Association of Elevated Body Mass Index with Tibial Tuberosity Avulsion Fractures in Pediatric Athletes: A Pilot Retrospective Study
Abstract
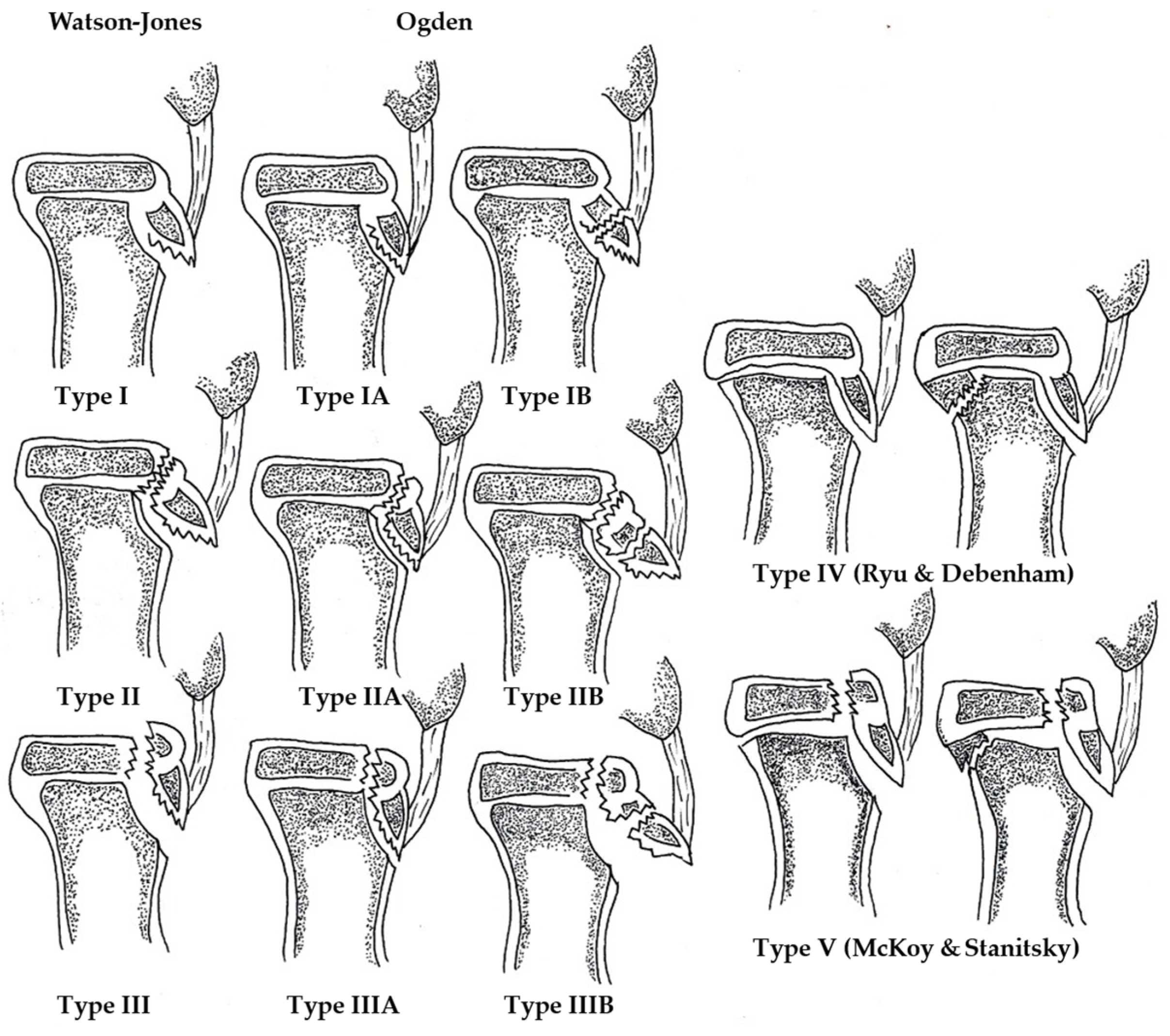
1. Introduction
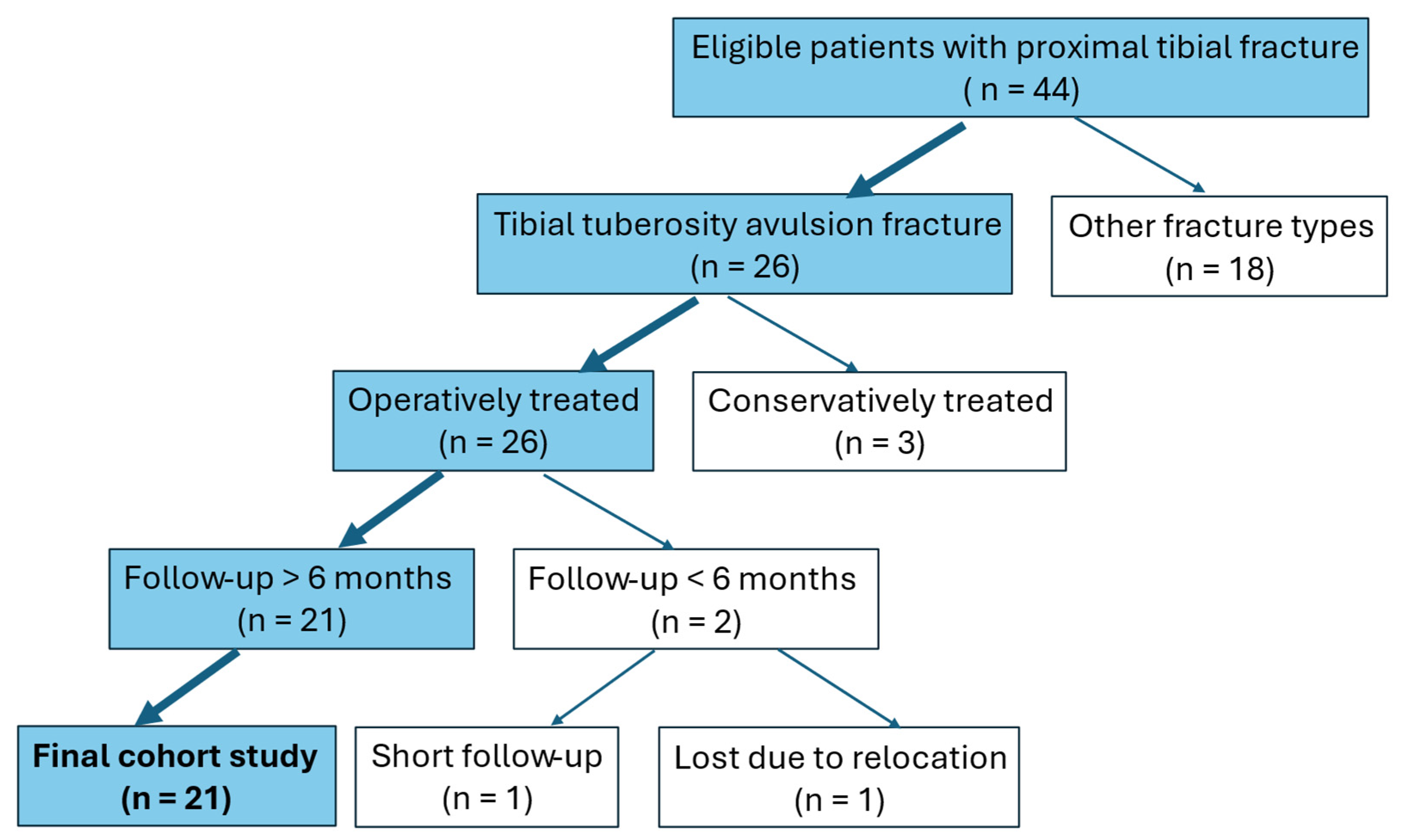
2. Materials and Methods
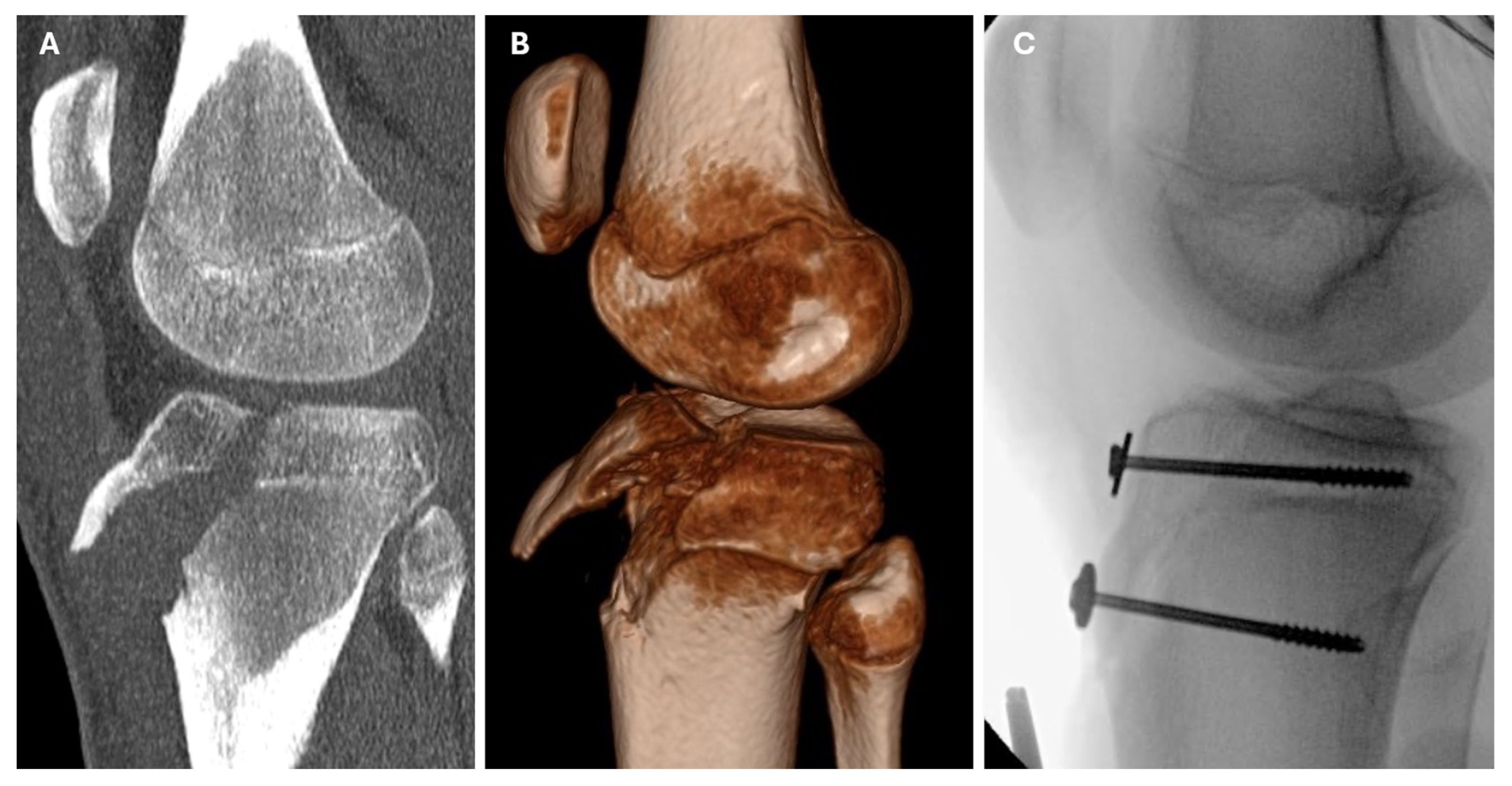
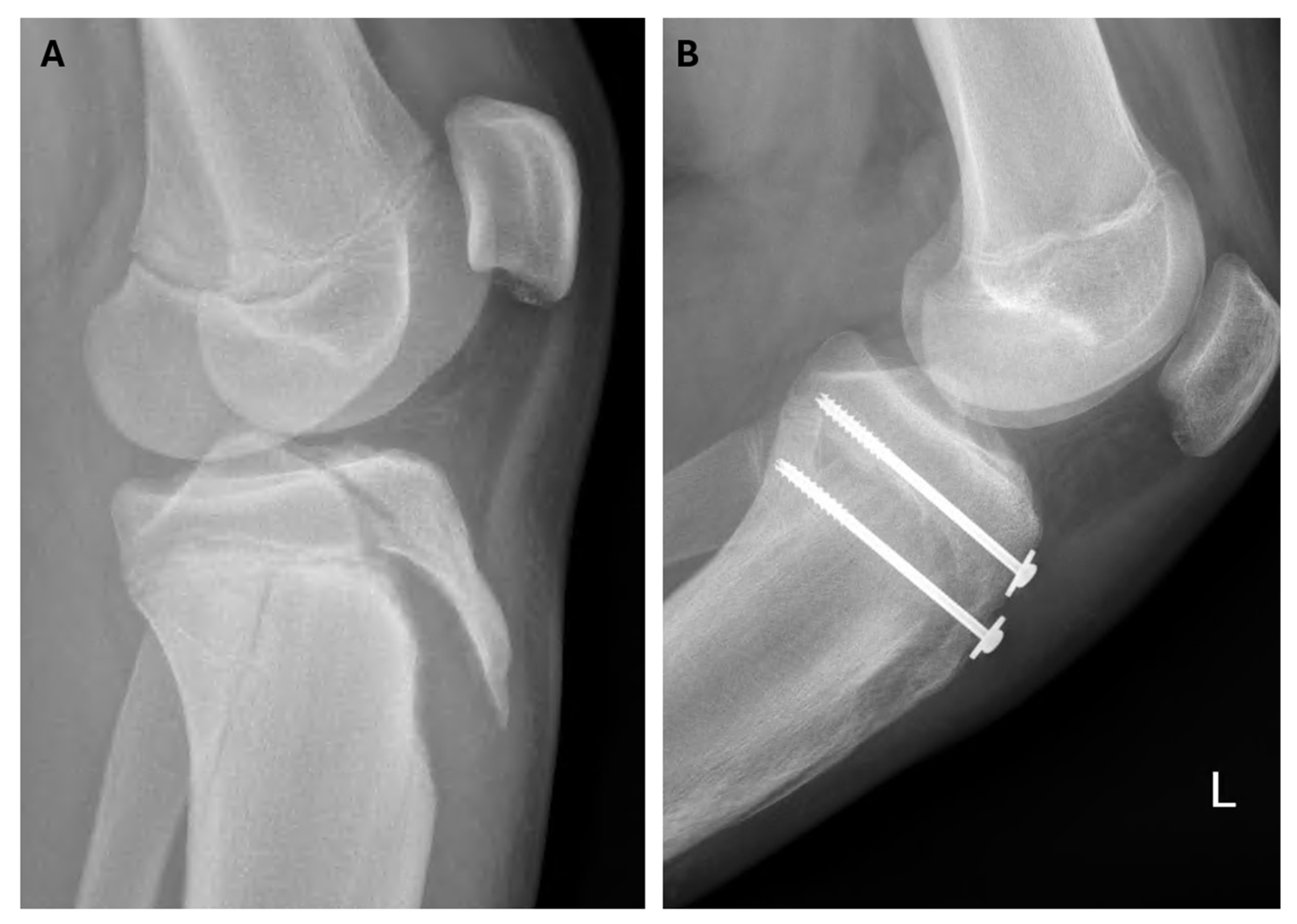
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| CDC | Centers for Disease Control and Prevention |
| CRIF | Closed Reduction and Internal Fixation |
| CT | Computed Tomography |
| IQR | Interquartile Range |
| MRI | Magnetic Resonance Imaging |
| ORIF | Open Reduction and Internal Fixation |
References
- Brey, J.M.; Conoley, J.; Canale, S.T.; Beaty, J.H.; Warner, W.C., Jr.; Kelly, D.M.; Sawyer, J.R. Tibial tuberosity fractures in adolescents: Is a posterior metaphyseal fracture component a predictor of complications? J. Pediatr. Orthop. 