Relationship between Problematic Internet Use, Sleep Problems, and Oral Health in Korean Adolescents: A National Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measurements
2.3. General Demographic Characteristics
2.4. Health Related Factors
2.5. Problematic Internet Use
2.6. Oral Health
2.7. Statistical Analysis
3. Results
3.1. Oral Disease Symptoms Experienced According to General Characteristics
3.2. Oral Disease Symptoms Experienced According to Health Related Factors and Problematic Internet Use
3.3. Risk of Oral Disease Symptoms According to Problematic Internet Use and Sleep Problems by Gender
3.4. Subgroup Analysis of the Relationship between Problematic Internet Use and Each of the Six Oral Disease Symptoms
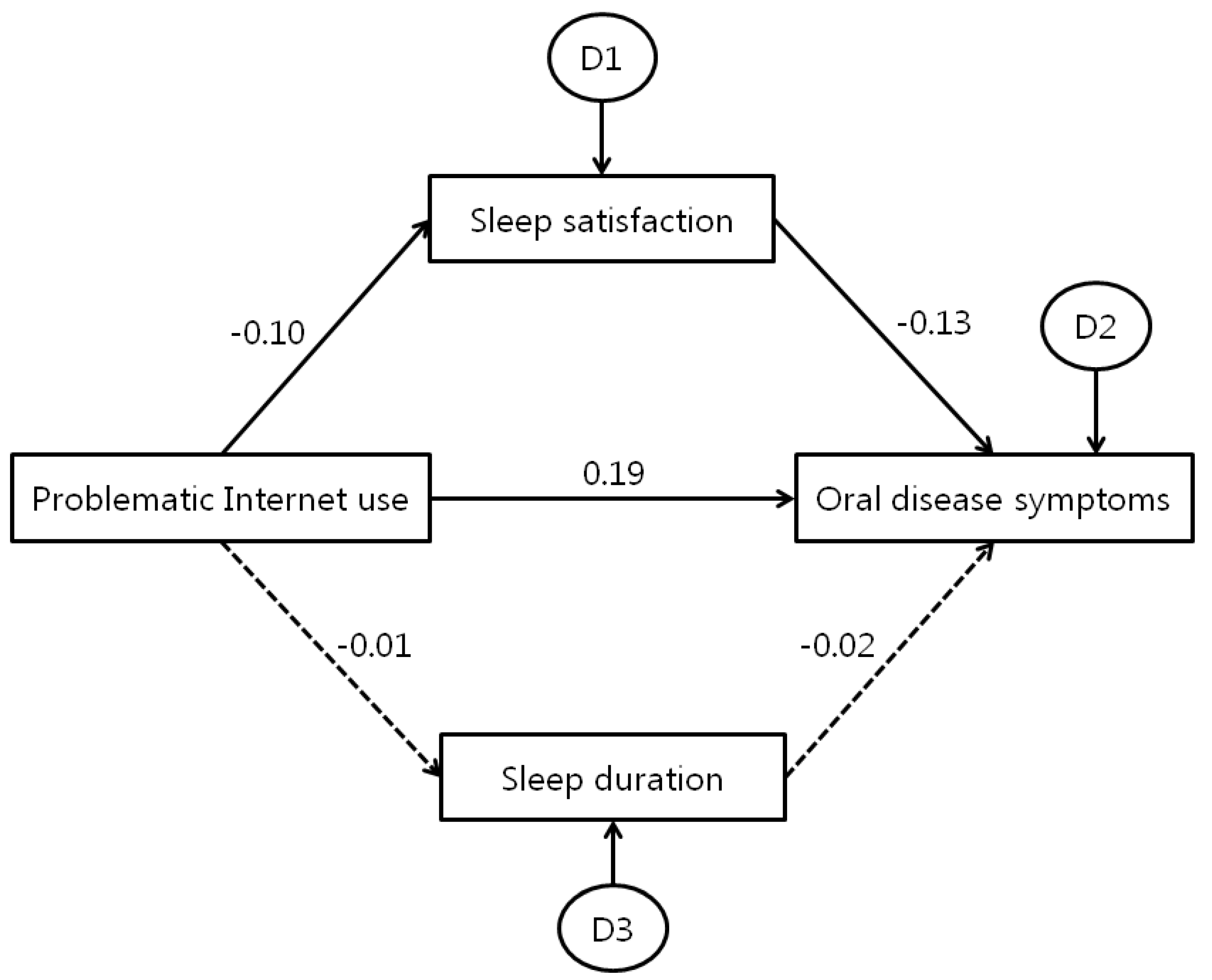
3.5. Path Analysis for Direct and Indirect Causal Relationships between Problematic Internet Use, Sleep, and Oral Health
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Heo, J.; Oh, J.; Subramanian, S.V.; Kim, Y.; Kawachi, I. Addictive internet use among Korean adolescents: A national survey. PLoS ONE 2014, 9, e87819. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Park, J.Y.; Kim, S.B.; Jung, I.K.; Lim, Y.S.; Kim, J.H. The effects of Internet addiction on the lifestyle and dietary behavior of Korean adolescents. Nutr. Res. Pract. 2010, 4, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Park, S. Associations of physical activity with sleep satisfaction, perceived stress, and problematic Internet use in Korean adolescents. BMC Public Health 2014, 14, 1143. [Google Scholar] [CrossRef] [PubMed]
- Park, M.H.; Jeon, H.O. Relationships between health behaviors, mental health and internet addiction by gender differences among Korean adolescents. J. Korean Acad. Ind. Coop. Soc. 2013, 14, 1283–1293. [Google Scholar] [CrossRef]
- Blinka, L.; Skarupova, K.; Sevcikova, A.; Wolfling, K.; Muller, K.W.; Dreier, M. Excessive Internet use in European adolescents: What determines differences in severity? Int. J. Public Health 2015, 60, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Nuutinen, T.; Roos, E.; Ray, C.; Villberg, J.; Valimaa, R.; Rasmussen, M.; Holstein, B.; Godeau, E.; Beck, F.; Léger, D.; et al. Computer use, sleep duration and health symptoms: A cross-sectional study of 15-year-olds in three countries. Int. J. Public Health 2014, 59, 619–628. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Ko, K.D.; Shin, S.I.; Ha, Y.J.; Kim, G.Y.; Kim, H.A. Association of oral health behaviors and status with depression: Results from the Korean National Health and Nutrition Examination Survey, 2010. J. Public Health Dent. 2014, 74, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Kaess, M.; Durkee, T.; Brunner, R.; Carli, V.; Parzer, P.; Wasserman, C.; Sarchiapone, M.; Hoven, C.; Apter, A.; Balazs, J.; et al. Pathological Internet use among European adolescents: Psychopathology and self-destructive behaviours. Eur. Child Adolesc. Psychiatry 2014, 23, 1093–1102. [Google Scholar] [CrossRef] [PubMed]
