The Role of Health Literacy in Explaining the Relation between Educational Level and Decision Making about Colorectal Cancer Screening
Abstract
1. Introduction
2. Methods
2.1. Study Participants
2.2. Data Collection
2.3. Independent Variable
2.4. Mediators
2.5. Dependent Variables
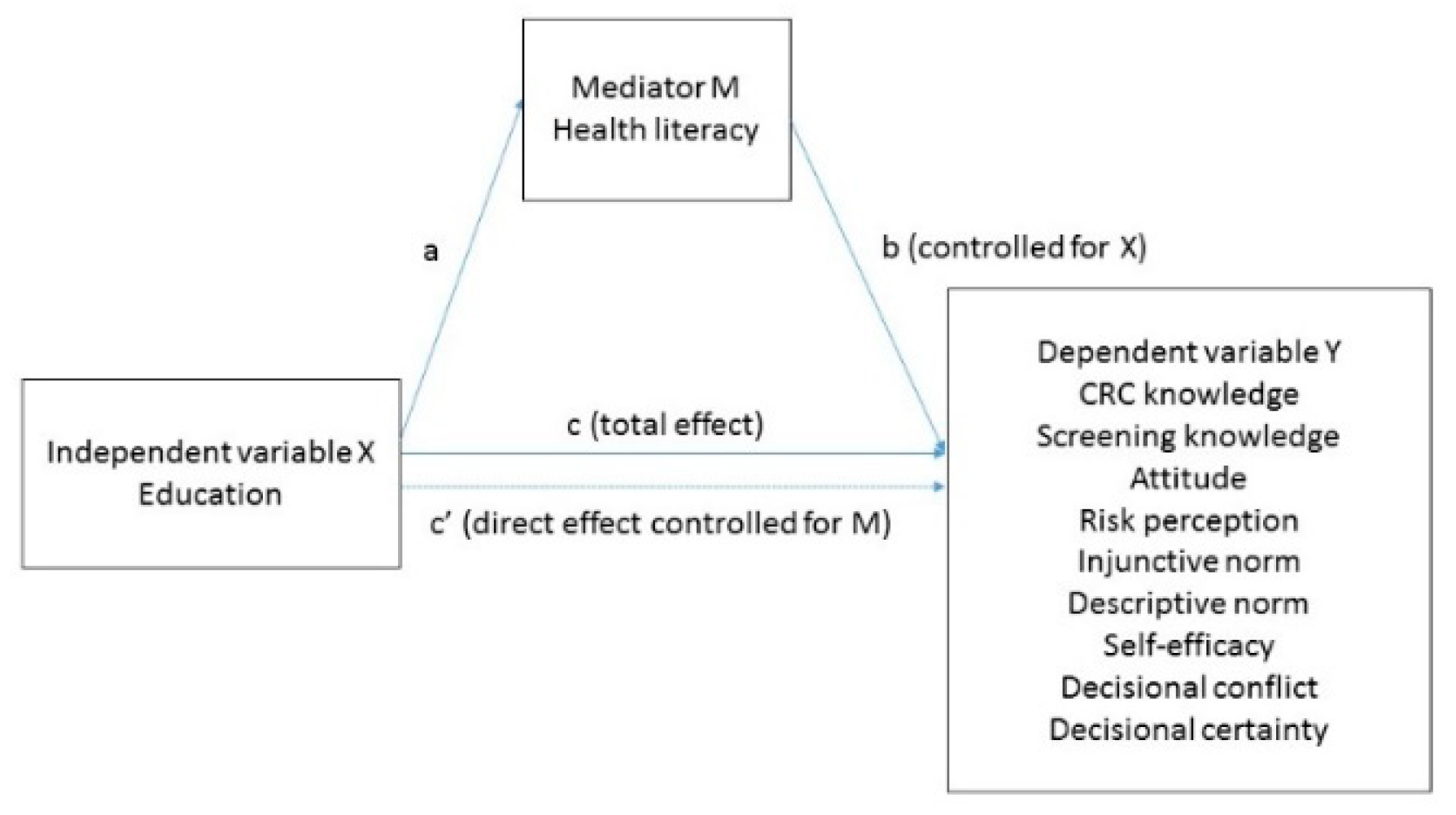
2.6. Data Analysis
2.7. Ethical considerations
3. Results
3.1. Descriptive Statistics
3.2. Education and Health Literacy Domains (a-Path)
3.3. Health Literacy Domains and Elements of Informed Decision Making (b-Path)
3.4. Education and Elements of Informed Decision Making (c-Path)
3.5. Education and Informed Decision Making Mediated through Health Literacy Domains (ab-Path)
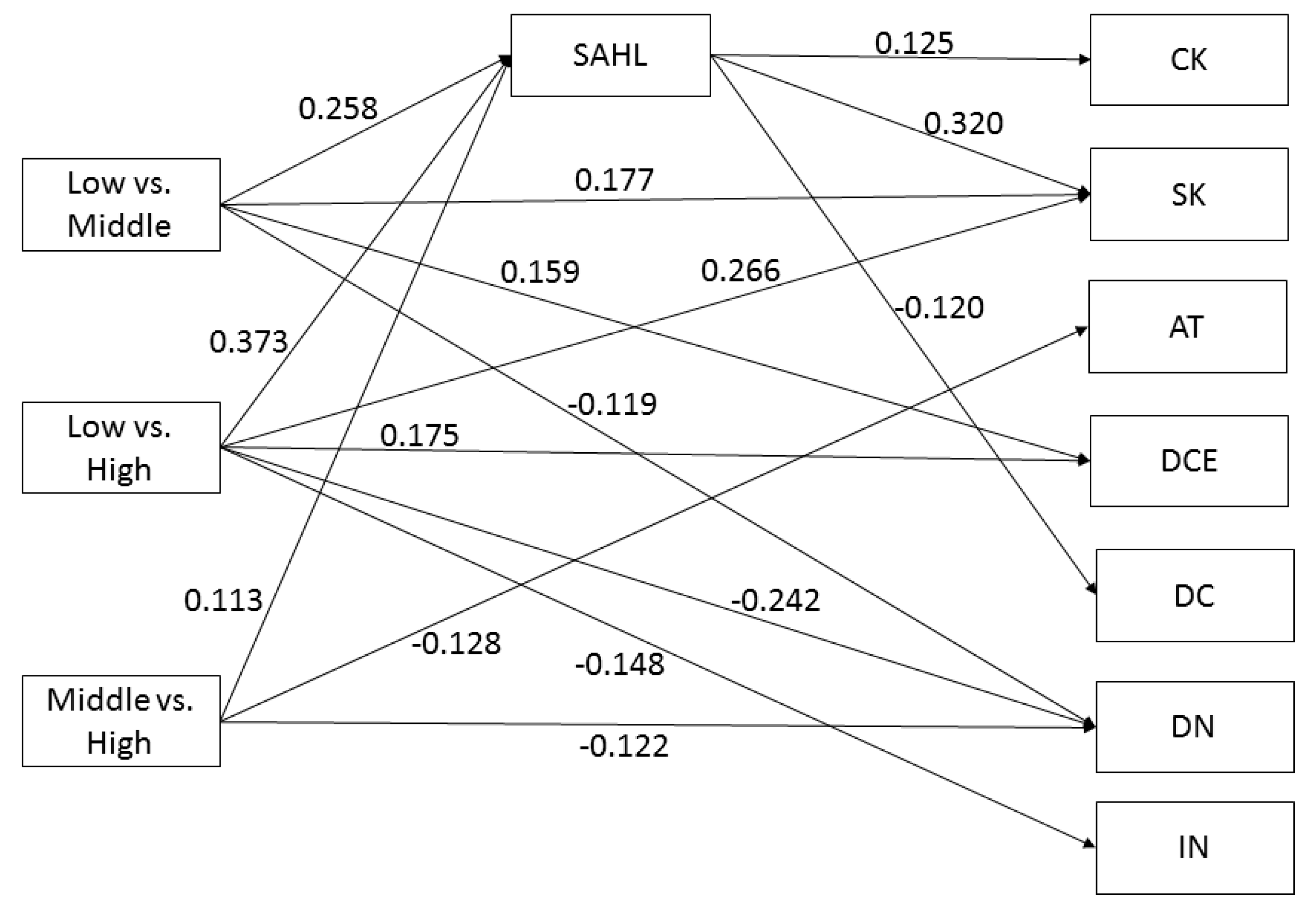
3.5.1. Mediator: Comprehension
3.5.2. Mediator: Application
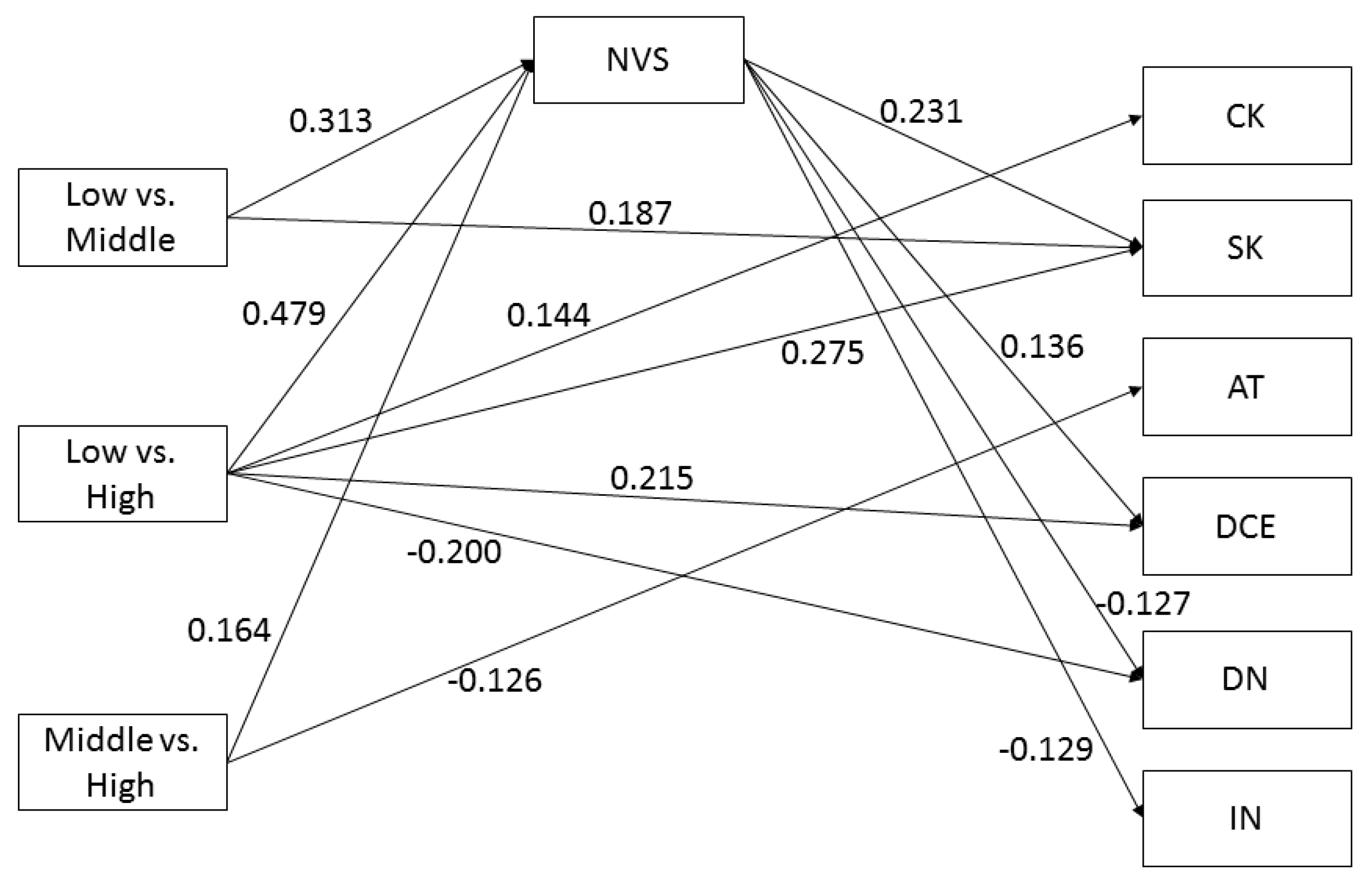
3.5.3. Mediator: Numeracy
