A Cluster Randomized Controlled Trial of a Total Worker Health® Intervention on Commercial Construction Sites
Abstract
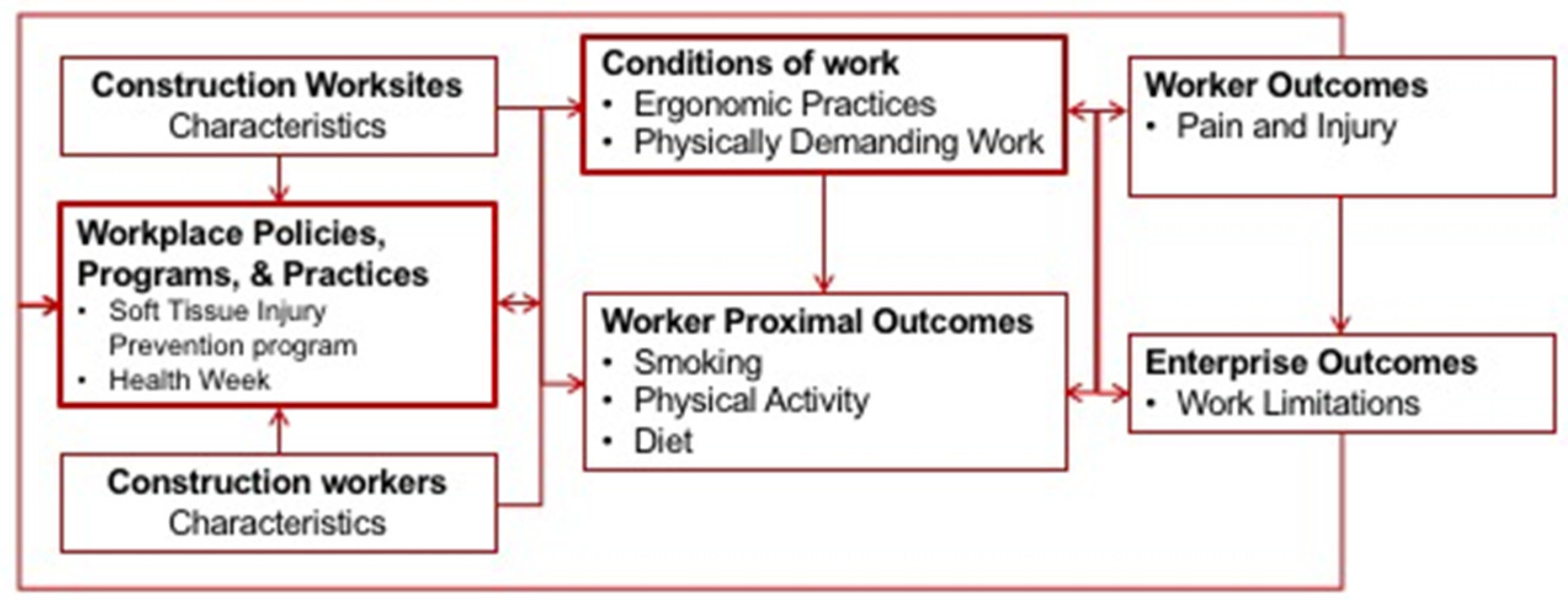
1. Introduction
2. Materials and Methods
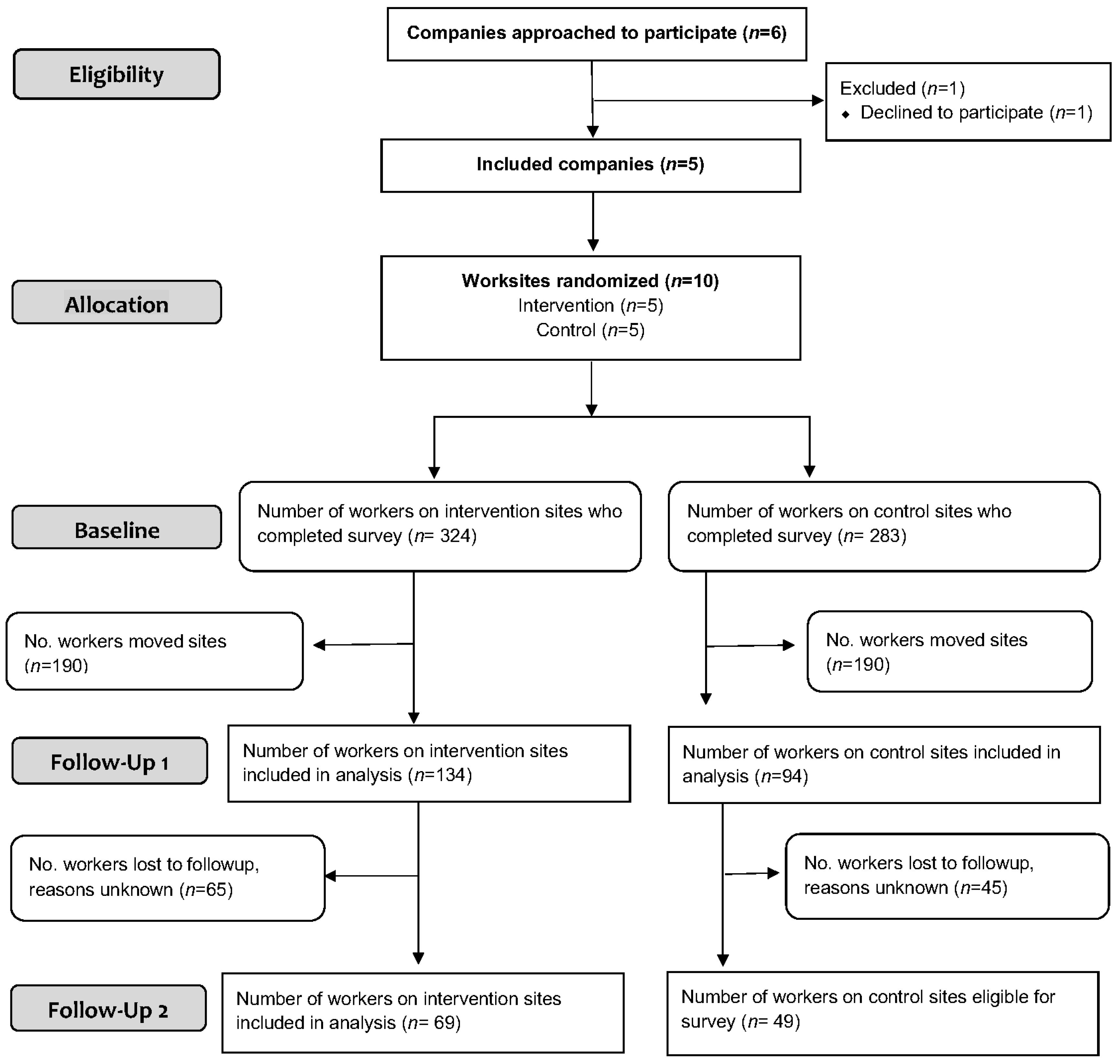
2.1. Study Design and Randomization
2.2. Recruitment and Eligibility
2.3. The “All the Right Moves” (ARM) Intervention
2.4. Control Site Activities
2.5. Worker Survey Data Collection
2.6. Primary and Secondary Outcome Measures
2.7. Other Variables Measured
2.8. Process Evaluation
2.9. Hypotheses
2.10. Data Analysis
3. Results
3.1. Study Characteristics and Response Rates
3.2. Outcomes
3.2.1. Pain and Injury
3.2.2. Physical Activity and Dietary Behaviors
3.2.3. Tobacco Use
3.2.4. Ergonomic Practices and Work Limitations
3.2.5. Sensitivity Analysis
3.3. Process Evaluation
3.3.1. Intervention Fidelity and Uptake
3.3.2. Barriers to Intervention Implementation
4. Discussion
Methodological Considerations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bush, D.M.; Lipari, R.N. The CBHSQ Report: Short Report—Substance Use and Substance Use Disorder by Industry; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2015. [Google Scholar]
- The Center for Construction Research and Training. The Construction Chart Book. The U.S. Construction Industry and Its Workers, 6th ed.; The Center for Construction Research and Training: Silver Spring, MD, USA, 2018. [Google Scholar]
- Punnett, L.; Warren, N.; Henning, R.; Nobrega, S.; Cherniack, M. CPH-NEW Research Team. Participatory ergonomics as a model for integrated programs to prevent chronic disease. J. Occup. Environ. Med. 2013, 55, S19–S24. [Google Scholar] [CrossRef] [PubMed]
- Caban-Martinez, A.J.; Lowe, K.A.; Herrick, R.; Kenwood, C.; Gagne, J.J.; Becker, J.F.; Schneider, S.P.; Dennerlein, J.T.; Sorensen, G. Construction workers working in musculoskeletal pain and engaging in leisure-time physical activity: Findings from a mixed-methods pilot study. Am. J. Ind. Med. 2014, 57, 819–825. [Google Scholar] [CrossRef] [PubMed]
- Umer, W.; Antwi-Afari, M.F.; Li, H.; Szeto, G.P.Y.; Wong, A.Y.L. The prevalence of musculoskeletal symptoms in the construction industry: A systematic review and meta-analysis. Int. Arch. Occup. Environ. Health 2018, 91, 125–144. [Google Scholar] [CrossRef] [PubMed]
- Pronk, N.P.; McLellan, D.L.; McGrail, M.P.; Olson, S.M.; McKinney, Z.J.; Katz, J.N.; Wagner, G.R.; Sorensen, G. Measurement tools for integrated worker health protection and promotion: Lessons learned from the Safewell Project. J. Occup. Environ. Med. 2016, 58, 651–658. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sorensen, G.; McLellan, D.L.; Sabbath, E.L.; Dennerlein, J.T.; Nagler, E.M.; Hurtado, D.A.; Pronk, N.P.; Wagner, G.R. Integrating worksite health protection and health promotion: A conceptual model for intervention and research. Prev. Med. 2016, 91, 188–196. [Google Scholar] [CrossRef] [PubMed]
