Impact of Nurses’ Intervention in the Prevention of Falls in Hospitalized Patients
Abstract
:1. Background
1.1. Framework
1.2. Justification
1.3. Objectives
2. Methods
2.1. Study Design
2.2. Population
2.3. Study Assessment Parameters
- Sex (men, women);
- Age categorized (in years) and age groups (15–50, 51–64, 65–79, ≥80);
- Nursing units (General Internal Medicine, Neurology and Neurosurgery, Traumatology and Urology, Vascular Surgery and Nephrology);
- Group (control and intervention);
- Type of nurse assessment on admission (traditional method, systematized method);
- Assessment of the risk of falls on admission according to the Downton scale (yes/no) [28] (this scale assesses factors related to the risk of falling, such as sensory deficits, mental state impairment, wandering, and intake of medication whose side effects may influence the occurrence of falls);
- Length of hospital stay in days and in two categories (0–7 and ≥8 days);
- Degree of mobility (non or impaired, unaided in and outside of the room and bathroom);
- Surgical intervention (yes/no);
- Altered consciousness (yes/no);
- Nutritional status on admission according to the Mini Nutritional Assessment-Short Form (MNA-SF) (risk and/or malnutrition and good nutritional status) [29];
- Supply of oxygen (yes/no);
- Has catheters (vascular access; nasogastric tubes; urinary catheterization) and categorized (does not have catheters, has a catheter, and has two or more catheters).
2.4. Procedure
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
3.1. Description of the Sample
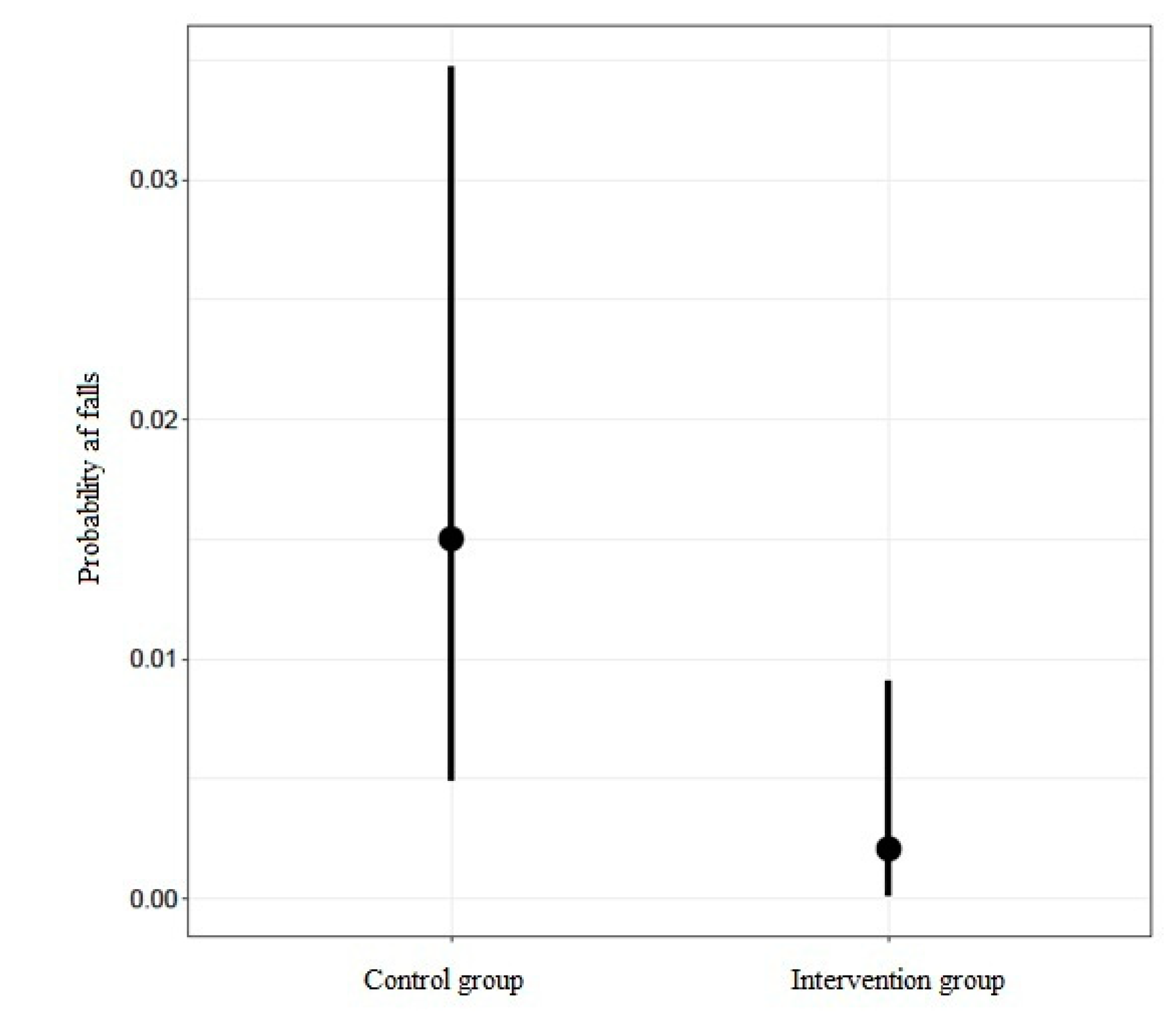
3.2. Incidence of Falls
3.3. Regression Model
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization (WHO). Acción Mundial en pro de la Seguridad del Paciente. 72. a Asamblea Mundial de la Salud; WHO: Ginebra, Switzerland, 2019; Available online: https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R6-sp.pdf?ua=1 (accessed on 18 July 2020).