3.5.4. Mediator: Communication
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- European Colorectal Cancer Screening Guidelines Working Group; von Karsa, L.; Patnick, J.; Segnan, N.; Atkin, W.; Halloran, S.; Lansdorp-Vogelaar, I.; Malila, N.; Minozzi, S.; Moss, S.; et al. European guidelines for quality assurance in colorectal cancer screening and diagnosis: Overview and introduction to the full supplement publication. Endoscopy 2013, 45, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, B. Ethical issues with colorectal cancer screening-a systematic review. J. Eval. Clin. Pract. 2017, 23, 631–641. [Google Scholar] [CrossRef] [PubMed]
- Hasnain-Wynia, R.; Wolf, M.S. Promoting health care equity: Is health literacy a missing link? Health Serv. Res. 2010, 45, 897–903. [Google Scholar] [CrossRef] [PubMed]
- Rimer, B.K.; Briss, P.A.; Zeller, P.K.; Chan, E.C.Y.; Woolf, S.H. Informed decision making: What is its role in cancer screening? Cancer Interdiscip. Int. J. Am. Cancer Soc. 2004, 101, 1214–1228. [Google Scholar] [CrossRef] [PubMed]
- Dharni, N.; Armstrong, D.; Chung-Faye, G.; Wright, A.J. Factors influencing participation in colorectal cancer screening—a qualitative study in an ethnic and socio-economically diverse inner city population. Health Expect. 2017, 20, 608–617. [Google Scholar] [CrossRef]
- McCaffery, K.; Wardle, J.; Waller, J. Knowledge, attitudes, and behavioral intentions in relation to the early detection of colorectal cancer in the United Kingdom. Prev. Med. 2003, 36, 525–535. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Health literacy: Report of the Council on Scientific Affairs. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. JAMA 1999, 281, 552–557.