- McLellan, D.; Moore, W.; Nagler, E.; Sorensen, G. Implementing an Integrated Approach Weaving Worker Health, Safety, and Well-being into the Fabric of Your Organization; Harvard Center for Work, Health and Wellbeing: Boston, MA, USA, 2017; pp. 1–141. [Google Scholar]
- Bureau of Labor Statistics. Nonfatal Occupational Injuries and Illnesses Requiring Days Away from Work. Available online: https://www.bls.gov/news.release/osh2.toc.htm (accessed on 1 June 2018).
- Viester, L.; Verhagen, E.; Bongers, P.M.; van der Beek, A.J. Effectiveness of a Worksite Intervention for Male Construction Workers on Dietary and Physical Activity Behaviors, Body Mass Index, and Health Outcomes: Results of a Randomized Controlled Trial. Am. J. Health Promot. 2018, 32, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Robroek, S.J.W.; Jarvholm, B.; van der Beek, A.J.; Proper, K.I.; Wahlstrom, J.; Burdorf, A. Influence of obesity and physical workload on disability benefits among construction workers followed up for 37 years. Occup. Environ. Med. 2017, 74, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Viester, L.; Verhagen, E.A.; Oude Hengel, K.M.; Koppes, L.L.; van der Beek, A.J.; Bongers, P.M. The relation between body mass index and musculoskeletal symptoms in the working population. BMC Musculoskelet. Disord. 2013, 14, 238. [Google Scholar] [CrossRef] [PubMed]
- Dietz, A.; Ramroth, H.; Urban, T.; Ahrens, W.; Becher, H. Exposure to cement dust, related occupational groups and laryngeal cancer risk: Results of a population based case-control study. Int. J. Cancer 2004, 108, 907–911. [Google Scholar] [CrossRef] [PubMed]
- Kurihara, N.; Wada, O. Silicosis and smoking strongly increase lung cancer risk in silica-exposed workers. Ind. Health 2004, 42, 303–314. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.N. Relation between exposure to asbestos and smoking jointly and the risk of lung cancer. Occup. Environ. Med. 2001, 58, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine and National Research Council. Musculoskeletal Disorders and the Workplaces: Low Back and Upper Extremities; The National Academies Press: Washington, DC, USA, 2001; pp. 1–512. ISBN 978-0-309-13200-2. [Google Scholar]
- Weil, D. The Fissured Workplace: Why Work Became So Bad for So Many and What Can Be Done to Improve it; Harvard University Press: Cambridge, MA, USA, 2014; pp. 1–424. ISBN 9780674975446. [Google Scholar]