- Aranaz-Andrés, J.M.; Aibar-Remón, C.; Vitaller-Murillo, J.; López, P.R.; Limón-Ramírez, R.; Terol-García, E. Incidence of adverse events related to health care in Spain: Results of the Spanish National Study of Adverse Events. J. Epidemiol. Community Health 2008, 62, 1022–1029. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Imagama, S.; Ando, K.; Inagaki, Y.; Suzuki, Y.; Nishida, Y.; Nagao, Y.; Ishiguro, N. Analysis of falls that caused serious events in hospitalized patients. Geriatr. Gerontol. Int. 2017, 17, 2403–2406. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Servicios Sociales e Igualdad (MSSSI). Estrategia Seguridad del Paciente del Sistema Nacional de Salud. Período 2015–2020; Gobierno de España: MSSSI: Madrid, España, 2016. Available online: https://www.seguridaddelpaciente.es/resources/documentos/2015/Estrategia%20Seguridad%20del%20Paciente%202015-2020.pdf?cdnv=2 (accessed on 18 April 2020).
- Cangany, M.; Back, D.; Hamilton-Kelly, T.; Altman, M.S.; Lacey, S. Bedside Nurses Leading the Way for Falls Prevention: An Evidence-Based Approach. Crit. Care Nurse 2015, 35, 82–84. [Google Scholar] [CrossRef]
- Jacobi, L.; Petzold, T.; Hänel, A.; Albrecht, M.; Eberlein-Gonska, M.; Schmitt, J. Epidemiologie und Vorhersage des Sturzrisikos von Patienten in der akutstationären Versorgung: Analyse von Routinedaten eines Universitätsklinikums. Z. Evidenz Fortbild. Qual. Gesundh. 2017, 120, 9–15. [Google Scholar] [CrossRef]
- Luzia, M.D.F.; Victor, M.A.D.G.; Lucena, A.D.F. Nursing Diagnosis Risk for falls: Prevalence and clinical profile of hospitalized patients. Rev. Lat.-Am. Enferm. 2014, 22, 262–268. [Google Scholar] [CrossRef]
- Goldsack, J.; Bergey, M.; Mascioli, S.; Cunningham, J. Hourly rounding and patient falls. Nursing 2015, 45, 25–30. [Google Scholar] [CrossRef]
- Melin, C.M. Reducing falls in the inpatient hospital setting. Int. J. Evid. Based Health 2018, 16, 25–31. [Google Scholar] [CrossRef]
- LeLaurin, J.H.; Shorr, R.I. Preventing Falls in Hospitalized Patients. Clin. Geriatr. Med. 2019, 35, 273–283. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Falls; WHO: Geneva, Switzerland, 2018; Available online: https://www.who.int/violence_injury_prevention/other_injury/falls/en (accessed on 18 April 2020).