- Chesser, A.K.; Keene Woods, N.; Smothers, K.; Rogers, N. Health Literacy and Older Adults: A Systematic Review. Gerontol. Geriatr. Med. 2016, 2, 2333721416630492. [Google Scholar] [CrossRef]
- Van der Heide, I.; Uiters, E.; Jantine Schuit, A.; Rademakers, J.; Fransen, M. Health literacy and informed decision making regarding colorectal cancer screening: A systematic review. Eur. J. Public Health 2015, 25, 575–582. [Google Scholar] [CrossRef]
- Arnold, C.L.; Rademaker, A.; Bailey, S.C.; Esparza, J.M.; Reynolds, C.; Liu, D.; Platt, D.; Davis, T.C. Literacy barriers to colorectal cancer screening in community clinics. J. Health Commun. 2012, 17, 252–264. [Google Scholar] [CrossRef] [PubMed]
- Mitsutake, S.; Shibata, A.; Ishii, K.; Oka, K. Association of eHealth literacy with colorectal cancer knowledge and screening practice among internet users in Japan. J. Med. Internet Res. 2012, 14, e153. [Google Scholar] [CrossRef] [PubMed]
- Von Wagner, C.; Semmler, C.; Good, A.; Wardle, J. Health literacy and self-efficacy for participating in colorectal cancer screening: The role of information processing. Patient Educ. Couns. 2009, 75, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Peterson, N.B.; Dwyer, K.A.; Mulvaney, S.A.; Dietrich, M.S.; Rothman, R.L. The influence of health literacy on colorectal cancer screening knowledge, beliefs and behavior. J. Natl. Med. Assoc. 2007, 99, 1105–1112. [Google Scholar]
- Woudstra, A.J.; Timmermans, D.R.M.; Uiters, E.; Dekker, E.; Smets, E.M.A.; Fransen, M.P. Health literacy skills for informed decision making in colorectal cancer screening: Perceptions of screening invitees and experts. Health Expect. 2018, 21, 636–646. [Google Scholar] [CrossRef]
- Smith, S.K.; Nutbeam, D.; McCaffery, K.J. Insights into the concept and measurement of health literacy from a study of shared decision-making in a low literacy population. J. Health Psychol. 2013, 18, 1011–1022. [Google Scholar] [CrossRef]
- Janz, N.K.; Becker, M.H. The Health Belief Model: A Decade Later; John Wiley & Sons. Inc.: Hoboken, NJ, USA, 1984; Volume 11. [Google Scholar]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Rawl, S.; Champion, V.; Menon, U.; Loehrer, P.J.; Vance, G.H.; Skinner, C.S. Validation of Scales to Measure Benefits of and Barriers to Colorectal Cancer Screening. J. Psychosoc. Oncol. 2001, 19, 47–63. [Google Scholar] [CrossRef]
- Sieverding, M.; Decker, S.; Zimmermann, F. Information About Low Participation in Cancer Screening Demotivates Other People. Psychol. Sci. 2010, 21, 941–943. [Google Scholar] [CrossRef]
- RIVM. Bevolkingsonderzoek Darmkanker [Colorectal Cancer Screening Programme]. Available online: https://www.rivm.nl/bevolkingsonderzoek-darmkanker (accessed on 31 May 2019).
