Maternal and Child Nutrition and Oral Health in Urban Vietnam
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Demographics
3.2. Nutrition
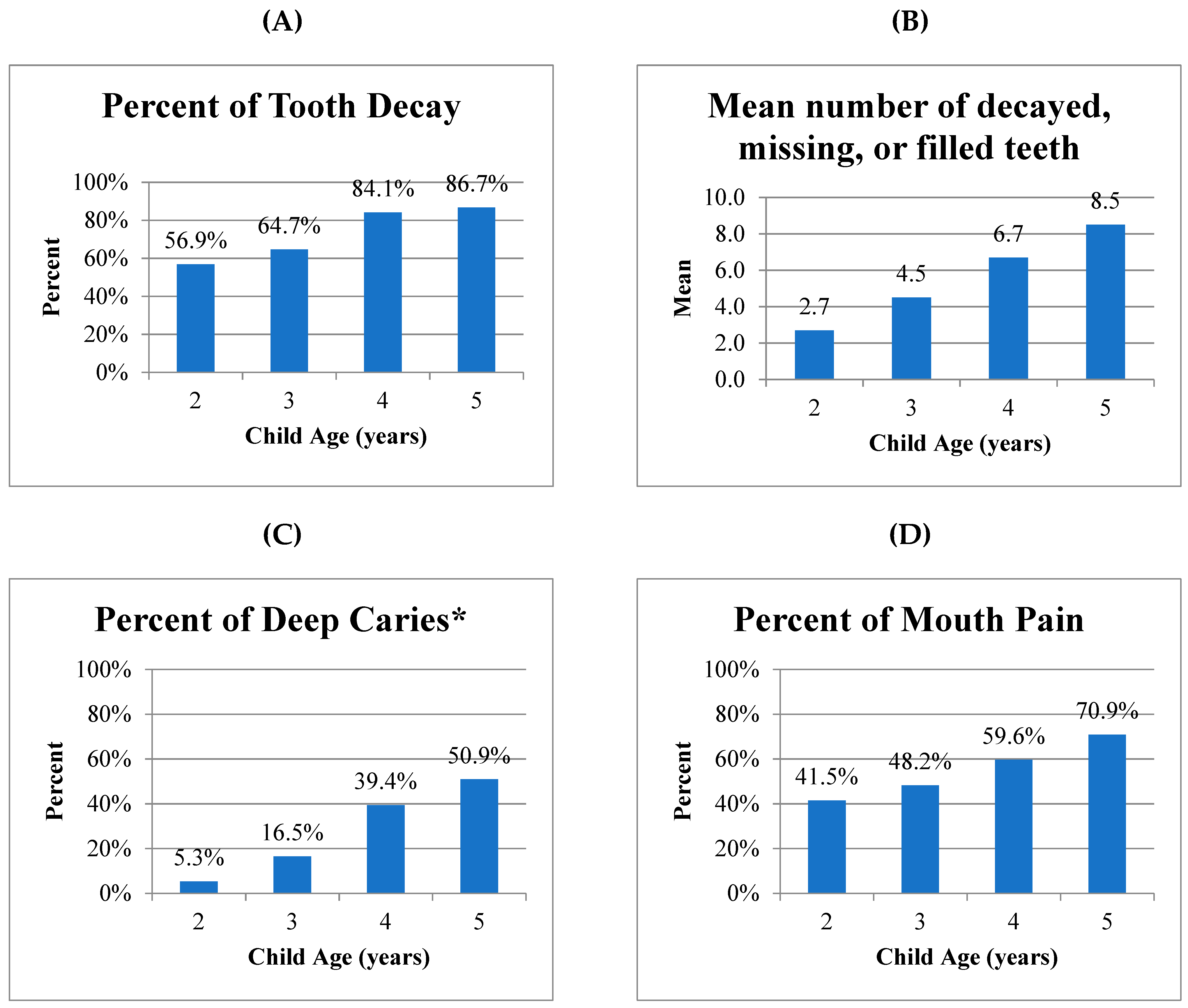
3.3. Oral Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Popkin, B.M. The nutrition transition: An overview of world patterns of change. Nutr. Rev. 2004, 62, S140–S143. [Google Scholar] [CrossRef] [PubMed]
- Phantumvanit, P.; Makino, Y.; Ogawa, H.; Rugg-Gunn, A.; Moynihan, P.; Petersen, P.E.; Evans, W.; Feldens, C.A.; Lo, E.; Khoshnevisan, M.H.; et al. WHO Global Consultation on Public Health Intervention against Early Childhood Caries. Community Dent. Oral Epidemiol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Sheiham, A. Dental caries affects body weight, growth and quality of life in pre-school children. Br. Dent. J. 2006, 201, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Albino, J.; Tiwari, T. Preventing Childhood Caries: A Review of Recent Behavioral Research. J. Dent. Res. 2016, 95, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Anil, S.; Anand, P.S. Early Childhood Caries: Prevalence, Risk Factors, and Prevention. Front. Pediatr. 2017, 5, 157. [Google Scholar] [CrossRef] [PubMed]
- Tinanoff, N.; Baez, R.J.; Diaz Guillory, C.; Donly, K.J.; Feldens, C.A.; McGrath, C.; Phantumvanit, P.; Pitts, N.B.; Seow, W.K.; Sharkov, N.; et al. Early childhood caries epidemiology, aetiology, risk assessment, societal burden, management, education, and policy: Global perspective. Int. J. Paediatr. Dent./Br. Paedodontic Soc. Int. Assoc. Dent. Child. 2019, 29, 238–248. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatric Dentistry. Policy on Early Childhood Caries (ECC): Classifications, Consequences, and Preventive Strategies. Pediatr. Dent. 2017, 39, 59–61. [Google Scholar]
- Lueangpiansamut, J.; Chatrchaiwiwatana, S.; Muktabhant, B.; Inthalohit, W. Relationship between dental caries status, nutritional status, snack foods, and sugar-sweetened beverages consumption among primary schoolchildren grade 4–6 in Nongbua Khamsaen school, Na Klang district, Nongbua Lampoo Province, Thailand. J. Med. Assoc. Thail. Chotmaihet Thangphaet 2012, 95, 1090–1097. [Google Scholar]
- Senesombath, S.; Nakornchai, S.; Banditsing, P.; Lexomboon, D. Early childhood caries and related factors in Vientiane, Lao PDR. Southeast Asian J. Trop. Med. Public Health 2010, 41, 717–725. [Google Scholar]
- Duangthip, D.; Gao, S.S.; Lo, E.C.M.; Chu, C.H. Early childhood caries among 5- to 6-year-old children in Southeast Asia. Int. Dent. J. 2017, 67, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Ly, K.A.; Ton, T.G.; Ngo, Q.V.; Vo, T.T.; Fitzpatrick, A.L. Double burden: A cross-sectional survey assessing factors associated with underweight and overweight status in Danang, Vietnam. BMC Public Health 2013, 13, 35. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.T.; Hoang, M.V. Non-communicable diseases, food and nutrition in Vietnam from 1975 to 2015: The burden and national response. Asia Pac. J. Clin. Nutr. 2018, 27, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Jacobsson, B.; Ho Thi, T.; Hoang Ngoc, C.; Hugoson, A. Sociodemographic conditions, knowledge of dental diseases, dental care, and dietary habits. J. Public Health Dent. 2015. [Google Scholar] [CrossRef] [PubMed]