- Sparer, E.H.; Herrick, R.F.; Dennerlein, J.T. Development of a safety communication and recognition program for construction. New Solut. 2015, 25, 42–58. [Google Scholar] [CrossRef] [PubMed]
- Breslin, F.C.; Smith, P. Trial by fire: A multivariate examination of the relation between job tenure and work injuries. Occup. Environ. Med. 2006, 63, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, G.; Barbeau, E.M. Integrating occupational health, safety and worksite health promotion: Opportunities for research and practice. Med. Lav. 2006, 97, 240–257. [Google Scholar] [PubMed]
- Magnavita, N. Obstacles and future prospects: Considerations on health promotion activities for older workers in Europe. Int. J. Environ. Res. Public Health 2018, 15, 662. [Google Scholar] [CrossRef] [PubMed]
- Bradley, C.J.; Grossman, D.C.; Hubbard, R.A.; Ortega, A.N.; Curry, S.J. integrated interventions for improving total worker health: A panel report from the national institutes of health pathways to prevention workshop: Total Worker Health-What’s work got to do with it? Ann. Intern. Med. 2016, 165, 279–283. [Google Scholar] [CrossRef] [PubMed]
- De Boer, A.G.; Burdorf, A.; van Duivenbooden, C.; Frings-Dresen, M.H. The effect of individual counselling and education on work ability and disability pension: A prospective intervention study in the construction industry. Occup. Environ. Med. 2007, 64, 792–797. [Google Scholar] [CrossRef]
- Okechukwu, C.A.; Krieger, N.; Chen, J.; Sorensen, G.; Li, Y.; Barbeau, E.M. The association of workplace hazards and smoking in a U.S. multiethnic working-class population. Public Health Rep. 2010, 125, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Oude Hengel, K.M.; Blatter, B.M.; Joling, C.I.; van der Beek, A.J.; Bongers, P.M. Effectiveness of an intervention at construction worksites on work engagement, social support, physical workload, and need for recovery: Results from a cluster randomized controlled trial. BMC Public Health 2012, 12, 1008. [Google Scholar] [CrossRef] [PubMed]
- Okechukwu, C.A.; Krieger, N.; Sorensen, G.; Li, Y.; Barbeau, E.M. MassBuilt: Effectiveness of an apprenticeship site-based smoking cessation intervention for unionized building trades workers. Cancer Cause. Control 2009, 20, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Saarela, K.L. A poster campaign for improving safety on shipyard scaffolds. J. Saf. Res. 1989, 20, 177–185. [Google Scholar] [CrossRef]
- Van der Molen, H.F.; Basnet, P.; Hoonakker, P.L.; Lehtola, M.M.; Lappalainen, J.; Frings-Dresen, M.H.; Haslam, R.; Verbeek, J.H. Interventions to prevent injuries in construction workers. Cochrane Database Syst. Rev. 2018, 2, CD006251. [Google Scholar] [CrossRef] [PubMed]
