Distribution of Hemoglobinopathy Disorders in Al-Kharj Province Based on Data from the Premarital Screening and Genetic Counseling Program
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample and Population
2.2. Premarital Screening Program and Genetic Counseling Program (PMSGC)
2.3. Hemoglobin Electrophoresis Analysis
2.4. Statistical Analysis
3. Results
3.1. Details of Hemoglobinopathy Disorders
3.1.1. Thalassemia Analysis
3.1.2. Screening of Thalassemia
3.2. Prevalence Rate of SCD
3.3. Prevalence of SCD Between 2017 and 2021
3.4. Prevalence Rate in Hemoglobinopathy Disorders
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PMSGC | Premarital Screening and Genetic Counseling Program |
| SCD | sickle cell disease |
| PMS | premarital screening program |
| HIV | human immunodeficiency |
| HPLC | high-performance liquid chromatography |
| MOH | Ministry of Health |
| CBC | complete blood count |
References
- Kumar, M.; Kargwal, V.; Goel, R.; Debnath, E.; Malhotra, S.; Balyan, K.; Zaidi, M.; Yadav, R. Screening and Diagnosis of Thalassemia and other hemoglobinopathies in North Indian population: Challenges faced. Pediatr. Hematol. Oncol. J. 2025, 10, 59–65. [Google Scholar] [CrossRef]
- Almutairi, G.; Harbi, G.S.A.; Almutairi, L.; Aljarallah, F.S.; Alzaydi, N.M.; Alradaddi, R.; Alofi, A.; Alharbi, M.M.; Alhumaidi, N.H.; Alhomaid, T.A. Knowledge and Attitude toward Hemoglobinopathy Premarital Screening program among students of health colleges at Qassim University. Cureus 2025, 17, e77081. [Google Scholar] [CrossRef] [PubMed]
- Alhowiti, A.; Shaqran, T. Premarital Screening Program Knowledge and Attitude among Saudi University Students in TABUK City 2019. Int. J. Med. Res. Health Sci. 2019, 8, 75–84. [Google Scholar]
- Binshihon, S.M.; Alsulami, M.O.; Alogaibi, W.M.; Mohammedsaleh, A.H.; Mandourah, H.N.; Albaity, B.S.; Qari, M.H. Knowledge and attitude toward hemoglobinopathies premarital screening program among unmarried population in western Saudi Arabia. Saudi Med. J. 2018, 39, 1226–1231. [Google Scholar] [CrossRef] [PubMed]
- Al-Shroby, W.A.; Sulimani, S.M.; Alhurishi, S.A.; Dayel, M.E.B.; Alsanie, N.A.; Alhraiwil, N.J. Awareness of Premarital Screening and Genetic Counseling among Saudis and its Association with Sociodemographic Factors: A National Study. J. Multidiscip. Healthc. 2021, 14, 389–399. [Google Scholar] [CrossRef] [PubMed]
- Gosadi, I.M. National screening programs in Saudi Arabia: Overview, outcomes, and effectiveness. J. Infect. Public Health 2019, 12, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Alsaeed, E.S.; Farhat, G.N.; Assiri, A.M.; Memish, Z.; Ahmed, E.M.; Saeedi, M.Y.; Al-Dossary, M.F.; Bashawri, H. Distribution of hemoglobinopathy disorders in Saudi Arabia based on data from the premarital screening and genetic counseling program, 2011–2015. J. Epidemiol. Glob. Health 2017, 7, S41. [Google Scholar] [CrossRef] [PubMed]