- UNESCO Instiute for Statistics. International Standard Classification of Education; UNESCO: Paris, France, 2014. [Google Scholar]
- Woudstra, A.J.; Smets, E.M.A.; Galenkamp, H.; Fransen, M.P. Validation of health literacy domains for informed decision making about colorectal cancer screening using classical test theory and item response theory. Patient Educ. Couns. 2019, 102, 2335–2343. [Google Scholar] [CrossRef]
- Pander Maat, H.; Essink-Bot, M.L.; Leenaars, K.E.; Fransen, M.P. A short assessment of health literacy (SAHL) in the Netherlands. BMC Public Health 2014, 14, 990. [Google Scholar] [CrossRef] [PubMed]
- Woudstra, A.J.; Meppelink, C.S.; Pander Maat, H.; Oosterhaven, J.; Fransen, M.P.; Dima, A.L. Validation of the short assessment of health literacy (SAHL-D) and short-form development: Rasch analysis. BMC Med. Res. Methodol. 2019, 19, 122. [Google Scholar] [CrossRef] [PubMed]
- Fransen, M.P.; Leenaars, K.E.; Rowlands, G.; Weiss, B.D.; Maat, H.P.; Essink-Bot, M.L. International application of health literacy measures: Adaptation and validation of the newest vital sign in The Netherlands. Patient Educ. Couns. 2014, 97, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Lipkus, I.M.; Samsa, G.; Rimer, B.K. General performance on a numeracy scale among highly educated samples. Med. Decis. Mak. Int. J. Soc. Med Decis. Mak. 2001, 21, 37–44. [Google Scholar] [CrossRef]
- Ten Klooster, P.M.; Oostveen, J.C.; Zandbelt, L.C.; Taal, E.; Drossaert, C.H.; Harmsen, E.J.; van de Laar, M.A. Further validation of the 5-item Perceived Efficacy in Patient-Physician Interactions (PEPPI-5) scale in patients with osteoarthritis. Patient Educ. Couns. 2012, 87, 125–130. [Google Scholar] [CrossRef]
- Denters, M.J.; Deutekom, M.; Essink-Bot, M.-L.; Bossuyt, P.M.; Fockens, P.; Dekker, E. Assessing knowledge and attitudes towards screening among users of Faecal Immunochemical Test (FIT). Health Expect. Int. J. Public Particip. Health Care Health Policy 2015, 18, 839–849. [Google Scholar] [CrossRef]
- O’Connor, A.M. Validation of a decisional conflict scale. Med. Decis. Mak. 1995, 15, 25–30. [Google Scholar] [CrossRef]
- Essink-Bot, M.L.; Dekker, E.; Timmermans, D.R.M.; Uiters, E.; Fransen, M.P. Knowledge and Informed Decision-Making about Population-Based Colorectal Cancer Screening Participation in Groups with Low and Adequate Health Literacy. Gastroenterol. Res. Pract. 2016, 2016, 7292369. [Google Scholar] [CrossRef]
- McKinnon, D.P. Introduction to Statistical Mediation Analysis; Lawrence Erlbaum Associates: New York, NY, USA, 2008. [Google Scholar]
- Gunzler, D.; Chen, T.; Wu, P.; Zhang, H. Introduction to mediation analysis with structural equation modeling. Shanghai Arch. Psychiatry 2013, 25, 390–394. [Google Scholar]
- Hayes, A.F.; Preacher, K.J. Statistical mediation analysis with a multicategorical independent variable. Br. J. Math. Stat. Psychol. 2014, 67, 451–470. [Google Scholar] [CrossRef]
- MacKinnon, D.P.; Fairchild, A.J.; Fritz, M.S. Mediation analysis. Annu. Rev. Psychol. 2007, 58, 593–614. [Google Scholar] [CrossRef] [PubMed]
- Kenny, D.A. Mediation. Available online: http://davidakenny.net/cm/mediate.htm (accessed on 31 October 2019).