- Bena, A.; Berchialla, P.; Coffano, M.E.; Debernardi, M.L.; Icardi, L.G. Effectiveness of the training program for workers at construction sites of the high-speed railway line between Torino and Novara: Impact on injury rates. Am. J. Ind. Med. 2009, 52, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Caban-Martinez, A.J.; Moore, K.J.; Clarke, T.C.; Davila, E.P.; Clark, J.D.; Lee, D.J.; Fleming, L.E. Health Promotion at the Construction Work Site: The Lunch Truck Pilot Study. Workplace Health Saf. 2018. [Google Scholar] [CrossRef] [PubMed]
- Lingard, H.; Rowlinson, S. Behavior-based safety management in Hong Kong’s construction industry. J. Saf. Res. 1997, 28, 243–256. [Google Scholar] [CrossRef]
- Wickizer, T.M.; Kopjar, B.; Franklin, G.; Joesch, J. Do drug-free workplace programs prevent occupational injuries? Evidence from Washington State. Health Serv. Res. 2004, 39, 91–110. [Google Scholar] [CrossRef] [PubMed]
- Van der Molen, H.F.; Sluiter, J.K.; Hulshof, C.T.; Vink, P.; van Duivenbooden, C.; Holman, R.; Frings-Dresen, M.H. Implementation of participatory ergonomics intervention in construction companies. Scand. J. Work Environ. Health 2005, 31, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Hess, J.A.; Hecker, S.; Weinstein, M.; Lunger, M. A participatory ergonomics intervention to reduce risk factors for low-back disorders in concrete laborers. Appl. Ergon. 2004, 35, 427–441. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, G.; McLellan, D.; Dennerlein, J.T.; Pronk, N.P.; Allen, J.D.; Boden, L.I.; Okechukwu, C.A.; Hashimoto, D.; Stoddard, A.; Wagner, G.R. Integration of health protection and health promotion: Rationale, indicators, and metrics. J. Occup. Environ. Med. 2013, 55, S12–S18. [Google Scholar] [CrossRef] [PubMed]
- Sparer, E.H.; Catalano, P.J.; Herrick, R.F.; Dennerlein, J.T. Improving safety climate through a communication and recognition program for construction: A mixed methods study. Scand. J. Work Environ. Health 2016, 42, 329–337. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sparer, E.H.; Okechukwu, C.A.; Manjourides, J.; Herrick, R.F.; Katz, J.N.; Dennerlein, J.T. Length of time spent working on a commercial construction site and the associations with worker characteristics. Am. J. Ind. Med. 2015, 58, 964–973. [Google Scholar] [CrossRef] [PubMed]
- American National Standards Institute. ANSI Essential Requirements: Due Process Requirements for American National Standards; American National Standards Institute: New York, NY, USA, 2012; pp. 1–27. [Google Scholar]
- The National Institute for Occupational Safety and Health. Simple Solutions: Ergonomics for Construction Workers. DHHS (NIOSH) Publication No. 2007-122. Available online: https://www.cdc.gov/niosh/docs/2007-122/default.html (accessed on 1 June 2018).
