The Role of Virtual Reality, Exergames, and Digital Technologies in Knee Osteoarthritis Rehabilitation Before or After Total Knee Arthroplasty: A Systematic Review of the Interventions in Elderly Patients
Abstract
1. Introduction
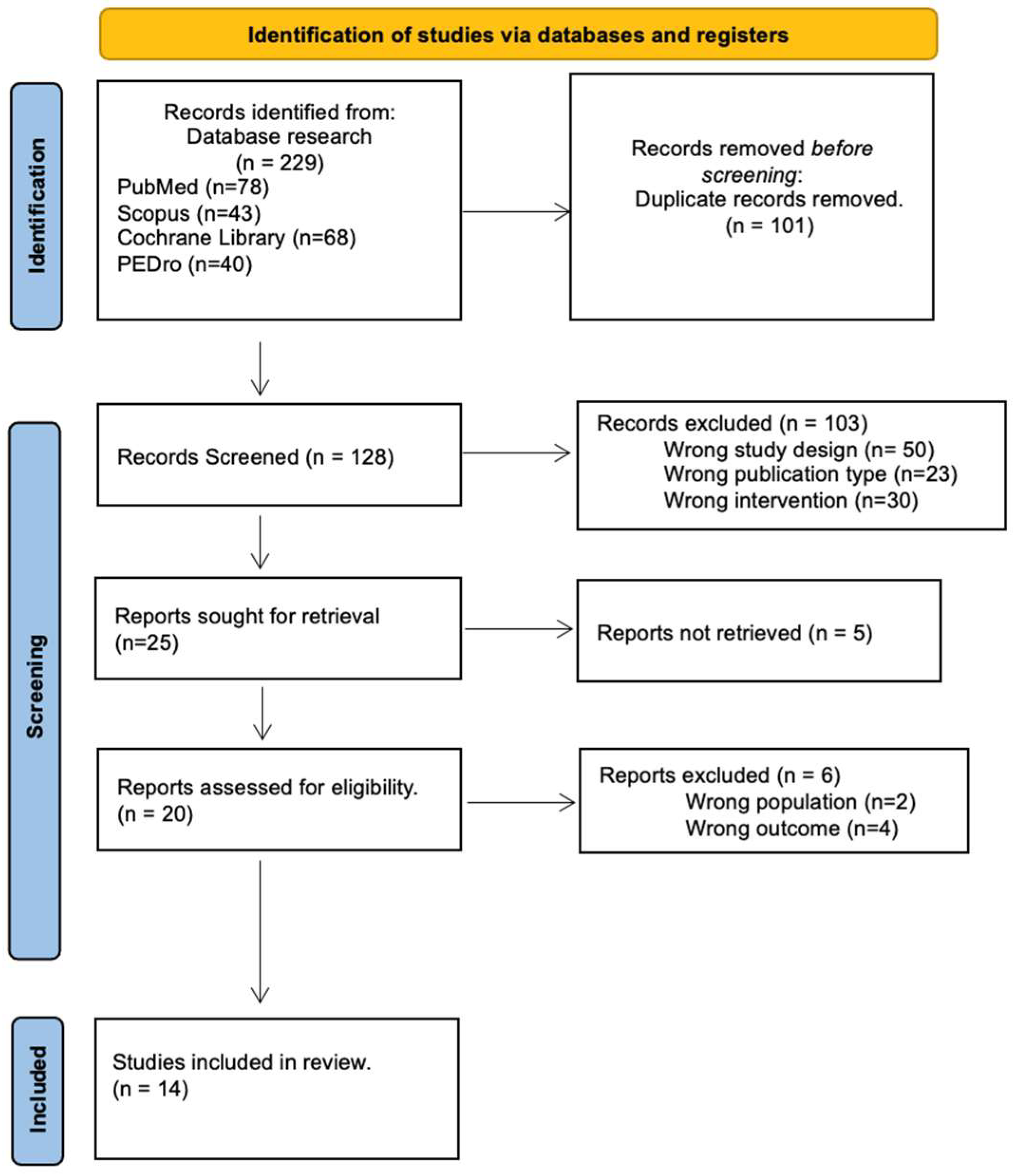
2. Materials and Methods
2.1. Data Source and Study Searching
2.2. Eligibility Criteria and PICO Principle
2.3. Data Extraction and Data Analysis
2.4. Risk of Bias Assessment
2.5. Statistical Analysis and Summary of Findings
3. Results
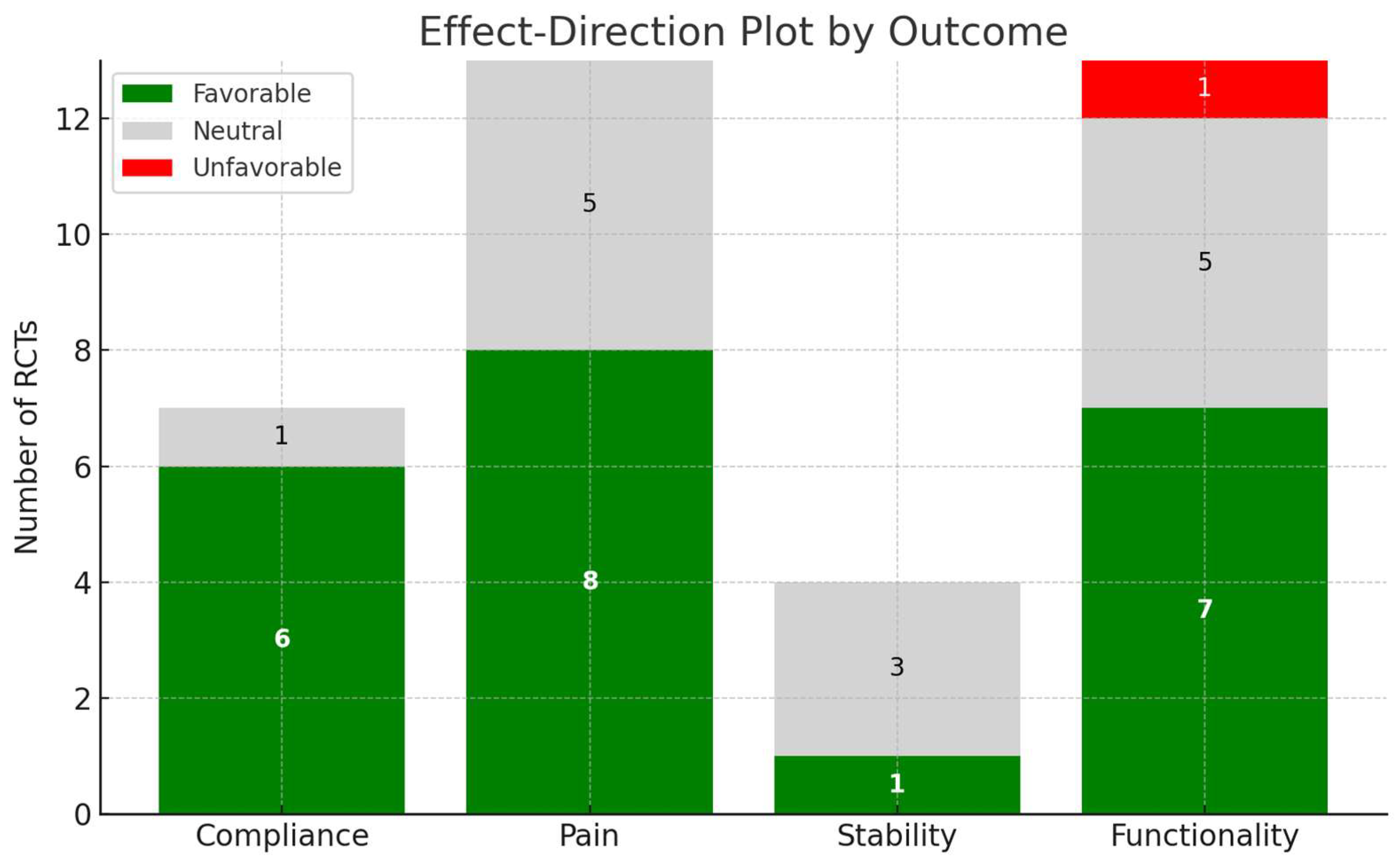
3.1. Compliance to the Therapy
3.2. Pain
3.3. Stability
3.4. Functionality
3.5. Risk of Bias
4. Discussions
4.1. Compliance to the Therapy
4.2. Pain
4.3. Stability
4.4. Functionality
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Giorgino, R.; Albano, D.; Fusco, S.; Peretti, G.M.; Mangiavini, L.; Messina, C. Knee Osteoarthritis: Epidemiology, Pathogenesis, and Mesenchymal Stem Cells: What Else Is New? An Update. Int. J. Mol. Sci. 2023, 24, 6405. [Google Scholar] [CrossRef] [PubMed]
- Michael, J.W.P.; Schlüter-Brust, K.U.; Eysel, P. Epidemiologie, ätiologie, diagnostik und therapie der gonarthrose. Dtsch. Aerzteblatt 2010, 107, 152–162. [Google Scholar] [CrossRef]
- Hunter, D.J.; Bierma-Zeinstra, S. Osteoarthritis. Lancet 2019, 393, 1745–1759. [Google Scholar] [CrossRef] [PubMed]
- Restuccia, R.; Ruggieri, D.; Magaudda, L.; Talotta, R. The preventive and therapeutic role of physical activity in knee osteoarthritis. Reumatismo 2022, 74, 1–21. [Google Scholar] [CrossRef]
- Basile, M.; Rumi, F.; Palmeri, M.; Mattozzi, I.; Manzoli, L.; Mammuccari, M.; Gigliotti, S.; Bernabei, R.; Cicchetti, A. Economic burden of prescriptive inadequacy in the management of osteoarthritis in Italy. Glob. Reg. Health Technol. Assess. 2020, 7, 101–108. [Google Scholar] [CrossRef]
- Spector, T.D.; Cicuttini, F.; Baker, J.; Loughlin, J.; Hart, D. Genetic influences on osteoarthritis in women: A twin study. BMJ 1996, 312, 940–943. [Google Scholar] [CrossRef]
- Blagojevic, M.; Jinks, C.; Jeffery, A.; Jordan, K. Risk factors for onset of osteoarthritis of the knee in older adults: A systematic review and meta-analysis. Osteoarthr. Cartil. 2010, 18, 24–33. [Google Scholar] [CrossRef]
- Neogi, T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr. Cartil. 2013, 21, 1145–1153. [Google Scholar] [CrossRef]
- Fazaa, A.; Rachdi, M.; Ben Salem, L.; El Ghardallou, M.; Miladi, S.; Boussaa, H.; Makhlouf, Y.; Ben Abdelghani, K.; Laatar, A. Functional Capacity and Quality of Life in Elderly Patients with Knee Osteoarthritis. Musculoskelet. Care 2024, 22, e70027. [Google Scholar] [CrossRef]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef]