- Dieu, H.T.; Dibley, M.J.; Sibbritt, D.; Hanh, T.T. Prevalence of overweight and obesity in preschool children and associated socio-demographic factors in Ho Chi Minh City, Vietnam. Int. J. Pediatr. Obes. 2007, 2, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Do, L.G. Distribution of caries in children: Variations between and within populations. J. Dent. Res. 2012, 91, 536–543. [Google Scholar] [CrossRef]
- Yen, N.T.H.; Kanchanakhan, N. Prevalence and factors related to dental caries among 6 year-old children in Nha Trang City, Khanh Hoa Province, Vietnam. J. Health Res. 2015, 29, 251–258. [Google Scholar]
- Ngoc, V.; Chu, D.; Le, D. Prevalence of early childhood caries and its related risk factors in preschoolers: Result from a cross sectional study in Vietnam. Pediatr. Dent. J. 2017, 27, 79–84. [Google Scholar]
- Nguyen, Y.; Ueno, M.; Zaitsu, T.; Nguyen, T.; Kawaguchi, Y. Early Childhood Caries and Risk Factors in Vietnam. J. Clin. Pediatr. Dent. 2018, 42, 173–181. [Google Scholar] [CrossRef]
- World Health Organization. Oral Health Surveys: Basic Methods; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006; p. 312. [Google Scholar]
- Thuy, T.T.; Nakagaki, H.; Ha, N.T.T.; Morita, I.; Tatematsu, M.; Lan, H.A.; Hung, H.T.; Robinson, C. Fluoride profiles in premolars after different durations of water fluoridation in Ho Chi Minh City, Vietnam. Arch. Oral Biol. 2003, 48, 369–376. [Google Scholar] [CrossRef]
- Dearden, K.A.; Quan, L.N.; Do, M.; Marsh, D.R.; Pachón, H.; Schroeder, D.G.; Lang, T.T. Work outside the Home is the Primary Barrier to Exclusive Breastfeeding in Rural Viet Nam: Insights from Mothers Who Exclusively Breastfed and Worked. Food Nutr. Bull. 2002, 23, 99–106. [Google Scholar] [CrossRef]
- Nguyen, T.T.; Withers, M.; Hajeebhoy, N.; Frongillo, E.A. Infant Formula Feeding at Birth Is Common and Inversely Associated with Subsequent Breastfeeding Behavior in Vietnam. J. Nutr. 2016, 146, 2102–2108. [Google Scholar] [CrossRef] [PubMed]
- Baker, P.; Smith, J.; Salmon, L.; Friel, S.; Kent, G.; Iellamo, A.; Dadhich, J.P.; Renfrew, M.J. Global trends and patterns of commercial milk-based formula sales: Is an unprecedented infant and young child feeding transition underway? Public Health Nutr. 2016, 19, 2540–2550. [Google Scholar] [CrossRef] [PubMed]
- Hop, L.T.; Gross, R.; Giay, T.; Sastroamidjojo, S.; Schultink, W.; Lang, N.T. Premature Complementary Feeding Is Associated with Poorer Growth of Vietnamese Children. J. Nutr. 2000, 130, 2683–2690. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.H.Q.; Worsley, A.; Lawrence, M.; Marshall, B. Perceptions of nutrition transition problems: A qualitative study of Vietnamese health and education professionals. Int. J. Health Promot. Educ. 2017, 55, 158–172. [Google Scholar] [CrossRef]
- Do, L.M.; Tran, T.K.; Eriksson, B.; Petzold, M.; Ascher, H. Prevalence and incidence of overweight and obesity among Vietnamese preschool children: A longitudinal cohort study. BMC Pediatr. 2017, 17, 150. [Google Scholar] [CrossRef] [PubMed]
