Living in the Restoration Public Housing after the Great East Japan Earthquake Correlates with Lower Subjective Well-Being of Older Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Participants
2.4. Dependent Variable
2.5. Key Independent Variable: Social Capital
2.6. Covariates
2.7. Statistical Methods
2.8. Ethical Issues
3. Results
3.1. Characteristics of Participants
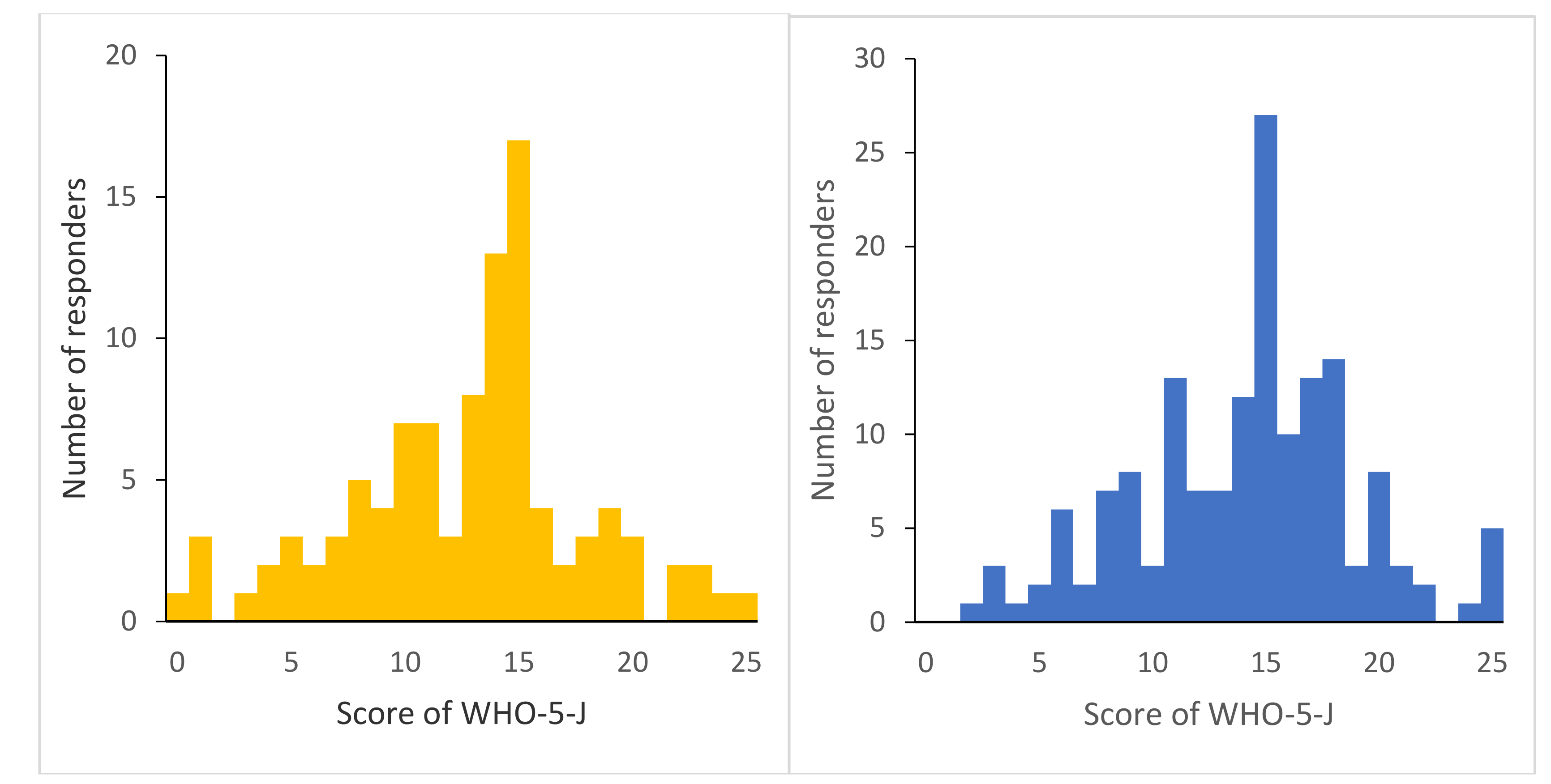
3.2. Status of SWB, Social Capital, and Health Indicators in Subjects between Groups among Groups
3.3. Association between SWB and Social Capital
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wellbeing and Health. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/225525/DH_wellbeing_health.PDF (accessed on 22 June 2019).