- Skjæret, N.; Nawaz, A.; Morat, T.; Schoene, D.; Helbostad, J.L.; Vereijken, B. Exercise and rehabilitation delivered through exergames in older adults: An integrative review of technologies, safety and efficacy. Int. J. Med Informatics 2016, 85, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, T.B.F.; de Medeiros, C.S.P.; de Oliveira, V.H.B.; Vieira, E.R.; de Cavalcanti, F.A.C. Effectiveness of exergames for improving mobility and balance in older adults: A systematic review and meta-analysis. Syst. Rev. 2020, 9, 163. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- Brown, D. A Review of the PubMed PICO Tool: Using Evidence-Based Practice in Health Education. Health Promot. Pr. 2019, 21, 496–498. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Lawford, B.J.; Hinman, R.S.; Kasza, J.; Nelligan, R.; Keefe, F.; Rini, C.; Bennell, K.L. Moderators of Effects of Internet-Delivered Exercise and Pain Coping Skills Training for People with Knee Osteoarthritis: Exploratory Analysis of the IMPACT Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, e10021. [Google Scholar] [CrossRef]
- Moutzouri, M.; Koumantakis, G.A.; Hurley, M.; Kladouchou, A.G.; Gioftsos, G. Effectiveness of a Web-Guided Self-Managed Telerehabilitation Program Enhanced with Outdoor Physical Activity on Physical Function, Physical Activity Levels and Pain in Patients with Knee Osteoarthritis: A Randomized Controlled Trial. J. Clin. Med. 2024, 13, 934. [Google Scholar] [CrossRef]
- Rini, C.; Porter, L.S.; Somers, T.J.; McKee, D.C.; DeVellis, R.F.; Smith, M.; Winkel, G.; Ahern, D.K.; Goldman, R.; Stiller, J.L.; et al. Automated Internet-based pain coping skills training to manage osteoarthritis pain. Pain 2015, 156, 837–848. [Google Scholar] [CrossRef]
- Oliveira, L.K.R.; Marques, A.P.; Andrade, K.F.A.; de Assis, J.C.S.; Brito, A.L.; Souza, G.S.; Callegari, B. Virtual Reality in Improving Anticipatory Postural Adjustments to Step Initiation in Individuals with Knee Osteoarthritis: A Randomized Controlled Trial. Games Health J. 2024, 13, 100–108. [Google Scholar] [CrossRef]
- Gür, O.; Başar, S. The effect of virtual reality on pain, kinesiophobia and function in total knee arthroplasty patients: A randomized controlled trial. Knee 2023, 45, 187–197. [Google Scholar] [CrossRef]
- Tousignant, M.; Moffet, H.; Boissy, P.; Corriveau, H.; Cabana, F.; Marquis, F. A randomized controlled trial of home telerehabilitation for post-knee arthroplasty. J. Telemed. Telecare 2011, 17, 195–198. [Google Scholar] [CrossRef]
- An, J.; Ryu, H.-K.; Lyu, S.-J.; Yi, H.-J.; Lee, B.-H. Effects of Preoperative Telerehabilitation on Muscle Strength, Range of Motion, and Functional Outcomes in Candidates for Total Knee Arthroplasty: A Single-Blind Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 6071. [Google Scholar] [CrossRef]
- Jin, C.; Feng, Y.; Ni, Y.; Shan, Z. Original Article Virtual reality intervention in postoperative rehabilitation after total knee arthroplasty: A prospective and randomized controlled clinical trial. Int. J. Clin. Exp. Med. 2018, 11, 6119–6124. Available online: https://e-century.us/files/ijcem/11/6/ijcem0067965.pdf (accessed on 27 August 2025).
- Zhao, R.; Cheng, L.; Zheng, Q.; Lv, Y.; Wang, Y.-M.; Ni, M.; Ren, P.; Feng, Z.; Ji, Q.; Zhang, G. A Smartphone Application-Based Remote Rehabilitation System for Post-Total Knee Arthroplasty Rehabilitation: A Randomized Controlled Trial. J. Arthroplast. 2023, 39, 575–581.e8. [Google Scholar] [CrossRef]