2012, 32, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Bolesta, M.J.; Fitch, R.D. Tibial tubercle avulsions. J. Pediatr. Orthop. 1986, 6, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Haber, D.B.; Tepolt, F.A.; McClincy, M.P.; Hussain, Z.B.; Kalish, L.A.; Kocher, M.S. Tibial tubercle fractures in children and adolescents: A large retrospective case series. J. Pediatr. Orthop. B 2021, 30, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Pretell-Mazzini, J.; Kelly, D.M.; Sawyer, J.R.; Esteban, E.M.; Spence, D.D.; Warner, W.C., Jr.; Beaty, J.H. Outcomes and Complications of Tibial Tubercle Fractures in Pediatric Patients: A Systematic Review of the Literature. J. Pediatr. Orthop. 2016, 36, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Frey, S.; Hosalkar, H.; Cameron, D.B.; Heath, A.; David Horn, B.; Ganley, T.J. Tibial tuberosity fractures in adolescents. J. Child. Orthop. 2008, 2, 469–474. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Reyes, C.D.; Wu, W.; Pandya, N.K. Adolescent Tibial Tubercle Fracture: Review of Outcomes and Complications. Curr. Rev. Musculoskelet. Med. 2023, 16, 392–397. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hamilton, S.W.; Gibson, P.H. Simultaneous bilateral avulsion fractures of the tibial tuberosity in adolescence: A case report and review of over 50 years of literature. Knee 2006, 13, 404–407. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, I.; Sepúlveda, M.; Birrer, E.; Tuca, M.J. Fracture of the anterior tibial tuberosity in children. EFORT Open Rev. 2020, 5, 260–267. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jakoi, A.; Freidl, M.; Old, A.; Javandel, M.; Tom, J.; Realyvasquez, J. Tibial tubercle avulsion fractures in adolescent basketball players. Orthopedics 2012, 35, 692–696. [Google Scholar] [CrossRef] [PubMed]
