Differences in Kinematic and Muscle Activity Between ACL Injury Risk and Healthy Players in Female Football: Influence of Change of Direction Amplitude in a Cross-Sectional Case–Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Marker and EMG Sensor Placement
2.4. Data Analysis
2.5. Sample Size
2.6. Statistical Analysis
3. Results
| Variable—Knee Kinematic | Mean Difference | p Value | 95% Confidence Intervals for Differences | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Sagittal Plane (Significant Main effects of Task) | |||||
| Peak Knee Flexion–Extension Angular Velocity | CODAT and GOB | 59.82 | 0.247 | −46.12 | 165.76 |
| CODAT and TURN | 93.29 | 0.035 * | 3.55 | 82.00 | |
| GOB and TURN | 33.47 | 0.046 * | 2.18 | 208.61 | |
| Transverse Plane (Significant Main effects of Group) | |||||
| Knee Internal–External Rotation Angle ROM | Injured and Healthy | 4.66 | 0.006 * | 1.42 | 7.89 |
| Minimum Knee External Rotation Angular Velocity | Injured and Healthy | 71.54 | 0.034 * | 5.92 | 137.15 |
| Variable—Muscle Activity EMG | |||||
| (Significant Main effects of Task) | |||||
| Average Biceps Femoris Load Phase | CODAT and GOB | 0.05 | 0.034 * | 0.00 | 0.10 |
| CODAT and TURN | 0.01 | 0.812 | −0.05 | 0.06 | |
| GOB and TURN | −0.05 | 0.040 * | −0.09 | −0.00 | |
| Average Vastus Medialis Load Phase | CODAT and GOB | 0.04 | 0.030 * | 0.01 | 0.08 |
| CODAT and TURN | −0.01 | 0.711 | −0.05 | 0.04 | |
| GOB and TURN | −0.05 | 0.046 * | −0.10 | −0.00 | |
| Peak Vastus Medialis Load Phase | CODAT and GOB | 0.24 | 0.018 * | 0.05 | 0.43 |
| CODAT and TURN | 0.06 | 0.535 | −0.13 | 0.25 | |
| GOB and TURN | −0.18 | 0.080 | −0.39 | 0.02 | |
| (Significant Main effects of Group) | |||||
| Average Vastus Medialis Load Phase | Injured and Healthy | 0.04 | 0.031 * | 0.00 | 0.08 |
| Average Lateral Gastrocnemius Load Phase | Injured and Healthy | 0.04 | 0.036 * | 0.00 | 0.08 |
| Variable Peak Lateral Gastrocnemius Load Phase | Mean Difference | p Value | 95% Confidence Intervals for Differences | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| CODAT | Injured and Healthy | −0.17 | 0.203 | −0.45 | 0.10 |
| GOB | Injured and Healthy | −0.09 | 0.616 | −0.44 | 0.27 |
| TURN | Injured and Healthy | 0.33 | 0.022 * | 0.05 | 0.60 |
4. Discussion
4.1. Limitations
4.2. Clinical Contributions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACL | Anterior Cruciate Ligament |
| EMG | Electromyography |
| ST | Semitendinosus |
| BF | Biceps Femoris |
| VM | Vastus Medialis |
| LG | Lateral Gastrocnemius |
| PREP | Preparation phase |
| LOAD | Load phase |
References