- Doiron-Cadrin, P.; Kairy, D.; Vendittoli, P.-A.; Lowry, V.; Poitras, S.; Desmeules, F. Feasibility and preliminary effects of a tele-prehabilitation program and an in-person prehablitation program compared to usual care for total hip or knee arthroplasty candidates: A pilot randomized controlled trial. Disabil. Rehabilit. 2020, 42, 989–998. [Google Scholar] [CrossRef]
- Bettger, J.P.; Green, C.L.; Holmes, D.N.; Chokshi, A.; Mather, R.C.; Hoch, B.T.; de Leon, A.J.; Aluisio, F.; Seyler, T.M.; Del Gaizo, D.J.; et al. Effects of Virtual Exercise Rehabilitation In-Home Therapy Compared with Traditional Care After Total Knee Arthroplasty. J. Bone Jt. Surg. 2020, 102, 101–109. [Google Scholar] [CrossRef]
- Shim, G.Y.; Kim, E.H.; Lee, S.J.; Chang, C.B.; Lee, Y.S.; Lee, J.I.; Hwang, J.H.; Lim, J.-Y. Postoperative rehabilitation using a digital healthcare system in patients with total knee arthroplasty: A randomized controlled trial. Arch. Orthop. Trauma Surg. 2023, 143, 6361–6370. [Google Scholar] [CrossRef]
- Russell, T.G.; Buttrum, P.; Wootton, R.; A Jull, G. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: A randomized controlled trial. J. Bone Jt. Surg. 2011, 93, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Piqueras, M.; Marco, E.; Coll, M.; Escalada, F.; Ballester, A.; Cinca, C.; Belmonte, R.; Muniesa, J. Effectiveness of an interactive virtual telerehabilitation system in patients after total knee arthoplasty: A randomized controlled trial. J. Rehabilit. Med. 2013, 45, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Zeng, Y.; Wu, Y.; Si, H.; Shen, B. Virtual reality-based rehabilitation in patients following total knee arthroplasty: A systematic review and meta-analysis of randomized controlled trials. Chin. Med J. 2021, 135, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Zupančič, M.O.; Šarabon, N. The Current State of Virtual Reality in the Management of Musculoskeletal Conditions and Associated Chronic Pain: Terminology, Technology, and Associations. Appl. Sci. 2025, 15, 2564. [Google Scholar] [CrossRef]
- Gazendam, A.; Zhu, M.; Chang, Y.; Phillips, S.; Bhandari, M. Virtual reality rehabilitation following total knee arthroplasty: A systematic review and meta-analysis of randomized controlled trials. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2548–2555. [Google Scholar] [CrossRef] [PubMed]
- Bevilacqua, R.; Maranesi, E.; Riccardi, G.R.; Di Donna, V.; Pelliccioni, P.; Luzi, R.; Lattanzio, F.; Pelliccioni, G. Non-Immersive Virtual Reality for Rehabilitation of the Older People: A Systematic Review into Efficacy and Effectiveness. J. Clin. Med. 2019, 8, 1882. [Google Scholar] [CrossRef] [PubMed]
- Zitti, M.; Regazzetti, M.; Federico, S.; Cieslik, B.; Cacciante, L.; Maselli, F.; Storari, L.; Ricci, A.; Pregnolato, G.; Kiper, P. Effectiveness of Virtual Reality for Pain Management in Musculoskeletal Disorders Across Anatomical Regions: A Systematic Review and Meta-Analysis. Musculoskelet. Care 2025, 23, e70041. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kemmler, W.; Shojaa, M.; Kohl, M.; von Stengel, S. Effects of Different Types of Exercise on Bone Mineral Density in Postmenopausal Women: A Systematic Review and Meta-analysis. Calcif. Tissue Int. 2020, 107, 409–439. [Google Scholar] [CrossRef]