- Kelley, K.J.; Gruber, E.M. Problematic Internet use and physical health. J. Behav. Addict. 2013, 2, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Lam, L.T. Risk factors of Internet addiction and the health effect of internet addiction on adolescents: A systematic review of longitudinal and prospective studies. Curr. Psychiatry Rep. 2014, 16, 508. [Google Scholar] [CrossRef] [PubMed]
- An, J.; Sun, Y.; Wan, Y.; Chen, J.; Wang, X.; Tao, F. Associations between problematic internet use and adolescents’ physical and psychological symptoms: Possible role of sleep quality. J. Addict. Med. 2014, 8, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Lam, L.T. Internet gaming addiction, problematic use of the internet, and sleep problems: A systematic review. Curr. Psychiatry Rep. 2014, 16, 444. [Google Scholar] [CrossRef] [PubMed]
- Cain, N.; Gradisar, M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010, 11, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Gau, S.S.-F. Sleep problems and internet addiction among children and adolescents: A longitudinal study. J. Sleep Res. 2016, 25, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Christensen, L.; Somers, S. Comparison of nutrient intake among depressed and nondepressed individuals. Int. J. Eat. Disord. 1996, 20, 105–109. [Google Scholar] [CrossRef]
- Choi, K.; Son, H.; Park, M.; Han, J.; Kim, K.; Lee, B.; Gwak, H. Internet overuse and excessive daytime sleepiness in adolescents. Psychiatry Clin. Neurosci. 2009, 63, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Grover, V.; Malhotra, R.; Kaur, H. Exploring association between sleep deprivation and chronic periodontitis: A pilot study. J. Indian Soc. Periodontol. 2015, 19, 304–307. [Google Scholar] [CrossRef] [PubMed]
- Wiener, R.C. Relationship of routine inadequate sleep duration and periodontitis in a nationally representative sample. Sleep Disord. 2016, 2016, 9158195. [Google Scholar] [CrossRef] [PubMed]
- Besedovsky, L.; Lange, T.; Born, J. Sleep and immune function. Pflug. Arch. 2012, 463, 121–137. [Google Scholar] [CrossRef] [PubMed]
- Dinges, D.F.; Douglas, S.D.; Hamarman, S.; Zaugg, L.; Kapoor, S. Sleep deprivation and human immune function. Adv. Neuroimmunol. 1995, 5, 97–110. [Google Scholar] [CrossRef]
- Carra, M.C.; Schmitt, A.; Thomas, F.; Danchin, N.; Pannier, B.; Bouchard, P. Sleep disorders and oral health: A cross-sectional study. Clin. Oral Investig. 2017, 21, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Celik, C.B.; Odaci, H.; Bayraktar, N. Is problematic internet use an indicator of eating disorders among Turkish university students? Eat. Weight Disord. 2015, 20, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Do, K.Y.; Lee, E.S.; Lee, K.S. Association between excessive internet use and oral health behaviors of Korean adolescents: A 2015 national survey. Community Dent. Health 2017, 34, 183–189. [Google Scholar] [PubMed]
- World Health Organization. Oral Health Fact Sheet No. 318. 2012. Available online: http://www.who.int/oral_health/publications/factsheet/en/ (accessed on 16 May 2017).
