Psychosocial Determinants of Patient Satisfaction in Orthodontic Treatment: A Pilot Cross-Sectional Survey in North-Eastern
Abstract
1. Introduction
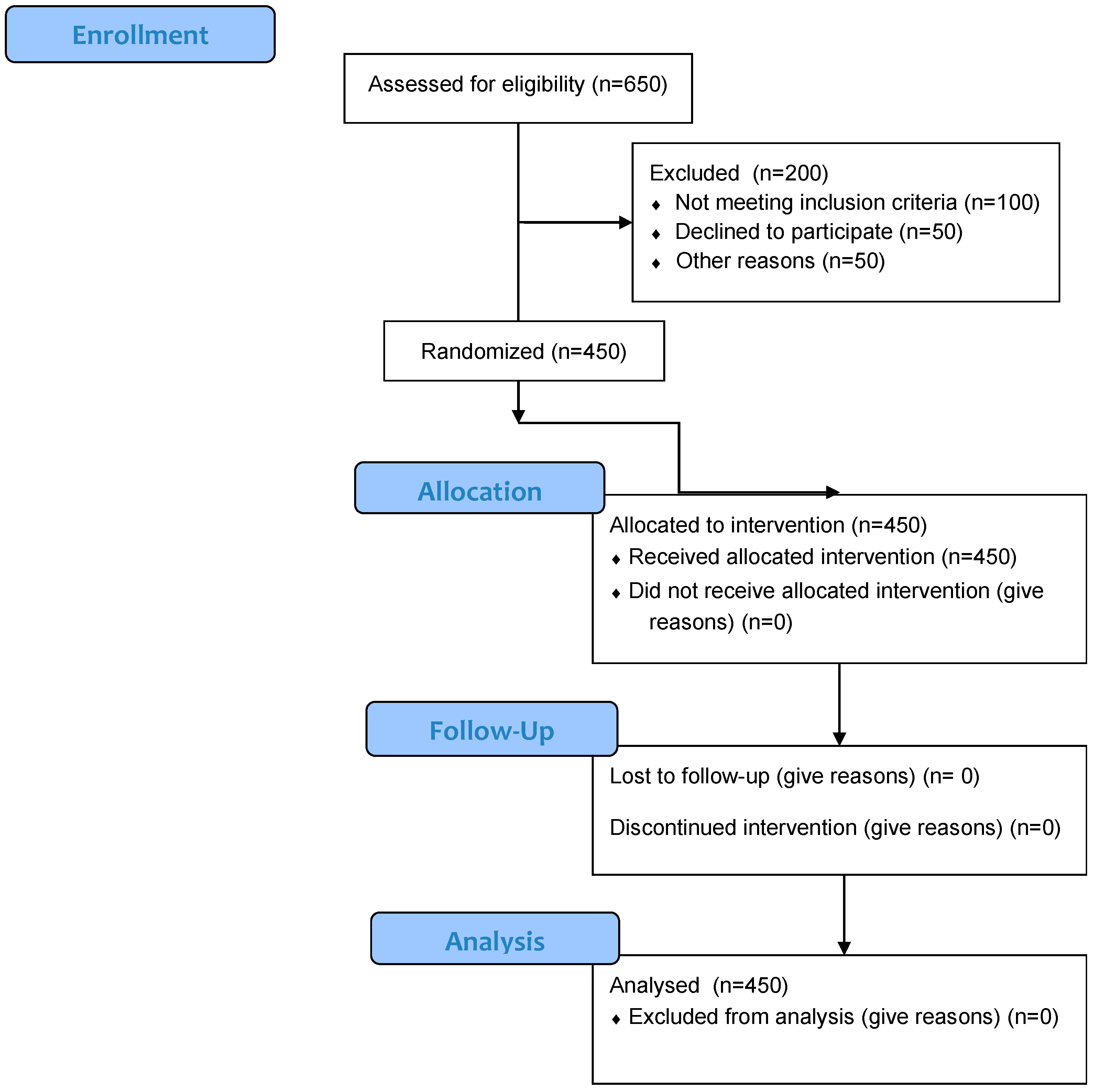
2. Materials and Methods
2.1. Study Framework
2.2. Ethics Statement
2.3. Sample Size Calculation
2.3.1. Inclusion Criteria
- Patients over 18 years old who had undergone or were undergoing orthodontic treatment.
- Patients who voluntarily agreed to participate in the study.
- Patients who completed the questionnaire with valid and complete responses.
2.3.2. Exclusion Criteria
- Patients who had not received orthodontic treatment.
- Individuals under 18 years old without parental consent.
- Respondents who provided incomplete or incorrect answers.
