Estimating the Double Burden of Malnutrition among 595,975 Children in 65 Low- and Middle-Income Countries: A Meta-Analysis of Demographic and Health Surveys
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Outcome Variable
2.3. Statistical Analysis
3. Results
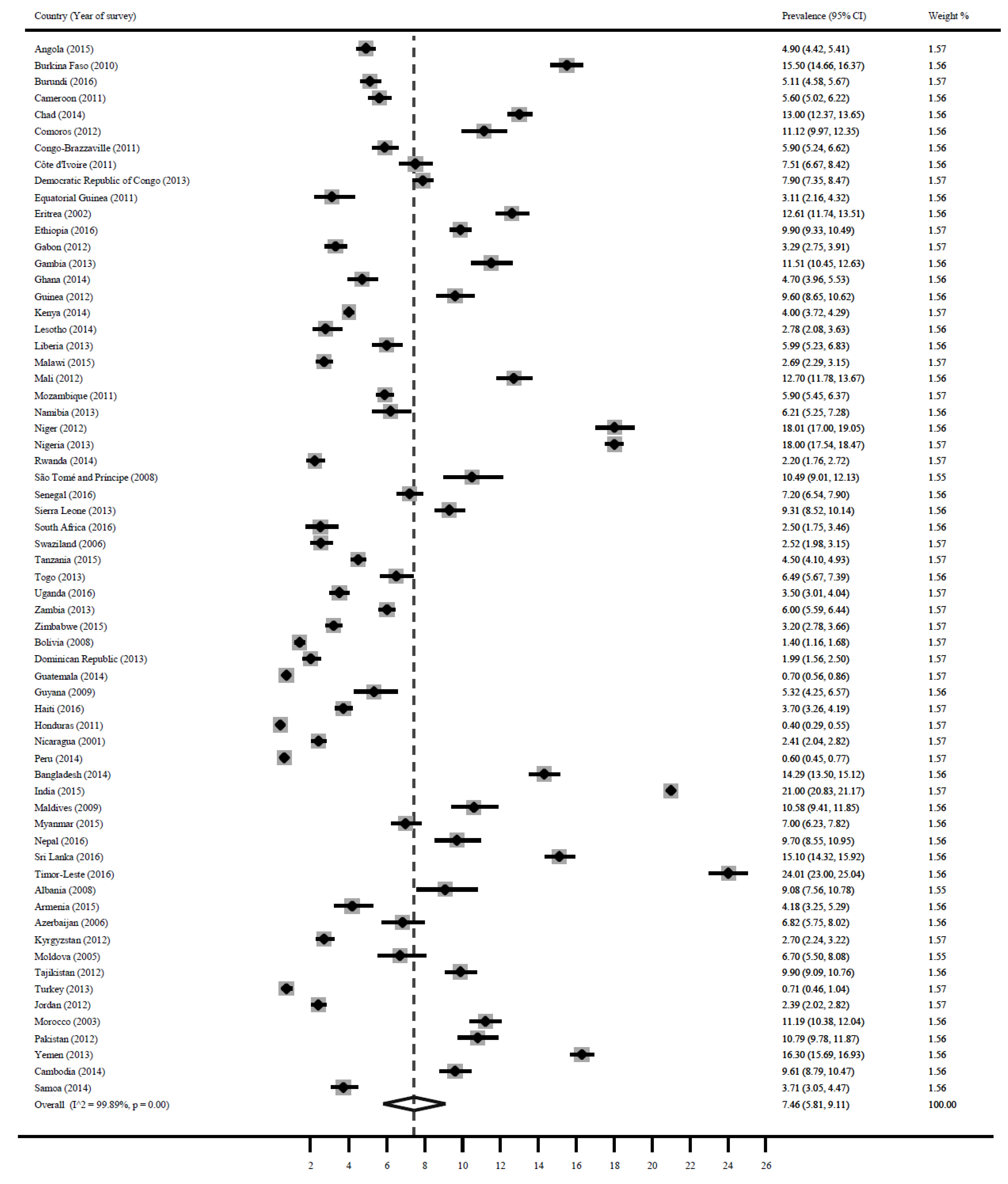
3.1. Stunting
3.2. Wasting
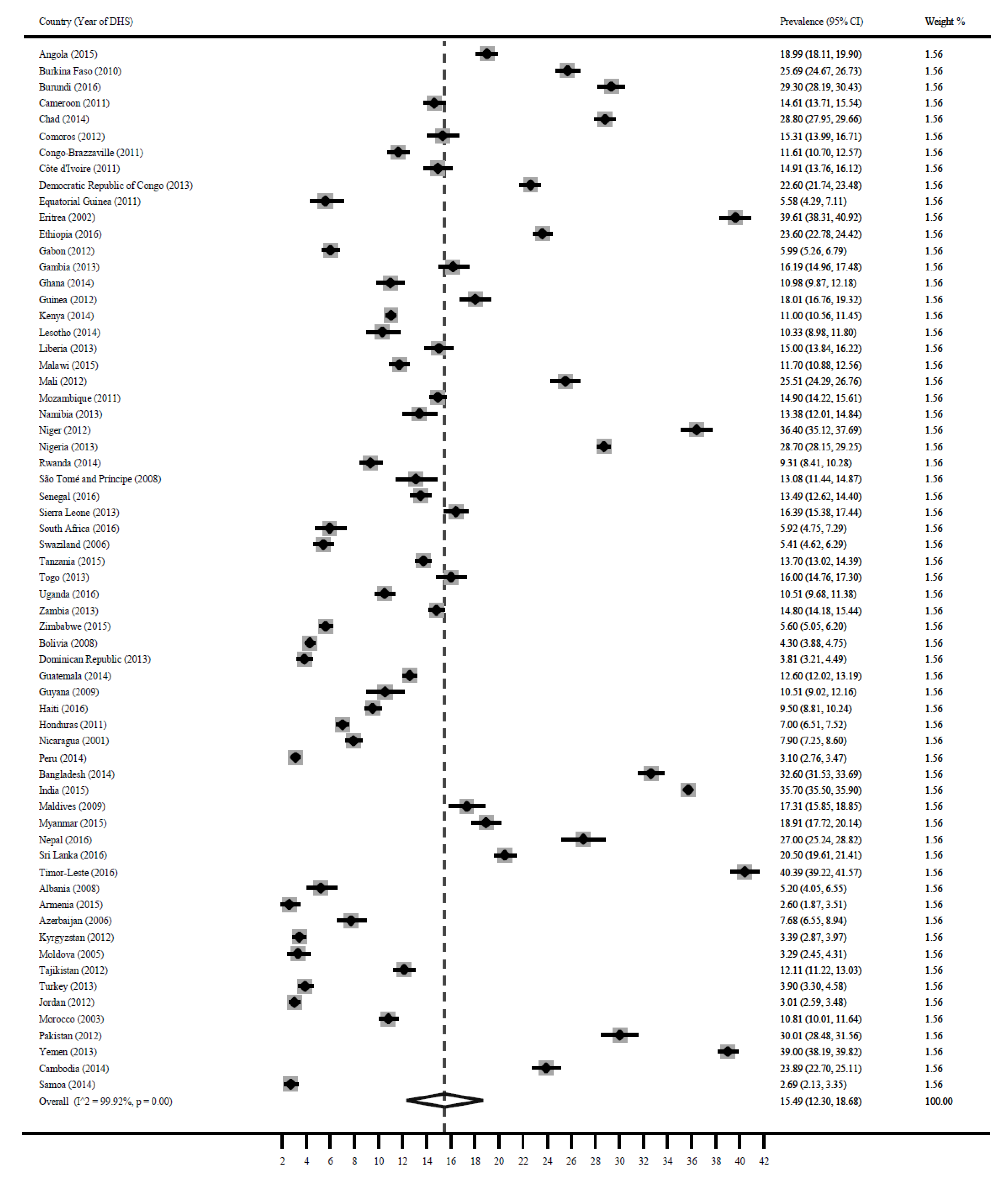
3.3. Underweight
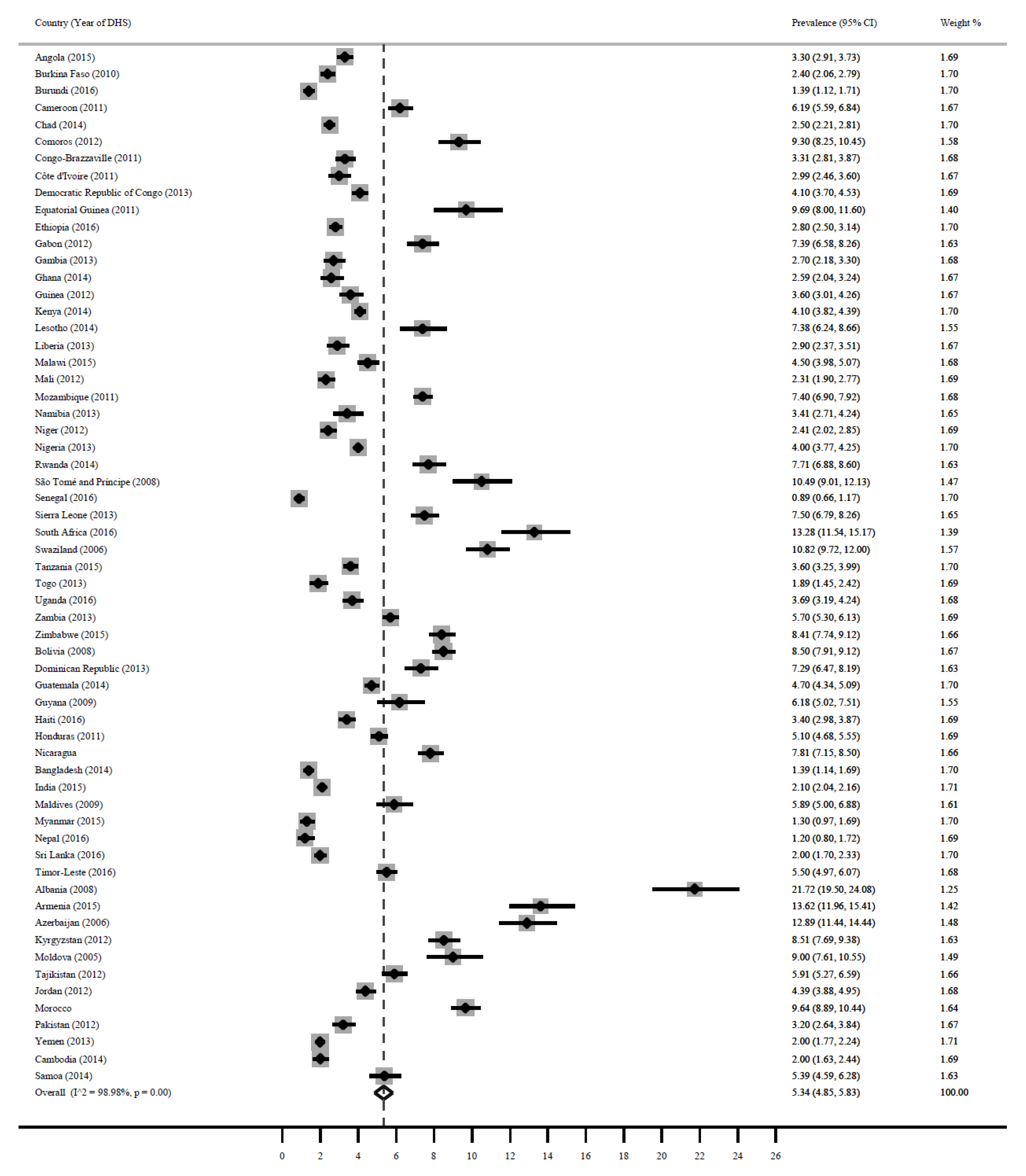
3.4. Overweight/Obesity
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- UNICEF. Improving Child Nutrition: The Achievable Imperative for Global Progress; UNICEF: New York, NY, USA, 2013; pp. 1–14. [Google Scholar]
- Calkins, K.; Devaskar, S.U. Fetal origins of adult disease. Curr. Probl. Pediatr. Adolesc. Health Care 2011, 41, 158–176. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Assessing and Managing Children at Primary Health-Care Facilities to Prevent Overweight and Obesity in the Context of the Double Burden of Malnutrition; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187. [Google Scholar]
- Shrimpton, R.; Rokx, C. Health, Nutrition and Population (HNP) Discussion Paper. In The Double Burden of Malnutrition: A Review of Global Evidence; World Bank: Washington, DC, USA, 2012; Available online: http://documents.worldbank.org/curated/en/905651468339879888/The-double-burden-of-malnutrition-a-review-of-global-evidence (accessed on 12 August 2019).
