A Systematic Review for Vaccine-Preventable Diseases on Ships: Evidence for Cross-Border Transmission and for Pre-Employment Immunization Need
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Question and Objectives
- What is the published evidence of cases and outbreaks of measles, mumps, rubella, varicella, diphtheria, tetanus, pertussis, meningococcal disease, hepatitis A, and hepatitis B that have been reported from on board ships and the methods applied on board for the prevention and control, worldwide, since 1990?
- What is the published evidence of exposure of travelers to measles, mumps, rubella, varicella, diphtheria, tetanus, pertussis, meningococcal disease, hepatitis A, and hepatitis B, based on serological examinations, worldwide, since 1990?
- To undertake descriptive epidemiology (person, place and time characteristics) of cases and outbreaks of VPDs (measles, mumps, rubella, varicella, diphtheria, tetanus, pertussis, meningococcal disease, hepatitis A, and hepatitis B) that have been reported from on board ships since 1990.
- To describe the cause/risk factors identified for introduction and transmission of these VPDs onto ships.
- To describe key methods applied for the prevention and control of these VPDs on ships.
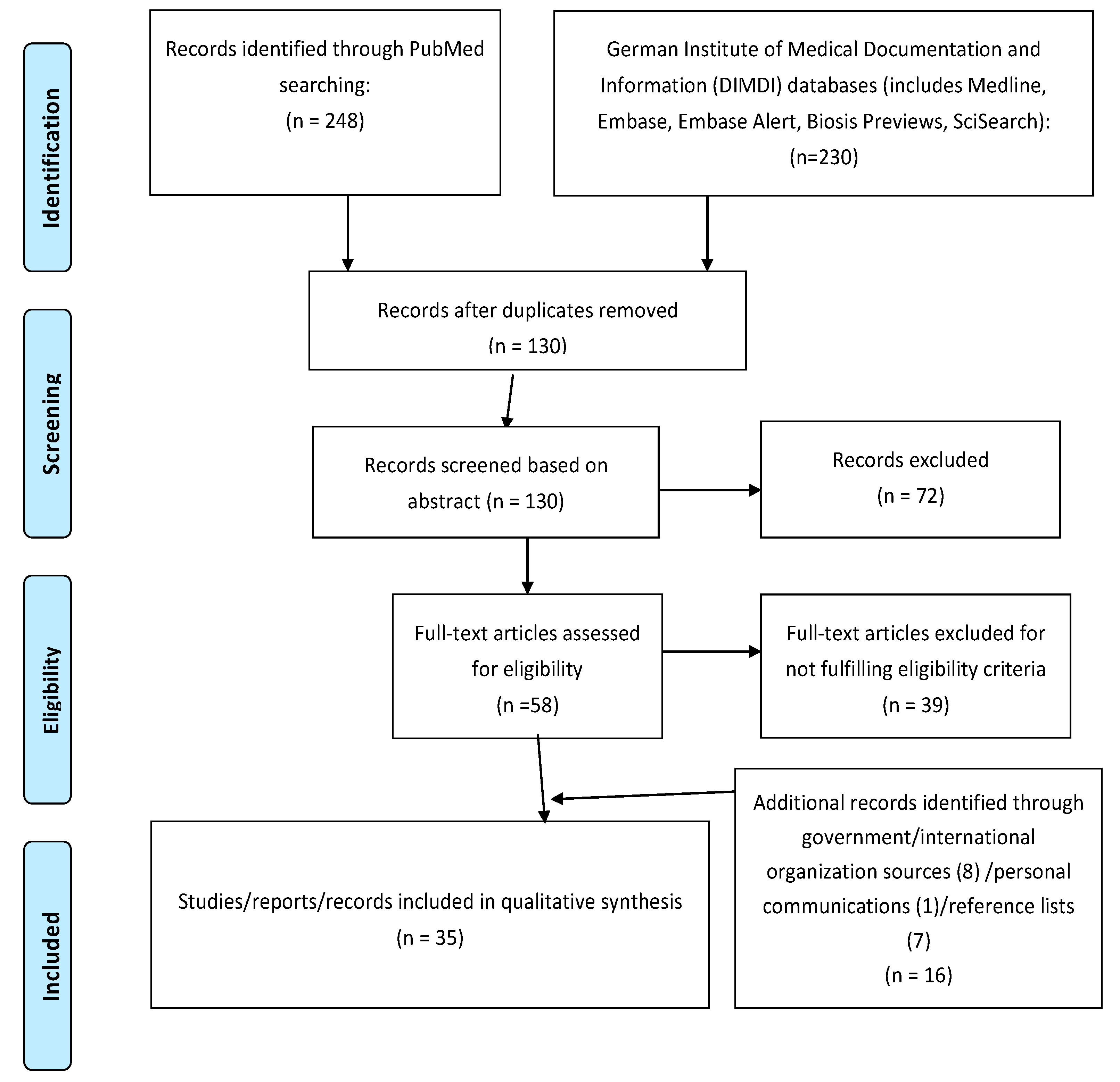
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction and Analysis
2.5. Ethical Approval
3. Results
3.1. Reports Included in the Review
3.2. Single Case Reports
3.3. Outbreaks Reported (Events with More Than One Case Involved)
3.3.1. Characteristics of Outbreak Setting and Affected Population
3.3.2. Secondary Cases on Land
3.3.3. Vaccination History of Travelers
3.3.4. Source of Outbreaks
3.3.5. Response Measures
3.4. Events of VPDs Identified through Record Review Studies
3.5. Evidence of VPDs Based on Serological Tests on Seafarers
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Mitruka, K.; Felsen, C.B.; Tomianovic, D.; Inman, B.; Street, K.; Yambor, P.; Reef, S.E. Measles, rubella, and varicella among the crew of a cruise ship sailing from Florida, United States, 2006. J. Travel Med. 2012, 19, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Public Health Agency Canada. Canada Communicable Disease Report (CCDR); Beaudoin, N., Ed.; Public Health Agency Canada: Ottawa, ON, Canada, 2005; pp. 1–17. [Google Scholar]
- Ziebold, C.; Hassenpflug, B.; Wegner-Bröse, H.; Wegner, K.; Schmitt, H.J. An outbreak of rubella aboard a ship of the German Navy. Infection 2003, 31, 136–142. [Google Scholar] [PubMed]
- EUROSTAT. Maritime Ports Freight and Passenger Statistics. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php/Maritime_ports_freight_and_passenger_statistics#Slight_increase_in_seaborne_goods_and_passengers_in_EU_ports (accessed on 7 May 2019).
