1. Introduction
Myofascial pain syndrome (MPS) is a soft tissue pain disorder characterized by localized and referred pain originating from trigger points (TrPs) within muscles or fascia. It is among the most common causes of both acute and chronic musculoskeletal pain, particularly in individuals exposed to prolonged static postures or repetitive strain, such as office workers and healthcare professionals [
1,
2,
3,
4]. Although the exact pathophysiology of MPS remains unclear [
5], factors such as trauma, postural imbalance, and psychological stress are believed to contribute to the development of TrPs [
3].
Cervical myofascial pain syndrome (C-MPS), a subtype of MPS, is one of the leading causes of chronic neck pain [
6]. TrPs in muscles such as the levator scapulae, upper trapezius, and infraspinatus not only generate localized discomfort but also cause radiating pain to the head and upper limbs [
6,
7,
8,
9]. These patterns may contribute to secondary musculoskeletal issues, including altered posture and referred neuropathic symptoms [
5].
Musculoskeletal pain disorders encompass more than just physical discomfort; they significantly diminish quality of life, impair occupational performance, and lead to increased utilization of healthcare resources [
10]. According to the World Health Organization (WHO) and the Global Burden of Disease study, musculoskeletal pain consistently ranks among the leading contributors to Disability-Adjusted Life Years (DALYs) worldwide [
11]. In the United States, over 100 million adults report experiencing chronic pain, with MPS and fibromyalgia identified as two of the most common underlying causes [
6]. Furthermore, in 2017, the global age-standardized prevalence and incidence rates of neck pain were reported as 3551.1 and 806.6 per 100,000 population, respectively, highlighting the significant global burden of this condition [
12,
13]. Similarly, in Republic of Korea, the Health Insurance Review and Assessment Service (HIRA) data from 2023 revealed that dorsalgia (M54, KCD-8), which includes cervicalgia (M54.2), ranked first in outpatient visits and reimbursement costs in Korean medicine services [
14]. These findings highlight the pressing need for effective and cost-efficient treatment strategies.
Reflecting this trend, clinical interest in C-MPS has been steadily increasing within the field of Korean medicine, accompanied by various non-surgical treatment approaches. A wide range of therapeutic modalities—including acupuncture, acupotomy, pharmacopuncture, and chuna manual therapy—has been utilized for C-MPS [