- Winichagoon, P.; Margetts, B.M. The Double Burden of Malnutrition in Low-and Middle-Income Countries. Available online: https://www.semanticscholar.org/paper/The-double-burden-of-malnutrition-in-low-and-Winichagoon-Margetts/99285f41a7b34b0460e2b46739d223766929c1a0 (accessed on 12 August 2019).
- WHO. Double-Duty Actions: Policy Brief; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- The World Bank. Improving Nutrition through Multi-Sectoral Approaches; The World Bank: Washington, DC, USA, 2013. [Google Scholar]
- United Nations Children’s Fund. UNICEF’s Approach to Scaling Up Nutrition for Mothers and Their Children; UNICEF: New York, NY, USA, 2015. [Google Scholar]
- The DHS Program. Available online: http://dhsprogram.com/data/data-collection.cfm (accessed on 12 August 2019).
- DHS Methodological Reports 14. 2014. Available online: https://www.dhsprogram.com/pubs/pdf/MR16/MR16.pdf (accessed on 12 August 2019).
- De Onis, M. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- World Health Organization. Global Nutrition Monitoring Framework: Operational Guidance for Tracking Progress in Meeting Targets for 2025; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Patsopoulos, N.A.; Evangelou, E.; Ioannidis, J.P. Sensitivity of between-study heterogeneity in meta-analysis: Proposed metrics and empirical evaluation. Int. J. Epidemiol. 2008, 37, 1148–1157. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, S.A.; Smith, C. Economic growth and child undernutrition. Lancet Glob. Health 2016, 4, e901–e902. [Google Scholar] [CrossRef] [Green Version]
- Hackett, M.; Melgar-Quiñonez, H.A.; Âlvarez, M.C. Household food insecurity associated with stunting and underweight among preschool children in Antioquia, Colombia. Revis. Panam. Salud Pública 2009, 25, 506–510. [Google Scholar] [CrossRef] [PubMed]
- Saxena, N.C. Hunger, under-nutrition and food security in India. In Poverty, Chronic Poverty and Poverty Dynamics, 1st ed.; Mehta, A.K., Bhide, S., Kumar, A., Shah, A., Eds.; Springer: New York, NY, USA, 2018; pp. 55–92. [Google Scholar]
- Mutisya, M.; Kandala, N.B.; Ngware, M.W.; Kabiru, C.W. Household food (in) security and nutritional status of urban poor children aged 6 to 23 months in Kenya. BMC Public Health 2015, 15, 1. [Google Scholar] [CrossRef] [PubMed]
- FAO. Regional Overview of Food Insecurity: African Food Security Prospects Brighter Than Ever; FAO: Accra, Ghana, 2015. [Google Scholar]
- Salami, A.; Kamara, A.B.; Brixiova, Z. Smallholder Agriculture in East Africa: Trends, Constraints and Opportunities; African Development Bank: Tunis, Tunisia, 2010. [Google Scholar]
- Gillespie, S.; van den Bold, M. Agriculture, Food Systems, and Nutrition: Meeting the Challenge. Glob. Chall. 2017, 1, 3. [Google Scholar] [CrossRef]
- Hollinger, F.; Staatz, J.M. Agricultural Growth in West Africa: Market and Policy Drivers; FAO/African Development Bank/ECOWAS: Rome, Italy, 2015. [Google Scholar]
- Lopriore, C.; Muehlhoff, E. Food security and nutrition trends in West Africa—Challenges and the way forward. In Proceedings of the 2nd International Workshop on Food-based Approaches for a Healthy Nutrition, Ouagadougou, Burkina-Faso, 23–28 September 2003. [Google Scholar]
- Bender, W.; Smith, M. Population food and nutrition. Popul. Bull. Wash. 1997, 51, 1–48. [Google Scholar]
- Ford, N.D.; Patel, S.A.; Narayan, K.V. Obesity in low-and middle-income countries: Burden, drivers, and emerging challenges. Annu. Rev. Public Health 2017, 38, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Popkin, B.M. The nutrition transition: New trends in the global diet. Nutr. Rev. 1997, 55, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, C.; Thow, A.M. Implications of the Central America-Dominican Republic-free trade agreement for the nutrition transition in Central America. Revis. Panam. Salud Pública 2008, 24, 345–360. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Water, Sanitation and Hygiene Interventions and the Prevention of Diarrhoea. Biological, Behavioural and Contextual Rationale. Available online: https://www.who.int/elena/titles/bbc/wsh_diarrhoea/en/ (accessed on 12 August 2019).