- Cruise Line International Association. Clia 2017 Annual Report; CLIA: Washington, DC, USA, 2017. [Google Scholar]
- International Chamber of Shipping. International Chamber of Shipping. Shaping the Future of Shipping 2019. Available online: http://www.ics-shipping.org/shipping-facts/shipping-and-world-trade/global-supply-and-demand-for-seafarers (accessed on 26 July 2019).
- Hadjichristodoulou, C.; Mouchtouri, V.A.; Guglielmetti, P.; Lemos, C.M.; Nichols, G.; Paux, T.; Schlaich, C.; Cornejo, M.D.; Martinez, C.V.; Dionisio, M.; et al. Actions for prevention and control of health threats related to maritime transport in European Union. Travel Med. Infect. Dis. 2013, 11, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Hadjichristodoulou, C.; Mouchtouri, A.V.; Martinez, C.V.; Nichols, G.; Riemer, T.; Rabinina, J.; Swan, C.; Pirnat, N.; Sokolova, O.; Kostara, E.; et al. Surveillance and control of communicable diseases related to passenger ships in Europe. Int. Marit. Health 2011, 62, 138–147. [Google Scholar] [PubMed]
- Instituto de Salud Carlos III and Spain. EU ShipSan Act Joint Action; EU SHIPSAN ACT joint action: Madrid, Spain, 2014. [Google Scholar]
- Mouchtouri, V.A.; Nichols, G.; Rachiotis, G.; Kremastinou, J.; Arvanitoyannis, I.S.; Riemer, T.; Jaremin, B.; Hadjichristodoulou, C. State of the art: Public health and passenger ships. Int. Marit. Health 2010, 61, 49–98. [Google Scholar] [PubMed]
- Stamatakis, C.E.; Rice, M.E.; Washburn, F.M.; Krohn, K.J.; Bannerman, M.; Regan, J.J. Maritime illness and death reporting and public health response, United States, 2010–2014. Travel Med. Infect. Dis. 2017, 19, 16–21. [Google Scholar] [CrossRef]
- Rapid Risk Assessment. Outbreak of Hepatitis A Virus Infection in Travellers Returning from Egypt; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2013. [Google Scholar]
- European Centre for Disease Prevention and Control. Communicable Disease Threats Report, 14–20 July 2019, Week 29; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2019. [Google Scholar]
- US Centers for Disease Control and Prevention. Guidance for Cruise Ships on Varicella (Chickenpox) Management; US Centers for Disease Control and Prevention: Atlanta, GA, USA, 2014.
- World Health Organization. Handbook for Management of Public Health Events on Board Ships; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- EU SHIPSAN ACT joint action. European Manual for Hygiene Standards and Communicable Diseases Surveillance on Passenger Ships; EU SHIPSAN: Larissa, Greece, 2016. [Google Scholar]
- European Council. Decision No 1082/2013/EU of the European Parliament and of the Council of 22 October 2013 on Serious Cross-Border Threats to Health an Repealing Decision No 2119/98/EC. Available online: https://ec.europa.eu/health/sites/health/files/preparedness_response/docs/decision_serious_crossborder_threats_22102013_en.pdf (accessed on 26 July 2019).
- World Health Organization. International Health Regulations, 3rd ed.; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- EU SHIPSAN ACT Joint Action. The Impact on Maritime Transport of Health Threats Due to Biological, Chemical and Radiological Agents, Including Communicable Diseases. Available online: http://www.shipsan.eu (accessed on 26 July 2019).
- Moher, D.; Moher, D.; Liberati, A.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- EU SHIPSAN ACT joint action. EU SHIPSAN ACT Information System (SIS). Available online: https://sis.shipsan.eu (accessed on 29 July 2019).
- Nieto-Vera, J.; Masa-Calles, J.; Dávila, J.; Molina-Font, J.; Jiménez, M.; Gallardo-García, V.; Mayoral-Cortés, J.M. An Outbreak of Measles in Algeciras, Spain, 2008—A Preliminary Report. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=18872 (accessed on 15 May 2008).