- Najafpour, Z.; Godarzi, Z.; Arab, M.; Yaseri, M. Risk Factors for Falls in Hospital In-Patients: A Prospective Nested Case Control Study. Int. J. Health Policy Manag. 2019, 8, 300–306. [Google Scholar] [CrossRef]
- Bittencourt, V.L.L.; Graube, S.L.; Stumm, E.M.F.; Battisti, I.D.E.; Loro, M.M.; Winkelmann, E.R. Factors associated with the risk of falls in hospitalized adult patients. Rev. Esc. Enferm. USP 2017, 51, 03237. [Google Scholar] [CrossRef] [Green Version]
- Saiz-Vinuesa, M.; Muñoz-Mansilla, E.; Muñoz-Serrano, T.; Corcoles-Jimenez, M.-P.; Ruiz-García, M.; Fernández-Pallarés, P.; Herreros-Sáez, L.; Calero-Yáñez, F. Implantación de una guía de buenas prácticas para la prevención de caídas: Percepción de los pacientes hospitalizados y sus cuidadores. Rev. Calid. Asist. 2016, 31, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Severo, I.M.; Almeida, M.D.A.; Kuchenbecker, R.; Vieira, D.F.V.B.; Hervé, M.E.W.; Pinto, L.R.C.; Klein, C.; Siqueira, A.P.D.O.; Panato, B.P. Risk factors for falls in hospitalized adult patients: An integrative review. Rev. Esc. Enferm. USP 2014, 48, 540–554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernández-Herrera, D.; Aguilera-Elizarraraz, N.; Vega-Argote, M.; González-Quirarte, N.; Castañeda-Hidalgo, H.; Isasi-Hernández, L. Aplicación de las actividades de la intervención de enfermería Prevención de caídas en adultos hospitalizados. Enfermería Univ. 2017, 14, 118–123. [Google Scholar] [CrossRef]
- Lerdal, A.; Sigurdsen, L.W.; Hammerstad, H.; Granheim, T.I.; Gay, C.; Risk Study Research Group. Associations between patient symptoms and falls in an acute care hospital: A cross-sectional study. J. Clin. Nurs. 2018, 27, 1826–1835. [Google Scholar] [CrossRef] [PubMed]
- Titler, M.G.; Conlon, P.; Reynolds, M.A.; Ripley, R.; Tsodikov, A.; Wilson, D.S.; Montie, M.; Information, P.E.K.F.C. The effect of a translating research into practice intervention to promote use of evidence-based fall prevention interventions in hospitalized adults: A prospective pre–post implementation study in the U.S. Appl. Nurs. Res. 2016, 31, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Miake-Lye, I.M.; Hempel, S.; Ganz, D.A.; Shekelle, P.G. Inpatient Fall Prevention Programs as a Patient Safety Strategy. Ann. Intern. Med. 2013, 158, 390–396. [Google Scholar] [CrossRef] [Green Version]
- Severo, I.M.; Kuchenbecker, R.; Vieira, D.F.V.B.; Pinto, L.R.C.; Hervé, M.E.W.; Lucena, A.F.; Almeida, M.A. A predictive model for fall risk in hospitalized adults: A case-control study. J. Adv. Nurs. 2018, 75, 563–572. [Google Scholar] [CrossRef]