- Sturnieks, D.L.; George, R.S.; Lord, S.R. Balance disorders in the elderly. Neurophysiol. Clin. 2008, 38, 467–478. [Google Scholar] [CrossRef]
- Lei, C.; Sunzi, K.; Dai, F.; Liu, X.; Wang, Y.; Zhang, B.; He, L.; Ju, M. Effects of virtual reality rehabilitation training on gait and balance in patients with Parkinson’s disease: A systematic review. PLoS ONE 2019, 14, e0224819. [Google Scholar] [CrossRef]
- Bravi, M.; Longo, U.G.; Laurito, A.; Greco, A.; Marino, M.; Maselli, M.; Sterzi, S.; Santacaterina, F. Supervised versus unsupervised rehabilitation following total knee arthroplasty: A systematic review and meta-analysis. Knee 2023, 40, 71–89. [Google Scholar] [CrossRef]
- Lin, H.-T.; Li, Y.-I.; Hu, W.-P.; Huang, C.-C.; Du, Y.-C. A Scoping Review of The Efficacy of Virtual Reality and Exergaming on Patients of Musculoskeletal System Disorder. J. Clin. Med. 2019, 8, 791. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mosadeghi, S.; Reid, M.W.; Martinez, B.; Rosen, B.T.; Spiegel, B.M. Feasibility of an Immersive Virtual Reality Intervention for Hospitalized Patients: An Observational Cohort Study. JMIR Ment. Health 2016, 3, e28. [Google Scholar] [CrossRef]
- Li, A.; Montaño, Z.; Chen, V.J.; I Gold, J. Virtual Reality and Pain Management: Current Trends and Future Directions. Pain Manag. 2011, 1, 147–157. [Google Scholar] [CrossRef]

| Study | Participants | Technologies | Questionnaires, Assessment Tools and Timing | Rehab Protocol | Control Protocol |
|---|---|---|---|---|---|
| Belinda J Lawford et al., 2018 [16] | Knee OA Intervention group (n = 74), mean age: 60.8 ± 6.5 Control group (n = 74), mean age: 61.5 ± 7.6 | Educational material + online interactive automated PCST program + physical therapist consultations via Skype | Arthritis Self-Efficacy Scale Numerical Rating Scale (NRS) Western Ontario and McMaster Universities Arthritis Index (WOMAC) Pain Catastrophizing Scale Five-point Likert scale At baseline, 3 months and 9 months | Educational material + an online interactive automated PCST program, involving completion of one 35 to 45 min training module per week for 8 weeks + seven physical therapist consultations via Skype over 12 weeks, with each consultation lasting 30 to 45 min. | Same educational material as the intervention group but did not have access to the PCST program |
| Maria Moutzouri et al., 2024 [17] | Knee OA Intervention group (n = 22), mean age: 65.1 ± 5.3 Control group (n = 22), mean age: 63.5 ± 5.6 | minA web-based structured video exercise program + KOA disease consultatory video sessions (ESCAPE-pain program) + outdoor PA (physical activity) walk journey | Knee Injury Osteoarthritis Outcome Score (KOOS) Modified Baecke Physical Activity Questionnaire (mBQ) Lower Extremity Activity Scale (LEAS) Tampa Scale of Kinesiophobia (TSK) Numerical Pain Rating Scale (NPRS) 30 s sit-to-stand test Time up-and-go [TUG] test Short-Form 12 (SF-12) Baseline and at 6 weeks | A web-based structured video exercise program (twice a week) + KOA disease consultatory video sessions (once a week) + outdoor PA walk journey 3 times/week for 6 weeks. | General web-based information and advice for KOA and patients were encouraged to follow outdoor PA 5 times/week. |