- Watson-Jones, R. Fractures and Joint Injuries; Lippincott Williams & Wilkins: Baltimore, MD, USA, 1955. [Google Scholar]
- Ogden, J.A.; Tross, R.B.; Murphy, M.J. Fractures of the tibial tuberosity in adolescents. J. Bone Jt. Surg. Am. 1980, 62, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Ryu, R.K.; Debenham, J.O. An unusual avulsion fracture of the proximal tibial epiphysis: Case report and proposed addition to the Watson-Jones classification. Clin. Orthop. Relat. Res. 1985, 194, 181–184. [Google Scholar]
- Frankl, U.; Wasilewski, S.A.; Healy, W.L. Avulsion fracture of the tibial tubercle with avulsion of the patellar ligament. Report of two cases. J. Bone Joint Surg. Am. 1990, 72, 1411–1413. [Google Scholar] [CrossRef] [PubMed]
- McKoy, B.E.; Stanitski, C.L. Acute tibial tubercle avulsion fractures. Orthop. Clin. N. Am. 2003, 34, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Pandya, N.K.; Edmonds, E.W.; Roocroft, J.H.; Mubarak, S.J. Tibial tubercle fractures: Complications, classification, and the need for intra-articular assessment. J. Pediatr. Orthop. 2012, 32, 749–759. [Google Scholar] [CrossRef]
- CDC BMI Percentile Calculator for Children and Teens. Centers for Disease Control and Prevention. 2023. Available online: https://www.cdc.gov/bmi/child-teen-calculator/widget.html (accessed on 24 January 2025).
- Hrvatski Zavod za Javno Zdravstvo. Hrvatski Zdravstveno-Statistički Ljetopis za 2023. Zagreb: HZJZ. 2024. Available online: https://www.hzjz.hr/hrvatski-zdravstveno-statisticki-ljetopis/hrvatski-zdravstveno-statisticki-ljetopis-za-2023-g-tablicni-podaci/ (accessed on 27 August 2025).