- Diener, E. Subjective well-being: The science of happiness and a proposal for a national index. Am. Psychol. 2000, 55, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Ryff, C.D.; Keyes, C.L. The structure of psychological well-being revisited. J. Pers. Soc. Psychol. 1995, 69, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Tilvis, R.S.; Laitala, V.; Routasalo, P.; Strandberg, T.E.; Pitkala, K.H. Positive life orientation predicts good survival prognosis in old age. Arch. Gerontol. Geriatr. 2012, 55, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Howell, R.T.; Kern, M.L.; Lyubomirsky, S. Health benefits: Meta-analytically determining the impact of well-being on objective health outcomes. Health Psychol. Rev. 2017, 1, 83–136. [Google Scholar] [CrossRef]
- Higashi Nihon Daishinsai ni Tsuite Report on the Great East Japan Earthquake. Available online: https://www.fdma.go.jp/disaster/higashinihon/items/159.pdf (accessed on 22 June 2019).
- Tsubokura, M.; Hara, K.; Matsumura, T.; Sugimoto, A.; Nomura, S.; Hinata, M.; Kami, M. The immediate physical and mental health crisis in residents proximal to the evacuation zone after Japan’s nuclear disaster: An observational pilot study. Disaster Med. Public Health Prep. 2014, 8, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, A.; Tanigawa, K.; Ohtsuru, A.; Yabe, H.; Maeda, M.; Shigemura, J.; Chhem, R.K. Health effects of radiation and other health problems in the aftermath of nuclear accidents, with an emphasis on Fukushima. Lancet 2015, 386, 479–488. [Google Scholar] [CrossRef]
- Murakami, M.; Harada, S.; Oki, T. Decontamination reduces radiation anxiety and improves subjective well-being after the Fukushima accident. Tohoku J. Exp. Med. 2017, 241, 103–116. [Google Scholar] [CrossRef]
- Hinan kuiki no Jyoukyou Hisaisya Shien Situation of Evacuation Area, Support for Victims. Available online: http://www.pref.fukushima.lg.jp/site/portal/list271.html (accessed on 22 June 2019).
- Kawasaki, K.; Suzuki, R.; Tsuzukihashi, K.; Fukaya, C.; Yabuki, R.; Yabe, M. Current status and consciousness of residents of public housing for nuclear disaster evacuees in Fukushima: A study of public housing for nuclear disaster evacuees in Fukushima (Part2). Rep. City Plan. Inst. Jpn. 2017, 15, 252–257. [Google Scholar]
- Moriyama, N.; Urabe, Y.; Onoda, S.; Maeda, N.; Oikawa, T. Effect of residence in temporary housing after the Great East Japan Earthquake on the physical activity and quality of life of older survivors. Disaster Med. Public Health Prep. 2017, 11, 701–710. [Google Scholar] [CrossRef]
- Kunii, Y.; Suzuki, Y.; Shiga, T.; Yabe, H.; Yasumura, S.; Maeda, M.; Abe, M. Severe psychological distress of evacuees in evacuation zone caused by the Fukushima Daiichi Nuclear Power Plant accident: The Fukushima Health Management Survey. PLoS ONE 2016, 11, e0158821. [Google Scholar] [CrossRef]
- Kawachi, I.; Subramanian, S.V.; Kim, D. Social capital and health: A decade of progress and beyond. In Social Capital and Health; Kawachi, I., Subramanian, S.V., Kim, D., Eds.; Springer: London, UK, 2008; pp. 1–28. [Google Scholar]
- Yamaguchi, M.; Inoue, Y.; Shinozaki, T.; Saito, M.; Takagi, D.; Kondo, K.; Kondo, N. Community social capital and depressive symptoms among older people in Japan: A multilevel longitudinal study. J. Epidemiol. 2018, JE20180078. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, A.; Ohira, T.; Maeda, M.; Yasumura, S.; Tanigawa, K. Emergency responses and health consequences after the Fukushima accident: Evacuation and relocation. Clin. Oncol. 2016, 28, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Jiji.com. Fukkou Juutaku, Nayamu Koritsu Restoration Public Housing, Worrisome Problem of Isolation. Available online: https://www.jiji.com/jc/article?k=2019030700758&g=soc (accessed on 22 June 2019).