- Individuals with conditions that could interfere with orthodontic treatment outcomes, such as severe periodontal disease or untreated dental infections.
2.4. Questionnaire Development
2.5. Data Collection and Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics of the Study Population
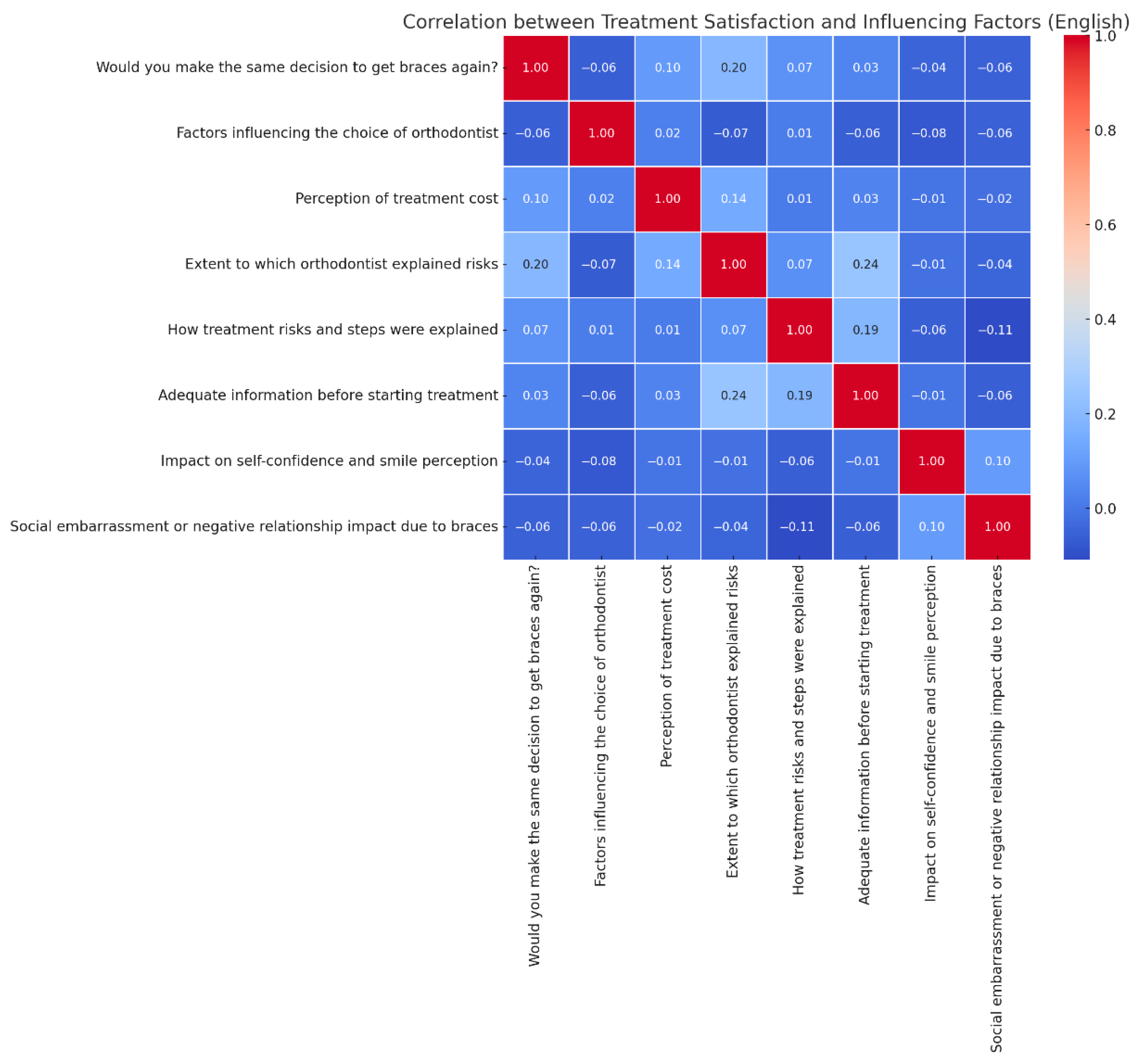
3.2. Correlation Between Patient Satisfaction and Influencing Factors in Orthodontic Treatment
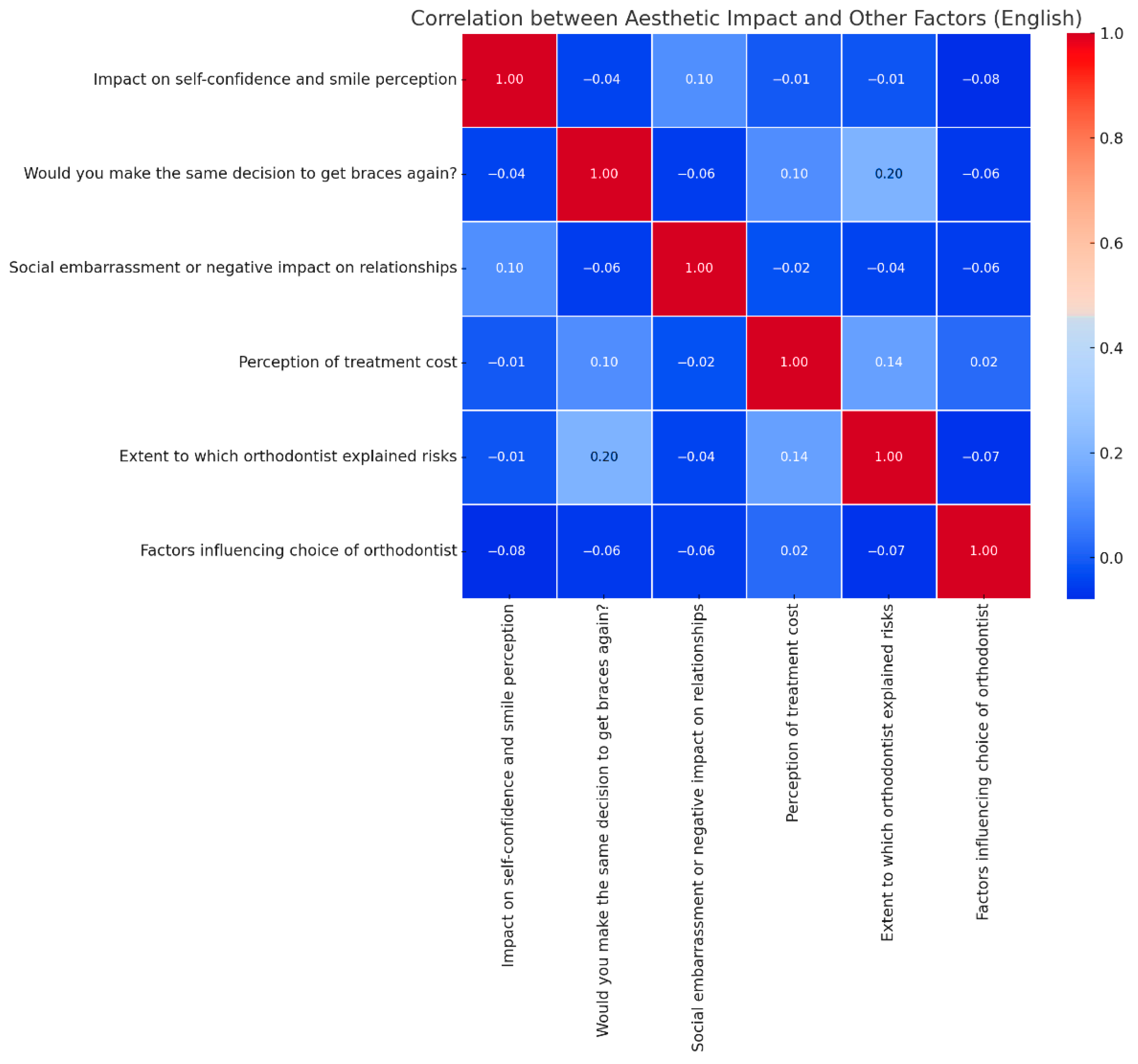
3.3. Correlation Between Aesthetic Function Improvement and Other Treatment-Related Factors
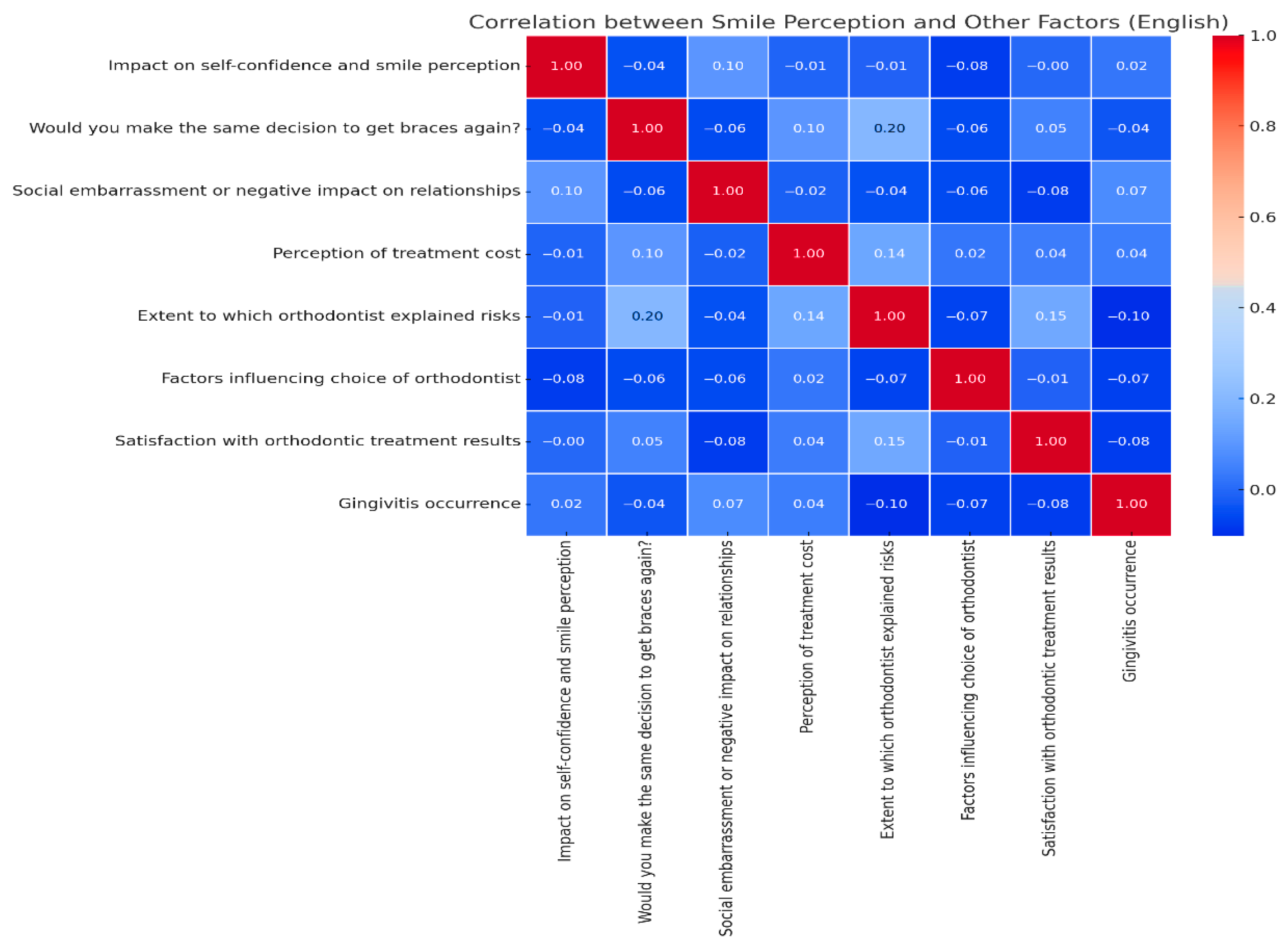
3.4. Correlation Between Smile Perception and Other Factors
3.5. Regression Analysis of Factors Influencing Patient Satisfaction with Orthodontic Treatment
4. Discussion
4.1. Self-Confidence and Smile Aesthetics (r = 0.62 − Strongest Predictor)
4.2. Orthodontist–Patient Communication/Explanation of Risks (r = 0.58, p = 0.002)