- Pasa, T.S.; Magnago, T.S.B.D.S.; Urbanetto, J.D.S.; Baratto, M.A.M.; Morais, B.X.; Carollo, J.B. Risk assessment and incidence of falls in adult hospitalized patients 1. Rev. Lat. Am. Enferm. 2017, 25, 2862. [Google Scholar] [CrossRef]
- Hou, W.-H.; Kang, C.-M.; Ho, M.; Kuo, J.M.-C.; Chen, H.-L.; Chang, W.-Y. Evaluation of an inpatient fall risk screening tool to identify the most critical fall risk factors in inpatients. J. Clin. Nurs. 2016, 26, 698–706. [Google Scholar] [CrossRef]
- Fridman, V. Redesigning a Fall Prevention Program in Acute Care: Building on Evidence. Clin. Geriatr. Med. 2019, 35, 265–271. [Google Scholar] [CrossRef]
- Avanecean, D.; Calliste, D.; Contreras, T.; Lim, Y.; Fitzpatrick, A. Effectiveness of patient-centered interventions on falls in the acute care setting compared to usual care. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 3006–3048. [Google Scholar] [CrossRef] [PubMed]
- Arribas Cachá, A.; Hernández Mellado, M.; Sellán Soto, C.; Santamaría García, J.M.; Díaz Martínez, M.L. Delimitación de la estructura normalizada del “Proceso de Valoración Enfermera” (I). NURE Inv. 2014, 11, 1–8. Available online: http://www.nureinvestigacion.es/OJS/index.php/nure/article/view/661/650 (accessed on 18 April 2020).
- Ahtisham, Y.; Jacoline, S. Integrating nursing theory and process into practice; Virginia’s Henderson Need Theory. Int. J. Caring Sci. 2015, 8, 443–450. Available online: http://www.internationaljournalofcaringsciences.org/docs/23_ahtisham.pdf (accessed on 18 April 2020).
- Lazenby, M. On the humanities of nursing. Nurs. Outlook. 2013, 61, e9–e14. [Google Scholar] [CrossRef] [PubMed]
- Bueno-García, M.J.; Roldán-Chicano, M.T.; Rodríguez-Tello, J.; Meroño-Rivera, M.D.; Dávila-Martínez, R.; Berenguer-García, N. Características de la escala Downton en la valoración del riesgo de caídas en pacientes hospitalizados. Enfermería Clín. 2017, 27, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, R.; Winning, K.; Uter, W.; Lesser, S.; Stehle, P.; Sieber, C.C.; Bauer, J.M. Comparison of two different approaches for the application of the mini nutritional assessment in nursing homes: Resident interviews versus assessment by nursing staff. J. Nutr. Health Aging. 2009, 13, 863–869. [Google Scholar] [CrossRef]
- Oliveira, D.U.; Ercole, F.F.; de Melo, L.S.; de Matos, S.S.; Campos, C.C.; Fonseca, E.A.M. Evaluation of falls in hospitalized elderly. Rev. Enferm. UFPE 2017, 11, 4589–4597. [Google Scholar] [CrossRef]
- Romano Duran, E.; Rodriguez Camarero, G.F.; Hernández Martínez-Esparza, E. Incidence and characteristics falls in a hospital intermediate care of Barcelona. Gerokomos 2017, 28, 78–82. Available online: http://www.gerokomos.com/wp-content/uploads/2017/07/28-2-2017-078.pdf (accessed on 18 April 2020).
