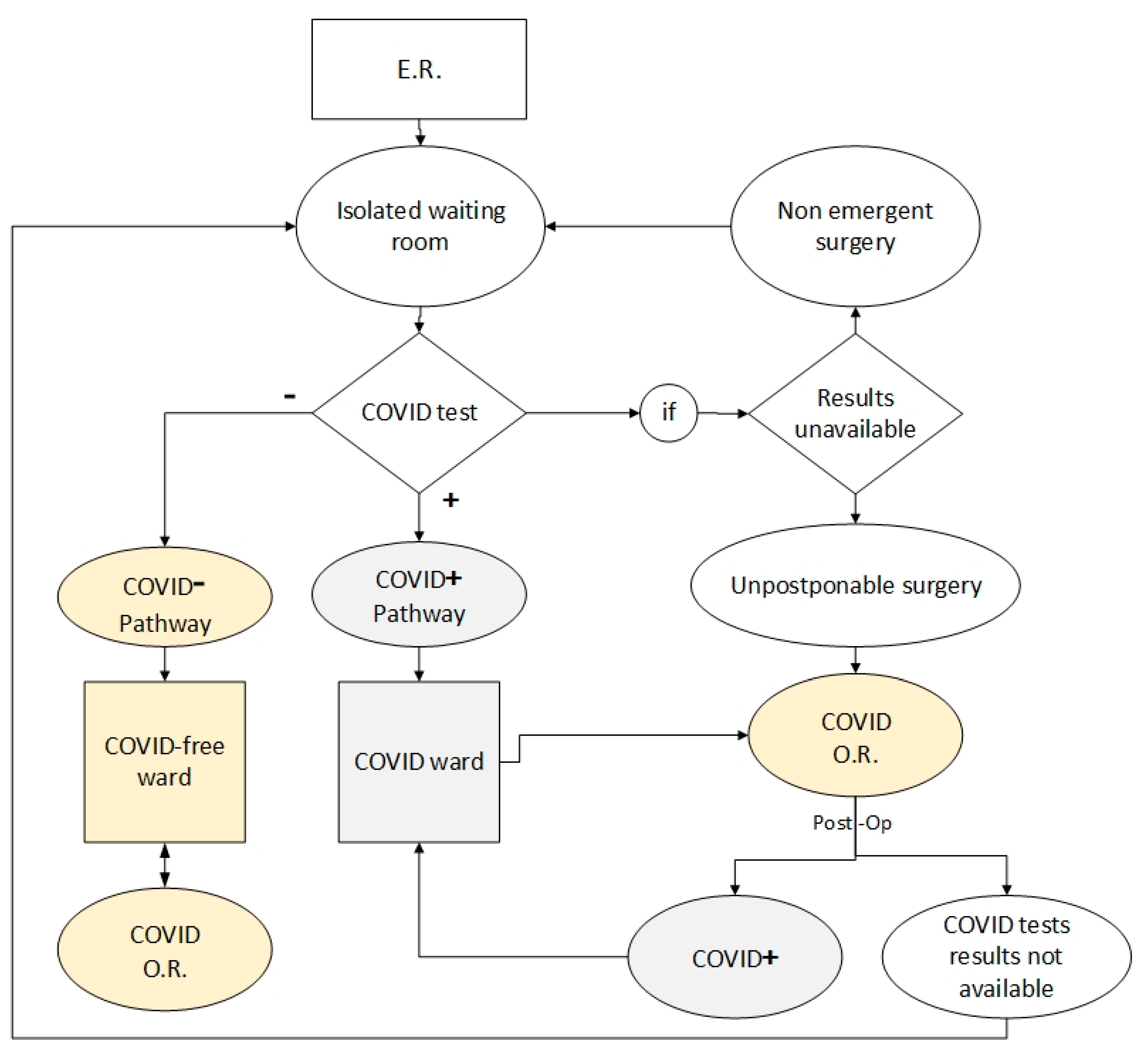
| Bettinelli et al. [2] | Providing an operative flowchart for COVID-19 patient treatment | Orthopaedic | Review of the activities performed, and the experiences gained | A workflow for patients attained in the ER in an Orthopaedic Hub is designed. |
| Ward Code | Ward Name | Number of Doctors/Technicians | Number of Equipment | PDF of Service Duration (Min) | Average Service Duration (Min) |
|---|---|---|---|---|---|
| A1 | Patient reception | 1 | - | U (5, 15) | 10 |
| A2 | Electrocardiography | 1 | 1 | U (2, 15) | 12 |
| A3 | Check-up | 2 | - | U (5, 20) | 15 |
| A4 | Echocardiography | 1 | 1 | U (5, 15) | 10 |
| A5 | Sport test | 1 | 1 | U (5, 60) | 33 |
| A6 | Angiography | 1 | 1 | U (120, 180) | 150 |
| A7 | Hospitalization | 1 | - | U (10, 30) | 20 |
| A8 | Log out | 1 | - | U (10, 30) | 20 |
| No. | Scenario Name | Number of Employees Added to A1 | Temporary Usage of Idle Staff of Other Wards |
|---|---|---|---|
| 1 | Scenario 1 | 2 | Yes |
| 2 | Scenario 2 | 3 | Yes |
| 3 | Scenario 3 | 4 | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeinalnezhad, M.; Chofreh, A.G.; Goni, F.A.; Klemeš, J.J.; Sari, E. Simulation and Improvement of Patients’ Workflow in Heart Clinics during COVID-19 Pandemic Using Timed Coloured Petri Nets. Int. J. Environ. Res. Public Health 2020, 17, 8577. https://doi.org/10.3390/ijerph17228577
Zeinalnezhad M, Chofreh AG, Goni FA, Klemeš JJ, Sari E. Simulation and Improvement of Patients’ Workflow in Heart Clinics during COVID-19 Pandemic Using Timed Coloured Petri Nets. International Journal of Environmental Research and Public Health. 2020; 17(22):8577. https://doi.org/10.3390/ijerph17228577
Chicago/Turabian StyleZeinalnezhad, Masoomeh, Abdoulmohammad Gholamzadeh Chofreh, Feybi Ariani Goni, Jiří Jaromír Klemeš, and Emelia Sari. 2020. "Simulation and Improvement of Patients’ Workflow in Heart Clinics during COVID-19 Pandemic Using Timed Coloured Petri Nets" International Journal of Environmental Research and Public Health 17, no. 22: 8577. https://doi.org/10.3390/ijerph17228577
APA StyleZeinalnezhad, M., Chofreh, A. G., Goni, F. A., Klemeš, J. J., & Sari, E. (2020). Simulation and Improvement of Patients’ Workflow in Heart Clinics during COVID-19 Pandemic Using Timed Coloured Petri Nets. International Journal of Environmental Research and Public Health, 17(22), 8577. https://doi.org/10.3390/ijerph17228577