- Wen, Z.; Fan, X. Monotonicity of effect sizes: Questioning kappa-squared as mediation effect size measure. Psychol. Methods 2015, 20, 193–203. [Google Scholar] [CrossRef] [PubMed]
- McCaffery, K.J.; Holmes-Rovner, M.; Smith, S.K.; Rovner, D.; Nutbeam, D.; Clayman, M.L.; Kelly-Blake, K.; Wolf, M.S.; Sheridan, S.L. Addressing health literacy in patient decision aids. BMC Med. Inf. Decis. Mak. 2013, 13, S2–S10. [Google Scholar] [CrossRef] [PubMed]
- Gabel, P.; Larsen, M.B.; Edwards, A.; Kirkegaard, P.; Andersen, B. Knowledge, attitudes, and worries among different health literacy groups before receiving first invitation to colorectal cancer screening: Cross-sectional study. Prev. Med. Rep. 2019, 14, 100876. [Google Scholar] [CrossRef] [PubMed]
- Von Wagner, C.; Hirst, Y.; Waller, J.; Ghanouni, A.; McGregor, L.M.; Kerrison, R.S.; Verstraete, W.; Vlaev, I.; Sieverding, M.; Stoffel, S.T. The impact of descriptive norms on motivation to participate in cancer screening–Evidence from online experiments. Patient Educ. Couns. 2019, 102, 1621–1628. [Google Scholar] [CrossRef] [PubMed]
- Van der Heide, I.; Wang, J.; Droomers, M.; Spreeuwenberg, P.; Rademakers, J.; Uiters, E. The Relationship Between Health, Education, and Health Literacy: Results From the Dutch Adult Literacy and Life Skills Survey. J. Health Commun. 2013, 18, 172–184. [Google Scholar] [CrossRef] [PubMed]
- Visscher, B.B.; Steunenberg, B.; Heijmans, M.; Hofstede, J.M.; Devillé, W.; van der Heide, I.; Rademakers, J. Evidence on the effectiveness of health literacy interventions in the EU: A systematic review. BMC Public Health 2018, 18, 1414. [Google Scholar] [CrossRef]
- Marteau, T.M.; Dormandy, E.; Michie, S. A measure of informed choice. Health Expect. Int. J. Public Particip. Health Care Health Policy 2001, 4, 99–108. [Google Scholar] [CrossRef]


| Participant Characteristics | Educational Level | |||
|---|---|---|---|---|
| Low (n = 91) % or Mean (SD) | Middle (n = 155) % or Mean (SD) | High (n = 161) % or Mean (SD) | All % or Mean (SD) | |
| Gender | ||||
| Male | 29 (31.9) | 76 (49.0) | 78 (48.4) | 183 (45.0) |
| Female | 62 (68.1) | 79 (51.0) | 83 (51.6) | 224 (55.0) |
| Read the CRC Screening Information | ||||
| Yes/A bit | 82 (90.1) | 146 (94.2) | 157 (97.5) | 385 (94.6) |
| No | 9 (9.9) | 9 (5.8) | 4 (2.5) | 22 (5.4) |
| Health Literacy Domain/Scale | ||||
| Comprehension/SAHL-D | 7.84 (3.28) a,b | 9.46 (2.84) b,c | 10.17 (2.84) a,c | 9.38 (3.07) |
| Numeracy/Risk | 1.43 (1.07) a,b | 2.2 (1.21) b,c | 2.70 (1.23) a,c | 2.23 (1.28) |
| Application/NVS-D | 3.58 (1.68) a,b | 4.61 (1.56) b,c | 5.15 (1.30) a,c | 4.59 (1.60) |
| Communication/PEPPI | 20.27 (2.26) | 20.04 (2.78) | 20.52 (2.92) | 20.28 (2.73) |
| IDM Elements | ||||
| CRC Knowledge | 4.22 (1.13) | 4.50 (1.03) | 4.55 (0.98) | 4.46 (1.04) |
| Screening Knowledge | 8.05 (2.09) a,b | 9.03 (1.75) b,c | 9.50 (1.52) a,c | 9.00 (1.83) |
| Attitude | 41.38 (7.14) | 41.94 (6.66) c | 40.0 (7.59) c | 41.05 (7.18) |
| Decisional Self-efficacy Missing | 4.40 (0.75) 1 (1.1) | 4.48 (0.68) 4 (2.6) | 4.59 (0.63) 1 (0.6) | 4.50 (0.68) 6 (1.5) |
| Risk Perception Missing | 5.67 (1.25) 1 (1.1) | 5.67 (1.17) 4 (2.6) | 5.63 (1.00) 1 (0.6) | 5.65 (1.12) 6 (1.5) |