- Hallén, A.; Tomás, R.; Ekstrand, J.; Bengtsson, H.; Van den Steen, E.; Hägglund, M.; Waldén, M. UEFA Women’s Elite Club Injury Study: A prospective study on 1527 injuries over four consecutive seasons 2018/2019 to 2021/2022 reveals thigh muscle injuries to be most common and ACL injuries most burdensome. Br. J. Sports Med. 2024, 58, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Lima, Y.L.; Collings, T.J.; Hall, M.; Bourne, M.N.; Diamond, L.E. Injury Prevention Programmes Fail to Change Most Lower Limb Kinematics and Kinetics in Female Team Field and Court Sports: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Sports Med. 2024, 54, 933–952. [Google Scholar] [CrossRef]
- Larruskain, J.; Lekue, J.A.; Angulo, P.; Santisteban, J.M.; Diaz-Beitia, G.; Martin-Garetxana, I.; Gil, S.M.; Bidaurrazaga-Letona, I.; Monasterio, X. An injury burden heat map of all men’s and women’s teams of a professional football club over a decade. Sports Med. 2024, 32, 740–750. [Google Scholar] [CrossRef]
- Ferrández-Laliena, L.; Sánchez-Rodríguez, R.; Vicente-Pina, L.; Lucha-López, M.O.; Ambrus, M.; Hidalgo-García, C.; Monti-Ballano, S.; Tricás-Moreno, J.M. Comparative Analysis of Neuromuscular Activation Patterns Associated with Force between Semi-Professional Female Soccer Players with Previous Anterior Cruciate Ligament Surgery and Healthy Players in Thigh Musculature Related to Valgus Collapse. Appl. Sci. 2024, 14, 6869. [Google Scholar] [CrossRef]
- Ramachandran, A.K.; Pedley, J.S.; Moeskops, S.; Oliver, J.L.; Myer, G.D.; Lloyd, R.S. Changes in Lower Limb Biomechanics Across Various Stages of Maturation and Implications for ACL Injury Risk in Female Athletes: A Systematic Review. Sports Med. 2024, 54, 1851–1876. [Google Scholar] [CrossRef]
- Hamoongard, M.; Letafatkar, A.; Thomas, A.C. The Effect of Neurocognitive Training on Biomechanical Risk Factors Related to Anterior Cruciate Ligament Injury in Athletes: A Narrative Review. J. Sport Rehabil. 2024, 33, 485–494. [Google Scholar] [CrossRef]
- Alenezi, F.; Herrington, L.; Jones, P.; Jones, R. Knee valgus angle and loading across common athletic tasks; reference values and gender differences in a healthy population. Br. J. Sports Med. 2017, 5, 286. [Google Scholar] [CrossRef]
- Chia, L.; Myer, G.D.; Hewett, T.E.; McKay, M.J.; Sullivan, J.; Ford, K.R.; Pappas, E. When puberty strikes: Longitudinal changes in cutting kinematics in 172 high-school female athletes. J. Sci. Med. Sport. 2021, 24, 1290–1295. [Google Scholar] [CrossRef]
- Dix, C.; Arundale, A.; Silvers-Granelli, H.; Marmon, A.; Zarzycki, R.; Snyder-Mackler, L. Biomechanical measures during two sport-specific tasks differentiate between soccer players who go on to anterior cruciate ligament injury and those who do not: A prospective cohort analysis. Int. J. Sports. Phys. Ther. 2020, 15, 928–935. [Google Scholar] [CrossRef]
- Zebis, M.K.; Aagaard, P.; Andersen, L.L.; Hölmich, P.; Clausen, M.B.; Brandt, M.; Husted, R.S.; Lauridsen, H.B.; Curtis, D.J.; Bencke, J. First-time anterior cruciate ligament injury in adolescent female elite athletes: A prospective cohort study to identify modifiable risk factors. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1341. [Google Scholar] [CrossRef]