- Oude Hengel, K.M.; Joling, C.I.; Proper, K.I.; Blatter, B.M.; Bongers, P.M. A worksite prevention program for construction workers: Design of a randomized controlled trial. BMC Public Health 2010, 10, 336. [Google Scholar] [CrossRef] [PubMed]
- Viester, L.; Verhagen, E.A.; Proper, K.I.; van Dongen, J.M.; Bongers, P.M.; van der Beek, A.J. VIP in construction: Systematic development and evaluation of a multifaceted health programme aiming to improve physical activity levels and dietary patterns among construction workers. BMC Public Health 2012, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sorensen, F.; Andersson, G.; Jorgensen, K. Standardized Nordic Questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Harley, A.E.; Yang, M.; Stoddard, A.M.; Adamkiewicz, G.; Walker, R.; Tucker-Seeley, R.D.; Allen, J.D.; Sorensen, G. Patterns and Predictors of Health Behaviors Among Racially/Ethnically Diverse Residents of Low-Income Housing Developments. Am. J. Health Promot. 2014, 29, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.J.; Velicer, W.F.; Nigg, C.R.; Prochaska, J.O. Methods of quantifying change in multiple risk factor interventions. Prev. Med. 2008, 46, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Pierannunzi, C.; Hu, S.S.; Balluz, L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med. Res. Methodol. 2013, 13, 49. [Google Scholar] [CrossRef] [PubMed]
- Cigarette Smoking among Adults—United States, 1992, and Changes in the Definition of Current Cigarette Smoking. MMWR. Morb. Mortal. Wkly. Rep. 1994, 43, 342. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00033250.htm (accessed on 1 June 2018).
- Amick, B.C.; Habeck, R.V.; Hunt, A.; Fossel, A.H.; Chapin, A.; Keller, R.B.; Katz, J.N. Measuring the impact of organizational behaviors on work disability prevention and management. J. Occup. Rehabil. 2000, 10, 21–38. [Google Scholar] [CrossRef]
- Lerner, D.; Amick, B.C.; Rogers, W.H.; Malspeis, S.; Bungay, K.; Cynn, D. The Work Limitations Questionnaire. Med. Care 2001, 39, 72–85. [Google Scholar] [CrossRef] [PubMed]
- Marras, W.S.; Lavender, S.A.; Leurgans, S.E.; Fathallah, F.A.; Ferguson, S.A.; Allread, W.G.; Rajulu, S.L. Biomechanical risk factors for occupationally related low back disorders. Ergonomics 1995, 38, 377–410. [Google Scholar] [CrossRef] [PubMed]
- Tveito, T.H.; Shaw, W.S.; Huang, Y.H.; Nicholas, M.; Wagner, G. Managing pain in the workplace: A focus group study of challenges, strategies and what matters most to workers with low back pain. Disabil. Rehabil. 2010, 32, 2035–2045. [Google Scholar] [CrossRef] [PubMed]
- Dennerlein, J.T. Chronic low back pain: A successful intervention for desk-bound workers. Occup. Environ. Med. 2018, 75, 319–320. [Google Scholar] [CrossRef] [PubMed]
- Harvard Business Review. 7 Ways to Improve Operations without Sacrificing Worker Safety by David Michaels. Available online: https://hbr.org/2018/03/7-ways-to-improve-operations-without-sacrificing-worker-safety (accessed on 21 March 2018).
- Dasgupta, P.; Sample, M.; Buchholz, B.; Brunette, M. Is worker involvement an ergonomic solution for construction intervention challenges: A systematic review. Theory Issues Ergon. Sci. 2017, 18, 433–441. [Google Scholar] [CrossRef]
- Dale, A.M.; Jaegers, L.; Welch, L.; Barnidge, E.; Weaver, N.; Evanoff, B.A. Facilitators and barriers to the adoption of ergonomic solutions in construction. Am. J. Ind. Med. 2017, 60, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Occupational Safety and Health Administration. Training Requirements in OSHA Standards. OSHA 2254-09R 2015. Available online: https://www.osha.gov/Publications/osha2254.pdf (accessed on 1 June 2018).