- Soares Luis, H.P.; Assunçao, V.A.; Soares Luis, L.F. Oral health habits, attitudes and behaviors of Portuguese adolescents. Int. J. Adolesc. Med. Health 2016, 28, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Calderon, S.J.; Mallory, C. A systematic review of oral health behavior research in American adolescents. J. Sch. Nurs. 2014, 30, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Lam, L.T. Parental mental health and Internet Addiction in adolescents. Addict. Behav. 2015, 42, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Hong, K.E.; Park, E.J.; Ha, K.S.; Yoo, H.J. The association between problematic internet use and depression, suicidal ideation and bipolar disorder symptoms in Korean adolescents. Aust. N. Z. J. Psychiatry 2013, 47, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Reed, P.; Vile, R.; Osborne, L.A.; Romano, M.; Truzoli, R. Problematic Internet Usage and Immune Function. PLoS ONE 2015, 10, e0134538. [Google Scholar] [CrossRef] [PubMed]
- Yoo, Y.S.; Cho, O.H.; Cha, K.S. Associations between overuse of the internet and mental health in adolescents. Nurs. Health Sci. 2014, 16, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Science and ICT; National Information Society Agency. The Survey on Smart Phone over Dependence; Ministry of Science and ICT: Gwacheon, Korea; National Information Society Agency: Daegu, Korea, 2017.
- Reners, M.; Brecx, M. Stress and periodontal disease. Int. J. Dent. Hyg. 2007, 5, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.-K. The Follow up Study of Internet Addiction Proneness Scale; Korea National Information Society Agency: Seoul, Korea, 2008. [Google Scholar]
- Chen, M.; Anderson, R.M.; Barmes, D.E.; Leclercq, M.-H.; Lyttle, C.S. Comparing Oral Health Care Systems: A Second International Collaborative Study; In Collaboration with the Center for Health Administration Studies, University of Chicago; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Korea Internet and Security Agency. Survey of Internet Usage; Korea Internet and Security Agency: Seoul, Korea, 2014. [Google Scholar]
- Block, J.J. Issues for DSM-V: Internet addiction. Am. J. Psychiatry 2008, 165, 306–307. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th ed.; American Psychiatric Publishing: Arlington, TX, USA, 2013. [Google Scholar]
- Griffiths, M.D.; Kuss, D.J.; Billieux, J.; Pontes, H.M. The evolution of Internet addiction: A global perspective. Addict. Behav. 2016, 53, 193–195. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.Y.; Lee, M.B.; Liao, S.C.; Chang, L.R. Risk factors of internet addiction among Internet users: An online questionnaire survey. PLoS ONE 2015, 10, e0137506. [Google Scholar] [CrossRef] [PubMed]
- Sundararajan, S.; Muthukumar, S.; Rao, S.R. Relationship between depression and chronic periodontitis. J. Indian Soc. Periodontol. 2015, 19, 294–296. [Google Scholar] [PubMed]
- Tothova, L.; Celecova, V.; Celec, P. Salivary markers of oxidative stress and their relation to periodontal and dental status in children. Dis. Markers 2013, 34, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Werner, H.; Hakeberg, M.; Dahlstrom, L.; Eriksson, M.; Sjogren, P.; Strandell, A.; Svanberg, T.; Svensson, L.; Wide Boman, U. Psychological Interventions for poor oral health: A systematic review. J. Dent. Res. 2016, 95, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Korea Centers for Disease Control and Prevention. Korea Youth Risk Behavior Web-Based Survey 2010: Survey Press Releases; Korea Centers for Disease Control and Prevention: Osong, Korea, 2011.