- Hannah, C. Lewis, Outbreaks of Measles. personal communication, 2015. [Google Scholar]
- Diphtheria acquired during a cruise in the Baltic Sea. Commun. Dis. Rep. CDR Wkly. 1997, 7, 207.
- Ellis, M.; Luna-Pinto, C.; George, T.; Regan, J.J.; Marin, M.; Lopez, A.; Rivera-Garcia, B.; Tardivel, K. Notes from the Field: Varicella fatality on a cargo vessel—Puerto Rico, 2015. Morb. Mortal. Wkly. Rep. 2017, 66, 410. [Google Scholar] [CrossRef][Green Version]
- Farr, W.; Gonzalez, M.J.; Garbauskas, H.; Zinderman, C.E.; Lamar, J.E. Suspected meningococcal meningitis on an aircraft carrier. Mil. Med. 2004, 169, 684–686. [Google Scholar] [CrossRef]
- Munne, M.S.; Altabert, N.R.; Vladimirsky, S.N.; Arribere, M.G.; Ortali, S.F.; Sijvarger, C.; Otegui-Mares, L.O.; Soto, S.S.; Brajterman, L.S.; González, J.E. Molecular surveillance of hepatitis A virus in Argentina: First subgenotype IB detected in a traveler. Ann. Hepatol. 2014, 13, 404–406. [Google Scholar] [CrossRef]
- Filia, A.; Bella, A.; del Manso, M.; Rota, M.C.; Magurano, F.; Nicoletti, L.; Declich, S. Extensive Nosocomial Transmission of Measles Originating in Cruise Ship Passenger, Sardinia, Italy, 2014. Emerg. Infect. Dis. 2015, 21, 1444–1446. [Google Scholar] [CrossRef] [PubMed]
- Stefanelli, P.; Fazio, C.; Neri, A.; Isola, P.; Sani, S.; Marelli, P.; Martinelli, C.; Mastrantonio, P.; Pompa, M.G. Cluster of Invasive Neisseria Meningitidis Infections on a Cruise Ship, Italy, October 2012. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20336 (accessed on 13 December 2012).
- Bernard, H.; Frank, C. Cluster of Hepatitis A Cases among Travellers Returning from Egypt, Germany, September through November 2008. Available online: https://edoc.rki.de/bitstream/handle/176904/457/20KmhhazbrGaU.pdf?sequence=1 (accessed on 22 January 2009).
- Lanini, S.; Capobianchi, M.R.; Puro, V.; Filia, A.; Del Manso, M.; Kärki, T.; Nicoletti, L.; Magurano, F.; Derrough, T.; Severi, E.; et al. Measles Outbreak on a Cruise Ship in the Western Mediterranean, February 2014, Preliminary Report. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20735 (accessed on 13 March 2014).
- Maloney, S.A.; Cetron, M. Investigation and management of infectious diseases on international conveyances (airplanes and cruise ships). In Textbook of Travel Medicine and Health, 2nd ed.; Dupont, H.L., Steffen, R., Eds.; BC Decker: Hamilton, ON, Canada, 2001. [Google Scholar]
- Cozza, V.; Chironna, M.; Leo, C.; Prato, R. Letter to the Editor: Measles on the Cruise Ship: Links with Virus Spreading into an Emergency Department in Southern Italy. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20800 (accessed on 15 May 2014).
- From the Centers for Disease Control and Prevention. Rubella among crew members of commercial cruise ships—Florida, 1997. JAMA 1998, 279, 348–350. [Google Scholar]
- Kuhlman, J.C. Mumps outbreak aboard the USS Reuben James. Mil. Med. 1994, 159, 255–257. [Google Scholar] [CrossRef] [PubMed]
- Couturier, E.; Roque-Afonso, A.M.; Letort, M.J.; Dussaix, E.; Vaillant, V.; De Valk, H. Cluster of Cases of Hepatitis A with a Travel History to Egypt, September–November 2008, France. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19094 (accessed on 22 January 2009).
- Robesyn, E.; Micalessi, M.I.; Quoilin, S.; Naranjo, M.; Thomas, I. Cluster of Hepatitis A Cases among Travellers Returning from Egypt, Belgium, September through November 2008. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19095 (accessed on 22 January 2009).