- Boschman, J.S.; Frings-Dresen, M.H.W.; van der Molen, H.F. Use of Ergonomic Measures Related to Musculoskeletal Complaints among Construction Workers: A 2-year Follow-up Study. Saf. Health Work 2015, 6, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Visser, S.; van der Molen, H.F.; Sluiter, J.K.; Frings-Dresen, M.H.W. The process evaluation of two alternative participatory ergonomics intervention strategies for construction companies. Ergonomics 2018, 61, 1156–1172. [Google Scholar] [CrossRef] [PubMed]
- Dale, A.M.; Jaegers, L.; Welch, L.; Gardner, B.T.; Buchholz, B.; Weaver, N.; Evanoff, B.A. Evaluation of a participatory ergonomics intervention in small commercial construction firms. Am. J. Ind. Med. 2016, 59, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Dennerlein, J.T.; O’Day, E.T.; Mulloy, D.F.; Somerville, J.; Stoddard, A.M.; Kenwood, C.; Teeple, E.; Boden, L.I.; Sorensen, G.; Hashimoto, D. Lifting and exertion injuries decrease after implementation of an integrated hospital-wide safe patient handling and mobilisation programme. Occup. Environ. Med. 2017, 74, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, G.; Sparer, E.; Williams, J.A.R.; Gundersen, D.; Boden, L.I.; Dennerlein, J.T.; Hashimoto, D.; Katz, J.N.; McLellan, D.L.; Okechukwu, C.A.; et al. Measuring best practices for workplace safety, health and wellbeing: The Workplace Integrated Safety and Health assessment. J. Occup. Environ. Med. 2018, 60, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Viester, L.; Verhagen, E.A.; Bongers, P.M.; van der Beek, A.J. The effect of a health promotion intervention for construction workers on work-related outcomes: Results from a randomized controlled trial. Int. Arch. Occup. Environ. Health 2015, 88, 789–798. [Google Scholar] [CrossRef] [PubMed]
- Manjourides, J.; Sparer, E.H.; Okechukwu, C.A.; Dennerlein, J.T. The Effect of Workforce Mobility on Intervention Effectiveness Estimates. Ann. Work Expo. Health 2018, 62, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N. Medical surveillance, continuous health promotion and a participatory intervention in a small company. Int. J. Environ. Res. Public Health 2018, 15, 662. [Google Scholar] [CrossRef] [PubMed]
- Sokas, R.K.; Jorgensen, E.; Nickels, L.; Gao, W.; Gittleman, J.L. An intervention effectiveness study of hazard awareness training in the construction building trades. Public Health Rep. 2009, 124, 160–168. [Google Scholar] [CrossRef] [PubMed]
- The Center for Construction Research and Training. Diffusing Ergonomic Innovations in Construction (Completed—2004–2009). Available online: http://orcehs.org/wiki/display/orcehs/Construction+Ergonomics (accessed on 31 October 2010).