4.3. Perceived High Costs (r = −0.41)
4.4. Social Embarrassment or Stigma Due to Braces (r = −0.47)
4.5. Gender Imbalance and Its Impact on the Generalizability of Findings
4.6. Global Context
4.6.1. Aesthetic Improvement in Global Orthodontic Satisfaction
4.6.2. Cost Perception and Healthcare Systems: A Global Perspective
4.7. Practical Implications
4.8. Study Limitations
- Cross-sectional design—The study captures data at a single point in time, which prevents the establishment of causal relationships between identified predictors and patient satisfaction.
- Pilot study—the questionnaire was not psychometrically validated, which may limit the generalizability of the findings.
- Gender imbalance—The sample was overwhelmingly female (93.6%), which limits the generalizability of results to male patients and may skew findings toward gender-specific psychosocial experiences.
- Convenience sampling—The recruitment method may have introduced selection bias, as those who chose to participate might differ in satisfaction levels or health-seeking behaviors compared to those who declined.
- Limited model fit—The regression model explained only a small proportion of the variance in patient satisfaction (adjusted R2 = 0.011), suggesting that relevant psychosocial variables (e.g., self-esteem, personality traits, social influence) were not captured.
4.9. Future Research Direction
- Adopt a longitudinal design to track satisfaction before, during, and after treatment completion, allowing for causal inference and the assessment of long-term psychosocial outcomes.
- Include a broader set of psychosocial and personality variables, ideally guided by validated theoretical frameworks such as the Health Belief Model or the Patient Activation Measure.