15]. More recently, ultrasound-guided acupuncture (UGA) has emerged as a promising alternative [
16,
17,
18], and ultrasound-guided pharmacopuncture (UGP) combines the therapeutic principles of pharmacopuncture treatment with the anatomical precision of real-time ultrasound imaging, allowing for accurate delivery of injectates into deep or complex interfascial spaces such as the SLS triangle (the interfascial space formed by the Splenius Capitis, Levator Scapulae, and Serratus Posterior Superior) [
7,
8,
19]. Early studies, including case reports and small trials, suggest that UGP improves pain and range of motion while minimizing procedural risks [
7,
8,
19].
However, most available evidence remains anecdotal or observational. Accordingly, this study was conducted as a multi-center, prospective observational study across seven Korean Medicine institutions, with the aim of objectively evaluating the clinical effectiveness and safety of UGP. We hypothesized that UGP would result in greater pain relief and functional improvement, with fewer adverse events, compared to non-guided pharmacopuncture for patients with acute C-MPS. This research serves as a follow-up to a previously published study protocol and is intended to provide foundational data for designing future randomized controlled trials (RCTs) [
8].
2. Materials and Methods
2.1. Study Design
This study was designed as a prospective observational study conducted in primary care clinics to evaluate the therapeutic effectiveness and safety of UGP in patients with acute C-MPS who present with neck and shoulder pain.
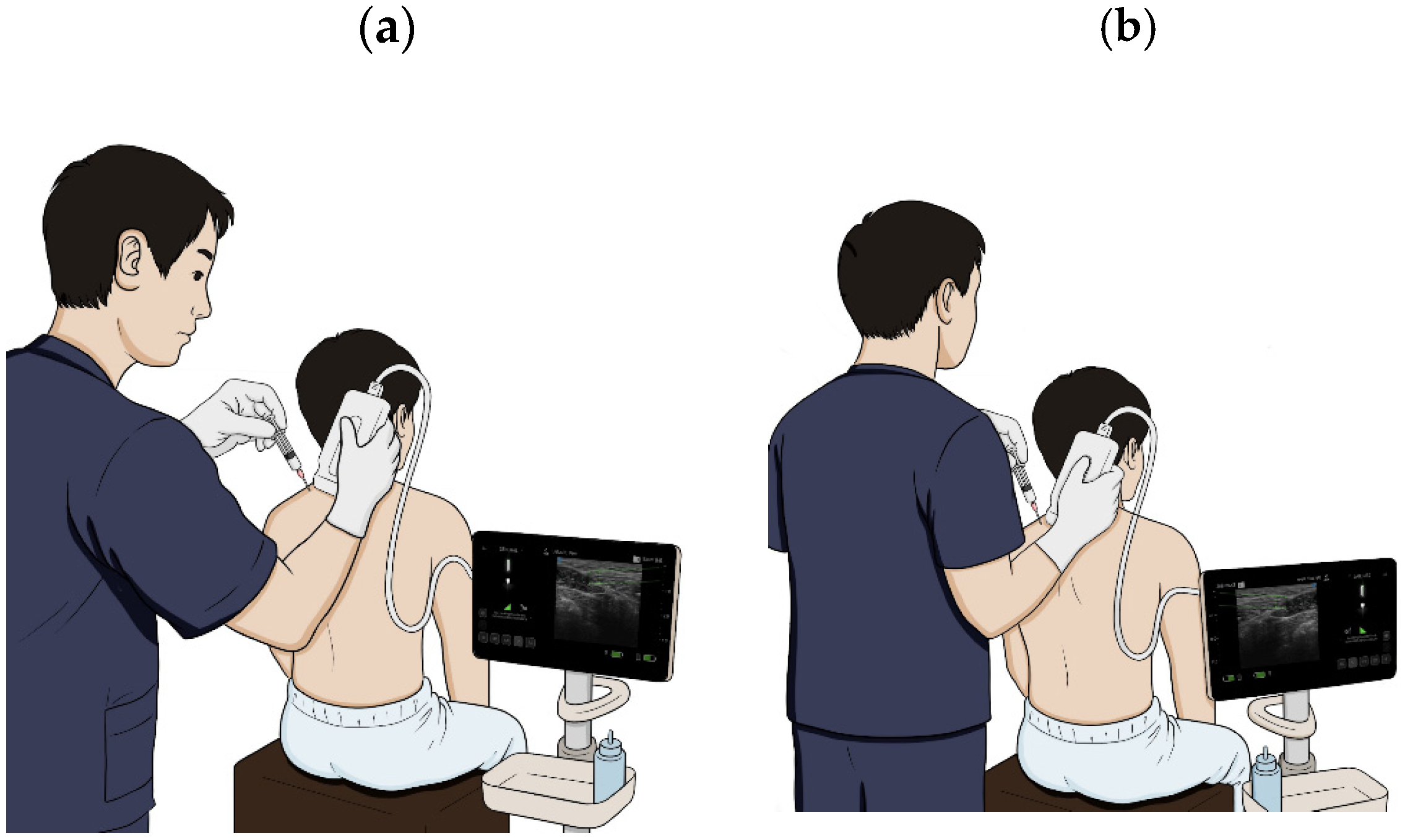
UGP was performed by identifying the interfascial space formed by the Splenius Capitis (SC), Levator Scapulae (LS), and Serratus Posterior Superior (SPS) muscles—referred to as the SLS triangle—under ultrasound guidance, followed by the injection of Hominis Placenta (HP) pharmacopuncture solution into the targeted area.
Participants were assigned to either the UGP group or the non-guided pharmacopuncture (NGP) group using a site-based allocation method, in which each institution recruited participants for only one of the two groups.
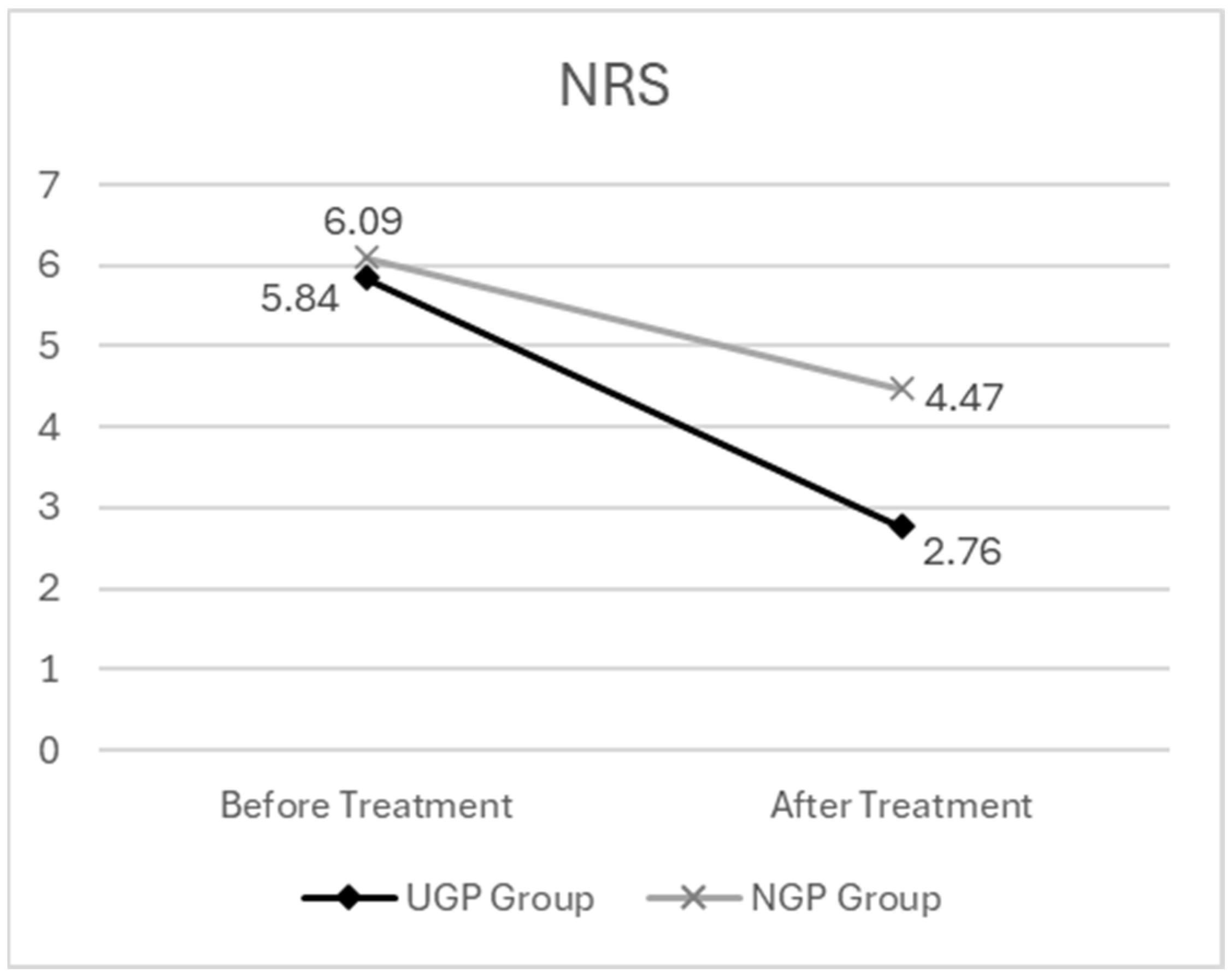
All participants received a single treatment session, and evaluations were conducted both before and after the procedure. These evaluations included pain assessment using the Numerical Rating Scale (NRS) and cervical function assessment using the Range of Motion (ROM) measurement. We monitored adverse events through a follow-up telephone interview conducted 24 to 36 h post-treatment.