| Study | Participants | Technologies | Questionnaires, Assessment Tools and Timing | Rehab Protocol | Control Protocol |
| Christine Rini et al. [18] | Knee or hip OA Intervention group (n = 58), mean age: 68.52 ± 7.65 Control group (n = 55), mean age: 66.67 ± 11.02 | Pain COACH program | Arthritis Impact Measurement Scale 2 (AIMS2) Arthritis Self-Efficacy Scale (ASES) Pain Anxiety Symptoms Scale (PASS-20) Positive and Negative Affect Scale (PANAS) At baseline, midpoint assessment and post-intervention (9 to 11 weeks after randomization) | Participants in this condition used the Pain COACH program, which translated an in-person pain-coping-skills training (PCST) protocol for delivery via the internet. Participants were led through the program by a “virtual coach”. Eight modules, each one took 35–45 min. One per week. | No access to Pain COACH at any point during or after the study. |
| Luana Karine Resende Oliveira et al., 2024 [19] | Knee OA Intervention group (n = 20), mean age: 62.35 ± 7.39 Control group (n = 20), mean age: 62.60 ± 8.62 | Virtual reality training using the Xbox 360 videogame with Microsoft Kinect 360 sensor. Game chosen: ‘‘Kinect Adventures’’ with three subgame modes: Reflex Ridge, 20,000 leaks, and RallyBall | Anticipatory postural adjustments (APAs) Mini-Balance Evaluation Systems Test (Mini-BESTest) WOMAC Visual Analog Pain Scale (VAS) at baseline and post-intervention | 30 min of kinesiotherapy + 20 min of exercise with non-immersive VR 8-week treatment, 50 min sessions, twice a week | 30 min of kinesiotherapy + 20 min of exercise with the objective of training postural control and balance 8-week treatment, 50 min session, twice a week |
| Study | Participants | Technologies | Questionnaires, Assessment Tools and Timing | Rehab Protocol | Control Protocol |
| Ozan Gür et al., 2023 [20] | TKA due to osteoarthritis Intervention group (n = 10), mean age: 63 Control group (n = 11), mean age: 61 | BOBOVR Z5 model VR devices | Numerical Pain Rating Scale (NPRS) Standardized Mini-Mental Test Tampa Kinesiophobia Scale Pain Catastrophizing Scale ROM (universal goniometer) Timed up and go test The stair-climb test WOMAC Short form 36 (SF-36) pre- and post-intervention | Exercise program 10 repetitions of each exercise twice a day + immersive VR application in addition to the exercise (10 min a day in the sitting position for 3 weeks, twice a week) | Only exercise program, 10 repetitions of each exercise twice a day |
| Michel Tousignant et al., 2011 [21] | TKA Experimental group (n = 21) Mean age: 66 ± 10 Control (n = 20) Mean age 66 ± 13 | Videoconferencing CODECs (550 MXP, Tandberg) with remote-controlled cameras, 50 cm LCD screens and associated software for user-friendly control | 30 s chair stand ROM (universal goniometer) WOMAC Timed up and go test Tinetti test Berg Balance scale Functional Autonomy Measurement System (SMAF) SF-36 At the beginning (T1) and at the end (T2) of the experimental intervention, and four months afterwards (T3). | The tele-treatments were delivered at a rate of two sessions per week for eight weeks, for a total of 16 sessions. | Conventional rehabilitation |