- Ensure gender-balanced and demographically diverse samples to improve generalizability and enable subgroup analyses (e.g., gender-based satisfaction patterns).
- Employ validated instruments with established reliability and factor structure to minimize measurement error and increase model accuracy.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OR | odds ratio |
| OHRQoL | Oral Health-Related Quality of Life |
| GDP | Domestic Product. |
References
- Shrestha, D. Intensity of pain after separator placement, banding and bonding in fixed orthodontic patients. Int. J. Emerg. Trends Sci. Technol. 2017, 4, 5039–5042. [Google Scholar] [CrossRef]
- Mollov, N.; Lindauer, S.; Best, A.; Shroff, B.; Tüfekçi, E. Patient attitudes toward retention and perceptions of treatment success. Angle Orthod. 2010, 80, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, W.; Wang, S. Relationships among satisfaction, treatment motivation, and expectations in orthodontic patients: A prospective cohort study. Patient Prefer. Adherence 2016, 10, 443–447. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Finkleman, S.A.; Todoki, L.S.; Funkhouser, E.; Greenlee, G.M.; Choi, K.W.; Ko, H.-C.; Wang, H.-F.; Shapiro, P.A.; Khosravi, R.; Baltuck, C.; et al. The national dental practice-based research network adult anterior open bite study: Patient satisfaction with treatment. Am. J. Orthod. Dentofac. Orthop. 2020, 158, e121–e136. [Google Scholar] [CrossRef] [PubMed]
- Othman, S.; Mansor, N.; Saub, R. Randomized controlled clinical trial of oral health-related quality of life in patients wearing conventional and self-ligating brackets. Korean J. Orthod. 2014, 44, 168. [Google Scholar] [CrossRef] [PubMed]
- Piya, A.; Shrestha, B.; Acharya, J. Perception of pain resulting from orthodontic separators in orthodontic patients visiting dental department at a private hospital. Nepal Med. Coll. J. 2018, 20, 150–154. [Google Scholar] [CrossRef]
- Campos, L.; Santos-Pinto, A.; Marôco, J.; Campos, J. Pain perception in orthodontic patients: A model considering psychosocial and behavioural aspects. Orthod. Craniofac. Res. 2019, 22, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Xie, T.; Wang, J. The efficacy of analgesics in controlling orthodontic pain: A systematic review and meta-analysis. BMC Oral Health 2020, 20, 259. [Google Scholar] [CrossRef] [PubMed]
- Pachêco-Pereira, C.; Pereira, J.; Dick, B.; Perez, A.; Flores-Mir, C. Factors associated with patient and parent satisfaction after orthodontic treatment: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Aljughaiman, A.; Alshammari, A.; Althumairi, A.; Alshammari, A.; Almasoud, N.; Nazir, M. Patient satisfaction with orthodontic treatment received in public and private hospitals in Dammam, Saudi Arabia. Open Access Maced. J. Med. Sci. 2018, 6, 1492–1497. [Google Scholar] [CrossRef] [PubMed]
- Almoammar, S. The role of tele-orthodontics in enhancing patient compliance and treatment monitoring. J. Pharm. Bioallied Sci. 2024, 16 (Suppl. S3), S2676–S2678. [Google Scholar] [CrossRef] [PubMed]
- Shhabat, Z.; Ghozlan, M.; Kana’an, N.; Tashtoush, A.; Alelaimat, A.; Saadeh, R. The impact of COVID-19 pandemic on patients receiving orthodontic treatment. Eur. J. Dent. 2022, 17, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Mathew, R.; Sathasivam, H.; Mohamednor, L.; Yugaraj, P. Knowledge, attitude and practice of patients towards orthodontic treatment. BMC Oral Health 2023, 23, 132. [Google Scholar] [CrossRef] [PubMed]
- Hrestha, R.; Bhattarai, P.; Dhakal, J.; Shrestha, S. Knowledge, attitude and practice of patients towards orthodontic treatment: A multi-centric study. Orthod. J. Nepal 2014, 4, 6–11. [Google Scholar] [CrossRef]
- Keles, F.; Bos, A. Satisfaction with orthodontic treatment. Angle Orthod. 2012, 83, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Bahar, A.; Sagi, M.; Zuhairi, F.; Hassan, W. Dental aesthetics and self-esteem of patients seeking orthodontic treatment. Healthcare 2024, 12, 1576. [Google Scholar] [CrossRef] [PubMed]
- Jones, A. Association between healthcare provider communication and patient adherence to treatment plans in Australia. Glob. J. Health Sci. 2024, 9, 55–66. [Google Scholar] [CrossRef]