- Hikichi, H.; Sawada, Y.; Tsuboya, T.; Aida, J.; Kondo, K.; Koyama, S.; Kawachi, I. Residential relocation and change in social capital: A natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Sci. Adv. 2017, 3, e1700426. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef]
- Heisei 27 Nendo Kokuzei Chousa Private Households, by Kind of Residence and Tenure of Dwelling (3 Groups), Type of Building (6 Groups) and Kind of City Planning Area (47 Groups) Japan, Prefectures, 21 Major Cities, ku of 21 Major Cities, Prefectural Capital Cities and shi with Population of 200,000 or More. Available online: https://www.e-stat.go.jp/stat-search/file-download?statInfId=000031473255&fileKind=1 (accessed on 22 June 2019).
- Van Voorhis, C.R.; Morgan, B.L. Understanding power and rules of thumb for determining sample size. Tutor. Quant. Methods Psychol. 2007, 3, 43–50. [Google Scholar] [CrossRef]
- Awata, S.; Bech, P.; Yoshida, S.; Hirai, M.; Suzuki, S.; Yamashita, M.; Oka, Y. Reliability and validity of the Japanese version of the World Health Organization-Five Well-Being Index in the context of detecting depression in diabetic patients. Psychiatry Clin. Neurosci. 2007, 61, 112–119. [Google Scholar] [CrossRef]
- Harpham, T. The measurement of community social capital through surveys. In Social Capital and Health; Kawachi, I., Subramanian, S.V., Kim, D., Eds.; Springer: New York, NY, USA, 2008; pp. 51–62. [Google Scholar]
- Ichida, Y.; Kondo, K.; Hirai, H.; Hanibuchi, T.; Yoshikawa, G.; Murata, C. Social capital, income inequality and selfrated health in Chita peninsula, Japan: A multilevel analysis of older people in 25 communities. Soc. Sci. Med. 2009, 69, 489–499. [Google Scholar] [CrossRef]
- Kobayashi, T.; Suzuki, E.; Noguchi, M.; Kawachi, I.; Takao, S. Community-level social capital and psychological distress among the elderly in Japan: A population-based study. PLoS ONE 2015, 10, e0142629. [Google Scholar]
- Yasunaga, A.; Park, H.; Watanabe, E.; Togo, F.; Park, S.; Shephard, R.J.; Aoyagi, Y. Development and evaluation of the physical activity questionnaire for elderly Japanese: The Nakanojo study. J. Aging Phys. Act. 2007, 15, 398–411. [Google Scholar] [CrossRef]
- Kenkou Zukuri no Tameno Shintai Katsudou Kijun Exercise and Physical Activity Guide for Health Promotion 2013. Available online: https://www.mhlw.go.jp/stf/houdou/2r9852000002xple-att/2r9852000002xpqt.pdf (accessed on 22 June 2019).
- Harpham, T.; Grant, E.; Thomas, E. Measuring social capital within health surveys: Key issues. Health Policy Plan. 2002, 17, 106–111. [Google Scholar] [CrossRef]
- Koyano, W.; Shibata, H.; Nakazato, K.; Haga, H.; Suyama, Y. Measurement of competence: Reliability and validity of the TMIG Index of Competence. Arch. Gerontol. Geriatr. 1991, 13, 103–116. [Google Scholar] [CrossRef]
- Fujiwara, T.; Kondo, K.; Shirai, K.; Suzuki, K.; Kawachi, I. Associations of childhood socioeconomic status and adulthood height with functional limitations among Japanese older people: Results from the JAGES 2010 Project. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 852–859. [Google Scholar] [CrossRef]
- Iwasa, H.; Inagaki, H.; Yoshida, Y.; Masui, Y.; Suzuki, T.; Yoshida, H.; Awata, S. Normative data for the Japanese version of the World Health Organization-Five Well-Being Index (WHO-5-J) among Japanese community dwelling older adults. Jpn. J. Gerontol. 2014, 36, 330–339. (In Japanese) [Google Scholar]
- Yasumura, S.; Hosoya, M.; Yamashita, S.; Kamiya, K.; Abe, M.; Akashi, M.; Ozasa, K. Study protocol for the Fukushima Health Management Survey. J. Epidemiol. 2012, 22, 375–383. [Google Scholar] [CrossRef]
- Office of International Cooperation, Radiation Medical Science Center for the Fukushima Health Management Survey Mental Health and Lifestyle Survey. Available online: http://fmu-global.jp/download/mental-health-and-lifestyle-survey-12/?wpdmdl=2699 (accessed on 19 July 2019).