| Study | Participants | Technologies | Questionnaires, Assessment Tools and Timing | Rehab Protocol | Control Protocol |
| Jung Ae An et al., 2021 [22] | Candidates for TKA with advanced knee OA Preoperative telerehabilitation group—PTG (n = 18), mean age: 71.1 ± 3.30 Preoperative patient education group—PEG (n = 17), mean age: 70.05 ± 2.41 Control (n = 18), mean age: 70.38 ± 2.59 | Telerehabilitation at home using a smartphone or tablet via a two-way video call | Isokinetic Strength Assessment WOMAC Knee Flexion-ROM Timed up and go (TUG) Test Pressure pain threshold (PPT) At 4 weeks preoperatively, post-interventionally, and 6 weeks after TKA | The PTG group took part in a 30 min/session, 2 times/day, 5 days/week for 3 weeks, for a total of 30 sessions before TKA. The PEG group participated in a preoperative education session, a non-supervised intervention performed for 30 min per session, 2 times/day, 5 days/week for 3 weeks, and the exercise timing was adjustable. | The control group received the usual care, such as following the guideline of surgical procedure, postoperative progress monitoring, discharge destination determination, and simple quadriceps exercise intervention. |
| Chi Jin et al., 2018 [23] | TKA in patients with knee OA Experimental (n = 33); mean age: 66.45 ± 3.49 Control (n = 33); mean age: 66.30 ± 4.41 | Games in an immersive virtual environment. Mide Technology Inc., Cangzhou, China. | WOMAC Hospital for Special Surgery Knee Score (HSS) Visual Analog Scale (VAS) Range of motion (ROM) Before TKA, 1 month after, 3 months after and 6 months after TKA | Exercises + VR intervention was applied in the experimental group beginning the second day after TKA. Patients were asked to row a boat using knee flexion in an immersive virtual environment for 30 min periods, three times a day. | Active and passive exercises. Patients in the control group were asked to flex their knees passively using their arms until pain tolerance was reached. |
| Study | Participants | Technologies | Questionnaires, Assessment Tools and Timing | Rehab Protocol | Control Protocol |
| Runkai Zhao et al., 2023 [24] | TKA in patients with knee osteoarthritis Experimental group (n = 50), mean age: 65 Control group (n = 50), mean age: 65 | The Vital Health Remote Rehabilitation System: patient-side APP, wearable sensors, and surgeon-side websites | Knee range of motion (ROM) WOMAC Knee Society Score (KSS) SF-36 Five times sit-to-stand Test Single-leg stance Test (SLST) At 2, 6, and 12 weeks after surgery | Postoperative rehabilitation protocol on the APP for 3 months + evaluation of the performance in terms of the quality and quantity of training movements completed every 2 weeks and generated a rehabilitation report and a new training plan for the next two weeks | Patients in the control group underwent home-based rehabilitation following written instructions, with regular outpatient clinic visits with a follow-up of 3 month |