- Aldegheishem, A.; Alfayadh, H.; Aldossary, M.; Asaad, S.; Eldwakhly, E.; Refaei, N.; Soliman, M. Perception of dental appearance and aesthetic analysis among patients, laypersons and dentists. World J. Clin. Cases 2024, 12, 5354–5365. [Google Scholar] [CrossRef] [PubMed]
- Dias, M. Is the orthodontic smile considered as aesthetic in adult patients? Open Access J. Dent. Oral Surg. 2023, 4, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Pandey, R.; Kamble, R.; Suchak, D.; Kanani, H. Assessment of aesthetic smile components in patients with skeletal class II vertical and horizontal growth patterns compared to class I cases. Cureus 2024, 16, E60399. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, A.; Kiaee, B.; Sanayei, S.; Khosravi, S.; Perillo, L. Orthodontic treatment of malocclusion and its impact on oral health-related quality of life. Open Dent. J. 2016, 10, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Alqefari, J.; Albelaihi, R.; Elmoazen, R.; Bilal, R. Three-dimensional assessment of the oral health-related quality of life undergoing fixed orthodontic therapy. J. Int. Soc. Prev. Community Dent. 2019, 9, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Freitas, L.; Oliveira, D. Orthodontic retreatment: Positive effects on the patient’s self-esteem and quality of life. Dent. Press J. Orthod. 2021, 26, e21bbo5. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Kang, K. Effect of malocclusion or orthodontic treatment on oral health-related quality of life in adults. Korean J. Orthod. 2014, 44, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Demirovic, K.; Habibovic, J.; Džemidžić, V.; Tiro, A.; Nakaš, E. Comparison of oral health-related quality of life in treated and non-treated orthodontic patients. Med. Arch. 2019, 73, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Xia, F.; Hughes, J.P.; Voldal, E.C.; Heagerty, P.J. Power and Sample Size Calculation for Stepped-Wedge Designs with Discrete Outcomes. Trials 2021, 22, 598. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Statistics (INSSE). Poverty and Social Exclusion in Romania: Indicators and Regional Disparities; National Institute of Statistics (INSSE): Bucharest, Romania, 2023. [Google Scholar]
- Eurostat. Regional GDP per Capita in the EU: Disparities Remain Significant. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=GDP_at_regional_level (accessed on 15 May 2025).
- Romero-Maroto, M.; Santos-Puerta, N.; González-Olmo, M.; Peñacoba, C. The impact of dental appearance and anxiety on self-esteem in adult orthodontic patients. Orthod. Craniofacial Res. 2015, 18, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Mariz, A.; Araújo, S.; Negrinho, L.; Pedrosa, M.; Pompeu, J.; Silva, C. Impact of dental treatment on self-esteem and oral health selfperception of children and adolescents victims of sexual abuse. Braz. Dent. Sci. 2018, 21, 185–197. [Google Scholar] [CrossRef][Green Version]
- Omar, A.; Khalid, A.; Mahmoud, A. Psychological impact on implant patients’ oral health-related quality of life. Clin. Oral Implant. Res. 2006, 17, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Ellakany, P.; Fouda, S.; Alghamdi, M.; Bakhurji, E. Factors affecting dental self-confidence and satisfaction with dental appearance among adolescents in saudi arabia: A cross sectional study. BMC Oral Health 2021, 21, 149. [Google Scholar] [CrossRef] [PubMed]
- Yassir, Y.; McIntyre, G.; Bearn, D. The impact of labial fixed appliance orthodontic treatment on patient expectation, experience, and satisfaction: An overview of systematic reviews. Eur. J. Orthod. 2019, 42, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Pattanaik, S.; Veeraraghavan, V.; Dasari, A.; Patil, S.; Alzahrani, S.; Fareed, M. Orthodontic treatment in adults: Challenges, outcomes, and factors affecting compliance and satisfaction. J. Orthod. Sci. 2024, 13, 14. [Google Scholar] [CrossRef] [PubMed]
- Pradyachaipimol, N.; Tangsathian, T.; Supanimitkul, K.; Sophon, N.; Suwanwichit, T.; Manopattanasoontorn, S.; Arunyanak, S.P.; Kungsadalpipob, K. Patient satisfaction following dental implant treatment: A survey. Clin. Implant. Dent. Relat. Res. 2023, 25, 613–623. [Google Scholar] [CrossRef] [PubMed]