- World Health Organization. Exclusive Breastfeeding to Reduce the Risk of Childhood Overweight and Obesity; Biological, Behavioural and Contextual Rationale; World Health Organization: Geneva, Switzerland, 2014; Available online: http://www.who.int/elena/titles/bbc/breastfeeding_childhood_obesity/en/ (accessed on 12 August 2019).

| Country | DHS | No. of Children (N) | No. of Stunted Children | No. of Wasted Children | No. of Underweight Children | No. of Overweight/Obese Children |
|---|---|---|---|---|---|---|
| Angola | 2015 | 7455 | 2803 | 365 | 1416 | 246 |
| Burkina Faso | 2010 | 6994 | 2448 | 1084 | 1797 | 168 |
| Burundi | 2016 | 6464 | 3620 | 330 | 1894 | 90 |
| Cameroon | 2011 | 5860 | 1934 | 328 | 856 | 363 |
| Chad | 2014 | 10,854 | 4342 | 1411 | 3126 | 271 |
| Comoros | 2012 | 2762 | 829 | 307 | 423 | 257 |
| Congo-Brazzaville | 2011 | 4591 | 1148 | 271 | 533 | 152 |
| Côte d’Ivoire | 2011 | 3581 | 1074 | 269 | 534 | 107 |
| DRC * | 2013 | 9030 | 3883 | 713 | 2041 | 370 |
| Equatorial Guinea | 2011 | 1094 | 284 | 34 | 61 | 106 |
| Eritrea | 2002 | 5466 | 2077 | 689 | 2165 | No data |
| Ethiopia | 2016 | 10,447 | 3970 | 1034 | 2465 | 293 |
| Gabon | 2012 | 3856 | 636 | 127 | 231 | 285 |
| Gambia | 2013 | 3372 | 843 | 388 | 546 | 91 |
| Ghana | 2014 | 2895 | 550 | 136 | 318 | 75 |
| Guinea | 2012 | 3531 | 1095 | 339 | 636 | 127 |
| Kenya | 2014 | 18,986 | 4936 | 759 | 2088 | 778 |
| Lesotho | 2014 | 1869 | 617 | 52 | 193 | 138 |
| Liberia | 2013 | 3520 | 1126 | 211 | 528 | 102 |
| Madagascar | 2008 | 5436 | 2718 | No data | No data | No data |
| Malawi | 2015 | 5752 | 2128 | 155 | 673 | 259 |
| Mali | 2012 | 4857 | 1846 | 617 | 1239 | 112 |
| Mozambique | 2011 | 10,313 | 4435 | 608 | 1537 | 763 |
| Namibia | 2013 | 2287 | 549 | 142 | 306 | 78 |
| Niger | 2012 | 5481 | 2412 | 987 | 1995 | 132 |
| Nigeria | 2013 | 26,190 | 9690 | 4714 | 7517 | 1048 |
| Rwanda | 2014 | 3813 | 1449 | 84 | 355 | 294 |
| São Tomé and Príncipe | 2008 | 1544 | 448 | 162 | 202 | 162 |
| Senegal | 2016 | 5722 | 973 | 412 | 772 | 51 |
| Sierra Leone | 2013 | 5094 | 1931 | 474 | 835 | 382 |
| South Africa | 2016 | 1401 | 384 | 35 | 83 | 186 |
| Swaziland | 2006 | 2940 | 850 | 74 | 159 | 318 |
| Tanzania | 2015 | 9848 | 3388 | 443 | 1349 | 355 |
| Togo | 2013 | 3282 | 903 | 213 | 525 | 62 |
| Uganda | 2016 | 5148 | 1488 | 180 | 541 | 190 |
| Zambia | 2013 | 12,328 | 2120 | 740 | 1825 | 703 |
| Zimbabwe | 2015 | 6352 | 1702 | 203 | 356 | 534 |
| Bolivia | 2008 | 8422 | 2282 | 118 | 362 | 716 |