- Acevedo, F.; Diskin, A.L.; Dahl, E. Varicella at sea: A two-year study on cruise ships. Int. Marit. Health 2011, 62, 254–261. [Google Scholar] [PubMed]
- Schlaich, C.; Riemer, T.; Lamshöft, M.; Hagelstein, J.-G.; Oldenburg, M. Public health significance of chickenpox on ships—Conclusions drawn from a case series in the port of Hamburg. Int. Marit. Health 2010, 61, 28–31. [Google Scholar] [PubMed]
- Cramer, E.H.; Slaten, D.D.; Guerreiro, A.; Robbins, D.; Ganzon, A. Management and control of varicella on cruise ships: A collaborative approach to promoting public health. J. Travel Med. 2012, 19, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Rice, M.E.; Slaten, D.D.; Guerreiro, A.; Robbins, D.; Ganzon, A. Maritime varicella illness and death reporting, U.S., 2010–2015. Travel Med. Infect. Dis. 2018, 23, 27–33. [Google Scholar] [CrossRef]
- Idnani, N. Varicella among seafarers: A case study on testing and vaccination as a cost-effective method of prevention. Int. Marit. Health 2010, 61, 32–35. [Google Scholar] [PubMed]
- Hansen, H.L.; Andersen, P.L.; Brandt, L.; Broløs, O. Antibodies against hepatitis viruses in merchant seamen. Scand. J. Infect. Dis. 1995, 27, 191–194. [Google Scholar] [CrossRef]
- Hawkins, R.E.; Malone, J.D.; Cloninger, L.A.; Rozmajzl, P.J.; Lewis, D.; Butler, J.; Cross, E.; Gray, S.; Hyams, K.C. Risk of viral hepatitis among military personnel assigned to US Navy ships. J. Infect. Dis. 1992, 165, 716–719. [Google Scholar] [CrossRef] [PubMed]
- Mazokopakis, E.; Vlachonikolis, J.; Philalithis, A.; Lionis, C. Seroprevalence of hepatitis A, B and C markers in Greek warship personnel. Eur. J. Epidemiol. 2000, 16, 1069–1072. [Google Scholar] [CrossRef] [PubMed]
- Regan, J.J.V.; Scott, J.; Brown, C.M. Infectious illnesses on cruise and cargo ships, in Infectious Diseases. A geographical guide. Infect. Dis. 2017, 35–44. [Google Scholar] [CrossRef]
- World Health Organization. International Medical Guide for Ships, 3rd ed.; Including the Ship’s Medicine Chest; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- World Health Organizartion. Handbook Inspection of Ships and Issuance of Ship Sanitation Certificates 2011; World Health Organizartion: Geneva, Switzerland, 2011. [Google Scholar]
- International Labour Organization. Maritime Labour Convention; International Labour Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Morof, D.C. Pregnant Travelers. In CDC Yellow Book 2018 Health Information for International Travel; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018. [Google Scholar]
- World Health Organization. Immunization, Vaccines and Biologicals. New Measles Surveillance Data for 2019; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- European Centre for Disease Prevention and Control, RISK ASSESSMENT. Who Is at Risk For Measles in the EU/EEA? Identifying Susceptible Groups to Close Immunity Gaps towards Measles Elimination. Available online: https://ecdc.europa.eu/sites/portal/files/documents/RRA-Measles-EU-EEA-May-2019.pdf (accessed on 28 July 2019).
- The European Parliament. European Parliament Legislative Resolution of 18 April 2019 on the Proposal for a Regulation of the European Parliament and of the Council Establishing a European Maritime Single Window Environment and Repealing Directive 2010/65/EU (COM(2018)0278-C8-0193/2018-2018/0139(COD)). (Ordinary Legislative Procedure: First Reading). 2019. Available online: http://www.europarl.europa.eu/doceo/document/TA-8-2019-0434_EN.html#title1 (accessed on 29 July 2019).
| Disease | Dates, Number of Affected Voyages (Duration) | Diagnosis/Case Definition | No. Cases (Crew, Pax, Other) | Age, Sex, Nationality of Cases | No. Hospitalizations (HR), No. Deaths | Crew Attack Rate (of Susceptible) | Place of Occurrence/Ship Type | Vaccination/Infection History | Source/Risk Factor | Control Measures Described * | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rubella | 2 May–28 June 1996, 1 (2 months) | Rubella IgM+ or IgG+ plus clinical exanthema | 20 (20, 0, 0) | 18–33 years (mean 22.6); all male, German | 0 (0%), 0 | 6% crew (57%) | Unkn. ‡. (ashore)/Military (German Navy ship) | A total of 9% (n = 27) had documentation of vaccination status, 81% (n = 242) had not been vaccinated or did not know status, 36% (n = 98) of crew indicated they had rubella in the past—of which three became cases; Susceptibility rate: 12% (35/292) including infected | Crew; Hypothesized source: off ship pre-employment/Highest risk of infection: sleeping aboard ratings deck | A, C, E | [3] |