- Alshali, R.; Mustafa, R.; Bukhary, D.; Almuntashiri, A.; Alshamrani, Z.; Albalushi, O. Assessment of the satisfaction of patients treated by undergraduate dental students at a saudi government university: A cross sectional study. Clin. Cosmet. Investig. Dent. 2024, 16, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.; Arruda, A.; Inglehart, M. Adolescent patients’ treatment motivation and satisfaction with orthodontic treatment. Angle Orthod. 2009, 79, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Gornitzky, A.; England, P.; Kiani, S.; Yellin, J.; Flynn, J. Why don’t adolescents wear their brace? a prospective study investigating psychosocial characteristics that predict scoliosis brace wear. J. Pediatr. Orthop. 2022, 43, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Goje, D. Gender differences in adherence to orthodontic practices: An evaluation of oral hygiene and appointment compliance: An observational study. Afr. J. Biomed. Res. 2024, 27, 1986–1993. [Google Scholar] [CrossRef]
- Rubby, M.; Sultana, N.; Mamun, A.; Jannath, F. Exploring the reasons for seeking orthodontic treatment among the patients attended in selected private settings. Update Dent. Coll. J. 2023, 13, 14–16. [Google Scholar] [CrossRef]
- Uslu, A.; Büyük, S. Factors affecting the seeking of orthodontic treatment of turkish adults. J. Indian Orthod. Soc. 2023, 58, 32–36. [Google Scholar] [CrossRef]
- Wong, L.; Ryan, F.; Christensen, L.; Cunningham, S. Factors influencing satisfaction with the process of orthodontic treatment in adult patients. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Bradley, E.; Shelton, A.; Hodge, T.; Morris, D.; Bekker, H.; Fletcher, S.; Barber, S. Patient-reported experience and outcomes from orthodontic treatment. J. Orthod. 2020, 47, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Wezel, N.; Bos, A.; Prahl, C. Expectations of treatment and satisfaction with dentofacial appearance in patients applying for orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Ernata, R.; Gayatri, G.; Suwargiani, A. Correlation of orthodontic treatment motivation and the level of treatment needs based on the index of orthodontic treatment need (iotn) of orthodontic patients. Padjadjaran J. Dent. 2020, 32, 182. [Google Scholar] [CrossRef]
- Kolawole, K.; Otuyemi, O.; Jeboda, S.; Umweni, A. Awareness of malocclusion and desire for orthodontic treatment in 11 to 14 year-old nigerian schoolchildren and their parents. Australas. Orthod. J. 2008, 24, 21–25. [Google Scholar] [CrossRef]
- Linjawi, A.; Abushal, A.; Alzahrani, A.; Bakhamis, B. Patients’ perceptions to reduced orthodontic treatment time in saudi arabia. Patient Prefer. Adherence 2019, 13, 1973–1981. [Google Scholar] [CrossRef] [PubMed]
| Question | Answer Options |
|---|---|
| 1. What is your age? | ☐ 18–30 ☐ 31–50 ☐ Over 50 |
| 2. What is your gender? | ☐ Female ☐ Male ☐ Other/Prefer not to answer |
| 3. What factors influenced your choice of orthodontist? | ☐ Previous experience with the orthodontist ☐ Recommendations from family/friends ☐ Reputation of the orthodontist ☐ Proximity of the clinic ☐ Cost of treatment ☐ Other (Specify) |
| 4. How did you find the cost of braces and orthodontic treatment? | ☐ Affordable—it was a financial effort, but worth it ☐ Expensive—I had difficulty paying for it ☐ Very expensive—the cost was a major issue ☐ Accessible—it was not a financial impediment |
| 5. Did your orthodontic treatment include mini dental implants? | ☐ Yes, it was recommended and I accepted it ☐ Yes, but I refused ☐ No, it was not recommended ☐ Not sure/I don’t know |
| 6. What motivated you to start orthodontic treatment with braces? | ☐ I noticed my own dental issues and wanted to fix them ☐ My dentist recommended an orthodontic consultation ☐ My parents/family made the decision for me ☐ Other (Specify) |
| 7. How long have you been wearing braces? | ☐ Less than 6 months ☐ 6 months—1 year ☐ 1–2 years ☐ More than 2 years |
| 8. How has wearing braces influenced your self-confidence and perception of your smile? | ☐ Yes, in a positive way—I feel better about myself ☐ Yes, but only at the beginning ☐ No, it had no significant impact ☐ Yes, but in a negative way—it affected my self-confidence |
| 9. Is this your first time wearing braces? | ☐ Yes, this is my first experience with braces ☐ No, I have worn braces before |