- Johannsen, A.; Rylander, G.; Soder, B.; Asberg, M. Dental plaque, gingival inflammation, and elevated levels of interleukin-6 and cortisol in gingival crevicular fluid from women with stress-related depression and exhaustion. J. Periodontol. 2006, 77, 1403–1409. [Google Scholar] [CrossRef] [PubMed]
- Rosania, A.E.; Low, K.G.; McCormick, C.M.; Rosania, D.A. Stress, depression, cortisol, and periodontal disease. J. Periodontol. 2009, 80, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Irwin, M. Effects of sleep and sleep loss on immunity and cytokines. Brain Behav. Immun. 2002, 16, 503–512. [Google Scholar] [CrossRef]
- Acar, M.; Türkcan, İ.; Özdaş, T.; Bal, C.; Cingi, C. Obstructive sleep apnoea syndrome does not negatively affect oral and dental health. J. Laryngol. Otol. 2015, 129, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Majde, J.A.; Krueger, J.M. Links between the innate immune system and sleep. J. Allergy Clin. Immunol. 2005, 116, 1188–1198. [Google Scholar] [CrossRef] [PubMed]
- Park, H. The relationship between Internet use for non-academic purposes and happiness and stress in adolescents. J. Korean Acad. Community Health Nurs. 2015, 26, 169–177. [Google Scholar] [CrossRef]
- Romano, M.; Osborne, L.A.; Truzoli, R.; Reed, P. Differential Psychological Impact of Internet Exposure on Internet Addicts. PLoS ONE 2013, 8, e55162. [Google Scholar] [CrossRef] [PubMed]

| Variable | Category | Oral Disease Symptoms N (Weighted %) | p-Value | |
|---|---|---|---|---|
| Yes | No | |||
| Sex | Boys | 23,973 (61.9) | 14,418 (38.1) | <0.001 |
| Girls | 24,551 (70.2) | 10,296 (29.8) | ||
| Grade | Middle School 1st (13-years-old) | 7557 (60.2) | 4911 (39.8) | <0.001 |
| Middle school 2nd (14-years-old) | 7559 (61.4) | 4740 (38.6) | ||
| Middle school 3rd (15-years-old) | 8183 (64.6) | 4420 (35.4) | ||
| High school 1st (16-years-old) | 8438 (69.4) | 3583 (30.6) | ||
| High school 2nd (17-years-old) | 8440 (68.9) | 3684 (31.1) | ||
| High school 3rd (18-years-old) | 8147 (70.4) | 3376 (29.6) | ||
| Academic Performance | High | 17,036 (65.1) | 8915 (34.9) | <0.001 |
| Middle | 12,795 (64.4) | 6856 (35.6) | ||
| Low | 18,693 (67.5) | 8943 (32.5) | ||
| Perceived Family Economic Status | High | 12,637 (59.7) | 8435 (40.3) | <0.001 |
| Middle | 22,558 (65.5) | 11,695 (34.5) | ||
| Low | 13,329 (74.1) | 4584 (25.9) | ||
| Living Status | Living with family | 45,885 (65.8) | 23,457 (34.2) | <0.001 |
| Living with relatives | 765 (67.9) | 355 (32.1) | ||
| Boarding, living in dorm | 1600 (67.4) | 665 (32.6) | ||
| Living in a care facility | 274 (53.0) | 237 (47.0) | ||
| Variable | Category | Oral Disease Symptoms N = 74,238 (Weighted %) | p-Value | |
|---|---|---|---|---|
| Yes | No | |||
| Health Related Factors | ||||
| Alcohol | Yes | 28,240 (69.6) | 12,118 (30.4) | <0.001 |
| No | 20,284 (61.2) | 12,596 (38.8) | ||
| Smoking | Yes | 13,738 (70.5) | 5647 (29.5) | <0.001 |
| No | 34,786 (64.2) | 19,067 (35.8) | ||