In both groups, HP pharmacopuncture solution was used as the sole intervention. In the UGP group, the practitioner monitored the ultrasound screen in real time and injected the pharmacopuncture solution into the targeted area within the SLS triangle. During the procedure, the ultrasound screen was shielded from the patient to prevent visual access. In contrast, in the NGP group, the practitioner estimated the location of the SLS triangle through palpation, positioned the ultrasound probe over the area, and administered the pharmacopuncture treatment without viewing the ultrasound image. In this group, neither the practitioner nor the patient had access to the ultrasound screen.
The design of this study was based on the methodology proposed by Kim Jong Uk et al. [
20]. More detailed information on the study design and intervention protocol can be found in our previously published protocol paper (Kim et al. [
8]).
An overview of the study procedure and flow is summarized in
Figure 1.
2.2. Ethical Considerations
The study was initially designed to implement a crossover approach, in which each participating institution would alternate between conducting UGP and NGP during different periods. This strategy aimed to minimize inter-institutional bias. However, the Institutional Review Board (IRB) advised that it would be inappropriate for a prospective observational study conducted in primary care clinics—none of which were registered clinical trial sites and without randomized assignment—to adopt a design resembling that of a RCT. Consequently, the study design was revised to employ a site-based allocation method, wherein each institution was assigned to recruit participants for only one of the two groups.
The study protocol was approved by the Institutional Review Board of Wonkwang University Gwangju Medical Center (approval number: WKIRB-2024/10-3), and written informed consent was obtained from all participants prior to their enrollment in the study.
2.3. Study Registration
This study was registered with the Clinical Research Information Service (CRIS) of the Korea National Institute of Health (NIH), Republic of Korea (KCT0009932, Trial Status: Protocol version 1.2 (6 September 2024)).
2.4. Participating Institutions
Because this study was based on outpatient treatment settings, participating institutions were limited to sites that not only provided outpatient care but were also equipped with portable ultrasound devices.
Seven institutions were selected from among the members of the Academy of Korean Medicine Clinical Anatomy, a preliminary member society of the Association of Korean Medicine, all of which utilized portable ultrasound equipment. To ensure consistency in imaging acquisition and analysis, all participating sites used the same portable ultrasound device—AcuViz Pocket (FCU Co., Daejeon, Republic of Korea).
The list of the eight participating institutions is as follows:
2.5. Participants
Participants were recruited through research information posters displayed both inside and outside each institution. Additionally, online advertisements, including blog posts, were used to supplement recruitment. As compensation, participants received the ultrasound-guided pharmacopuncture treatment at no cost.
2.5.1. Inclusion Criteria
All study participants can only participate in the study if they meet all of the following criteria:
Adults aged 20 to 64 years;
Individuals who have experienced acute cervical pain within the past 7 days and are complaining of cervical pain and range of motion restrictions;
Individuals diagnosed with acute cervical myofascial pain syndrome at the outpatient clinic of the conducting medical institution or other medical facilities;
Individuals who have not received treatment for acute cervical myofascial pain syndrome at other hospitals after being diagnosed;
Individuals who voluntarily decide to participate in this study and sign an informed consent form.
2.5.2. Exclusion Criteria
The exclusion criteria are listed below, and any individual who met at least one of these criteria was excluded from participation.
Individuals who have taken medication or received related treatments for muscle pain or discomfort in the neck or shoulder area that occurred within the past 7 days (including both Western and Korean medicine);
Individuals with a surgical history in the cervical area within the past 3 months;
Individuals who have experienced a sprain in the cervical area due to trauma, such as a traffic accident or contusion, within the past 3 months;
(For women only) Individuals who are pregnant or have given birth within the past 6 months;
Individuals with symptoms such as edema due to diseases of the renal endocrine system;
Patients currently taking anticoagulants;
Individuals whose cognitive function is impaired, making it difficult to understand the consent form and provide voluntary consent;
Individuals taking psychiatric medications due to reasons such as depression;
Any other individuals deemed unsuitable for participation in the study by the medical staff.
Details regarding the criteria for early termination and dropout are described in the previous study conducted by Kim et al. [
8].
2.6. Device and Intervention
In this study, a portable ultrasound device, the AcuViz Pocket (FCU Co., Daejeon, Republic of Korea), was used to perform UGP. This device is equipped with a needle navigation system based on magnetic sensors, which allows real-time tracking of the position and direction of a magnetized needle. The system visualizes this information on the ultrasound image, thereby enhancing procedural accuracy.
The magnetized needle used in the procedure was a 26-gauge, 60 mm Acu-tracking needle (Youngchang Needle Co., Gimpo, Republic of Korea), which was designed to be removed after the injection of the pharmacopuncture solution.
HP pharmacopuncture solution was utilized as the sole pharmacological agent in this study. HP solution was prepared by the Anjung Korean Medicine Clinic Extramural Herbal Dispensary (Seoul, Republic of Korea) and is a biologically derived product obtained through the enzymatic hydrolysis of placental tissue collected from healthy donors [
21]. HP solution has been reported to exhibit anti-inflammatory, analgesic, antioxidant, and tissue regenerative effects [
22]. In this study, the injection was administered into the area of maximum tenderness within the SLS triangle, covering a region approximately 5 cm in diameter. A disposable 5 cc syringe (Bukwang Medical, Yangju-si, Gyeonggi-do, Republic of Korea) containing 2 cc of HP pharmacopuncture solution was utilized for each treatment [
23]. The injection was performed using a 26-gauge × 60 mm guiding needle (Yongchang Co., Gimpo-si, Gyeonggi-do, Republic of Korea) under ultrasound guidance.