- Maeda, M.; Oe, M. Mental health consequences and social issues after the Fukushima disaster. Asia Pac. J. Public Health 2017, 29, 36S–46S. [Google Scholar] [CrossRef]
- Ishii, T.; Ochi, S.; Tsubokura, M.; Kato, S.; Tetsuda, T.; Kato, J.; Nishikawa, Y.; Tachiya, H. Physical performance deterioration of temporary housing residents after the Great East Japan Earthquake. Prev. Med. Rep. 2015, 2, 916–919. [Google Scholar] [CrossRef]
- Ohira, T.; Hosoya, M.; Yasumura, S.; Satoh, H.; Suzuki, H.; Sakai, A.; Abe, M. Evacuation and risk of hypertension after the Great East Japan Earthquake: The Fukushima Health Management Survey. Hypertension 2016, 68, 558–564. [Google Scholar] [CrossRef]
- Hashimoto, S.; Nagai, M.; Fukuma, S.; Ohira, T.; Hosoya, M.; Yasumura, S.; Abe, M. Influence of Post-disaster Evacuation on Incidence of Metabolic Syndrome. J. Atheroscler. Thromb. 2017, 24, 327–337. [Google Scholar] [CrossRef]
- Satoh, H.; Ohira, T.; Hosoya, M.; Sakai, A.; Watanabe, T.; Ohtsuru, A.; Abe, M. Evacuation after the Fukushima Daiichi nuclear power plant accident is a cause of diabetes: Results from the Fukushima Health Management Survey. J. Diabetes Res. 2015, 2015, 1–9. [Google Scholar] [CrossRef]
- Nomura, S.; Blangiardo, M.; Tsubokura, M.; Ozaki, A.; Morita, T.; Hodgson, S. Postnuclear disaster evacuation and chronic health in adults in Fukushima, Japan: A long-term retrospective analysis. BMJ Open 2016, 6, e010080. [Google Scholar] [CrossRef]
- Yokoyama, Y.; Otsuka, K.; Kawakami, N.; Kobayashi, S.; Ogawa, A.; Tannno, K.; Sakata, K. Mental health and related factors after the Great East Japan earthquake and tsunami. PLoS ONE 2014, 9, e102497. [Google Scholar] [CrossRef]
- Fox, K.R.; Stathi, A.; McKenna, J.; Davis, M.G. Physical activity and mental well-being in older people participating in the Better Ageing Project. Eur. J. Appl. Physiol. 2007, 100, 591–602. [Google Scholar] [CrossRef]
- Fu, R.; Noguchi, H.; Tachikawa, H.; Aiba, M.; Nakamine, S.; Kawamura, A.; Tamiya, N. Relation between social network and psychological distress among middle-aged adults in Japan: Evidence from a national longitudinal survey. Soc. Sci. Med. 2017, 175, 58–65. [Google Scholar] [CrossRef]
- Okuyama, N.; Inaba, Y. Influence of natural disasters on social engagement and post-disaster well-being: The case of the Great East Japan Earthquake. Jpn. World Econ. 2017, 44, 1–13. [Google Scholar] [CrossRef]
- Carol, D.R.; Barry, T.R.; Elliot, M.F. Persistent psychological well-being predicts improved self-rated health over 9–10 years: Longitudinal evidence from MIDUS. Health Psychol. 2015, 2, 2055102915601582. [Google Scholar]
- Hommerich, C. Trust and subjective well-being after the Great East Japan Earthquake, tsunami and nuclear meltdown: Preliminary results. Int. J. Jpn. Sociol. 2013, 21, 46–64. [Google Scholar] [CrossRef]