| April–June 1997, multiple (3 months) | Rash illness | 7 (7, 0, 0) | Unkn., unkn. 95% not US-born | 0 (0%), 0 | 0.8% crew (unkn) | Florida (USA) to Bahamas/Passenger (cruise) | Substantial proportion (96%, n = 865) of crew had no documentation of rubella vaccination or immunity | Unkn. | B, I | [34] | |
| 30 May–2 August 1997, multiple (2 months) | Rubella IgM+ or clinical Rubella plus epi-link to confirmed case | 16 (16, 0, 0) | Unkn., unkn. 85% not US born from 50 countries | 0 (0%), 0 | 4.2% crew (64%) | Florida (USA) to Bahamas/Passenger (cruise) | 75% of crew had negative or unknown vaccination history, Susceptibility rate: 11% (41//366) including infected | Unkn. | B, E, F, G, I | [34] | |
| Measles | 2 February–18 July 2008, N/A (6 months) | Confirmed or epi-linked clinical measles | 155 (2, 1, 152) | Age range: 5 months-41 years (38% 20–29 years: 19% <2 years); 54% male, unkn. | 13 (8,4%),0 | N/A | Algeciras (Spain)—Tanger (Morocco)/Passenger (ferry) and Land (Algeciras and surrounds) | 72.1% of cases not previously vaccinated | Index cases were 2 crew and 1 passenger | A, F, G, N (vaccination and Ig to susceptible contacts) | [22] |
| 19–26 Aug 2011, Various (8 days) | Confirmed measles | 5 (5, 0, 0) | Unkn., 4 male, 1 female, Philippines: 3, Honduras: 1, Italy: 1 | 0 (0%), 0 | 0.5% (unkn.) | Spain, Malta, Italy/Passenger | Unkn. | Unkn. | A, B, C, D, E, F, G, H, I, J | [21] | |
| 8 February–July 2014, N/A (6 months) | Epi-linked and confirmed | 80 (0, 1, 79) | Median age 26 years (range: 8 months–55 years); 50 (62.5%) female, N/A | 35/78 (44.9%), 0 | Unkn. | Sardinia, Italy/Land | 74/76 cases (97.4%) unvaccinated: 2 (2.6%) with one dose of measles vaccine | Cruise ship passenger | H, G, N (all susceptible staff invited for vaccination) | [28] | |
| 20 February–10 March 2014, 1 (7 days) | Clinical, epi- linked and confirmed | 29 (23, 6, 0) | 1–42 years (median 26); 21/27 (78%) male, Asia (71%), Europe (21%), S. America and Caribbean (7%), Africa (0.5%) Median age 19 years (range: 0–39 years); 17 (53%) female, Italy: 6, India: 5, Philippines: 3, Honduras: 2, Austria: 1, Brazil: 1, Indonesia: 1 | 10/27 (37%), 0 | 2.4% (unkn.) | Mediterranean Sea (Italy, France, Spain)/Passenger (cruise) | Vaccination status of 24 cases: unkn. (n = 12), unvaccinated (n = 9), vaccinated with one to two doses (n = 2, n = 1). Of crew, 142 recalled vaccination and 108 history of measles = 150/968 | Index case: crew member(s): infected during cruise, possibly at one of stops | A, B, E, F, G, H, I, J, K, O | [3,31] | |
| 27 February–May 2014, N/A (3 months) | Clinical, epi- linked and confirmed | 32 (0, 1, 31) | Unkn. | Unkn. | Unkn. | Brindisi province, Puglia Region, Italy/Land | Unknown; 1/32 cases vaccinated with one dose of MMR | Cruise ship passenger | H, N (MMR vaccination for 2 cases on land as PEP and of close contacts) | [33] | |
| Varicella | 1998, unkn. (unkn.) | Clinical varicella case | 3 (3, 0, 0) | Unkn., Most foreign-borne, many from tropical climates | Unkn. | <1% (unkn.) | New York Harbor/Passenger (cruise) | Susceptibility rate including infected 13%. | Unkn. | A, C, I | [32] |
| 28 January–15 April 2006 Multiple (7 days), (11 weeks) | Rash illness | 16 (16, 0, 0) | Index cases 23 and 35 years, unkn., Ukraine and Philippines. Secondary cases: unkn., unkn., majority from tropical countries. | 0 (0%), 0 | 1.3% (unkn.) | Florida (US) to Caribbean./Passenger (cruise) | Three crew members (<1%) had proof of immunity (vaccine record) to measles and rubella | All index cases were crew members; close crew interactions outside of work as risk factor | A, B, E, F, G, H, I | [1] | |
| February–November 2008 5 ships (unkn.), (10 months) | Clinical varicella case | 28 (28, 0, 0) | Unkn., 70% crew from subtropical/tropical countries | 0 (0%), 0 | Unkn. | Mediterranean Sea/Passenger | Unkn. | Unkn. | I | [23] | |
| 20 February–30 March 2012, 1 (5 weeks) | Clinical varicella case | 3 (2, 1, 0) | 4 years, male, unkn. | 0 (0%), 0 | <1% (unkn.) | UK, Spain, Portugal/Passenger | Unkn. | Unkn. | A, B, C, D, E, G, I | [21] | |
| 29 September–2 October 2014, 1 (4 days) | Clinical varicella case | 1 (1, 0, 0) | 27 years, male, unkn. | 0 (0%), 0 | Unkn. | Malta, Spain/Passenger | Unkn. | Unkn. | A, B, C, D, E, G, I | [21] | |
| 16 January–20 February 2015 Various (5 weeks) | Clinical varicella case | 5 (5, 0, 0) | 34 years, male, unkn., Indonesia | 0 (0%), 0 | Unkn. | Spain, Italy/Passenger | Unkn. | Unkn. | A, B, C, D, E, G, I | [21] | |