- Matana, A.; Krajinović, H. Prevalence of Overweight and Obesity and Association with Risk Factors in Secondary School Children in Croatia. Children 2024, 11, 1464. [Google Scholar] [CrossRef]
- Formiconi, F.; D’Amato, R.D.; Voto, A.; Panuccio, E.; Memeo, A. Outcomes of surgical treatment of the tibial tuberosity fractures in skeletally immature patients: An update. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 789–798. [Google Scholar] [CrossRef] [PubMed]
- Cole, W.W., 3rd; Brown, S.M.; Vopat, B.; Heard, W.M.R.; Mulcahey, M.K. Epidemiology, Diagnosis, and Management of Tibial Tubercle Avulsion Fractures in Adolescents. JBJS Rev. 2020, 8, e0186. [Google Scholar] [CrossRef] [PubMed]
- Mubarak, S.J.; Kim, J.R.; Edmonds, E.W.; Pring, M.E.; Bastrom, T.P. Classification of proximal tibial fractures in children. J. Child. Orthop. 2009, 3, 191–197. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ares, O.; Seijas, R.; Cugat, R.; Alvarez, P.; Aguirre, M.; Catala, J. Treatment of fractures of the tibial tuberosity in adolescent soccer players. Acta Orthop. Belg. 2011, 77, 78–82. [Google Scholar]
- Nikander, R.; Kannus, P.; Rantalainen, T.; Uusi-Rasi, K.; Heinonen, A.; Sievänen, H. Cross-sectional geometry of weight-bearing tibia in female athletes subjected to different exercise loadings. Osteoporos. Int. 2010, 21, 1687–1694. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, T.J.; Rice, H.M.; Greeves, J.P. Biomechanical Basis of Predicting and Preventing Lower Limb Stress Fractures During Arduous Training. Curr. Osteoporos. Rep. 2021, 19, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Barros, W.M.A.; da Silva, K.G.; Silva, R.K.P.; Souza, A.P.D.S.; da Silva, A.B.J.; Silva, M.R.M.; Fernandes, M.S.S.; de Souza, S.L.; Souza, V.O.N. Effects of Overweight/Obesity on Motor Performance in Children: A Systematic Review. Front. Endocrinol. 2022, 12, 759165. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rodin, U.; Cerovecki, I.; Jezdic, D. Demographic Trends in Croatia in 2023. Hrvatski Zavod za Javno Zdravstvo. 2024. Available online: https://www.hzjz.hr/wp-content/uploads/2024/10/HZJZ_-_prirodno_kretanje_2023._g..pdf (accessed on 24 January 2025).
- Musić Milanović, S.; Lang Morović, M.; Križan, H. European Childhood Obesity Initiative. Croatia 2018/2019 (CroCOSI); Croatian Institute of Public Health: Zagreb, Croatia, 2021. [Google Scholar]
- Checa Betegón, P.; Arvinius, C.; Cabadas González, M.I.; Martínez García, A.; Del Pozo Martín, R.; Marco Martínez, F. Management of pediatric tibial tubercle fractures: Is surgical treatment really necessary? Eur. J. Orthop. Surg. Traumatol. 2019, 29, 1073–1079. [Google Scholar] [CrossRef] [PubMed]

| Patient | Sex | Age | Side | Osgood–Schlatter Disease | BMI (kg/m2) | BMI Percentile |
|---|---|---|---|---|---|---|
| 1 | M | 16 | R | - | 24.8 | 87.1 |
| 2 | M | 12 | L | - | 18.0 | 44.3 |
| 3 | M | 14 | L | - | 32.7 | 98.9 |
| 4 | M | 13 | L | - | 24.8 | 93.2 |
| 5 | M | 13 | L | - | 27.2 | 96.8 |