| Stress Level | Not at all | 725 (42.0) | 969 (58.0) | <0.001 |
| Not much | 5144 (51.4) | 4367 (48.6) | ||
| A little | 19,022 (63.8) | 10,647 (36.2) | ||
| A lot | 16,427 (72.5) | 6158 (27.5) | ||
| Very much | 7206 (75.3) | 2303 (24.7) | ||
| Sleep Satisfaction | Completely sufficient | 3073 (55.2) | 2438 (44.8) | <0.001 |
| Sufficient | 8866 (59.4) | 5950 (40.6) | ||
| Moderate | 16,123 (64.9) | 8443 (35.1) | ||
| Not sufficient | 13,726 (70.7) | 5471 (29.3) | ||
| Not at all sufficient | 6736 (74.3) | 2412 (25.7) | ||
| Sleep Duration (night/per day) | Less than 5 h | 5832 (66.4) | 2851 (33.6) | 0.201 |
| ≥5–7 h | 31,738 (65.9) | 16,040 (34.1) | ||
| ≥7–9 h | 10,382 (65.0) | 5528 (35.0) | ||
| More than 9 h | 572 (65.9) | 295 (34.1) | ||
| a PIU Group | General group | 45,340 (65.0) | 23,857 (35.0) | <0.001 |
| Potential risk group | 1468 (78.8) | 398 (21.2) | ||
| High risk group | 1716 (79.9) | 459 (20.1) | ||
| Time of Internet Use (hours/day, weekend) | Less than 1 h | 1408 (66.7) | 699 (33.3) | <0.001 |
| ≥1–2 h | 7859 (63.3) | 4478 (36.7) | ||
| ≥2–3 h | 10,279 (66.5) | 5162 (33.5) | ||
| ≥3–4 h | 7760 (68.5) | 3546 (31.5) | ||
| ≥4–5 h | 4552 (69.4) | 1988 (30.6) | ||
| ≥5–6 h | 2661 (73.4) | 998 (26.6) | ||
| More than 6 h | 3679 (72.4) | 1387 (27.6) | ||
| Variable | Model I a OR (95% CI) | Model II b AOR (95% CI)d | Model III c AOR (95% CI) |
|---|---|---|---|
| Problematic Internet Use | |||
| Group (Boys) | |||
| General group | 1 | 1 | 1 |
| Potential risk group | 1.78 (1.49–2.14) | 1.74 (1.45–2.09) | 1.59 (1.32–1.91) |
| High risk group | 2.25 (1.91–2.64) | 2.14 (1.82–2.53) | 1.92 (1.63–2.28) |
| Duration of Internet use (h/day, weekends) | |||
| Within 1 h | 1 | 1 | 1 |
| ≥1–2 h | 0.85 (0.71–1.02) | 0.85 (0.70–1.02) | 0.86 (0.71–1.03) |
| ≥2–3 h | 0.98 (0.82–1.17) | 0.97 (0.81–1.17) | 0.96 (0.80–1.15) |
| ≥3–4 h | 1.05 (0.87–1.27) | 1.04 (0.86–1.27) | 1.01 (0.84–1.23) |
| ≥4–5 h | 1.04 (0.85–1.27) | 1.02 (0.82–1.26) | 0.96 (0.78–1.19) |
| ≥5–6 h | 1.24 (1.01–1.53) | 1.23 (0.99–1.51) | 1.13 (0.92–1.41) |
| More than 6 h | 1.16 (0.95–1.42) | 1.12 (0.92–1.38) | 1.03 (0.84–1.26) |
| Sleep satisfaction | |||
| Completely sufficient | 1 | 1 | |
| Sufficient | 1.15 (1.03–1.28) | 1.04 (0.93–1.16) | |
| Moderately sufficient | 1.45 (1.31–1.60) | 1.19 (1.07–1.31) | |
| Not sufficient | 1.87 (1.66–2.11) | 1.41 (1.25–1.59) | |
| Not at all sufficient | 2.01 (1.76–2.29) | 1.40 (1.23–1.60) | |
| Sleep duration | 0.99 (0.97–1.02) | 1.01 (0.97–1.04) | |
| Problematic Internet Use Group (Girls) | |||
| General group | 1 | 1 | 1 |
| Potential risk group | 2.27 (1.74–2.97) | 2.15 (1.65–2.80) | 1.89 (1.44–2.48) |
| High risk group | 2.41 (1.83–3.17) | 2.23 (1.70–2.93) | 1.98 (1.50–2.63) |
| Duration of Internet use (h/day, weekends) | |||
| Within 1 h | 1 | 1 | 1 |
| ≥1–2 h | 0.90 (0.79–1.04) | 0.90 (0.78–1.04) | 0.89 (0.77–1.02) |
| ≥2–3 h | 1.05 (0.90–1.22) | 1.04 (0.90–1.20) | 0.96 (0.83–1.11) |