2.7. Outcome Measures
In this study, the outcome measures were established by comparing patient status immediately before and after the procedure to quantitatively assess changes in pain and functional mobility. To ensure both clinical relevance and practicality in real-world settings, pain was evaluated using the NRS, and cervical function was assessed by measuring the ROM of the cervical spine.
The NRS is a simple and sensitive tool widely used for subjective pain assessment, allowing patients to rate their perceived pain on a scale from 0 (indicating no pain) to 10 (representing the worst imaginable pain) [
24].
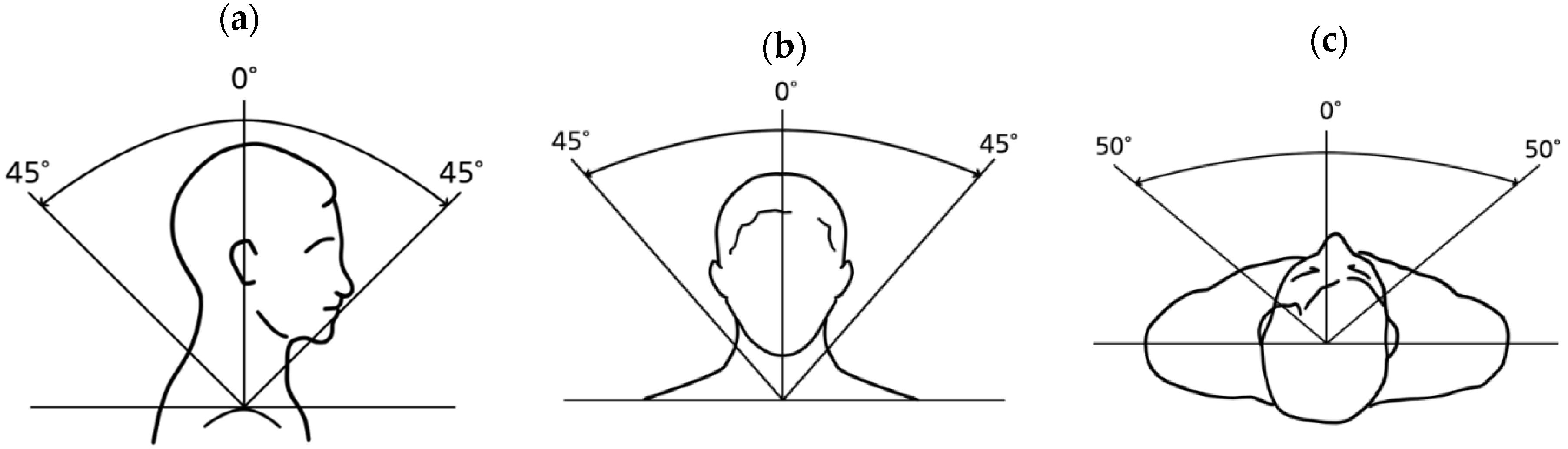
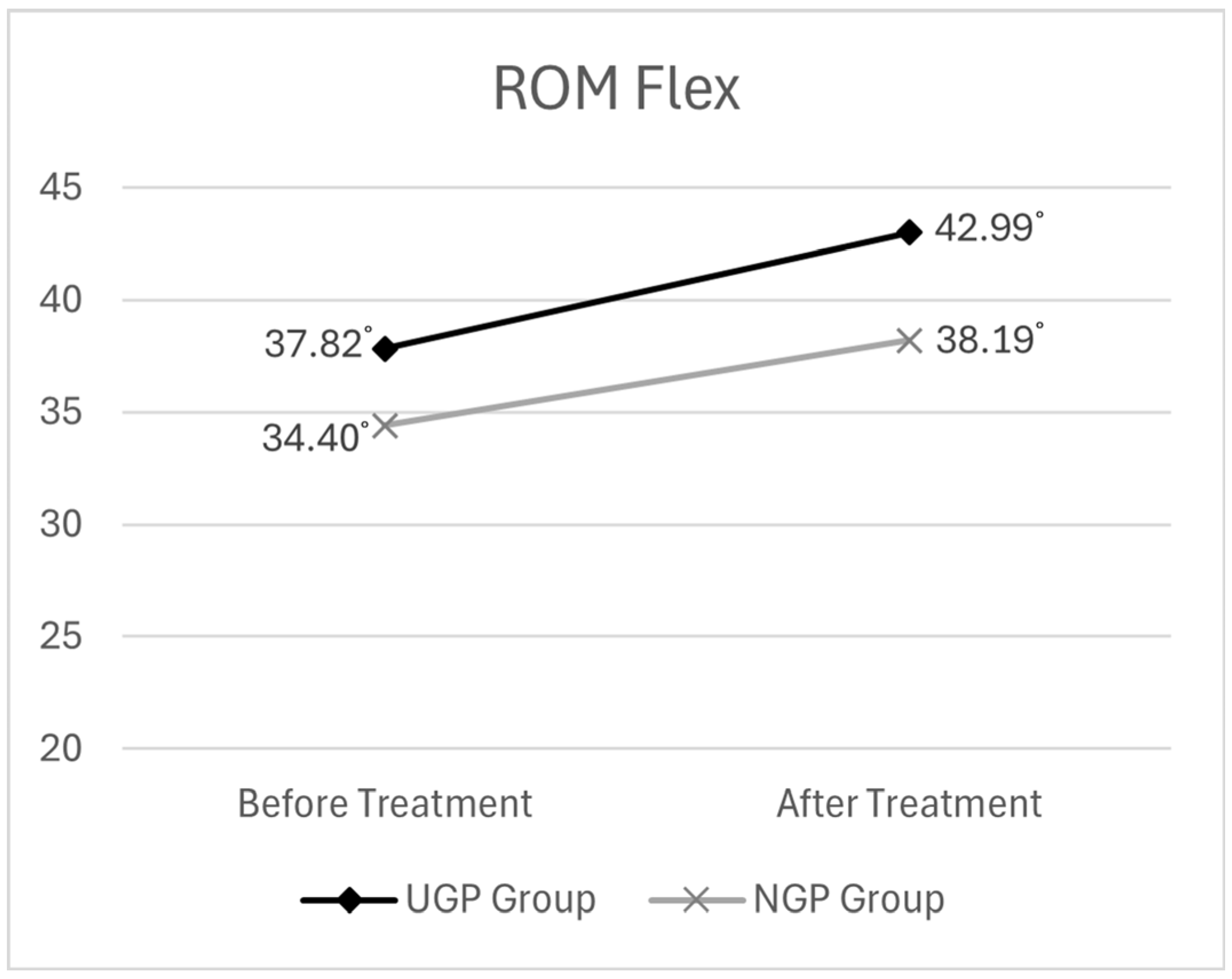
Cervical ROM was assessed as Active Range of Motion (A-ROM), including flexion, extension, lateral flexion to both sides, and rotation to both sides. All ROM measurements were conducted using a goniometer [
25], with the evaluator’s line of sight and posture fixed in a standardized position, in accordance with the impairment evaluation guidelines of the Korea Occupational Safety and Health Agency. An illustration of the standardized measurement posture is provided in
Figure 2.