- Kusama, T.; Aida, J.; Sugiyama, K.; Matsuyama, Y.; Koyama, S.; Sato, Y.; Osaka, K. Does the type of temporary housing make a difference in social participation and health for evacuees of the Great East Japan Earthquake and Tsunami? A Cross-sectional Study. J. Epidemiol 2018, JE20180080. [Google Scholar] [CrossRef]
- Nemoto, T. Subjective norms toward social support among Japanese American elderly in New York City: Why help does not always help. J. Community Psychol. 1998, 26, 293–316. [Google Scholar] [CrossRef]
- Işık, Ö.; Özer, N.; Sayın, N.; Mishal, A.; Gündoğdu, O.; Özçep, F. Are women in Turkey both risks and resources in disaster management? Int. J. Environ. Res. Public Health 2015, 12, 5758–5774. [Google Scholar] [CrossRef]
- Kasl, S.V. Physical and mental health effects of involuntary relocation and institutionalization on the elderly—A review. Am. J. Public Health 1972, 62, 377–384. [Google Scholar] [CrossRef]
- Tepco’s Compensation for 3/11 Victims has Made Matters Worse for Many. Available online: https://www.japantimes.co.jp/news/2018/04/13/national/tepcos-compensation-3-11-victims-made-matters-worse-many/#.XM_6yfZuLVI (accessed on 22 June 2019).
- Murakami, M.; Kumagai, A.; Ohtsuru, A. Building risk communication capabilities among professionals: Seven essential characteristics of risk communication. Radiat. Prot. Dosim. 2012, 182, 120–127. [Google Scholar] [CrossRef]
- Murakami, M.; Sato, A.; Matsui, S.; Goto, A.; Kumagai, A.; Tsubokura, M.; Ochi, S. Communicating with residents about risks following the Fukushima nuclear accident. Asia Pac. J. Public Health 2017, 29, 74S–89S. [Google Scholar] [CrossRef]
| RPH | Non-RPH | Total | p | ||
|---|---|---|---|---|---|
| n = 101 (%) | n = 158 (%) | n = 259 (%) | |||
| Sex | Male | 48 (47.5) | 75 (47.5) | 123 (47.5) | 0.99 |
| Female | 53 (52.5) | 83 (52.5) | 136 (52.5) | ||
| Age | Mean (Standard deviation) | 75.0 (7.6) | 73.8 (6.6) | 74.3 (7.0) | 0.12 |
| Physical activity level | Inactive | 17 (16.8) | 21 (13.3) | 38 (14.7) | 0.43 |
| Active | 84 (83.2) | 137 (86.7) | 221 (85.3) | ||
| Social network | Low | 50 (49.5) | 75 (47.5) | 125 (48.3) | 0.75 |
| High | 51 (50.5) | 83 (52.5) | 134 (51.7) | ||
| Functional health | Dependent | 72 (71.3) | 86 (54.4) | 158 (61.0) | <0.01 |
| Independent | 29 (28.7) | 72 (45.6) | 101 (39.0) | ||
| Chronic disease history | Presence | 79 (78.2) | 105 (66.5) | 184 (71.0) | 0.04 |
| Absence | 22 (21.8) | 53 (33.5) | 75 (29.0) | ||
| Household structure | Living alone | 57 (56.4) | 20 (12.7) | 77 (29.7) | <0.01 |
| Couple/nuclear family/other | 43 (42.6) | 125 (79.1) | 168 (64.9) | ||
| Three-generation family | 1 (1.0) | 13 (8.2) | 14 (5.4) |
| RPH | Non-RPH | Total | p-Value | ||
|---|---|---|---|---|---|
| n = 101 (%) | n = 158 (%) | n = 259 (%) | |||
| SWB | Mean (Standard deviation) | 12.76 (5.18) | 14.11 (4.82) | 13.59 (5.00) | 0.03 |
| Trust | Mistrust | 63 (62.4) | 44 (27.8) | 107 (41.3) | <0.01 |