- Strickland, J.R.; Smock, N.; Casey, C.; Poor, T.; Kreuter, M.W.; Evanoff, B.A. Development of targeted messages to promote smoking cessation among construction trade workers. Health Educ. Res. 2015, 30, 107–120. [Google Scholar] [CrossRef] [PubMed]
- Dale, A.M.; Strand, J.; Schneider, S.; Cain, C.; Rempel, D. Piloting of a social marketing campaign to reduce musculoskeletal risks related to manual materials handling on construction projects. Occup. Environ. Med. 2018, 75. [Google Scholar] [CrossRef]
- Rempel, D.; Star, D.; Barr, A.; Janowitz, I. Overhead drilling: Comparing three bases for aligning a drilling jig to vertical. J. Saf. Res. 2010, 41, 247–251. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Total (N = 607) | Control (n = 283) | Intervention (n = 324) | Test of Equivalence, p-Value | ||||
|---|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | N | Mean (SD) | ||
| Age | 586 | 40.42 (10.78) | 40.28 (11.05) | 40.55 (10.55) | 0.7643 | ||
| N | n (%) | N | n (%) | N | n (%) | ||
| Gender | 592 | 275 | 317 | 0.0736 | |||
| Male | 573 (97%) | 270 (98%) | 303 (96%) | ||||
| Female | 19 (3%) | 5 (2%) | 14 (4%) | ||||
| Race/Ethnicity | 595 | 244 | 351 | 0.7883 | |||
| White | 457 (77%) | 214 (77%) | 243 (77%) | ||||
| Black/AA | 57 (10%) | 24 (9%) | 33 (11%) | ||||
| Latino/Hispanic | 35 (6%) | 16 (6%) | 19 (6%) | ||||
| Other | 46 (8%) | 24 (9%) | 22 (7%) | ||||
| Education | 587 | 274 | 313 | 0.5762 | |||
| <H.S. | 33 (6%) | 17 (6%) | 16 (5%) | ||||
| H.S./G.E.D. | 317 (54%) | 151 (55%) | 166 (53%) | ||||
| Some college | 194 (33%) | 90 (33%) | 104 (33%) | ||||
| College graduate | 43 (7%) | 16 (6%) | 27 (9%) | ||||
| Title | 554 | 256 | 298 | 0.3400 | |||
| Apprentice | 104 (19%) | 40 (16%) | 64 (22%) | ||||
| Journeyman | 330 (59%) | 156 (61%) | 174 (58%) | ||||
| Foreman | 100 (18%) | 50 (19%) | 50 (17%) | ||||
| Supervisor | 20 (4%) | 10 (4%) | 10 (3%) | ||||
| Trade | 499 | 226 | 273 | 0.1643 | |||
| Finishing | 59 (12%) | 25 (11%) | 34 (12%) | ||||
| Mechanical | 366 (73%) | 168 (74%) | 198 (73%) | ||||
| Laborers | 30 (6%) | 18 (8%) | 12 (4%) | ||||
| Ironworkers | 44 (9%) | 15 (7%) | 29 (11%) | ||||
| Outcome Variable | Control | Treatment | ||||
|---|---|---|---|---|---|---|
| Baseline (N = 283) | FU1 (N = 94) | FU2 (N = 49) | Baseline (N = 324) | FU1 (N = 134) | FU2 (N = 69) | |
| Worker Outcomes | ||||||
| n (%)[N] | n (%)[N] | n (%)[N] | n (%)[N] | n (%)[N] | n (%)[N] | |
| New pain or injury 2 | 83 (30.0%)[277] | 20 (21.5%)[93] | 15 (31.3%)[48] | 115 (36.4%)[316] | 27 (20.6%)[131] | 15 (21.7%)[69] |
| Pain interfering with work | 197 (69.9%)[282] | 54 (57.5%)[94] | 37 (75.5%)[49] | 234 (72.4%)[323] | 78 (58.2%)[134] | 48 (69.6%)[69] |
| Current Smoker | 82 (30.4%)[269] | 12 (24.5%)[49] | 99 (33.9%)[292] | 18 (26.1%)[69] | ||
| Mean (SD)[N] | Mean (SD)[N] | Mean (SD)[N] | Mean (SD)[N] | Mean (SD)[N] | Mean (SD)[N] | |
| Physical activity | 76.57 (76.70)[229] | 67.69 (95.55)[45] | 67.76 (61.95)[270] | 69.04 (93.66)[66] | ||
| Healthy diet | 5.60 (2.32)[276] | 5.42 (1.67)[48] | 5.62 (2.24)[318] | 5.48 (2.01)[69] | ||
| Unhealthy diet | 2.05 (1.21)[274] | 2.12 (1.37)[47] | 2.25 (1.31)[317] | 1.76 (1.15)[69] | ||
| Diet balance | 3.57 (2.48)[274] | 3.24 (1.92)[47] | 3.36 (2.46)[317] | 3.72 (2.25)[69] | ||
| Enterprise Outcomes | ||||||
| Work limitations | 1.51 (0.64)[277] | 1.39 (0.57)[91] | 1.27 (0.41)[49] | 1.53 (0.67)[321] | 1.46 (0.62)[128] | 1.27 (0.54)[68] |
| Conditions of Work | ||||||
| n (%)[N] | n (%)[N] | n (%)[N] | n (%)[N] | n (%)[N] | n (%)[N] | |