Both NRS and ROM were measured using the same methods immediately before and after the procedure. We monitored adverse events through telephone follow-ups conducted immediately after treatment and again 24 to 48 h later. All assessments were performed by evaluators who had completed pre-study training and followed standardized measurement protocols. However, due to the nature of the study being conducted in a real-world clinical setting, evaluator blinding was not implemented; therefore, the possibility of measurement bias should be taken into account when interpreting the results.
2.8. Statistical Analysis
In this study, a two-way mixed analysis of variance (ANOVA) was conducted using the Statistical Package for the Social Sciences (SPSS) for Windows (Version 20.0; IBM Corp., Armonk, NY, USA) and RStudio (Version 2021.09.2+32; Posit Software, Boston, MA, USA) to evaluate the effects of ultrasound guidance (UGP vs. NGP) and time (pre-treatment vs. post-treatment) on participants’ pain levels (measured by the NRS) and cervical ROM. Additionally, the study aimed to examine the interaction effects between these factors. This statistical method is particularly well suited for analyzing repeated measures of dependent variables, such as NRS and ROM, and allows for the assessment of whether treatment effects differ between groups over time.
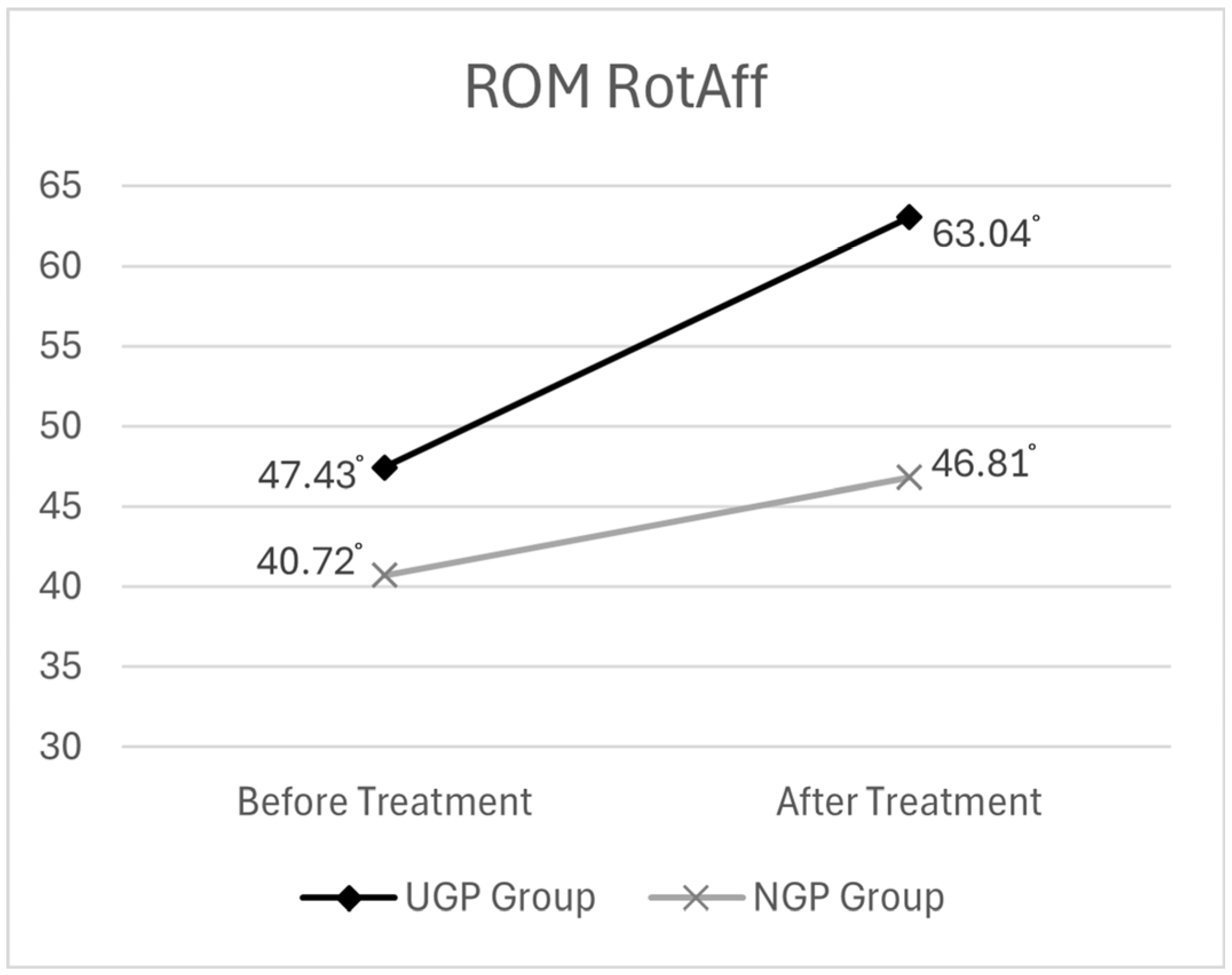
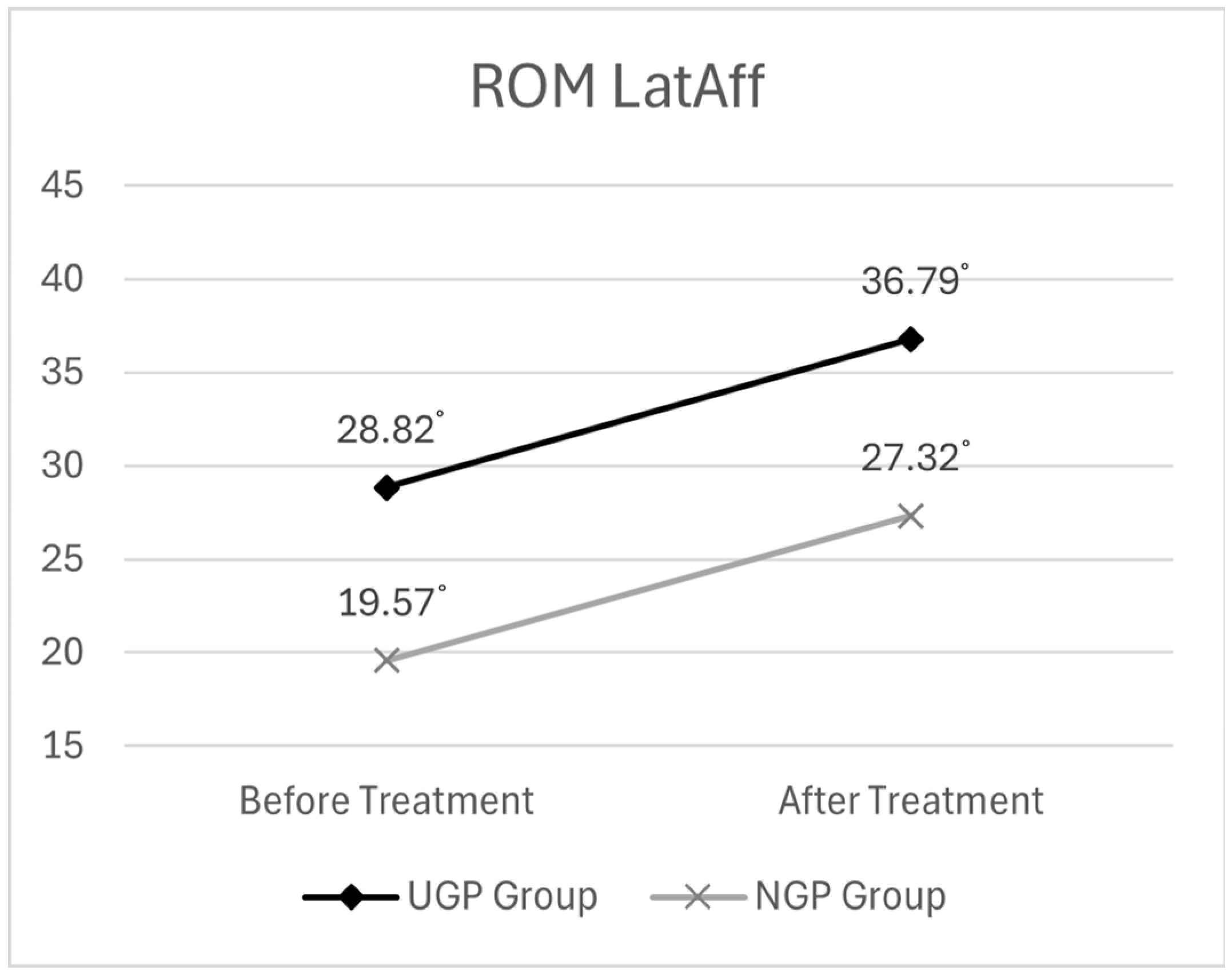
During the analysis of the study results, it was observed that, due to the characteristics of cervical myofascial pain syndrome, limitations in cervical rotation were often unilateral and predominantly occurred in a specific direction. Even in cases with bilateral limitations, patients typically exhibited more severe tenderness or reported greater pain subjectively on one side. Accordingly, NRS values were recorded based on the symptomatic side, and while ROM was measured bilaterally, the analysis of pre- and post-treatment changes focused on the affected direction for movements with lateral asymmetry. In particular, for cervical rotation and lateral flexion—where patients presented with varying directions of motion limitation—the data were standardized by aligning measurements to the affected side. These were designated as RotAff. (rotation on the affected side) and LatAff. (lateral flexion on the affected side), respectively, to enable consistent statistical comparisons.