| Injunctive Norm Missing | 3.39 (1.43) a 1 (1.1) | 3.19 (1.30) 2 (1.3) | 2.89 (1.34) a 0 | 3.11 (1.35) 3 (0.7) |
| Descriptive Norm Missing | 4.24 (0.88) a 1 (1.1) | 3.95 (1.00) 2 (1.3) | 3.68 (1.31) a 0 | 3.91 (1.05) 3 (0.7) |
| Decisional Conflict Missing | 31.33 (22.74) 1 (1.1) | 25.20 (19.38) 5 | 24.72 (20.03) 1 (0.6) | 26.39 (20.56) 7 (1.72) |
| Decisional Certainty Missing | 9.44 (1.55) b 20 (22.0) | 9.93 (1.45) b 25 (16.1) | 10.00 (1.49) 35 (21.7) | 9.85 (1.50) 80 (19.7) |
| Comparison | Effect | CK | SK | AT | SE | RP | IN | DN | DC | DCE |
|---|---|---|---|---|---|---|---|---|---|---|
| Low * vs. Middle Education | Total | 0.129 * | 0.260 * | 0.038 | 0.051 | 0.002 | −0.072 | −0.133 * | −0.147 * | 0.168 * |
| Direct | 0.097 | 0.177 * | 0.047 | 0.034 | 0.007 | −0.050 | −0.119 * | −0.116 | 0.159 * | |
| Indirect | 0.032 * | 0.083 * | −0.009 | 0.016 | −0.005 | −0.022 | −0.014 | −0.031 | 0.009 | |
| Effect size | 0.25 | 0.32 | −0.24 | 0.31 | −2.5 | 0.31 | 0.11 | 0.21 | 0.05 | |
| Low * vs. High Education | Total | 0.156* | 0.386 * | −0.094 | 0.087 | −0.018 | −0.179 * | −0.262 * | −0.157 * | 0.187 * |
| Direct | 0.110 | 0.266 * | −0.081 | 0.063 | −0.011 | −0.148 * | −0.262 * | −0.112 | 0.175 * | |
| Indirect | 0.046 * | 0.119 * | −0.014 | 0.024 | −0.007 | −0.031 | −0.020 | −0.045 * | 0.012 | |
| Effect size | 0.29 | 0.31 | 0.15 | 0.28 | 0.39 | 0.17 | 0.08 | 0.29 | 0.06 | |
| Middle * vs. High Education | Total | 0.026 | 0.124 * | −0.132 * | 0.036 | −0.020 | −0.107 * | −0.128 * | −0.009 | 0.018 |
| Direct | 0.012 | 0.087 | −0.128 * | 0.029 | −0.018 | −0.098 | −0.122 * | 0.004 | 0.014 | |
| Indirect | 0.014 | 0.038 * | −0.004 | 0.007 | −0.002 | −0.010 | −0.006 | −0.014 | 0.004 | |
| Effect size | 0.54 | 0.31 | 0.03 | 0.19 | 0.10 | 0.09 | 0.05 | 1.56 | 0.22 |
| Comparison | Effect | CK | SK | AT | SE | RP | IN | DN | DC | DCE |
|---|---|---|---|---|---|---|---|---|---|---|
| Low * vs. Middle Education | Total | 0.129 * | 0.260 * | 0.038 | 0.058 | 0.002 | −0.070 | −0.132 * | −0.147 * | 0.175 * |
| Direct | 0.121 | 0.187 * | 0.049 | 0.026 | 0.001 | −0.030 | −0.092 | −0.133 * | 0.132 | |
| Indirect | 0.017 | 0.072 * | −0.012 | 0.033 | 0.001 | −0.040 * | −0.040 * | −0.013 | 0.043 * | |
| Effect size | 0.13 | 0.28 | −0.31 | 0.57 | 0.5 | 0.57 | 0.30 | 0.09 | 0.25 | |
| Low * vs. High Education | Total | 0.156 * | 0.386 * | −0.094 | 0.133 | −0.018 | −0.178 * | −0.261 * | −0.157 * | 0.193 * |
| Direct | 0.144 * | 0.275 * | −0.077 | 0.083 | −0.020 | −0.116 * | −0.200 * | −0.137 | 0.127 | |
| Indirect | 0.012 | 0.111 * | −0.018 | 0.050 | 0.002 | −0.062 * | −0.061 * | −0.020 | 0.065 * | |
| Effect size | 0.08 | 0.29 | 0.19 | 0.38 | −0.11 | 0.35 | 0.23 | 0.13 | 0.34 | |
| Middle * vs. High Education | Total | 0.026 | 0.124 * | −0.132 * | 0.074 | −0.020 | −0.107 * | −0.128 * | −0.009 | 0.018 |
| Direct | 0.022 | 0.087 | −0.126 * | 0.057 | −0.021 | −0.086 | −0.107 | −0.002 | 0.014 | |
| Indirect | 0.004 | 0.038 * | −0.006 | 0.017 | 0.001 | −0.021 | −0.021 | −0.007 | 0.004 | |
| Effect size | 0.15 | 0.31 | 0.04 | 0.23 | −0.05 | 0.20 | 0.16 | 0.78 | 0.22 |
| Comparison | Effect | CK | SK | AT | SE | RP | IN | DN | DC | DCE |
|---|---|---|---|---|---|---|---|---|---|---|
| Low * vs. Middle Education | Total | 0.129 * | 0.260 * | 0.038 | 0.051 | 0.002 | −0.071 | −0.133 * | −0.147 * | 0.170 * |