| 6 | M | 15 | L | - | 23.2 | 80 |
| 7 | M | 14 | R | - | 33.3 | 98.6 |
| 8 | F | 6 | L | - | 18.4 | 92.7 |
| 9 | M | 13 | L | Yes | 20.3 | 72 |
| 10 | M | 14 | L | - | 18.3 | 26 |
| 11 | M | 12 | R | - | 23.8 | 92.5 |
| 12 | M | 16 | L | - | 20.1 | 40.5 |
| 13 | M | 15 | L | - | 33.8 | 99.1 |
| 14 | M | 14 | L | - | 20.8 | 67.4 |
| 15 | M | 14 | L | Yes | 19.3 | 46.6 |
| 16 | M | 13 | L | - | 25.8 | 95.8 |
| 17 | M | 14 | L | - | 21.1 | 69.1 |
| 18 | M | 15 | L | - | 20.8 | 60.1 |
| 19 | M | 16 | L | - | 24.9 | 87.8 |
| 20 | M | 16 | R | - | 20.3 | 44.2 |
| 21 | M | 13 | R | - | 32.4 | 98 |
| Patient Number | Sport Causing Injury | Additional Imaging | Modified Ogden Classification | Treatment Method | Fixation Type | Associated Injuries | Complications | Follow-Up (Months) |
|---|---|---|---|---|---|---|---|---|
| 1 | Soccer | MRI, CT | Ib | ORIF | screws | patellar ligament | wound dehiscence | 10.8 |
| 2 | Athletics | - | IVb | ORIF | K wires | patellar ligament, tibialis anterior muscle | - | 10.0 |
| 3 | Soccer | - | IIIa | ORIF | screws | patellar ligament | - | 6.8 |
| 4 | Soccer | - | IIIb | ORIF | screws | - | - | 11.6 |
| 5 | Handball | CT | IIIb | ORIF | screws | quadriceps tendon | intra-articular screw prominence | 10.7 |
| 6 | Running | - | IIIa | ORIF | screws | patellar ligament | - | 8.7 |
| 7 | Running | CT | IIIa | ORIF | screws | retinacula | - | 18.7 |
| 8 | Athletics | CT | IVa | CRIF | K wires | - | - | 18.4 |
| 9 | Soccer | CT | IVb | ORIF | screws | patellar ligament | - | 7.8 |
| 10 | Soccer | - | IIIb | ORIF | screws | patellar ligament | - | 9.2 |
| 11 | Athletics | CT | Ib | ORIF | screws | - | - | 8.5 |
| 12 | Basketball | CT | IVb | ORIF | screws | retinacula, patellar luxation, fibular head fracture | - | 7.3 |
| 13 | Athletics | - | IVb | CRIF | screws | - | - | 29.9 |
| 14 | Soccer | CT | IIIa | ORIF | screws | quadriceps tendon | - | 7.4 |
| 15 | Soccer | CT | IIb | ORIF | screws | patellar ligament | - | 10.0 |
| 16 | Soccer | - | IVb | ORIF | screws | - | - | 10.2 |
| 17 | Running | CT | IVb | ORIF | screws | patellar ligament | - | 7.2 |
| 18 | Soccer | CT | IIIa | ORIF | screws | patellar ligament | - | 9.7 |
| 19 | Basketball | - | IVb | ORIF | screws | fibular head fracture, skin avulsion | superficial skin infection | 7.9 |
| 20 | Soccer | CT | IVb | ORIF | screws | retinacula | - | 7.2 |
| 21 | Soccer | CT | V | ORIF | screws | patellar ligament | - | 7.6 |
| Variable | Me (IQR) | Min–Max | Me (IQR) | p ** | Hodges–Lehmann Median Difference | |
|---|---|---|---|---|---|---|
| Total | Normal <85th Percentile | Overweight ≥85th Percentile | 95%CI | |||
| Height percentile | 88.6 (74.7 to 98.0) | 25.0 to 99.9 | 85.9 (67.5 to 91.8) | 89.3 (77.3 to 98.9) | 0.46 | 3.4 (−41.1 to 73.9) |
| Weight percentile | 91.3 (76.7 to 98.0) | 34.6 to 99.7 | 75.7 (61.3 to 82.1) | 98.0 (95.4 to 99.5) | <0.001 | 22.3 (1.5 to 64.9) |
| BMI percentile | 87.1 (60.1 to 95.8) | 26.0 to 99.1 | 53.4 (44.2 to 68.7) | 95.8 (92.6 to 98.3) | <0.001 | 42.4 (6.0 to 52.5) |