| 26–30 December 2015, N/A (1 week) | Varicella pneumonia | 1 (1, 0, 0) | 50 years, male, Indian | 1/1 (100%), 1 (cause of death varicella pneumonia) | 1/24 (unkn.) | Puerto Rico/Cargo | Unkn. | Unkn. | A, B, E, I | [25] | |
| 12–21 September 2016 | 5 (5, 0, 0) | Unkn. | 0 (0%), 0 | Unkn. | Belgium/Cargo ship | Unkn. | New crew members from the Philippines arrived (22/08/2016) prior to the outbreak or by contacting people in the port | A, B, C, E, I | [21] | ||
| February 2018, 1 | Clinically diagnosed varicella | 1 (1, 0, 0) | Unkn., male, Philippines | 0 (0%), 0 | Unkn. | Spain/Container ship | Unkn. | Unkn. | A, B, I, E | [21] | |
| Hepatitis A | 1 September–30 November/2008, 3 (3 months) | Clinically compatible case with IgM anti-HAV, disease onset 1 Sept–30 Nov and travel history to Egypt 2–6 weeks prior to symptom onset | 10 (0, 10, 0) | Median 41 years (range 23–59); male to female ratio 3:7, N/A | 1 (10%), 0 | Unkn. | Nile river, Belgium/Passenger (river cruise | No case vaccinated against hepatitis A | Continuing common source, most likely linked to river cruise | B | [37] |
| September–November 2008, 6 (5–14 days), (10 weeks) | Hepatitis A cases (symptoms + lab confirmation of acute infection) with onset from 1 Sept 2008 and travel to Egypt 15–50 days prior to symptom onset | 34 (0, 34, 0) | Mean age 40.1 years (range 11–69); 59% female, N/A | 20 (59%), 0 | Unkn. | Nile river, Germany/Passenger (river cruise | No case vaccinated against hepatitis A | Continuing common source, most likely linked to river cruise | B | [30] | |
| 13 September–28 October 2009, 5 (9 weeks) | Person with IgM anti-HAV who had stayed in Egypt 2–6 weeks prior to symptom onset | 26 (0, 26, 0) | Mean age 32.8 years (range 10–65); 50% female, N/A | 17 (65%), 0 | Unkn. | Nile river, France/Passenger (river cruise | No case vaccinated against hepatitis A | Continuing common source, most likely linked to river cruise | B | [36] | |
| January 2011, 1 (unkn.) | Subgenotype IB imported case | 1 (1, 0, 0) | 28 years, male, Polish | 0, 0 | Unkn. | Argentina (USA–South American Pacific–Atlantic Coast)/Passenger (river cruise | Self-report of one dose hepatitis A vaccine in previous year | Crew index case; Possible risk factor: consumption of shellfish on land in Mexico | O | [27] | |
| Mumps | 15 June–13 August 1992, 1 (unkn.) (2 months) | Clinical mumps | 9 (9, 0, 0) | Mean 24 years (Range: 18–35); unkn., unkn. | 2 (22%), 0 | 4% (unkn.) | Western Pacific, route: Japan to Hawaii (US)/Military (“US Reuben James” Navy ship) | Three cases had mumps or MMR vaccine documented | Unkn. | O | [35] |
| Diphtheria | 1997, 1 (12 days) | Confirmed Corynebacterium diphtheriae | 1 (0, 1, 0) | 72 years, female, unkn. | 1 (100%), 0 | N/A | Baltic sea/Passenger (cruise) | Unkn. | Travelling in former USSR/Baltic | C, N (Diptheria antitoxin and antibiotics to case and close family, contacts received antibiotic prophylaxis and low dose diphtheria vaccine boosters) | [24] |
| Meningitis | May 2003, 1 (unkn.) | Clinical meningococcal meningitis | 1 (1, 0, 0) | 24 years, male, unkn. | 0, 0 | Unkn. | Mid Atlantic ocean/Military (aircraft carrier) | Patient had received meningococcal vaccine three years previously. | Unkn. | A, C, H, N (Chemoprophylaxis to close contacts from the ship) | [26] |
| October 2012, 1 (unkn.), (<1 month) | Confirmed Neisseria meningitides | 4 (4, 0, 0) | Unkn., unkn., originated from three different continents | 4 (100%), 1 (25%) | Unkn. | Italian coast/Passenger (cruise) | Unkn. | All cases worked in ship kitchen | B, N (Chemoprophylaxis to all passengers and crew on ship) | [29] | |
| October 2017, 1 | Clinical meningitis | 1 (1, 0, 0) | Unkn., female, unkn. | 1, unkn. | Unkn. | Greece/Passenger (cruise) | Unkn. | Unkn. | A, B, D, I, O | [21] |
| Disease | Dates (Number of Affected Voyages, Duration) | Diagnosis/Case Definition | No. Cases (Crew, Passenger, Other) | Age (Years), Sex, Nationality of Cases | Population at Risk/Crew Attack Rate (of Susceptible) | Place of Occurrence/Ship Type | Control Measures Described * | Reference |
|---|---|---|---|---|---|---|---|---|
| Varicella | 2005–2009 (unkn., 5 years) | Clinical varicella case | 357 (278, 0, 79) | Crew: Median age 29 (range 20–66), 80% male Three-quarters of crew cases were from Caribbean countries, Indonesia, the Philippines, or India Most cases in spring and winter | 2305 maritime illness reports | Sailing in US waters/passenger | A, B, C, E, F, G, H, I, J | [40] |