- Aoki, A.; Kubota, S.; Morinaga, K.; Zheng, N.N.; Wang, S.S.; Gamada, K. Detection of knee wobbling as a screen to identify athletes who may be at high risk for ACL injury. Int. Biomech. 2021, 8, 30–41. [Google Scholar] [CrossRef]
- Wakabayashi, K.; Ogasawara, I.; Suzuki, Y.; Nakata, K.; Nomura, T. Exploring pre-impact landing kinematics associated with increase and decrease in the anterior cruciate ligament injury risk. J. Biomech. 2022, 145, 111382. [Google Scholar] [CrossRef]
- Nasseri, A.; Lloyd, D.G.; Bryant, A.L.; Headrick, J.; Sayer, T.A.; Saxby, D.J. Mechanism of Anterior Cruciate Ligament Loading during Dynamic Motor Tasks. Med. Sci. Sports Exerc. 2021, 53, 1235–1244. [Google Scholar] [CrossRef]
- Nagano, Y.; Ida, H.; Akai, M.; Fukubayashi, T. Biomechanical characteristics of the knee joint in female athletes during tasks associated with anterior cruciate ligament injury. Knee 2009, 16, 153–158. [Google Scholar] [CrossRef]
- Kikuchi, N.; Kanamori, A.; Kadone, H.; Kajiwara, M.; Okuno, K.; Hyodo, K.; Yamazaki, M. Relationship Between Posterior Tibial Slope and Lower Extremity Biomechanics During a Single-Leg Drop Landing Combined with a Cognitive Task in Athletes After ACL Reconstruction. Orthop. J. Sports Med. 2022, 10, 23259671221107931. [Google Scholar] [CrossRef]
- Jeong, J.; Choi, D.H.; Shin, C.S. Association Between the Medial-Lateral Quadriceps and Hamstring Muscle Thickness and the Knee Kinematics and Kinetics During Single-Leg Landing. Sports Health 2023, 15, 519–526. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S.; Colosimo, A.J.; McLean, S.G.; Van Den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Mokhtarzadeh, H.; Yeow, C.H.; Hong-Goh, J.C.; Oetomo, D.; Malekipour, F.; Lee, P.V.S. Contributions of the Soleus and Gastrocnemius muscles to the anterior cruciate ligament loading during single-leg landing. J. Biomech. 2013, 46, 1913–1920. [Google Scholar] [CrossRef]
- Picot, B.; Lempereur, M.; Morel, B.; Forestier, N.; Rémy-Néris, O. Lack of Proprioceptive Strategy Modulation Leads to At-Risk Biomechanics for Anterior Cruciate Ligament in Healthy Athletes. Med. Sci. Sports Exerc. 2024, 56, 942–952. [Google Scholar] [CrossRef]
- Behnke, A.L.; Parola, L.R.; Karamchedu, N.P.; Badger, G.J.; Fleming, B.C.; Beveridge, J.E. Neuromuscular function in anterior cruciate ligament reconstructed patients at long-term follow-up. Clin. Biomech. 2021, 81, 105231. [Google Scholar] [CrossRef]
- Lucarno, S.; Zago, M.; Buckthorpe, M.; Grassi, A.; Tosarelli, F.; Smith, R.; Della Villa, F. Systematic Video Analysis of Anterior Cruciate Ligament Injuries in Professional Female Soccer Players. Am. J. Sports Med. 2021, 49, 1794–1802. [Google Scholar] [CrossRef] [PubMed]
- Ebner, C.; Granacher, U.; Gehring, D. Effects of Anticipation and Dual-Tasking on Lower Limb Biomechanics While Performing Change-of-Direction Tasks in Physically Active Individuals: A Systematic Review with Meta-Analysis. Sports Med. 2025, 55, 857–876. [Google Scholar] [CrossRef]