| Variable | Category | n (%) | p ** | Cramer’s V † | ||
|---|---|---|---|---|---|---|
| Total | Normal <85th Percentile | Overweight ≥85th Percentile | ||||
| Sex | M | 20 (95.2) | 10 (100.0) | 10 (90.9) | >0.99 | 0.218 |
| F | 1 (4.8) | 0 | 1 (9.1) | |||
| Modified Ogden Classification | Ib | 2 (9.5) | 1 (10.0) | 1 (9.1) | <0.99 | 0.282 |
| IIb | 1 (4.8) | 1 (10.0) | 0 | |||
| IIIa | 6 (28.6) | 3 (30.0) | 3 (27.3) | |||
| IIIb | 2 (9.5) | 1 (10.0) | 1 (9.1) | |||
| IVa | 1 (4.8) | 1 (10.0) | 0 | |||
| IVb | 8 (38.1) | 4 (40.0) | 4 (36.4) | |||
| V | 1 (4.8) | 0 | 1 (9.1) | |||
| Side | R | 5 (23.8) | 2 (20.0) | 3 (27.3) | >0.99 | 0.117 |
| L | 16 (76.2) | 8 (80.0) | 8 (72.7) | |||
| Associated Injuries | none | 6 (28.6) | 0 | 6 (54.5) | 0.01 | 0.612 |
| patellar ligament | 10 (47.6) | 9 (90.0) | 1 (9.1) | <0.001 | 0.788 | |
| tibialis anterior muscle | 1 (4.8) | 1 (10.0) | 0 | >0.99 | 0.218 | |
| quadriceps tendon | 2 (9.5) | 0 | 2 (18.2) | 0.48 | 0.343 | |
| retinacula | 3 (14.3) | 1 (10.0) | 2 (18.2) | >0.99 | 0.148 | |
| patellar luxation | 1 (4.8) | 0 | 1 (9.1) | 0.47 | 0.248 | |
| fibular head fracture | 2 (9.5) | 0 | 2 (18.2) | 0.48 | 0.343 | |
| skin avulsion | 1 (4.8) | 0 | 1 (9.1) | >0.99 | 0.218 | |
| Complications | yes | 3 (14.3) | 0 | 3 (27.3) | 0.21 | 0.411 |
| no | 18 (85.7) | 10 (100.0) | 7 (72.7) | |||
| Variable | Me (IQR) | Min–Max |
|---|---|---|
| Time until surgery (h) | 5.8 (3.1 to 15.8) | 1.8–73.5 |
| Duration of surgery (min) | 70 (50.0–95.0) | 30–120 |
| Immobilization time (days) | 37 (31 to 40) | 20–46 |
| Radiographic healing time (days) | 38 (34–44) | 20–65 |
| Hardware removal (days) | 244 (208–291) | 37–556 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kocur, J.; Čičak, S.; Dimnjaković, D.; Kiš, I.; Kristek, G.; Ivković, K.; Kristek, D.; Divković, D. Association of Elevated Body Mass Index with Tibial Tuberosity Avulsion Fractures in Pediatric Athletes: A Pilot Retrospective Study. Medicina 2025, 61, 1698. https://doi.org/10.3390/medicina61091698
Kocur J, Čičak S, Dimnjaković D, Kiš I, Kristek G, Ivković K, Kristek D, Divković D. Association of Elevated Body Mass Index with Tibial Tuberosity Avulsion Fractures in Pediatric Athletes: A Pilot Retrospective Study. Medicina. 2025; 61(9):1698. https://doi.org/10.3390/medicina61091698
Chicago/Turabian StyleKocur, Josip, Slavko Čičak, Damjan Dimnjaković, Izabela Kiš, Gordana Kristek, Krešimir Ivković, Dalibor Kristek, and Dalibor Divković. 2025. "Association of Elevated Body Mass Index with Tibial Tuberosity Avulsion Fractures in Pediatric Athletes: A Pilot Retrospective Study" Medicina 61, no. 9: 1698. https://doi.org/10.3390/medicina61091698
APA StyleKocur, J., Čičak, S., Dimnjaković, D., Kiš, I., Kristek, G., Ivković, K., Kristek, D., & Divković, D. (2025). Association of Elevated Body Mass Index with Tibial Tuberosity Avulsion Fractures in Pediatric Athletes: A Pilot Retrospective Study. Medicina, 61(9), 1698. https://doi.org/10.3390/medicina61091698