| Patrick Doiron-Cadrin et al., 2018 [25] | TKA candidates with severe knee OA Telerehabilitation (n = 12) Mean age: 69.9 ± 9.1 In person (n = 11) Mean age: 61.3 ± 8.1 Control (n = 11) Mean age: 66.7 ± 9.2 | Telerehabilitation with REACTS LiteVR medical consultation application | Lower Extremity Functional Scale (LEFS) WOMAC The Short Form (36) Health Survey (SF-36) Global Rating of Change scale (GRC) Timed up and go (TUG) Self-paced walk (SPW) Timed stair tests (ST) Satisfaction questionnaire At baseline and after 12 weeks | The in-person prehabilitation group received a 12-week rehabilitation program. Tele-prehabilitation group received the same exercise program and advice through an internet-based telecommunication mobile application after initial assessment. | Usual care |
| Study | Participants | Technologies | Questionnaires, Assessment Tools and Timing | Rehab Protocol | Control Protocol |
| Prvu Bettger et al., 2020 [26] | TKA for non-traumatic causes Virtual physical therapy (PT) Group (n = 153) Mean age: 65.4 ± 7.7 Traditional physical therapy (PT) Group (n = 153) Mean age: 65.1 ± 9.2 | VERA system (Virtual Exercise Rehabilitation Assistant) | Knee Injury and Osteoarthritis Outcome Score—KOOS Patient-Reported Outcomes Measurement Information System (PROMIS) 10-item global health assessment Patient-Specific Functional Scale Physical activity 10 m walk test ROM knee At baseline, at 6 weeks post-discharge and at 12 weeks post-discharge | Post-surgery patients used the system immediately after hospital discharge to view their own progress and could perform exercises as often as desired, with no restrictions on usage frequency or duration. Patients in the virtual PT group engaged for 5.9 ± 1.7 days per week. | Patients received usual physical therapy sessions at their residence or could visit clinics for their therapy sessions. Patients typically engaged in physical therapy 3.3 ± 2.0 days per week on average. |
| Ga Yang Shim et al., 2023 [27] | TKA Digital healthcare rehabilitation (DR) group (n = 28) Mean age: 68.25 ± 5.80 Conventional rehabilitation (CR) group (n = 28) Mean age: 72.96 ± 4.56 | Brochure-based exercises + AR-based digital healthcare system (UINCARE Home +; UINCARE Corp., Seoul, Republic of Korea) | 4 m gait speed WOMAC Health-related quality of life (EQ5D5L) Pain NRS Berg Balance Scale (BBS) Range of motion (ROM) Satisfaction questionnaire Manual muscle yest (MMT) At baseline (T0) and 3 (T1), 12 (T2), and 24 (T3) weeks after randomization. | Brochure-based exercises for 3 weeks followed by AR-based exercises for 9 weeks, 30 min per session at 12 levels of intensity. Each session consisted of 10 motions, 3 sets of 10 repetitions. | The control group performed only brochure-based exercises for 12 weeks, according to the standard rehabilitation protocol for patients after TKA |
| Study | Participants | Technologies | Questionnaires, Assessment Tools and Timing | Rehab Protocol | Control Protocol |