| Dominican Republic | 2013 | 3619 | 253 | 72 | 138 | 264 |
| Guatemala | 2014 | 12,567 | 5906 | 88 | 1583 | 591 |
| Guyana | 2009 | 1522 | 274 | 81 | 160 | 94 |
| Haiti | 2016 | 6618 | 1456 | 245 | 629 | 225 |
| Honduras | 2011 | 10,167 | 2338 | 41 | 712 | 519 |
| Nicaragua | 2001 | 6277 | 1701 | 151 | 496 | 490 |
| Peru | 2014 | 9540 | 1431 | 57 | 296 | No data |
| Bangladesh | 2014 | 7318 | 2634 | 1046 | 2386 | 102 |
| India | 2015 | 219,796 | 83,522 | 46,157 | 78,467 | 4616 |
| Maldives | 2009 | 2513 | 477 | 266 | 435 | 148 |
| Myanmar | 2015 | 4088 | 1186 | 286 | 773 | 53 |
| Nepal | 2016 | 2422 | 872 | 235 | 654 | 29 |
| Sri Lanka | 2016 | 7865 | 1337 | 1188 | 1612 | 157 |
| Timor-Leste | 2016 | 6798 | 3127 | 1632 | 2746 | 374 |
| Albania | 2008 | 1289 | 245 | 117 | 67 | 280 |
| Armenia | 2015 | 1579 | 142 | 66 | 41 | 215 |
| Azerbaijan | 2006 | 1979 | 495 | 135 | 152 | 255 |
| Kyrgyzstan | 2012 | 4337 | 781 | 117 | 147 | 369 |
| Moldova | 2005 | 1522 | 170 | 102 | 50 | 137 |
| Tajikistan | 2012 | 5080 | 1321 | 503 | 615 | 300 |
| Turkey | 2013 | 3668 | 440 | 26 | 143 | No data |
| Jordan | 2012 | 5851 | 468 | 140 | 176 | 257 |
| Morocco | 2003 | 5682 | 1352 | 636 | 614 | 548 |
| Pakistan | 2012 | 3466 | 1560 | 374 | 1040 | 111 |
| Yemen | 2013 | 13,823 | 6359 | 2253 | 5391 | 276 |
| Cambodia | 2014 | 4893 | 1566 | 470 | 1169 | 98 |
| Samoa | 2014 | 2859 | 143 | 106 | 77 | 154 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akombi, B.J.; Chitekwe, S.; Sahle, B.W.; Renzaho, A.M.N. Estimating the Double Burden of Malnutrition among 595,975 Children in 65 Low- and Middle-Income Countries: A Meta-Analysis of Demographic and Health Surveys. Int. J. Environ. Res. Public Health 2019, 16, 2886. https://doi.org/10.3390/ijerph16162886
Akombi BJ, Chitekwe S, Sahle BW, Renzaho AMN. Estimating the Double Burden of Malnutrition among 595,975 Children in 65 Low- and Middle-Income Countries: A Meta-Analysis of Demographic and Health Surveys. International Journal of Environmental Research and Public Health. 2019; 16(16):2886. https://doi.org/10.3390/ijerph16162886
Chicago/Turabian StyleAkombi, Blessing J., Stanley Chitekwe, Berhe W. Sahle, and Andre M.N. Renzaho. 2019. "Estimating the Double Burden of Malnutrition among 595,975 Children in 65 Low- and Middle-Income Countries: A Meta-Analysis of Demographic and Health Surveys" International Journal of Environmental Research and Public Health 16, no. 16: 2886. https://doi.org/10.3390/ijerph16162886