- Teshome, A.; Yitayeh, A. Relationship between periodontal disease and preterm low birth weight: Systematic review. Pan Afr. Med. J. 2016, 24, 215. [Google Scholar] [CrossRef] [PubMed]
- Leong, P.M.; Gussy, M.G.; Barrow, S.-Y.L.; de Silva-Sanigorski, A.; Waters, E. A systematic review of risk factors during first year of life for early childhood caries. Int. J. Paediatr. Dent. 2013, 23, 235–250. [Google Scholar] [CrossRef]
- Wong, D.; Perez-Spiess, S.; Julliard, K. Attitudes of Chinese parents toward the oral health of their children with caries: A qualitative study. Pediatr. Dent. 2005, 27, 505–512. [Google Scholar]
- Hayden, C.; Bowler, J.O.; Chambers, S.; Freeman, R.; Humphris, G.; Richards, D.; Cecil, J.E. Obesity and dental caries in children: A systematic review and meta-analysis. Community Dent. Oral Epidemiol. 2013, 41, 289–308. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Maintaining and Improving the Oral Health of Young Children. Section on oral Health. Pediatrics 2014, 134, 1224–1229. [Google Scholar] [CrossRef] [PubMed]
- Colchero, M.A.; Rivera-Dommarco, J.; Popkin, B.M.; Ng, S.W. In Mexico, Evidence of Sustained Consumer Response Two Years After Implementing A Sugar-Sweetened Beverage Tax. Health Aff. (Proj. Hope) 2017, 36, 564–571. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Number of Respondents (n = 571 Families) | % or Mean (SD) |
|---|---|---|
| Locations: | ||
| Central Vietnam | 339 | 59.4% |
| South Vietnam | 232 | 40.6% |
| Maternal Characteristics: | ||
| Mother Age (years) | 553 | 33.1 (5.0) |
| Mother Education Level (years) | 485 | 12.8 (3.7) |
| Child Characteristics: | ||
| Child Age (years) | ||
| 2 | 65 | 11.4% |
| 3 | 201 | 35.2% |
| 4 | 207 | 36.2% |
| 5 | 98 | 17.2% |
| Child Sex (% Male–% Female) | 287–274 | 51.2%–48.8% |
| Household Characteristics: | ||
| Number of children in household | 567 | 1.6 (0.6) |
| Number of people in household | 532 | 4.5 (1.7) |
| Home has electricity | 563 | 99.5% |
| Home has potable water | 531 | 98.7% |
| Time to walk from home to store selling processed snack food (minutes) | 560 | 5.0 (7.5) |
| Nutrition Characteristics | Total Number of Respondents | Percent Daily | Mean (SD) or % |
|---|---|---|---|
| Mother’s Nutrition Practices | |||
| Frequency of milk consumption | 557 | 27.7 % daily | 3.3 (4.4) times/week |
| Frequency of soda consumption | 547 | 2.7% daily | 0.9 (1.6) times/week |
| Frequency of chips consumption | 548 | 1.3% daily | 0.8 (1.3) times/week |
| Child Nutrition Practices | |||
| Breastfed | 548 | 95.3% | |
| Duration of breastfeeding (months) | 482 | 14.7 (7.8) months | |
| Bottle-fed | 537 | 83.1% | |
| Duration of bottle-feeding (months) | 155 | 19.6 (11.7) months | |
| Fell asleep with the baby bottle in mouth | |||
| Occasionally | 432 | 17.6% | |
| Frequently/almost always | 10.2% | ||
| Frequency of milk consumption | 486 | 91.2 % daily | 13.9 (5.8) times/week |
| Frequency of soda consumption | 441 | 5.7% daily | 1.3 (2.8) times/week |
| Frequency of chips consumption | 478 | 11.1% daily | 1.9 (2.7) times/week |
| Frequency of sweets consumption | 462 | 11.9% daily | 2.0 (3.0) times/week |
| Child Nutrition Status | |||