- More, P. A Review of Importance of Premarital Checkup and Counselling among Young Adults. Psychol. Educ. J. 2021, 58, 6369–6373. [Google Scholar] [CrossRef]
- Singh, V.; Biswas, A.K.; Baranwal, A.K.; Asthana, B.; Dahiya, T. Prevalence of hemoglobinopathies using high-performance liquid chromatography as diagnostic tool in anemic patients of tertiary care center of Western India. Asian J. Transfus. Sci. 2022, 18, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Attallah, S.; Alhadad, M.; Alqarni, W.; Filfilan, D.; Zaharani, A.; Alharby, A.; Malki, A.A.; Algabry, N.; Jamil, E.; Hakami, A.; et al. PB2542: Molecular spectrum of alpha thalassemia mutations in the western province of saudi arabia and recommendation for premarital screening. HemaSphere 2023, 7, e15174c0. [Google Scholar] [CrossRef]
- Olwi, D.I.; Merdad, L.A.; Ramadan, E.K. Thalassemia: A prevalent disease yet unknown term among college students in Saudi Arabia. J. Community Genet. 2017, 9, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Alasmari, S.Z. Premarital screening programme in Saudi Arabia: Insights into men’s awareness and perceptions. PubMed 2024, 28, 63–73. [Google Scholar]
- Moustafa, A.Z.; Almalki, R.A.; Qhashgry, E.I.; Qari, R.A.; Anwar, Z.S.; Alfahmi, A.M.; Fageeh, S.M.; Hendawy, D.; Balkhair, R. Prevalence of hemoglobin abnormality in the premarital screening Saudi population in Makkah city in a cross-sectional study Abstract. Deleted J. 2022, 2, 17–25. [Google Scholar] [CrossRef]
- Alhuthali, H.M.; Ataya, E.F.; Alsalmi, A.; Elmissbah, T.E.; Alsharif, K.F.; Alzahrani, H.A.; Alsaiari, A.A.; Allahyani, M.; Gharib, A.F.; Qanash, H.; et al. Molecular patterns of alpha-thalassemia in the kingdom of Saudi Arabia: Identification of prevalent genotypes and regions with high incidence. Thromb. J. 2023, 21, 115. [Google Scholar] [CrossRef] [PubMed]
- Al Eissa, M.M.A.; Almsned, F.; Alkharji, R.R.; Aldossary, Y.M.; AlQurashi, R.; Hawsa, E.A.; AlDosari, S.M.; Alqahtani, A.S.; Alotibi, R.S.; Farzan, R.; et al. The perception of genetic diseases and premarital screening tests in the central region of Saudi Arabia. BMC Public Health 2024, 24, 1556. [Google Scholar] [CrossRef] [PubMed]
- AlOtaiby, S.; Alqahtani, A.; Saleh, R.; Mazyad, A.; Albohigan, A.; Kutbi, E. Comprehension of premarital screening and genetic disorders among the population of Riyadh. J. Taibah Univ. Med. Sci. 2023, 18, 822–830. [Google Scholar] [CrossRef] [PubMed]
- Makkawi, M.; Alasmari, S.; Hawan, A.A.; Shahrani, M.M.A.; Dera, A.A. Hemoglobinopathies. Saudi Med. J. 2021, 42, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Aljabry, M.; Sulimani, S.; Alotaibi, G.; Aljabri, H.; Alomary, S.; Aljabri, O.; Sallam, M.; Alsultan, A. Prevalence and Regional Distribution of Beta-Hemoglobin Variants in Saudi Arabia: Insights from the National Premarital Screening Program. J. Epidemiol. Glob. Health 2024, 14, 1242–1248. [Google Scholar] [CrossRef] [PubMed]