| High | 38 (37.6) | 114 (72.2) | 152 (58.7) | ||
| Reciprocity | Lack of reciprocity | 45 (44.6) | 38 (24.1) | 83 (32.0) | <0.01 |
| High | 56 (55.4) | 120 (75.9) | 176 (68.0) | ||
| Participation | Absence | 42 (41.6) | 69 (43.7) | 111 (42.9) | 0.40 |
| One or two | 40 (39.6) | 69 (43.7) | 109 (42.1) | ||
| More than three | 19 (18.8) | 20 (12.7) | 39 (15.1) |
| WHO-5-J Score | p | 99% CI | ||
|---|---|---|---|---|
| Mean (SD) | ||||
| Trust | Mistrust (n = 107) | 11.58 (4.47) | <0.01 | 1.88, 4.96 |
| High (n = 152) | 15.00 (4.88) | |||
| Reciprocity | Lack of reciprocity (n = 83) | 12.67 (4.85) | 0.04 | −0.37, 3.06 |
| High (n = 176) | 14.02 (5.02) | |||
| Participation | Absence (n = 111) a | 12.25 (5.34) | <0.01 | b-a: −0.09, 3.77 c-a: 1.05, 6.39 c-b: −0.79, 4.56 |
| One to two (n = 109) b | 14.09 (4.11) | |||
| More than three (n = 39) c | 15.97 (5.20) | |||
| Sex | Male (n = 123) | 13.30 (4.69) | 0.34 | −1.83, 0.64 |
| Female (n = 136) | 13.90 (5.32) | |||
| Physical activity level | Inactive (n = 38) | 9.89 (5.74) | <0.01 | 1.69, 6.96 |
| Active (n = 221) | 14.22 (4.58) | |||
| Social network | Low (n = 125) | 11.97 (4.92) | <0.01 | 1.59, 4.66 |
| High (n = 134) | 15.10 (4.60) | |||
| Functional health | Dependent (n = 158) | 11.28 (5.00) | <0.01 | 1.84, 4.87 |
| Independent (n = 101) | 15.63 (4.28) | |||
| Chronic disease history | Presence (n = 184) | 13.43 (4.88) | 0.43 | −1.23, 2.32 |
| Absence (n = 75) | 13.97 (5.29) | |||
| Household structure | Living alone (n = 77) d | 13.47(4.73) | 0.80 | e-d: −1.94, 2.16 f-d: −3.35, 5.29 f-e: −3.28, 4.91 |
| Couple/nuclear family (n = 168) e | 13.57(5.20) | |||
| Three-generation family (n = 14) f | 14.43 (4.03) |
| β | p | β | p | β | p | |
|---|---|---|---|---|---|---|
| (99% CI) | (99% CI) | (99% CI) | ||||
| Trust (for mistrust) | −0.293 | <0.01 | - | - | - | - |
| (−0.535, −0.051) | ||||||
| Reciprocity (for lack of reciprocity) | - | 0.077 | 0.43 | - | - | |
| (−0.175, 0.329) | ||||||
| Participation (for less participation) | - | - | - | −0.238 | 0.02 | |
| (−0.495, 0.020) | ||||||
| Sex (for female) | −0.005 | 0.95 | −0.043 | 0.67 | −0.016 | 0.87 |
| (−0.258, 0.247) | (−0.307, 0.222) | (−0.274, 0.241) | ||||
| Age | 0.084 | 0.38 | 0.119 | 0.24 | 0.123 | 0.21 |
| (−0.167, 0.336) | (−0.145, 0.384) | (−0.134, 0.379) | ||||
| Physical activity (for inactive) | −0.234 | 0.02 | −0.271 | <0.01 | −0.205 | 0.04 |
| (−0.484, 0.016) | (−0.536, −0.005) | (−0.466, 0.056) | ||||
| Social network (for low) | −0.158 | 0.11 | −0.155 | 0.14 | −0.113 | 0.27 |
| (−0.417, 0.102) | (−0.431, 0.121) | (−0.385, 0.159) | ||||
| Functional health (for poor) | −0.151 | 0.14 | −0.23 | 0.03 | −0.196 | 0.06 |
| (−0.417, 0.116) | (−0.507, 0.048) | (−0.463, 0.072) | ||||
| Chromic disease history (for presence) | 0 | 0.99 | −0.044 | 0.65 | −0.002 | 0.98 |
| (−0.239, 0.240) | (−0.296, 0.209) | (−0.248, 0.243) | ||||