- Bencke, J.; Zebis, M.K. The influence of gender on neuromuscular pre-activity during side-cutting. J. Electromyogr. Kinesiol. 2011, 21, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Di Paolo, S.; Bragonzoni, L.; Della-Villa, F.; Grassi, A.; Zaffagnini, S. Do healthy athletes exhibit at-risk biomechanics for anterior cruciate ligament injury during pivoting movements? Sports Biomech. 2024, 2, 2995–3008. [Google Scholar] [CrossRef] [PubMed]
- Navacchia, A.; Ueno, R.; Ford, K.R.; DiCesare, C.A.; Myer, G.D.; Hewett, T.E. EMG-Informed Musculoskeletal Modeling to Estimate Realistic Knee Anterior Shear Force During Drop Vertical Jump in Female Athletes. Ann. Biomed. Eng. 2019, 47, 2416–2430. [Google Scholar] [CrossRef]
- Zebis, M.K.; Andersen, L.L.; Bencke, J.; Kjær, M.; Aagaard, P. Identification of athletes at future risk of anterior cruciate ligament ruptures by neuromuscular screening. Am. J. Sports Med. 2009, 37, 1967–1973. [Google Scholar] [CrossRef] [PubMed]
- Ferrández-Laliena, L.; Vicente-Pina, L.; Sánchez-Rodríguez, R.; Orantes-González, E.; Heredia-Jimenez, J.; Lucha-López, M.O.; Hidalgo-García, C.; Tricás-Moreno, J.M. Diagnostics Using the Change-of-Direction and Acceleration Test (CODAT) of the Biomechanical Patterns Associated with Knee Injury in Female Futsal Players: A Cross-Sectional Analytical Study. Diagnostics 2023, 13, 928. [Google Scholar] [CrossRef]
- Arundale, A.J.H.; Bizzini, M.; Giordano, A.; Hewett, T.E.; Logerstedt, D.S.; Mandelbaum, B.; Scalzitti, D.A.; Silvers-Granelli, H.; Snyder-Mackler, L.; Altman, R.D.; et al. Exercise-based knee and anterior cruciate ligament injury prevention. J. Orthop. Sports Phys. Ther. 2018, 48, A1–A42. [Google Scholar] [CrossRef]
- World Medical Association. Ethical principles for medical research involving human subjects. Eur. J. Emerg. Med. 2001, 8, 221–223. [Google Scholar] [CrossRef]
- Brophy, R.H.; Stepan, J.G.; Silvers, H.J.; Mandelbaum, B.R. Defending Puts the Anterior Cruciate Ligament at Risk During Soccer: A Gender-Based Analysis. Sports Health 2015, 7, 244. [Google Scholar] [CrossRef]
- Lockie, R.G.; Schultz, A.B.; Callaghan, S.J.; Jeffriess, M.D.; Berry, S.P. Reliability and Validity of a New Test of Change-of-Direction Speed for Field-Based Sports: The Change-of-Direction and Acceleration Test (CODAT). J. Sports Sci. Med. 2013, 12, 88–96. [Google Scholar] [PubMed]
- Di Paolo, S.; Zaffagnini, S.; Tosarelli, F.; Aggio, F.; Bragonzoni, L.; Grassi, A.; Della Villa, F. A 2D qualitative movement assessment of a deceleration task detects football players with high knee joint loading. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 4032–4404. [Google Scholar] [CrossRef] [PubMed]