| Direct | 0.117 | 0.197 * | 0.058 | 0.017 | −0.007 | −0.045 | −0.109 | −0.130 | 0.154 | |
| Indirect | 0.012 | 0.063 * | −0.020 | 0.034 * | 0.009 | −0.026 | −0.023 | −0.016 | 0.016 | |
| Effect size | 0.09 | 0.24 | −0.53 | 0.67 | 0.37 | 0.17 | 0.11 | 0.09 | ||
| Low * vs. High Education | Total | 0.156 * | 0.386 * | −0.094 | 0.087 | −0.018 | −0.179 * | −0.262 * | −0.157 * | 0.188 * |
| Direct | 0.136 | 0.281 * | −0.061 | 0.030 | −0.033 | −0.135 | −0.223 * | −0.130 | 0.161 * | |
| Indirect | 0.020 | 0.105 * | −0.034 | 0.057 * | 0.015 | −0.044 | −0.039 | −0.027 | 0.026 | |
| Effect size | 0.128 | 0.27 | 0.36 | 0.66 | −0.83 | 0.25 | 0.15 | 0.17 | 0.14 | |
| Middle * vs. High Education | Total | 0.026 | 0.124 * | −0.132 * | 0.035 | −0.020 | −0.108 * | −0.129 * | −0.009 | 0.017 |
| Direct | 0.018 | 0.041 * | −0.119 * | 0.013 | −0.026 | −0.090 | −0.113 * | 0.001 | 0.006 | |
| Indirect | 0.008 | 0.083 | −0.013 | 0.022 | 0.006 | −0.017 | −0.015 | −0.011 | 0.010 | |
| Effect size | 0.31 | 0.67 | 0.10 | 0.63 | −0.3 | 0.16 | 0.12 | 1.22 | 0.59 |
| Comparison | Effect | CK | SK | AT | SE | RP | IN | DN | DC | DCE |
|---|---|---|---|---|---|---|---|---|---|---|
| Low * vs. Middle Education | Total | 0.129 * | 0.260 * | 0.038 | 0.059 | 0.002 | −0.071 | −0.133 * | −0.147 * | 0.167 * |
| Direct | 0.127 | 0.261 * | 0.046 | 0.066 | 0.004 | −0.002 | −0.128 | −0.149 * | 0.172 * | |
| Indirect | 0.002 | −0.001 | −0.008 | −0.007 | −0.003 | −0.069 | −0.005 | 0.002 | −0.005 | |
| Effect size | - | - | - | - | - | - | - | - | - | |
| Low * vs. High Education | Total | 0.156 * | 0.386 * | −0.094 | 0.134 | −0.018 | −0.179 * | −0.262 * | −0.157 * | 0.186 * |
| Direct | 0.158 * | 0.385 * | −0.103 | 0.126 | −0.021 | −0.181 * | −0.267 * | −0.155 * | 0.182 * | |
| Indirect | −0.002 | 0.001 | 0.008 | 0.008 | 0.003 | 0.002 | 0.005 | −0.002 | 0.005 | |
| Effect size | - | - | - | - | - | - | - | - | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woudstra, A.J.; Smets, E.M.A.; Verdam, M.G.E.; Fransen, M.P. The Role of Health Literacy in Explaining the Relation between Educational Level and Decision Making about Colorectal Cancer Screening. Int. J. Environ. Res. Public Health 2019, 16, 4644. https://doi.org/10.3390/ijerph16234644
Woudstra AJ, Smets EMA, Verdam MGE, Fransen MP. The Role of Health Literacy in Explaining the Relation between Educational Level and Decision Making about Colorectal Cancer Screening. International Journal of Environmental Research and Public Health. 2019; 16(23):4644. https://doi.org/10.3390/ijerph16234644
Chicago/Turabian StyleWoudstra, Anke J., Ellen M. A. Smets, Mathilde G. E. Verdam, and Mirjam P. Fransen. 2019. "The Role of Health Literacy in Explaining the Relation between Educational Level and Decision Making about Colorectal Cancer Screening" International Journal of Environmental Research and Public Health 16, no. 23: 4644. https://doi.org/10.3390/ijerph16234644
APA StyleWoudstra, A. J., Smets, E. M. A., Verdam, M. G. E., & Fransen, M. P. (2019). The Role of Health Literacy in Explaining the Relation between Educational Level and Decision Making about Colorectal Cancer Screening. International Journal of Environmental Research and Public Health, 16(23), 4644. https://doi.org/10.3390/ijerph16234644