| November 2007–April 2008 (4 ships, 6 months) | Clinical varicella case | 5 (5, 0, 0) | 26–42 years, male Majority from SE Asia and Eastern European countries. Crew cases: Indonesia (2), the Philippines (1), Sri Lanka (2) Index: child passenger on cruise (1) and crew coming from home country during incubation period (3) | 13, 377, 28, and 882 crew, respectively | Baltic sea/Europe/Med/USA and Caribbean/passenger (2) cargo (1) work (feeder) ship (1) | A, B, C, E, F, G, H, I, J (instructed but unclear what was carried out) | [39] | |
| 2009–2010, 34 ships (2–25 days, 2 years) | Clinical varicella case (probable case) | 187 (151, 36, 0) | Unkn. >130 countries. 26 countries for crew cases with 58% from 5 sub-tropical or tropical countries (the Philippines, Indonesia, India, Jamaica, St. Vincent and the Grenadines) | 694–6300 passengers per ship; 400–2160 crew per ship. Crew attack rate (of susceptible) For crew clusters reported: (i) 29/860 (3.4%), (ii) 10/2400 (0.4%) | World-wide/passenger | A, B, C, E, F, G, H, I, J | [38] | |
| January 2010–December 2015, 99 outbreaks | Diagnosis of authority’s medical officer | 967 (823 including 758 cruise ship crew, 144, 0) | Crew: 20–49: 394/399, 50+: 5/399, Pax: <1: 3/99, 1–9: 46/99, 10–19: 18/99, 20–49: 24/99 50+: 8/99 Male 395/479 crew 60/106 pax Female 84/479 crew 46/106 pax Indonesia (21.7%, 80/369), Philippines (17.6%, 65/369), or India (17.3%, 64/369) | Unknown | USA/63 cargo ships, 900 cruise ships | A, B, C, H, I, J, O | [41] | |
| Herpes zoster | January 2010–December 2015 | Diagnosis of authority’s medical officer | 13 (9 including 7 cruise ship crew, 4, 0) | Unkn. | Unkn. | USA/2 cargo ships, 11 cruise ships | Unkn. | [41] |
| Mumps | January 2010–December 2014 | Presumptive or final diagnoses based on the information available from healthcare facilities, health departments, medical examiners, or laboratories, when available, and review by a quarantine medical officer | 35 (13, 22, 0) | Unkn. | Unkn. | Unkn. | Unkn. | [11] |
| Meningitis/meningococcal disease | January 2010–December 2014 | Presumptive or final diagnoses based on the information available from healthcare facilities, health departments, medical examiners, or laboratories, when available, and review by a quarantine medical officer | 25 (9, 16, 0) | Unkn. | Unkn. | Unkn. | Unkn. | [11] |
| Hepatitis A | January 2010–December 2014 | Presumptive or final diagnoses based on the information available from healthcare facilities, health departments, medical examiners, or laboratories, when available, and review by a quarantine medical officer | 22 (19, 3, 0) | Unkn. | Unkn. | Unkn. | Unkn. | [11] |
| Measles | January 2010–December 2014 | Any probable or confirmed measles case determined to be contagious during travel. Presumptive or final diagnoses based on the information available from healthcare facilities, health departments, medical examiners, or laboratories, when available, and review by a quarantine medical officer | 21 (10, 11) | Unkn. | Unkn. | Unkn. | Unkn. | [11] |
| Rubella | January 2010–December 2014 | Presumptive or final diagnoses based on the information available from healthcare facilities, health departments, medical examiners, or laboratories, when available, and review by a quarantine medical officer | 10 (4, 6) | Unkn. | Unkn. | Unkn. | Unkn. | [11] |
| Pertussis | January 2010–December 2014 | Presumptive or final diagnoses based on the information available from healthcare facilities, health departments, medical examiners, or laboratories, when available, and review by a quarantine medical officer | 9 (0, 9) | Unkn. | Unkn. | Unkn. | Unkn. | [11] |
| Disease, Study Duration [Reference] | Study Date (Duration) | Study Sample | Serological Markers * | No. Study Subjects (Age, Sex, Nationality | Seropositivity | Seropositivity By Age | Seropositivity by Nationality | Susceptibility | Vaccination/Infection History | Risk Factors |
|---|---|---|---|---|---|---|---|---|---|---|
| Hepatitis Study/1989–1991 [44] | 1989–1991 (3 years) | US military personnel scheduled for deployment on 11 US Navy ships | Anti-HAV+, Anti-HBc+, Anti-HBsAg+ Anti-HDV, Anti-HCV+ | 2072 (male, mean 24 years; 72% white) | Anti-HAV+ 210 (10.1%); Anti-HBc+ 76 (3.7 %); Anti-HCV+ 9 (0.4%) | Increasing with age: HAV+ 7.8% in 18–24 years; 28.7% in >34 years Anti-HBc+: 2.2% in 18–24 yo; 7.2% in 25–34 years; 8.3% in >34 years | For country of birth: Anti-HAV+ 8% for USA and 39.3% for foreign; HBV+ for 3.2% USA, 10.7% for foreign | HAV: 90% | 28 subjects reported a history of acute hepatitis (50% were anti HAV+ compared to 9.6% without a history) | Anti-HAV positivity associated with age, non-white racial/ethnic group, born outside US and prior Caribbean deployment for <1 year. Anti-HBV with black and Philippino race, foreign birth, a history of STD and South Pacific/Indian Ocean deployment for <12 months, and S Pacific or Med duty for >1 year |