| Demanding Work 1,3 | 213 (79.3%)[269] | 43 (47.3%)[91] | 30 (61.2%)[49] | 206 (66.9%)[308] | 60 (46.2%)[130] | 31 (45.6%)[68] |
| Mean (SD)[N] | Mean (SD)[N] | Mean (SD)[N] | Mean (SD)[N] | Mean (SD)[N] | Mean (SD)[N] | |
| Ergonomic practices | 3.89 (0.67)[276] | 3.69 (0.78)[93] | 3.8 (0.62)[313] | 3.68 (0.80)[132] | ||
| Outcome Variable | Unadjusted | Adjusted 1 | ||||
|---|---|---|---|---|---|---|
| N | OR (95% CI) | p-Value | N | OR (95% CI) | p-Value | |
| FU1 (1 month) | ||||||
| New pain or injury 2 | 216 | 1.01 (0.49, 2.07) | 0.982 | 208 | 0.58 (0.39, 0.86) | 0.012 ** |
| Pain in last 3 months | 228 | 1.03 (0.65, 1.63) | 0.884 | 219 | 0.85 (0.63, 1.15) | 0.252 |
| FU2 (6 months) | ||||||
| New pain or injury 2 | 115 | 0.48 (0.13, 1.73) | 0.227 | 112 | 0.60 (0.24, 1.49) | 0.236 |
| Pain in last 3 months | 116 | 0.74 (0.32, 1.69) | 0.429 | 116 | 0.85 (0.37, 1.99) | 0.683 |
| Outcome Variable | Unadjusted | Adjusted 1 | ||||
|---|---|---|---|---|---|---|
| N | B (95% CI) | p-Value | N | B (95% CI) | p-Value | |
| Recreational physical activity | 97 | 12.54 (−24.42, 49.51) | 0.462 | 84 | 35.20 (5.35, 65.04) | 0.026 ** |
| Dietary balance | 116 | 0.83 (−0.62, 2.28) | 0.229 | 100 | 1.05 (−0.02, 2.13) | 0.054 * |
| Healthy diet | 118 | 0.63 (0.33, 1.59) | 0.173 | 101 | 0.63 (−0.17, 1.43) | 0.008 ** |
| Unhealthy diet | 116 | −0.07 (−1.11, 0.99) | 0.89 | 100 | −0.12 (−0.81, 0.56) | 0.691 |
| Outcome Variable | Unadjusted | Adjusted 1 | ||||
|---|---|---|---|---|---|---|
| N | B (95% CI) | p-Value | N | B (95% CI) | p-Value | |
| FU1 (1 month) | ||||||
| Ergonomic practices | 182 | 0.00 (−0.21, 0.20) | 0.953 | 182 | 0.20 (0.09, 0.31) | 0.002 ** |
| Physically demanding work | 208 | 0.17 (−0.05, 0.37) | 0.121 | 174 | 0.17 (−0.06, 0.40) | 0.129 |
| Work limitations (8-item) | 216 | 0.11 (−0.08, 0.30) | 0.225 | 179 | 0.09 (−0.06, 0.24) | 0.212 |
| FU2 (6 months) | ||||||
| Physically demanding work | 114 | −0.14 (−0.51, 0.23) | 0.407 | 100 | −0.25 (−0.41, −0.08) | 0.008 ** |
| Work limitations (8-item) | 119 | 0.02 (−0.08, 0.13) | 0.641 | 102 | 0.04 (−0.07, 0.15) | 0.432 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peters, S.E.; Grant, M.P.; Rodgers, J.; Manjourides, J.; Okechukwu, C.A.; Dennerlein, J.T. A Cluster Randomized Controlled Trial of a Total Worker Health® Intervention on Commercial Construction Sites. Int. J. Environ. Res. Public Health 2018, 15, 2354. https://doi.org/10.3390/ijerph15112354
Peters SE, Grant MP, Rodgers J, Manjourides J, Okechukwu CA, Dennerlein JT. A Cluster Randomized Controlled Trial of a Total Worker Health® Intervention on Commercial Construction Sites. International Journal of Environmental Research and Public Health. 2018; 15(11):2354. https://doi.org/10.3390/ijerph15112354
Chicago/Turabian StylePeters, Susan E., Michael P. Grant, Justin Rodgers, Justin Manjourides, Cassandra A. Okechukwu, and Jack T. Dennerlein. 2018. "A Cluster Randomized Controlled Trial of a Total Worker Health® Intervention on Commercial Construction Sites" International Journal of Environmental Research and Public Health 15, no. 11: 2354. https://doi.org/10.3390/ijerph15112354
APA StylePeters, S. E., Grant, M. P., Rodgers, J., Manjourides, J., Okechukwu, C. A., & Dennerlein, J. T. (2018). A Cluster Randomized Controlled Trial of a Total Worker Health® Intervention on Commercial Construction Sites. International Journal of Environmental Research and Public Health, 15(11), 2354. https://doi.org/10.3390/ijerph15112354