- Aliaga, B.; Molina, N.; Noguera, M.; Espinoza, P.; Sánchez, S.; Lara, B.; Carrasco, M.; Eymin, G. Prevalencia de pacientes con alto riesgo de caídas en un servicio médico-quirúrgico de un hospital universitario. Revista Médica Chile 2018, 146, 862–868. [Google Scholar] [CrossRef] [Green Version]
- Chang, J.T.; Morton, S.C.; Rubenstein, L.Z.; Mojica, W.A.; Maglione, M.; Suttorp, M.J.; Roth, E.A.; Shekelle, P.G. Interventions for the prevention of falls in older adults: Systematic review and meta-analysis of randomised clinical trials. BMJ 2004, 328, 680. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, L.H.; Vu, G.T.; Ha, G.H.; Nguyen, C.T.; Vu, H.M.; Nguyen, T.Q.; Tran, T.H.; Pham, K.T.H.; Latkin, C.A.; Tran, B.X.; et al. Fear of Falling among Older Patients Admitted to Hospital after Falls in Vietnam: Prevalence, Associated Factors and Correlation with Impaired Health-Related Quality of Life. Int. J. Environ. Res. Public Health 2020, 17, 2493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, K.D.; Vu, M.; Walsh, W. Falls in the acute hospital setting—Impact on resource utilisation. Aust. Health Rev. 2007, 31, 471–477. [Google Scholar] [CrossRef] [PubMed]
- López-Soto, P.J.; Smolensky, M.H.; Sackett-Lundeen, L.L.; De Giorgi, A.; Rodríguez-Borrego, M.A.; Manfredini, R.; Pelati, C.; Fabbian, F. Temporal Patterns of In-Hospital Falls of Elderly Patients. Nurs. Res. 2016, 65, 435–445. [Google Scholar] [CrossRef]
- Laguna-Parras, J.M.; Carrascosa-Corral, R.R.; Zafra López, F.; Carrascosa-García, M.T.; Luque Martínez, F.M.; Alejo Esteban, J.A.; García-Fernández, F.P. Effectiveness of interventions for prevention falls in the elderly: Systematic review. Gerokomos 2010, 21, 97–107. [Google Scholar] [CrossRef]
- Quigley, P.A.; Barnett, S.D.; Bulat, T.; Friedman, Y. Reducing Falls and Fall-Related Injuries in Medical-Surgical Units. J. Nurs. Care Qual. 2016, 31, 1–145. [Google Scholar] [CrossRef] [PubMed]
- Hernández Herrera, D.E.; Barcellos Dalri, M.C.; Marin da Silva Canini, S.R.; Villarreal Rios, E.; Campos de Carvalho, E. Factores de riesgo de caídas en adultos hospitalizados. Desarro. Cientif Enferm. 2011, 19, 171–174. Available online: http://www.index-f.com/dce/19pdf/19-171.pdf (accessed on 18 April 2020).
- Van Gaal, B.G.I.; Schoonhoven, L.; Groot, J.A.M.-D.; Defloor, T.; Habets, H.; Voss, A.; Van Achterberg, T.; Koopmans, R.T. Concurrent Incidence of Adverse Events in Hospitals and Nursing Homes. J. Nurs. Sch. 2013, 46, 187–198. [Google Scholar] [CrossRef]
- AbuAlRub, R.F.; Abu Alhijaa, E.H. The Impact of Educational Interventions on Enhancing Perceptions of Patient Safety Culture Among Jordanian Senior Nurses. Nurs. Forum. 2014, 49, 139–150. [Google Scholar] [CrossRef]
- Kuhlenschmidt, M.L.; Reeber, C.; Wallace, C.; Chen, Y.; Sloan, A.E.; Mazanec, S.R. Tailoring Education to Perceived Fall Risk in Hospitalized Patients with Cancer: A Randomized, Controlled Trial. Clin. J. Oncol. Nurs. 2016, 20, 84–89. [Google Scholar] [CrossRef] [Green Version]