- Chattanta, V.; Verma, N.; Mehra, P. Quantifying the difference between male and female agility in football players: A cross-sectional study. Phys. Ther. Sport. 2024, 1, 90–94. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Watcharakhueankhan, P.; Chapman, G.J.; Sinsurin, K.; Jaysrichai, T.; Richards, J. The immediate effects of Kinesio Taping on running biomechanics, muscle activity, and perceived changes in comfort, stability and running performance in healthy runners, and the implications to the management of Iliotibial band syndrome. Gait Posture 2022, 91, 179–185. [Google Scholar] [CrossRef]
- Hanzlíková, I.; Richards, J.; Hébert-Losier, K.; Smékal, D. The effect of proprioceptive knee bracing on knee stability after anterior cruciate ligament reconstruction. Gait Posture 2019, 67, 242–247. [Google Scholar] [CrossRef]
- Karacan, I.; Topkara-Arslan, B.; Karaoglu, A.; Aydin, T.; Gray, S.; Ungan, P.; Türker, K.S. Estimating and minimizing movement artifacts in surface electromyogram. J. Electromyogr. Kinesiol. 2023, 70, 102778. [Google Scholar] [CrossRef]
- Ruan, M.; Zhang, Q.; Wu, X. Acute effects of static stretching of hamstring on performance and anterior cruciate ligament injury risk during stop-jump and cutting tasks in female athletes. J. Strength Cond. Res. 2017, 31, 1241–1250. [Google Scholar] [CrossRef]
- Bates, N.A.; Schilaty, N.D.; Nagelli, C.V.; Krych, A.J.; Hewett, T.E. Multiplanar Loading of the Knee and Its Influence on Anterior Cruciate Ligament and Medial Collateral Ligament Strain During Simulated Landings and Noncontact Tears. Am. J. Sports Med. 2019, 47, 1844–1853. [Google Scholar] [CrossRef] [PubMed]
- Markström, J.L.; Grinberg, Y.; Sole, G.; Häger, C.K. Strategies for knee stabilising and pivot-shift avoidance in a step-down and cross-over task observed sub-acutely after anterior cruciate ligament reconstruction. Clin. Biomech. 2024, 1, 115. [Google Scholar] [CrossRef]
- Bates, N.A.; Nesbitt, R.J.; Shearn, J.T.; Myer, G.D.; Hewett, T.E. The influence of internal and external tibial rotation offsets on knee joint and ligament biomechanics during simulated athletic tasks. Clin. Biomech. 2018, 1, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Torg, J.S.; Boden, B.P. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: Lateral trunk and knee abduction motion are combined components of the injury mechanism. Br. J. Sports Med. 2009, 43, 417–422. [Google Scholar] [CrossRef] [PubMed]
- McBurnie, A.J.; Dos’Santos, T.; Jones, P.A. Biomechanical Associates of Performance and Knee Joint Loads During A 70–90° Cutting90° Cutting Maneuver in Subelite Soccer Players. J. Strength Cond. Res. 2019, 35, 3190–3198. [Google Scholar] [CrossRef]
- Di Paolo, S.; Grassi, A.; Tosarelli, F.; Crepaldi, M.; Bragonzoni, L.; Zaffagnini, S.; Della Villa, F. Two-Dimensional and Three-Dimensional Biomechanical Factors During 90° Change of Direction are Associated to Non-Contact ACL injury in Female Soccer Players. Int. J. Sports Phys. Ther. 2023, 18, 887. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.; Landry, S.; Urquhart, N.; Coady, C.; Rutherford, D. Drop landing between subjects post anterior cruciate ligament reconstruction and uninjured controls: A biomechanical and neuromuscular analysis. Clin. Biomech. 2025, 124, 106504. [Google Scholar] [CrossRef]