| Trevor G Russell et al., 2011 [28] | TKA Telerehabilitation group (n = 34) Control group (n = 31) Mean age: 68 ± 7.9 years | A computer-based telerehabilitation system specifically engineered for this study | WOMAC The Patient-Specific Functional Scale The Spitzer Quality-of-Life Uniscale Timed up and go test Pain intensity (VAS) Knee ROM Quadriceps muscle strength Gait Assessment Rating Scale Limb girth measurements Baseline and after 6 weeks from TKA | Forty-five minutes sessions, during which physical therapists administered, a rehabilitation program that consisted of self-applied techniques under the guidance of the remote therapist, along with exercises and education in the postoperative management of the total knee replacement. | Rehabilitation was administered in an outpatient physical therapy department, according to standard clinical protocol. Intervention sessions were of forty-five minutes. |
| Mercè Piqueras et al., 2013 [29] | TKA for knee OA Control group (n = 70) Intervention group (n = 72) Mean age: 73.3 ± 6.5 | Interactive virtual telerehabilitation (IVT) | ROM (goniometer) Quadriceps strength dynamometer Nicholas manual muscle tester (NMMT) Hamstring strength VAS Timed up and go test WOMAC Baseline, after completing rehabilitation and at 3-month follow-up | The group IVT received 1 h sessions for 10 days | The control group received the standard clinical protocol of TKA rehabilitation consisting of 1 h sessions for 10 days |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Curzio, L.D.; Paolucci, T.; Miccinilli, S.; Bravi, M.; Santacaterina, F.; Giorgi, L.; Sterzi, S.; Zollo, L.; Bernetti, A.; Bressi, F. The Role of Virtual Reality, Exergames, and Digital Technologies in Knee Osteoarthritis Rehabilitation Before or After Total Knee Arthroplasty: A Systematic Review of the Interventions in Elderly Patients. Medicina 2025, 61, 1587. https://doi.org/10.3390/medicina61091587
Curzio LD, Paolucci T, Miccinilli S, Bravi M, Santacaterina F, Giorgi L, Sterzi S, Zollo L, Bernetti A, Bressi F. The Role of Virtual Reality, Exergames, and Digital Technologies in Knee Osteoarthritis Rehabilitation Before or After Total Knee Arthroplasty: A Systematic Review of the Interventions in Elderly Patients. Medicina. 2025; 61(9):1587. https://doi.org/10.3390/medicina61091587
Chicago/Turabian StyleCurzio, Ludovica Di, Teresa Paolucci, Sandra Miccinilli, Marco Bravi, Fabio Santacaterina, Lucrezia Giorgi, Silvia Sterzi, Loredana Zollo, Andrea Bernetti, and Federica Bressi. 2025. "The Role of Virtual Reality, Exergames, and Digital Technologies in Knee Osteoarthritis Rehabilitation Before or After Total Knee Arthroplasty: A Systematic Review of the Interventions in Elderly Patients" Medicina 61, no. 9: 1587. https://doi.org/10.3390/medicina61091587
APA StyleCurzio, L. D., Paolucci, T., Miccinilli, S., Bravi, M., Santacaterina, F., Giorgi, L., Sterzi, S., Zollo, L., Bernetti, A., & Bressi, F. (2025). The Role of Virtual Reality, Exergames, and Digital Technologies in Knee Osteoarthritis Rehabilitation Before or After Total Knee Arthroplasty: A Systematic Review of the Interventions in Elderly Patients. Medicina, 61(9), 1587. https://doi.org/10.3390/medicina61091587