- Manchester, J.; Gray-Miceli, D.; Metcalf, J.A.; Paolini, C.A.; Napier, A.H.; Coogle, C.L.; Owens, M.G. Facilitating Lewin’s change model with collaborative evaluation in promoting evidence based practices of health professionals. Eval. Program Plan. 2014, 47, 82–90. [Google Scholar] [CrossRef] [Green Version]
- Bunn, F.; Dickinson, A.; Simpson, C.; Narayanan, V.; Humphrey, D.; Griffiths, C.; Martin, W.; Victor, C. Preventing falls among older people with mental health problems: A systematic review. BMC Nurs. 2014, 13, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gea-Caballero, V.; Castro-Sánchez, E.; Juárez-Vela, R.; Díaz-Herrera, M.Á.; De Miguel-Montoya, I.; Martínez-Riera, J.R. Elementos esenciales de los entornos profesionales enfermeros en Atención Primaria y su influencia en la calidad del cuidado. Enfermería Clín. 2018, 28, 27–35. [Google Scholar] [CrossRef] [Green Version]
| Variables | Totals n = 581 n (%) | Control Group n = 278 n (%) | Intervention Group n = 303 n (%) |
|---|---|---|---|
| Gender: | |||
| Men | 294 (50.6) | 135 (48.6) | 159 (52.5) |
| Women | 287 (49.4) | 143 (51.4) | 144 (47.5) |
| Mean Age ± Standard Deviation | 68.3 ± 16.2 | 66.78 ± 17.08 | 69.67 ± 15.32 |
| Age Group: | |||
| 15–50 years | 85 (14.6) | 51 (18.3) | 34 (11.2) |
| 51–64 years | 105 (18.1) | 47 (16.9) | 58 (19.1) |
| 65–79 years | 224 (38.6) | 107 (38.5) | 117 (38.6) |
| ≥80 years | 167 (28.7) | 73 (26.3) | 73 (26.3) |
| Nurse assessment on admission: | |||
| Traditional Method | 372 (69) | 269 (96.8) | 103 (34) |
| Systematic method | 209 (31) | 9 (3.2) | 200 (66) |
| Risk assessment of falls on admission: | |||
| Yes | 213 (36.7) | 10 (3.6) | 203 (67.0) |
| No | 368 (63.3) | 268 (96.4) | 100 (33.0) |
| Average Hospital Stay | |||
| ± Standard Deviation (days) | 12.2 ± 9 | 13.71 ± 10.19 | 10.89 ± 7.49 |
| Days interval: | |||
| 0 to 7 days | 205 (35.3) | 76 (27.3) | 128 (42.4) |
| ≥8 days | 376 (63.7) | 202 (72.7) | 174 (57.6) |
| Mobility | |||
| None (bed-to-armchair) | 146 (25.1) | 65 (23.4) | 81 (26.7) |
| Unaided in room/bathroom | 124 (21.3) | 45 (16.5) | 78 (25.7) |
| Unaided outside the room | 311 (53.5) | 167 (60.1) | 144 (47.5) |
| Surgical intervention: | |||
| Yes | 270 (46.5) | 42 (15.1) | 228 (75.2) |
| No | 311 (53.5) | 236 (84.9) | 75 (24.8) |
| Altered consciousness: | |||
| Yes | 59 (10.2) | 41 (14.7) | 18 (5.9) |
| No | 522 (89.8) | 237 (85.3) | 285 (94.1) |
| Nutritional status: | |||
| Risk and/or malnutrition | 272 (46.8) | 150 (54) | 122 (40.3) |
| Normal nutritional status | 309 (53.2) | 128 (46) | 181 (59.7) |
| Supply of Oxygen: | |||
| Yes | 119 (20.5) | 50 (18) | 69 (22.8) |
| No | 462 (79.5) | 228 (82) | 233 (77.2) |
| Catheters (intravenous line, gastric, bladder tube, drainage): | |||
| None | 7 | 5 (1.8) | 3 (1) |
| Has one catheter | 263 | 205 (73.7) | 96 (31.7) |
| Has 2 or more catheters | 308 | 68 (24.5) | 204 (67.3) |
| Variables | Falls | |
|---|---|---|
| No n (%) | Yes n (%) | |
| Gender | ||
| Men | 288 (50.2) | 6 (85.7) |
| Women | 286 (49.8) | 1 (14.3) |
| Age | ||
| 15–50 years | 85 (14.8) | 0 (0) |
| 51–64 years | 104 (18.1) | 1 (14.2) |
| 65–79 years | 221 (38.5) | 3 (42.9) |
| ≥80 years | 85 (14.8) | 3 (42.9) |