| Household structure (for living alone) | −0.072 | 0.43 | −0.107 | 0.26 | −0.126 | 0.17 |
| (−0.309, 0.165) | (−0.354, 0.140) | (−0.367, 0.115) |
| β | p | β | p | β | p | |
|---|---|---|---|---|---|---|
| (99% CI) | (99% CI) | (99% CI) | ||||
| Trust (for mistrust) | −0.2 | <0.01 | - | - | - | - |
| (−0.395, −0.004) | ||||||
| Reciprocity (for lack of reciprocity) | - | −0.125 | 0.1 | - | - | |
| (−0.320, 0.070) | ||||||
| Participation (for less participation) | - | - | - | −0.038 | 0.64 | |
| (−0.255, 0.178) | ||||||
| Sex (for female) | −0.149 | 0.05 | −0.165 | 0.03 | −0.163 | 0.03 |
| (−0.342, 0.044) | (−0.360, 0.029) | (−0.363, 0.037) | ||||
| Age | 0.038 | 0.63 | 0.066 | 0.41 | 0.08 | 0.32 |
| (−0.169, 0.245) | (−0.141, 0.273) | (−0.128, 0.287) | ||||
| Physical activity (for inactive) | −0.188 | 0.02 | −0.193 | 0.01 | −0.185 | 0.02 |
| (−0.388, 0.012) | (−0.395, 0.010) | (−0.392, 0.022) | ||||
| Social network (for low) | −0.207 | 0.01 | −0.211 | 0.01 | −0.212 | 0.02 |
| (−0.420, 0.007) | (−0.428, 0.005) | (−0.444, 0.019) | ||||
| Functional health (for poor) | −0.202 | 0.01 | −0.215 | 0.01 | −0.222 | <0.01 |
| (−0.416, 0.011) | (−0.431, 0.002) | (−0.440, −0.004) | ||||
| Chromic disease history (for presence) | 0.06 | 0.42 | 0.049 | 0.51 | 0.045 | 0.58 |
| (−0.133, 0.253) | (−0.147, 0.245) | (−0.154, 0.243) | ||||
| Household structure (for living alone) | −0.038 | 0.6 | −0.101 | 0.54 | −0.068 | 0.36 |
| (−0.153, 0.228) | (−0.148, 0.239) | (−0.126, 0.262) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moriyama, N.; Iwasa, H.; Tsubokura, M.; Kuroda, Y.; Yasumura, S. Living in the Restoration Public Housing after the Great East Japan Earthquake Correlates with Lower Subjective Well-Being of Older Adults. Int. J. Environ. Res. Public Health 2019, 16, 2696. https://doi.org/10.3390/ijerph16152696
Moriyama N, Iwasa H, Tsubokura M, Kuroda Y, Yasumura S. Living in the Restoration Public Housing after the Great East Japan Earthquake Correlates with Lower Subjective Well-Being of Older Adults. International Journal of Environmental Research and Public Health. 2019; 16(15):2696. https://doi.org/10.3390/ijerph16152696
Chicago/Turabian StyleMoriyama, Nobuaki, Hajime Iwasa, Masaharu Tsubokura, Yujiro Kuroda, and Seiji Yasumura. 2019. "Living in the Restoration Public Housing after the Great East Japan Earthquake Correlates with Lower Subjective Well-Being of Older Adults" International Journal of Environmental Research and Public Health 16, no. 15: 2696. https://doi.org/10.3390/ijerph16152696
APA StyleMoriyama, N., Iwasa, H., Tsubokura, M., Kuroda, Y., & Yasumura, S. (2019). Living in the Restoration Public Housing after the Great East Japan Earthquake Correlates with Lower Subjective Well-Being of Older Adults. International Journal of Environmental Research and Public Health, 16(15), 2696. https://doi.org/10.3390/ijerph16152696