- Thomas, C.; Dos’Santos, T.; Comfort, P.; Jones, P.A. Male and female soccer players exhibit different knee joint mechanics during pre-planned change of direction. Sports Biomech. 2020, 23, 118–131. [Google Scholar] [CrossRef]


| Total (n = 16) | Injured (n = 8) | Healthy (n = 8) | |
|---|---|---|---|
| Age (years) | 23.93 ± 5.16 | 23.00 ± 4.04 | 24.75 ± 6.13 |
| Position (Goalkeeper/Back/Wing/Pivot) | 3:4:7:2 | 1:3:3:1 | 2:1:4:1 |
| Height (cm) | 161.24 ± 5.41 | 162.71 ± 5.87 | 159.95 ± 4.97 |
| Limb dominance (Right/Left) | 13:3 | 6:2 | 7:1 |
| Football Experience | 15.75 ± 1.98 | 16.63 ± 1.19 | |
| Injury limb (Dominant Limb/Non-Dominant Limb) | 4:4 | 4:4 |
| CODAT | GOB | TURN | Task p Value | Injured p Value | Interaction Effect | ||||
|---|---|---|---|---|---|---|---|---|---|
| Injured | Healthy | Injured | Healthy | Injured | Healthy | ||||
| Variables | |||||||||
| Sagittal Plane | |||||||||
| Joint Angle | |||||||||
| Minimum Knee Flexion Angle | 19.06 ± 4.49 | 23.64 ± 8.77 | 20.10 ± 4.49 | 21.22 ± 11.96 | 22.65 ± 2.26 | 23.83 ± 9.11 | 0.599 | 0.307 | 0.741 |
| Peak Knee Flexion–Extension Angle | −53.64 ± 8.46 | 54.30 ± 12.04 | −62.26 ± 10.18 | 59.46 ± 8.18 | −60.01 ± 10.69 | 58.41 ± 14.88 | 0.150 | 0.696 | 0.884 |
| Knee Flexion–Extension Angle ROM | −34.59 ± 9.05 | 30.66 ± 11.17 | 42.16 ± 10.04 | 38.23 ± 10.91 | 37.36 ± 11.57 | 34.59 ± 9.05 | 0.134 | 0.265 | 0.986 |
| Angular Velocity | |||||||||
| Minimum Knee Flexion Angular Velocity | −517.30 ± 127.17 | −501.68 ± 126.55 | −462.53 ± 64.01 | −471.95 ± 11.96 | −536.92 ± 109.41 | −485.78 ± 124.02 | 0.380 | 0.556 | 0.710 |
| Peak Knee Flexion–Extension Angular Velocity | 46.24 ± 140.89 | 143.81 ± 224.30 | 11.79 ± 50.65 | 58.63 ± 77.11 | 7.32 ± 18.88 | −3.85 ± 19.01 | 0.049 * | 0.201 | 0.164 |
| Knee Flexion–Extension Angular Velocity ROM | 562.06 ± 201.87 | 643.98 ± 197.75 | 471.74 ± 77.73 | 524.55 ± 163.86 | 534.60 ± 110.51 | 464.36 ± 119.65 | 0.184 | 0.628 | 0.264 |
| Coronal Plane | |||||||||
| Joint Angle | |||||||||
| Minimum Knee Abduction Angle | −6.67 ± 5.59 | −7.87 ± 4.24 | −4.42 ± 5.37 | −8.80 ± 6.96 | −7.07 ± 5.81 | −6.65 ± 4.99 | 0.942 | 0.289 | 0.511 |
| Peak Knee Abduction–Adduction Angle | 0.90 ± 3.39 | −2.25 ± 3.99 | 2.68 ± 5.72 | 2.91 ± 7.55 | 0.67 ± 3.54 | 1.76 ± 6.80 | 0.173 | 0.698 | 0.385 |
| Knee Abduction–Adduction Angle ROM | 7.58 ± 4.37 | 5.62 ± 2.52 | 7.09 ± 2.78 | 11.71 ± 5.50 | −7.73 ± 2.92 | 8.41 ± 3.87 | 0.152 | 0.320 | 0.086 |
| Angular Velocity | |||||||||
| Minimum Knee Abduction Angular Velocity | −118.01 ± 76.41 | −114.89 ± 37.91 | −138.28 ± 77.59 | −133.43 ± 45.78 | −154.99 ± 137.08 | −105.27 ± 51.92 | 0.672 | 0.405 | 0.721 |