| Hepatitis Study/1993 [43] | April–December 1993 (9 months) | Seamen attending five clinics performing mandatory health examinations of seamen in Denmark | Anti-HAV+, Anti-HBc+, Anti-HBsAg+, Anti-HCV+ | 515 (86% male; 94% Scandinavian) | Anti-HAV+ 79 (15.3%); Anti-HBc+ 47 (9.1%); Anti-HCV+ 6 (1.2%) | Increasing with age: HAV+ 0.3% in <40; 71% in 60–69 years. HBV+: 2.7% in <40; 35.7% in >60 | For origin: Anti-HAV+ 12.8% for Scandinavian and 52.4% for foreign; HBV+ 7.9% for Scandinavian, 28.5% for foreign | HAV: 85% | 1 HAV+ case previously had HAV vaccination | Anti-HAV and HBV positivity associated with age. HAV seroprevalence highest among those who sailed in international trade (outside USA and Europe) |
| Hepatitis Study/1998 [45] | February–July 1998 (6 months) | Personnel from a Greek warship | Anti-HAV+, Anti-HBsAg+ Anti-HBc+, Anti-HBs+, Anti-HCV+ | 263; (male, mean age 24.4 years) | Anti-HAV+ 0 (0%); Anti-HBsAg+ 3 (1.1 %); Anti-HBc+, 4 (1.5%) Anti-HBs+ 45 (17.1%); Anti-HCV+ 1 (0.4%) | Unkn. | Unkn. | HAV: 100% | 23 subjects reported vaccination against Hepatitis B (three doses by 14 subjects) | Unkn. |
| Varicella Study/2008 [42] | 1–23 December 2008 (3 weeks) | Cruise ship crew members undergoing pre-employment medical exam in Mumbai and Goa | VZV IgM+ and IgG + | 121 (male, 21–42 years, 100% Indian) | 100 (82.7%) IgG+ 0 (0%) IgM+ | Unkn. | Unkn. | 16.5% susceptibility | 60% IgG pos. crew could remember disease or vaccine history | Unkn. |
| Disease | No. Clusters/Outbreaks > 1 Cases | No. Crew Cases | No. Pax Cases | Total Crew, Pax/Total Cases n = 1795 (%) | No. Other Cases | Male/Female | Origin of Cases | Ship Type | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Out. Rep. ‡ | Rev.Rec. ∞ | Out. Rep. | Rev. Rec | |||||||
| Measles | 3 | 30 | 10 | 7 | 11 | 40, 18/58 (3, 2) | 262 * | 25/7 | Asia, Europe, S. America, Caribbean, Africa, Italy, India, Philippines, Honduras, Austria, Brazil, Indonesia, unkn. | 1 ferry, 2 cruise |
| Rubella | 3 | 43 | 4 | - | 6 | 47, 6/53 (3, 0) | 0 | 20/- | German, unkn. | 2 cruise, 1 military |
| Hepatitis A | 3 | - | 19 | 70 | 3 | 19, 73/92 (5, 1) | 0 | 31/40 | Polish, unkn. | 4 river cruise ships |
| Meningococcal meningitis | 1 | 4 | 9 | - | 16 | 13, 16/ 29 (1, 6) | 0 | 1/1 | unkn. | 2 cruise, 1 military |
| Mumps | 1 | 9 | 13 | - | 22 | 22, 22/44 (2, 5) | 0 | -/- | unkn. | 1 military |
| Pertussis | unkn √. | - | - | - | 9 | 0, 9/9 (0, 5) | 0 | -/- | unkn. | - |
| Herpes zoster | unkn. | - | 9 | - | 4 | 9, 4/13 (0, 7) | 0 | -/- | unkn. | 11 cruise, 2 cargo |
| Varicella | 104 | 59 | 1257 | 1 | 180 | 1316, 181/1497 (83, 4) | 79 † | 687/130 | Indonesia, India, Philippines, SE Asia, Eastern European countries, Sri Lanka, Caribbean countries, unkn. | 909 cruise, 69 cargo |
| Total | 115 | 145 | 1321 | 78 | 251 | 223, 1572/1795 | 341 | 764/179 | 1006 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mouchtouri, V.A.; Lewis, H.C.; Hadjichristodoulou, C.; the EU SHIPSAN ACT Joint Action Partnership. A Systematic Review for Vaccine-Preventable Diseases on Ships: Evidence for Cross-Border Transmission and for Pre-Employment Immunization Need. Int. J. Environ. Res. Public Health 2019, 16, 2713. https://doi.org/10.3390/ijerph16152713
Mouchtouri VA, Lewis HC, Hadjichristodoulou C, the EU SHIPSAN ACT Joint Action Partnership. A Systematic Review for Vaccine-Preventable Diseases on Ships: Evidence for Cross-Border Transmission and for Pre-Employment Immunization Need. International Journal of Environmental Research and Public Health. 2019; 16(15):2713. https://doi.org/10.3390/ijerph16152713
Chicago/Turabian StyleMouchtouri, Varvara A., Hannah C. Lewis, Christos Hadjichristodoulou, and the EU SHIPSAN ACT Joint Action Partnership. 2019. "A Systematic Review for Vaccine-Preventable Diseases on Ships: Evidence for Cross-Border Transmission and for Pre-Employment Immunization Need" International Journal of Environmental Research and Public Health 16, no. 15: 2713. https://doi.org/10.3390/ijerph16152713
APA StyleMouchtouri, V. A., Lewis, H. C., Hadjichristodoulou, C., & the EU SHIPSAN ACT Joint Action Partnership. (2019). A Systematic Review for Vaccine-Preventable Diseases on Ships: Evidence for Cross-Border Transmission and for Pre-Employment Immunization Need. International Journal of Environmental Research and Public Health, 16(15), 2713. https://doi.org/10.3390/ijerph16152713