| Nursing Units | ||
| General Internal Medicine | 135 (23.5) | 4 (57.1) |
| Neurology/Neurosurgery | 137 (23.9) | 2 (28.2) |
| Traumatology/Urology | 206 (35.9) | 0 (0) |
| Vascular Surgery/Nephrology | 96 (16.7) | 1 (14.2) |
| Groups | ||
| Intervention | 302 (52.6) | 1 (14.3) |
| Control | 272 (47.4) | 6 (85.7) |
| Nurse assessment on admission | ||
| Traditional Method | 208 (36.2) | 1 (14.3) |
| Systematic method | 366 (63.1) | 6 (85.7) |
| Risk assessment of falls on admission | ||
| No | 212 (36.2) | 6 (85.7) |
| Yes | 362 (63.8) | 1 (14.3) |
| Hospital Stay (days) | ||
| 0–7 days | 204 (35.5) | 1 (14.3) |
| ≥8 days | 370 (64.6) | 6 (85.7) |
| Mobility | ||
| None (bed-to-armchair) | 146 (25.4) | 0 (0) |
| Unaided in room/bathroom | 120 (20.9) | 4 (57.1) |
| Unaided outside the room | 308 (53.7) | 3 (42.9) |
| Surgical intervention | ||
| Yes | 264 (46) | 1 (14.2) |
| No | 310 (54) | 6 (85.7) |
| Altered consciousness | ||
| Yes | 59 (10.3) | 0 (0) |
| No | 515 (89.7) | 7 (100) |
| Nutritional status on admission | ||
| Risk and/or malnutrition | 267 (46.5) | 5 (71.4) |
| Normal nutritional status | 307 (53.5) | 2 (28.6) |
| Supply of Oxygen | ||
| Yes | 117 (20.4) | 2 (28.6) |
| No | 457 (79.6) | 5 (71.4) |
| Catheter (intravenous, gastric/bladder, drainage) | ||
| None | 8 (1.4) | 0 (0) |
| Has one catheter | 294 (51.2) | 7 (100) |
| Has 2 or more catheters | 272 (47.4) | 0 (28.6) |
| Estimate | Std. Error | OR * | Lower 95% | Upper 95% | |
|---|---|---|---|---|---|
| Intercept | −6842 | 2581 | 0.001 | 0 | 0.088 |
| Intervention Group | −2062 | 1054 | 0.127 | 0.013 | 0.821 |
| Stay | −0.04 | 0.053 | 0.961 | 0.849 | 1044 |
| Age | 0.045 | 0.032 | 1,046 | 0.991 | 1119 |
| WAIC | 76,754 | 23,922 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montejano-Lozoya, R.; Miguel-Montoya, I.; Gea-Caballero, V.; Mármol-López, M.I.; Ruíz-Hontangas, A.; Ortí-Lucas, R. Impact of Nurses’ Intervention in the Prevention of Falls in Hospitalized Patients. Int. J. Environ. Res. Public Health 2020, 17, 6048. https://doi.org/10.3390/ijerph17176048
Montejano-Lozoya R, Miguel-Montoya I, Gea-Caballero V, Mármol-López MI, Ruíz-Hontangas A, Ortí-Lucas R. Impact of Nurses’ Intervention in the Prevention of Falls in Hospitalized Patients. International Journal of Environmental Research and Public Health. 2020; 17(17):6048. https://doi.org/10.3390/ijerph17176048
Chicago/Turabian StyleMontejano-Lozoya, Raimunda, Isabel Miguel-Montoya, Vicente Gea-Caballero, María Isabel Mármol-López, Antonio Ruíz-Hontangas, and Rafael Ortí-Lucas. 2020. "Impact of Nurses’ Intervention in the Prevention of Falls in Hospitalized Patients" International Journal of Environmental Research and Public Health 17, no. 17: 6048. https://doi.org/10.3390/ijerph17176048
APA StyleMontejano-Lozoya, R., Miguel-Montoya, I., Gea-Caballero, V., Mármol-López, M. I., Ruíz-Hontangas, A., & Ortí-Lucas, R. (2020). Impact of Nurses’ Intervention in the Prevention of Falls in Hospitalized Patients. International Journal of Environmental Research and Public Health, 17(17), 6048. https://doi.org/10.3390/ijerph17176048