| Peak Knee Adduction Angular Velocity | 196.10 ± 73.84 | 140.87 ± 98.07 | 183.62 ± 73.92 | 175.43 ± 85.87 | 244.57 ± 97.19 | 179.37 ± 91.62 | 0.388 | 0.097 | 0.601 |
| Knee Abduction–Adduction Angular Velocity ROM | 314.11 ± 123.82 | 255.76 ± 127.85 | 321.90 ± 148.60 | 308.86 ± 92.26 | 399.56 ± 223.63 | 284.64 ± 108.42 | 0.557 | 0.145 | 0.636 |
| Transverse Plane | |||||||||
| Joint Angle | |||||||||
| Minimum Knee External Rotation Angle | −1.55 ± 8.45 | −0.97 ± 8.48 | −6.89 ± 9.86 | −4.18 ± 9.51 | −6.16 ± 9.22 | −2.44 ± 7.35 | 0.386 | 0.365 | 0.867 |
| Peak Knee Internal Rotation Angle | 11.55 ± 7.96 | 8.19 ± 7.33 | 6.54 ± 6.65 | 7.92 ± 8.63 | 11.15 ± 6.23 | 6.19 ± 5.76 | 0.626 | 0.269 | 0.435 |
| Knee Internal–External Rotation Angle ROM | 13.11 ± 5.21 | 9.16 ± 4.40 | 13.43 ± 5.09 | 12.10 ± 5.54 | 17.31 ± 7.37 | 8.63 ± 5.14 | 0.558 | 0.006 * | 0.223 |
| Angular Velocity | |||||||||
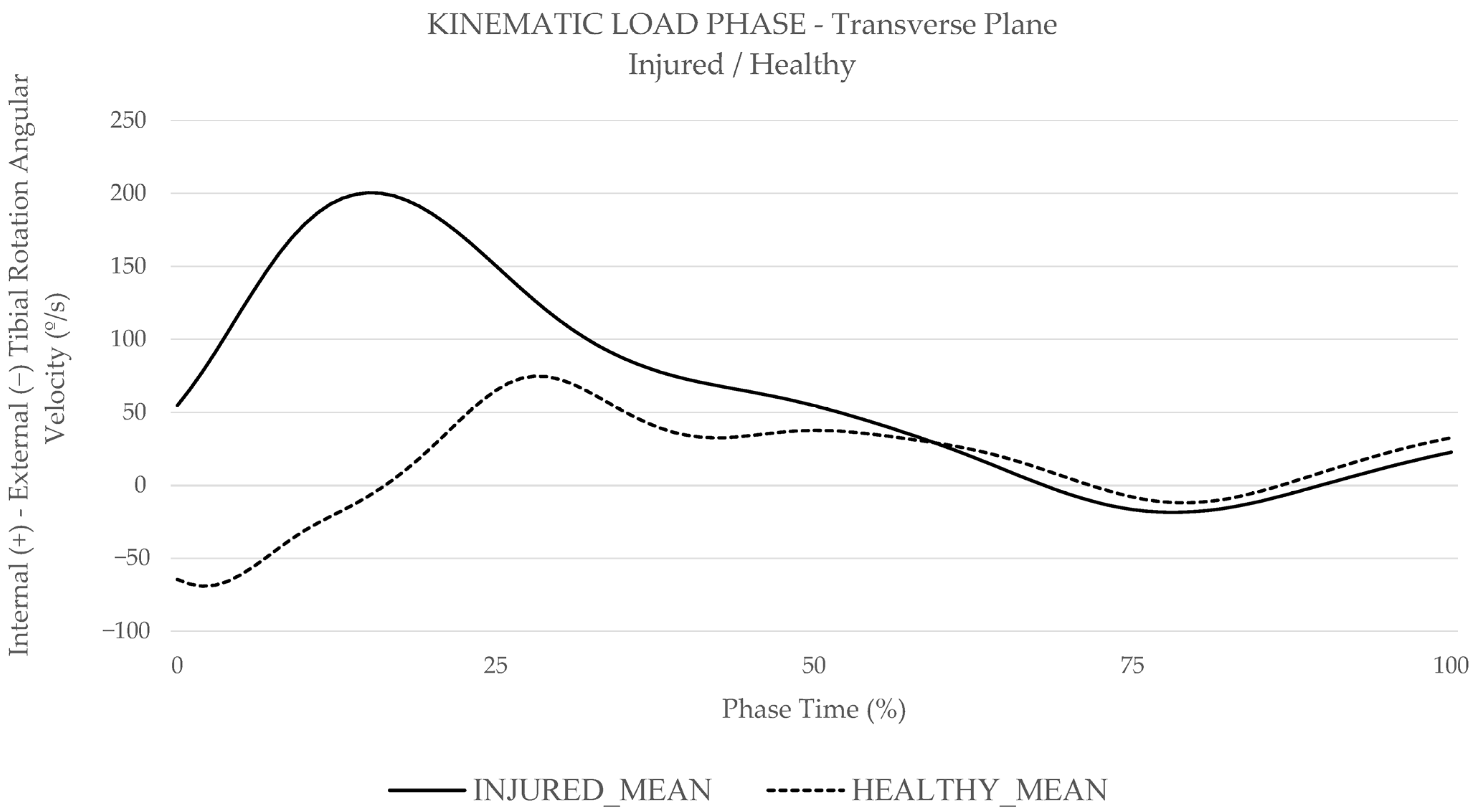
| Minimum Knee External Rotation Angular Velocity | −96.61 ± 92.06 | −164.32 ± 145.82 | −173.90 ± 120.09 | −254.06 ± 134.48 | −109.27 ± 58.56 | −176.00 ± 96.89 | 0.129 | 0.034 * | 0.983 |
| Peak Knee Internal Rotation Angular Velocity | 253.16 ± 155.06 | 215.68 ± 126.86 | 270.14 ± 124.14 | 233.24 ± 115.39 | 366.58 ± 200.39 | 215.80 ± 88.08 | 0.552 | 0.071 | 0.461 |
| Knee Internal–External Rotation Angular Velocity ROM | 349.77 ± 225.48 | 380.00 ± 249.73 | 444.04 ± 116.70 | 487.30 ± 221.62 | 475.85 ± 206.39 | 391.81 ± 141.91 | 0.411 | 0.952 | 0.564 |
| CODAT | GOB | TURN | Task p Value | Group p Value | Interaction Effect | ||||
|---|---|---|---|---|---|---|---|---|---|
| Injured | Healthy | Injured | Healthy | Injured | Healthy | ||||
| Variables | |||||||||
| Average Biceps Femoris | 0.14 ± 0.05 | 0.13 ± 0.11 | 0.12 ± 0.04 | 0.10 ± 0.07 | 0.15 ± 0.05 | 0.14 ± 0.12 | 0.326 | 0.483 | 0.893 |
| Peak Biceps Femoris | 0.63 ± 0.24 | 0.59 ± 0.37 | 0.51 ± 0.12 | 0.38 ± 0.25 | 0.68 ± 0.26 | 0.53 ± 0.42 | 0.122 | 0.206 | 0.842 |
| Average Semitendinosus | 0.17 ± 0.09 | 0.15 ± 0.05 | 0.19 ± 0.05 | 0.16 ± 0.06 | 0.19 ± 0.08 | 0.14 ± 0.07 | 0.791 | 0.097 | 0.887 |
| Peak Semitendinosus | 0.71 ± 0.33 | 0.75 ± 0.23 | 0.68 ± 0.20 | 0.63 ± 0.22 | 0.78 ± 0.24 | 0.63 ± 0.18 | 0.656 | 0.403 | 0.576 |
| Average Vastus Medialis | 0.11 ± 0.06 | 0.08 ± 0.05 | 0.08 ± 0.03 | 0.07 ± 0.04 | 0.10 ± 0.05 | 0.07 ± 0.05 | 0.335 | 0.092 | 0.867 |
| Peak Vastus Medialis | 0.49 ± 0.18 | 0.43 ± 0.31 | 0.47 ± 0.21 | 0.33 ± 0.18 | 0.53 ± 0.23 | 0.46 ± 0.25 | 0.420 | 0.197 | 0.850 |
| Average Lateral Gastrocnemius | 0.08 ± 0.06 | 0.08 ± 0.06 | 0.06 ± 0.04 | 0.07 ± 0.04 | 0.05 ± 0.02 | 0.05 ± 0.04 | 0.217 | 0.618 | 0.959 |
| Peak Lateral Gastrocnemius | 0.40 ± 0.18 | 0.48 ± 0.31 | 0.26 ± 0.19 | 0.35 ± 0.25 | 0.38 ± 0.25 | 0.31 ± 0.29 | 0.274 | 0.612 | 0.633 |
| CODAT | GOB | TURN | Task p Value | Group p Value | Interaction Effect | ||||
|---|---|---|---|---|---|---|---|---|---|
| Injured | Healthy | Injured | Healthy | Injured | Healthy | ||||