4. Discussion
In this study, we confirmed that the clinical effectiveness of pharmacopuncture treatment for patients with acute C-MPS, characterized by neck and shoulder pain, varied based on the use of ultrasound guidance. The NRS scores showed a significantly greater reduction in the UGP group compared to the NGP group, indicating a more substantial alleviation of pain. This suggests that real-time ultrasound-guided targeting allows for more precise delivery of treatment to the intended anatomical structures, thereby enhancing therapeutic efficacy. These findings imply that real-time ultrasound-guided targeting provides a clinical advantage over conventional “blind” pharmacopuncture techniques.
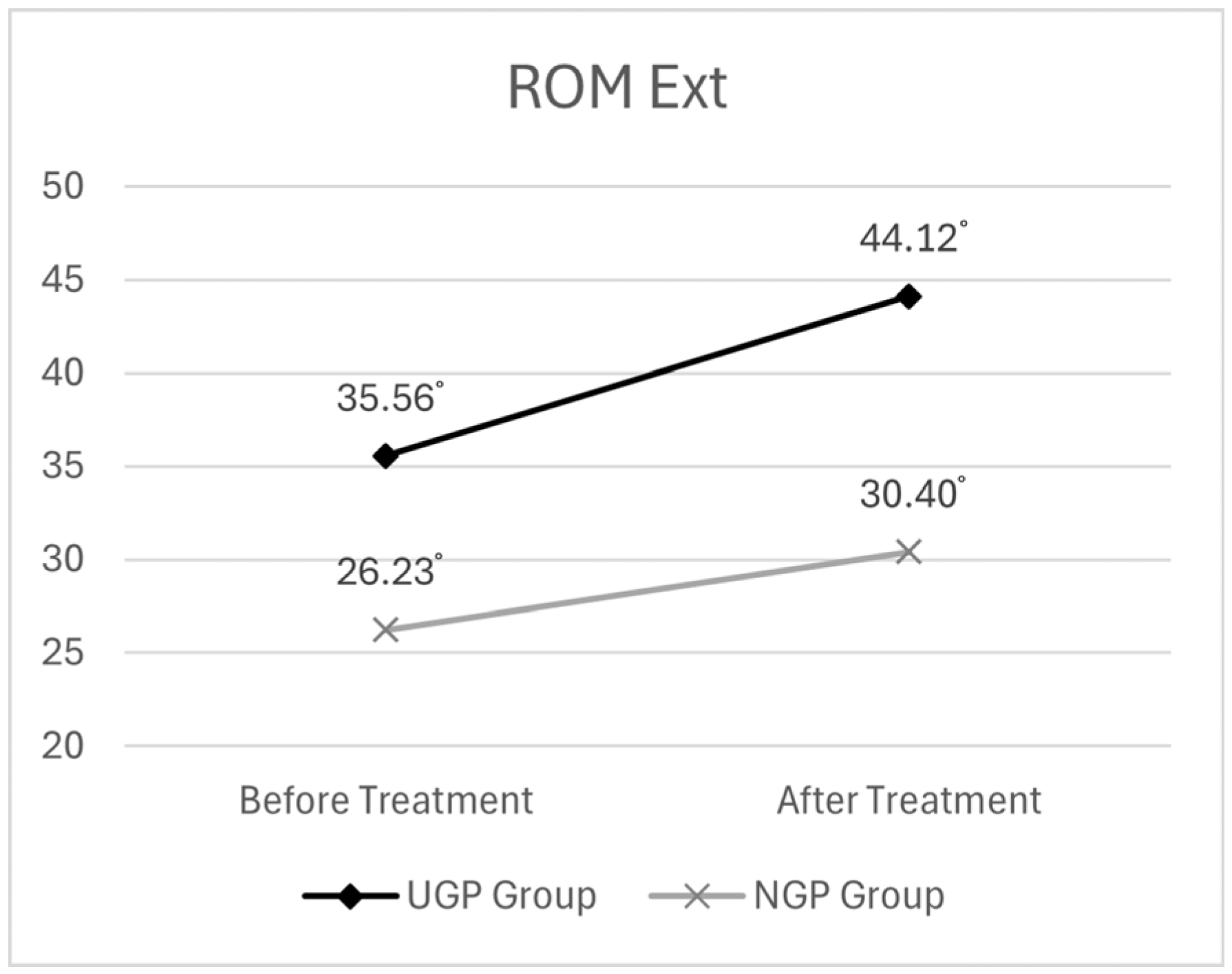
In the cervical ROM rotation (on the affected side) and extension measures, the UGP group exhibited significantly greater improvements compared to the NGP group. This difference may be attributed to the anatomical complexity of the posterior cervical region—particularly the deep interfascial structures, such as the SLS triangle (the interfascial space formed by the intersection of the Splenius Capitis, Levator Scapulae, and Serratus Posterior Superior muscles)—which are challenging to accurately target without imaging guidance. UGP enables the precise delivery of injectates into these anatomically complex regions, thereby enhancing functional recovery.
These findings are consistent with the known pathophysiology of musculoskeletal pain. Adhesions and impaired sliding between fascial layers are recognized as major contributors to such pain, and interfascial injections can help alleviate these restrictions, restore fascial gliding, and subsequently improve both pain and function [
26,
27]. Additionally, it has been hypothesized that pharmacological agents act on nociceptors located within the interfascial space, modulating pain sensitivity [
28]. Thus, the ability of ultrasound guidance to deliver medication accurately to these anatomical targets may have played a key role in producing the statistically significant and clinically meaningful improvements in cervical ROM observed in this study. In this context, HP pharmacopuncture—chosen for its anti-inflammatory, analgesic, and tissue-regenerative properties—may have further contributed to these effects. The targeted delivery of HP to inflamed and dysfunctional tissues through ultrasound guidance is presumed to have enhanced both pain relief and functional recovery.