| ≥3–4 h | 1.19 (1.02–1.40) | 1.17 (0.99–1.37) | 1.04 (0.89–1.23) |
| ≥4–5 h | 1.35 (1.14–1.59) | 1.29 (1.09–1.53) | 1.12 (0.94–1.32) |
| ≥5–6 h | 1.69 (1.40–2.04) | 1.61 (1.33–1.94) | 1.38 (1.14–1.67) |
| More than 6 h | 1.48 (1.23–1.77) | 1.40 (1.16–1.67) | 1.17 (0.97–1.40) |
| Sleep satisfaction | |||
| Completely sufficient | 1 | 1 | |
| Sufficient | 1.06 (0.92–1.22) | 1.00 (0.87–1.16) | |
| Moderately sufficient | 1.26 (1.09–1.46) | 1.07 (0.93–1.24) | |
| Not sufficient | 1.59 (1.38–1.83) | 1.23 (1.07–1.42) | |
| Not at all sufficient | 2.10 (1.81–2.44) | 1.44 (1.24–1.67) | |
| Sleep duration | 0.99 (0.97–1.02) | 1.01 (0.99–1.04) |
| Variable (Six Oral Disease Symptoms) | PIU Group | Model I OR (95% CI) | Model II a AOR (95% CI) |
|---|---|---|---|
| Chipped or broken tooth (Yes) | General group | 1 | 1 |
| Potential group | 1.29 (1.116–1.487) | 1.03 (0.872–1.211) | |
| High risk group | 1.60 (1.392–1.829) | 1.14 (0.977–1.334) | |
| Toothache when eating | General group | 1 | 1 |
| Potential group | 1.77 (1.590–1.971) | 1.53 (1.357–1.856) | |
| High risk group | 1.88 (1.702–2.083) | 1.71 (1.523–1.923) | |
| Throbbing and sore tooth | General group | 1 | 1 |
| Potential group | 1.66 (1.48–1.875) | 1.55 (1.349–1.786) | |
| High risk group | 1.96 (1.770–2.164) | 1.71 (1.520–1.927) | |
| Sore and bleeding gums | General group | 1 | 1 |
| Potential group | 1.65 (1.466–1.853) | 1.40 (1.215–1.601) | |
| High risk group | 2.11 (1.905–2.331) | 1.63 (1.458–1.827) | |
| Pain in tongue or inside Cheeks | General group | 1 | 1 |
| Potential group | 1.72 (1.501–1.969) | 1.49 (1.265–1.756) | |
| High risk group | 2.29 (2.052–2.548) | 1.90 (1.667–2.164) | |
| Bad breath | General group | 1 | 1 |
| Potential group | 2.05 (1.838–2.290) | 1.69 (1.497–1.900) | |
| High risk group | 2.66 (2.407–2.930) | 2.05 (1.825–2.298) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Do, K.-Y.; Lee, K.-S. Relationship between Problematic Internet Use, Sleep Problems, and Oral Health in Korean Adolescents: A National Survey. Int. J. Environ. Res. Public Health 2018, 15, 1870. https://doi.org/10.3390/ijerph15091870
Do K-Y, Lee K-S. Relationship between Problematic Internet Use, Sleep Problems, and Oral Health in Korean Adolescents: A National Survey. International Journal of Environmental Research and Public Health. 2018; 15(9):1870. https://doi.org/10.3390/ijerph15091870
Chicago/Turabian StyleDo, Kyung-Yi, and Kang-Sook Lee. 2018. "Relationship between Problematic Internet Use, Sleep Problems, and Oral Health in Korean Adolescents: A National Survey" International Journal of Environmental Research and Public Health 15, no. 9: 1870. https://doi.org/10.3390/ijerph15091870
APA StyleDo, K.-Y., & Lee, K.-S. (2018). Relationship between Problematic Internet Use, Sleep Problems, and Oral Health in Korean Adolescents: A National Survey. International Journal of Environmental Research and Public Health, 15(9), 1870. https://doi.org/10.3390/ijerph15091870