| Variables | |||||||||
| Average Biceps Femoris | 0.16 ± 0.06 | 0.13 ± 0.09 | 0.10 ± 0.03 | 0.08 ± 0.07 | 0.15 ± 0.04 | 0.13 ± 0.08 | 0.042 * | 0.208 | 0.884 |
| Peak Biceps Femoris | 0.78 ± 0.25 | 0.69 ± 0.31 | 0.59 ± 0.25 | 0.47 ± 0.40 | 0.71 ± 0.26 | 0.67 ± 0.34 | 0.188 | 0.376 | 0.946 |
| Average Semitendinosus | 0.11 ± 0.06 | 0.14 ± 0.07 | 0.10 ± 0.02 | 0.10 ± 0.05 | 0.13 ± 0.07 | 0.11 ± 0.05 | 0.264 | 0.755 | 0.653 |
| Peak Semitendinosus | 0.64 ± 0.35 | 0.74 ± 0.24 | 0.52 ± 0.12 | 0.63 ± 0.28 | 0.59 ± 0.27 | 0.73 ± 0.26 | 0.395 | 0.143 | 0.969 |
| Average Vastus Medialis | 0.20 ± 0.05 | 0.12 ± 0.07 | 0.13 ± 0.05 | 0.10 ± 0.07 | 0.17 ± 0.06 | 0.16 ± 0.09 | 0.052 * | 0.031 * | 0.153 |
| Peak Vastus Medialis | 0.91 ± 0.14 | 0.73 ± 0.31 | 0.68 ± 0.25 | 0.49 ± 0.32 | 0.71 ± 0.23 | 0.81 ± 0.32 | 0.051 * | 0.253 | 0.245 |
| Average Lateral Gastrocnemius | 0.15 ± 0.07 | 0.14 ± 0.07 | 0.12 ± 0.07 | 0.08 ± 0.04 | 0.15 ± 0.08 | 0.08 ± 0.04 | 0.174 | 0.036 * | 0.433 |
| Peak Lateral Gastrocnemius | 0.69 ± 0.28 | 0.86 ± 0.23 | 0.52 ± 0.31 | 0.60 ± 0.35 | 0.79 ± 0.26 | 0.46 ± 0.25 | 0.096 | 0.770 | 0.025 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrández-Laliena, L.; Vicente-Pina, L.; Sánchez-Rodríguez, R.; Chapman, G.J.; Heredia-Jimenez, J.; Hidalgo-García, C.; Tricás-Moreno, J.M.; Lucha-López, M.O. Differences in Kinematic and Muscle Activity Between ACL Injury Risk and Healthy Players in Female Football: Influence of Change of Direction Amplitude in a Cross-Sectional Case–Control Study. Medicina 2025, 61, 1259. https://doi.org/10.3390/medicina61071259
Ferrández-Laliena L, Vicente-Pina L, Sánchez-Rodríguez R, Chapman GJ, Heredia-Jimenez J, Hidalgo-García C, Tricás-Moreno JM, Lucha-López MO. Differences in Kinematic and Muscle Activity Between ACL Injury Risk and Healthy Players in Female Football: Influence of Change of Direction Amplitude in a Cross-Sectional Case–Control Study. Medicina. 2025; 61(7):1259. https://doi.org/10.3390/medicina61071259
Chicago/Turabian StyleFerrández-Laliena, Loreto, Lucía Vicente-Pina, Rocío Sánchez-Rodríguez, Graham J Chapman, Jose Heredia-Jimenez, César Hidalgo-García, José Miguel Tricás-Moreno, and María Orosia Lucha-López. 2025. "Differences in Kinematic and Muscle Activity Between ACL Injury Risk and Healthy Players in Female Football: Influence of Change of Direction Amplitude in a Cross-Sectional Case–Control Study" Medicina 61, no. 7: 1259. https://doi.org/10.3390/medicina61071259
APA StyleFerrández-Laliena, L., Vicente-Pina, L., Sánchez-Rodríguez, R., Chapman, G. J., Heredia-Jimenez, J., Hidalgo-García, C., Tricás-Moreno, J. M., & Lucha-López, M. O. (2025). Differences in Kinematic and Muscle Activity Between ACL Injury Risk and Healthy Players in Female Football: Influence of Change of Direction Amplitude in a Cross-Sectional Case–Control Study. Medicina, 61(7), 1259. https://doi.org/10.3390/medicina61071259