In contrast, while both groups showed significant post-treatment improvements in cervical lateral flexion (on the affected side) and flexion, the differences between the groups were not statistically significant. This may be explained by the fact that the muscles surrounding the treatment site—specifically the SLS triangle—are not primarily responsible for these movements. Anatomically, cervical flexion is mainly driven by anterior muscles such as the longus colli and sternocleidomastoid, whereas lateral flexion primarily involves lateral muscles, including the sternocleidomastoid and scalenes. The musculature adjacent to the injection site in this study does not directly contribute to these specific motions. Nevertheless, the improvements observed in both groups may be linked to pain reduction in the levator scapulae region, which likely resulted in decreased muscular tension in adjacent areas, thereby facilitating smoother and more functional cervical movement overall.
In terms of safety, the advantages of UGP are clearly evident. Among a total of 97 procedures, no adverse events were reported on the day of treatment. One patient did experience mild headache and flu-like symptoms; however, according to the patient’s statement, these symptoms were attributed to an underlying cold rather than the pharmacopuncture itself, and the condition resolved spontaneously. These findings suggest that ultrasound-guided procedures may significantly reduce the risk of complications commonly associated with invasive interventions, such as bleeding, infection, or nerve damage [
29]. This is particularly significant for procedures performed in anatomically sensitive areas, such as the posterior cervical region, where vascular and neural structures are densely located. The ability to visualize and avoid these critical structures under ultrasound guidance facilitates safer and more precise injection of the pharmacopuncture solution. Consequently, this supports the potential role of ultrasound guidance in enhancing procedural safety across various myofascial conditions.
In recent years, the field of Korean medicine has evolved traditional therapeutic techniques by integrating them with modern medical technology. The clinical application of ultrasound devices serves as a representative example. Ultrasound provides the advantage of real-time visualization of anatomical structures, significantly enhancing the precision and safety of invasive procedures [
8,
17]. Due to these characteristics, ultrasound-guided techniques have gained increasing attention, particularly in pharmacopuncture and other interventions within Korean medicine [
25].
For instance, Kim Jong-Uk et al. (2019) conducted a prospective study on patients with shoulder pain and found that ultrasound-guided acupuncture (UGA) exhibited greater procedural accuracy and improved patient safety compared to non-guided procedures [
20]. In addition, Lee Jin-Ho et al. conducted a systematic review and meta-analysis on the efficacy and safety of ultrasound-guided pharmacopuncture (UGP) for various musculoskeletal disorders. Their findings indicated that, compared to non-guided pharmacopuncture, UGP was significantly more effective in reducing pain and improving function, while also being associated with a lower incidence of adverse events [
19]. These previous findings support the rationale for incorporating ultrasound guidance into pharmacopuncture procedures.
This study represents the first multi-center, prospective observational investigation in Korea aimed at quantitatively evaluating the clinical effectiveness and safety of UGP in patients with Cervical Myofascial Pain Syndrome (C-MPS). Conducted in real-world primary care outpatient settings and based on actual patient treatment outcomes, this research addresses the limitations of previous studies, which has largely been confined to case reports or survey-based studies with limited generalizability. In this context, the present study holds significant value as foundational research, demonstrating both clinical reproducibility and practical applicability.
In particular, the study demonstrates significant practical relevance, as it was conducted using a treatment protocol that can be realistically implemented in everyday clinical practice. The ultrasound equipment utilized was a portable device rather than a fixed model typically found in large hospitals, thereby enabling replication of the procedure in primary care clinics, including outpatient settings for Korean medicine. This highlights the feasibility of broader clinical adoption of UGP and underscores its potential for widespread application in community-based medical environments.
Moreover, the use of ultrasound imaging allowed for anatomically guided procedures that improved both precision and safety. The short-term therapeutic effects were objectively evaluated by comparing changes in pain, measured using the Numerical Rating Scale (NRS), and cervical Range of Motion (ROM) before and after treatment. Follow-up monitoring of adverse events was also conducted to evaluate the safety of the procedure.
Based on these findings, this study establishes a crucial foundation for designing high-quality clinical trials, including future randomized controlled trials (RCTs), and supports the clinical applicability of UGP as a non-surgical intervention within the Korean primary care system. Furthermore, it provides insights into the clinical significance, limitations, and future research directions regarding UGP.
This study presents the first multi-center observational evidence for the clinical use of UGP in real-world practice. However, several limitations must be acknowledged. First, the non-randomized observational design and institution-based group allocation introduce a risk of selection and performance bias. Second, the study was limited to short-term outcomes within 48 h post-treatment, providing no information on long-term efficacy. Third, interoperator variability in ultrasound proficiency may have affected the outcomes, and this was not adjusted in the analysis. Fourth, a single type of pharmacopuncture solution was used in this study, without specific standardization of its composition and concentration.
These limitations highlight important areas for improvement in future research. High-quality clinical trials with randomized allocation and blinding are needed to objectively validate the efficacy of UGP, and mid- to long-term follow-up studies are necessary to assess the durability of treatment effects. It is also important to compare the therapeutic outcomes of various pharmacopuncture solutions and evaluate how pharmacological efficacy may differ when the injectate is more precisely delivered to target tissues under ultrasound guidance. Further studies should aim to quantify differences in practitioner proficiency and explore the applicability of this intervention across a wider range of musculoskeletal conditions.
In summary, while this multi-center observational study provides preliminary clinical evidence supporting the use of UGP, it has several limitations, including its non-randomized design, short-term outcome measures, and lack of standardization in the composition of pharmacopuncture solutions. These findings highlight the need for future randomized controlled trials with extended follow-up periods and standardized protocols. Importantly, this study contributes to the foundational development of a standardized protocol for UGP, offering a valuable reference framework for future research. This framework can facilitate comparative studies of different pharmacopuncture solutions utilizing the same ultrasound-guided technique. With continued research, UGP may evolve into a precise and reliable standard intervention for musculoskeletal pain management in routine clinical practice.