| 10. How much pain or discomfort did you experience during orthodontic treatment? | ☐ A lot—it was hard to endure ☐ Moderate—I felt discomfort but it was bearable ☐ A little—only in the first few days ☐ Not at all |
| 11. To what extent did you have difficulties maintaining oral hygiene due to braces? | ☐ Very difficult ☐ Some difficulties, but I managed ☐ No significant difficulties |
| 12. Was the duration of your orthodontic treatment as expected? | ☐ Yes, the duration was as expected ☐ No, it lasted longer than expected ☐ No, it was shorter than expected |
| 13. Were you satisfied with the aesthetic results of your orthodontic treatment? | ☐ Yes, completely satisfied ☐ Yes, but I wish some aspects were different ☐ No, the results were not as expected |
| 14. How would you rate communication with your orthodontist throughout the treatment? | ☐ Very good—the doctor explained every step ☐ Good—I received enough information ☐ Poor—sometimes I didn’t fully understand the next steps ☐ Very poor—I was dissatisfied with the lack of explanations |
| 15. Have you ever felt social embarrassment or a negative impact on relationships due to braces? | ☐ Yes ☐ No |
| 16. What do you consider the biggest risks associated with wearing braces? (Check all that apply) | ☐ Demineralization/white spots on teeth ☐ Chewing problems or dietary modifications ☐ Temporomandibular joint issues ☐ Pain or discomfort |
| 17. To what extent did your orthodontist explain the risks and possible complications of the treatment? | ☐ Very well—I received all necessary information ☐ Well—risks were explained but I still had questions ☐ Not at all—risks were not explained |
| 18. If you had to decide again, would you choose to wear braces? | ☐ Yes, without hesitation ☐ Yes, but with some reservations ☐ Not sure ☐ No, I would not wear braces again |
| 19. What criteria do you consider essential for evaluating a good orthodontist? | ☐ Clearly explains treatment and answers questions ☐ Has experience and good recommendations ☐ Has an empathetic and communicative attitude |
| Variable | Category | No (%) |
|---|---|---|
| Gender | Female | 421 (93.6%) |
| Male | 29 (6.4%) | |
| Age group | 18–30 years | 390 (86.7%) |
| 31–50 years | 55 (12.2%) | |
| Over 50 years | 5 (1.1%) |
| Variable | Coefficient | Standard Error | t-Statistic | p-Value | Odds Ratio (OR) | OR 95% Lower | OR 95% Upper |
|---|---|---|---|---|---|---|---|
| Constant | 1.320 | 0.393 | 3.358 | 0.000 | 3.747 | 1.729876 | 8.11657 |
| Age | 0.119 | 0.130 | 0.917 | 0.359 | 1.126 | 0.872 | 1.455 |
| Cost Perception | 0.021 | 0.048 | 0.452 | 0.650 | 1.022 | 0.929 | 1.124 |
| Duration of Appliance | 0.020 | 0.037 | 0.540 | 0.588 | 1.020 | 0.947 | 1.099 |
| Type of Appliance | −0.045 | 0.043 | −1.057 | 0.290 | 0.955 | 0.877 | 1.040 |
| Oral Hygiene Difficulties | 0.029 | 0.075 | 0.390 | 0.696 | 1.029 | 0.887 | 1.194 |
| Pain | 0.005 | 0.069 | 0.079 | 0.936 | 1.005 | 0.877 | 1.152 |
| Risk Explanation | 0.178 | 0.057 | 3.074 | 0.002 | 1.195 | 1.066 | 1.339 |
| R-squared | 0.026 | 1.027 | |||||
| Adj. R-squared | 0.011 | 1.011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panaite, T.; Romanec, C.L.; Adina, A.; Carina, B.; Savin, C.; Sîrghie, A. Psychosocial Determinants of Patient Satisfaction in Orthodontic Treatment: A Pilot Cross-Sectional Survey in North-Eastern. Medicina 2025, 61, 1328. https://doi.org/10.3390/medicina61081328
Panaite T, Romanec CL, Adina A, Carina B, Savin C, Sîrghie A. Psychosocial Determinants of Patient Satisfaction in Orthodontic Treatment: A Pilot Cross-Sectional Survey in North-Eastern. Medicina. 2025; 61(8):1328. https://doi.org/10.3390/medicina61081328
Chicago/Turabian StylePanaite, Tinela, Cristian Liviu Romanec, Armencia Adina, Balcos Carina, Carmen Savin, and Ana Sîrghie. 2025. "Psychosocial Determinants of Patient Satisfaction in Orthodontic Treatment: A Pilot Cross-Sectional Survey in North-Eastern" Medicina 61, no. 8: 1328. https://doi.org/10.3390/medicina61081328
APA StylePanaite, T., Romanec, C. L., Adina, A., Carina, B., Savin, C., & Sîrghie, A. (2025). Psychosocial Determinants of Patient Satisfaction in Orthodontic Treatment: A Pilot Cross-Sectional Survey in North-Eastern. Medicina, 61(8), 1328. https://doi.org/10.3390/medicina61081328