| Gender | Thalassemia Trait | SCD | Hemoglobinopathy Disorders |
|---|---|---|---|
| Males | 163 (48.9%) | 86 (49.1%) | 249 (49%) |
| Females | 170 (51.1%) | 89 (50.9%) | 259 (51%) |
| Gender | Total Cases | <18 Years | 18–25 Years | 26–35 Years | 36–45 Years | 46–55 Years |
|---|---|---|---|---|---|---|
| Males | 163 (100%) | 37 (22.70%) | 33 (20.75%) | 30 (18.40%) | 32 (19.63%) | 31 (19.02%) |
| Females | 170 (100%) | 36 (21.18%) | 34 (20%) | 37 (21.76%) | 34 (20%) | 29 (17.06%) |
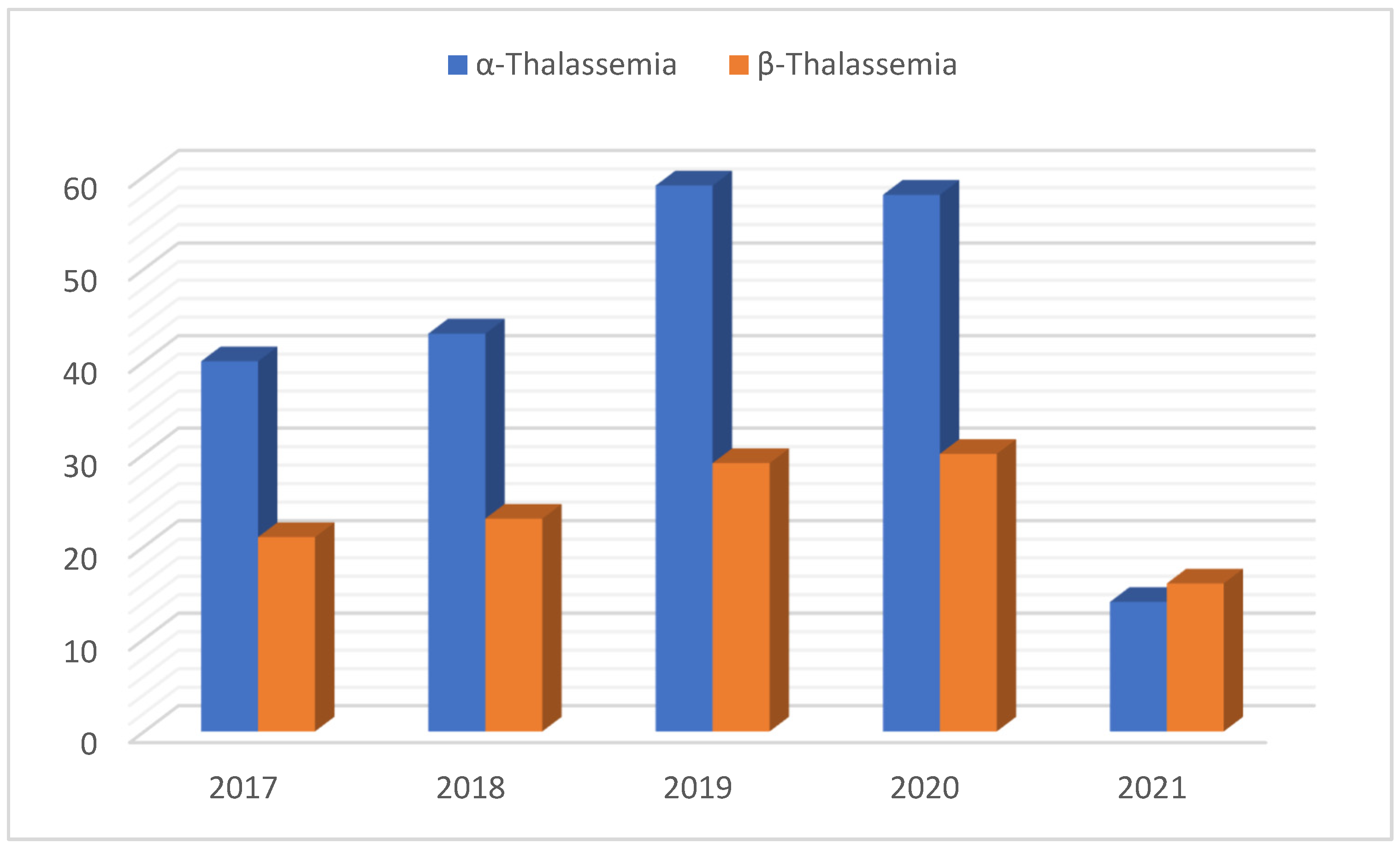
| Year | α-Thalassemia Trait (n = 214) | β-Thalassemia Trait (n = 119) |
|---|---|---|
| 2017 | 40 (18.7%) | 21 (17.6%) |
| 2018 | 43 (20.1%) | 23 (19.3%) |
| 2019 | 59 (27.6%) | 29 (24.4%) |
| 2020 | 58 (27.1%) | 30 (25.2%) |
| 2021 | 14 (6.5%) | 16 (13.4%) |
| Gender | <18 Years | 18–25 Years | 26–35 Years | 36–45 Years | 46–55 Years |
|---|---|---|---|---|---|
| Males | 17 (9.7%) | 18 (10.3%) | 23 (13.1%) | 15 (8.6%) | 13 (7.4%) |
| Females | 20 (11.4%) | 26 (14.9%) | 13 (7.4%) | 18 (10.3%) | 12 (6.9%) |
| Year-Wise | Diagnosis of Sickle Cell Traits (n = 175) |
|---|---|
| 2017 | 33 (18.9%) |
| 2018 | 35 (20.0%) |
| 2019 | 38 (21.7%) |
| 2020 | 45 (25.7%) |
| 2021 | 24 (13.7%) |
| Population Screened | α-Thalassemia | β-Thalassemia | ||
|---|---|---|---|---|
| Year | Total Participants (n = 21,150) | Positive Subjects (n = 119) | Confirmed Subjects (n = 214) | PR |
| 2017 | 5000 (23.6%) | 40 (18.7%) | 21 (17.6%) | 12.20% |
| 2018 | 5000 (23.6%) | 43 (20.1%) | 23 (19.3%) | 13.20% |
| 2019 | 5000 (23.6%) | 59 (27.6%) | 29 (24.4%) | 17.60% |
| 2020 | 5000 (23.6%) | 58 (27.1%) | 30 (25.2%) | 17.60% |
| 2021 | 1150 (5.4%) | 14 (6.5%) | 16 (13.4%) | 26% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Dayan, N. Distribution of Hemoglobinopathy Disorders in Al-Kharj Province Based on Data from the Premarital Screening and Genetic Counseling Program. Medicina 2025, 61, 1458. https://doi.org/10.3390/medicina61081458
Al-Dayan N. Distribution of Hemoglobinopathy Disorders in Al-Kharj Province Based on Data from the Premarital Screening and Genetic Counseling Program. Medicina. 2025; 61(8):1458. https://doi.org/10.3390/medicina61081458
Chicago/Turabian StyleAl-Dayan, Noura. 2025. "Distribution of Hemoglobinopathy Disorders in Al-Kharj Province Based on Data from the Premarital Screening and Genetic Counseling Program" Medicina 61, no. 8: 1458. https://doi.org/10.3390/medicina61081458
APA StyleAl-Dayan, N. (2025). Distribution of Hemoglobinopathy Disorders in Al-Kharj Province Based on Data from the Premarital Screening and Genetic Counseling Program. Medicina, 61(8), 1458. https://doi.org/10.3390/medicina61081458