| Height-for-age malnutrition | 554 | 4.2% | |
| Weight-for-age malnutrition | 554 | 2.4% | |
| Weight-for-height malnutrition | 477 | 1.1% | |
| BMI-for-age malnutrition | 553 | 1.5% | |
| BMI-for-age overweight/obesity | 553 | 23.2% | |
| Oral Health Characteristics | Mean or % | ||
| Mother’s Oral Health Status | |||
| Mother report of current oral health problem (e.g., pain, decayed tooth, abscess, inflammation, bleeding gums) | 425 | 91.1% | |
| Mother ever visited a dentist | 557 | 98.0% | |
| Time since mother’s last dental visit (months) | 377 | 8.5 (14.8) months | |
| Mother received prenatal care | 554 | 100% | |
| Mother’s Knowledge about Child Oral Health | |||
| Knows that sweets and candy can cause tooth decay | 480 | 67.5% | |
| Knows that sweet drinks can cause tooth decay | 480 | 5.2% | |
| Knows that bottle-feeding can cause tooth decay | 480 | 2.7% | |
| Knows that not brushing teeth can cause tooth decay | 480 | 52.7% | |
| Maternal-Child Oral Health Practices | |||
| Child has own toothbrush at home | 545 | 99.1% | |
| Family has toothpaste at home | 545 | 96.0% | |
| Mother helps child brush teeth frequently/almost always | 545 | 80.7% | |
| Child ever visited a dentist | 455 | 44.4% | |
| Child Oral Health Status | |||
| Percent of children with any tooth decay | 571 | 74.6% | |
| Average proportion of teeth with untreated decay* (d/dmft) | 429 | 96.4% | |
| Number of teeth with active decay (d) | 571 | 5.5 (5.2) | |
| Decayed, missing, filled teeth (dmft) index | 571 | 5.8 (5.4) | |
| Presence of deep decay near pulp (data from Da Nang only) | 339 | 29.8% | |
| Child complains of pain in mouth/teeth | 423 | 56.3% | |
| Child has problems eating due to mouth pain | 533 | 40.7% | |
| Child has problems sleeping due to mouth pain | 538 | 21.9% | |
| Mother’s assessment of child’s oral health as poor | 547 | 14.8% | |
| Mother’s assessment of child’s overall health as poor | 542 | 2.0% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, D.; Sokal-Gutierrez, K.; Chung, K.; Lin, W.; Khanh, L.N.; Chung, R.; Hoang, H.T.; Ivey, S.L. Maternal and Child Nutrition and Oral Health in Urban Vietnam. Int. J. Environ. Res. Public Health 2019, 16, 2579. https://doi.org/10.3390/ijerph16142579
Huang D, Sokal-Gutierrez K, Chung K, Lin W, Khanh LN, Chung R, Hoang HT, Ivey SL. Maternal and Child Nutrition and Oral Health in Urban Vietnam. International Journal of Environmental Research and Public Health. 2019; 16(14):2579. https://doi.org/10.3390/ijerph16142579
Chicago/Turabian StyleHuang, Debbie, Karen Sokal-Gutierrez, Kenny Chung, Wenting Lin, Linh Ngo Khanh, Raymond Chung, Hung Trong Hoang, and Susan L. Ivey. 2019. "Maternal and Child Nutrition and Oral Health in Urban Vietnam" International Journal of Environmental Research and Public Health 16, no. 14: 2579. https://doi.org/10.3390/ijerph16142579
APA StyleHuang, D., Sokal-Gutierrez, K., Chung, K., Lin, W., Khanh, L. N., Chung, R., Hoang, H. T., & Ivey, S. L. (2019). Maternal and Child Nutrition and Oral Health in Urban Vietnam. International Journal of Environmental Research and Public Health, 16(14), 2579. https://doi.org/10.3390/ijerph16142579





