Quantitative and Qualitative Segmental Surface Growth in Infants with Unilateral Cleft Lip and Palate: A Prospective In Vivo Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
2.2. Patients
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Sample Size Calculation
2.6. Data Collection
2.7. Statistical Analysis
3. Results
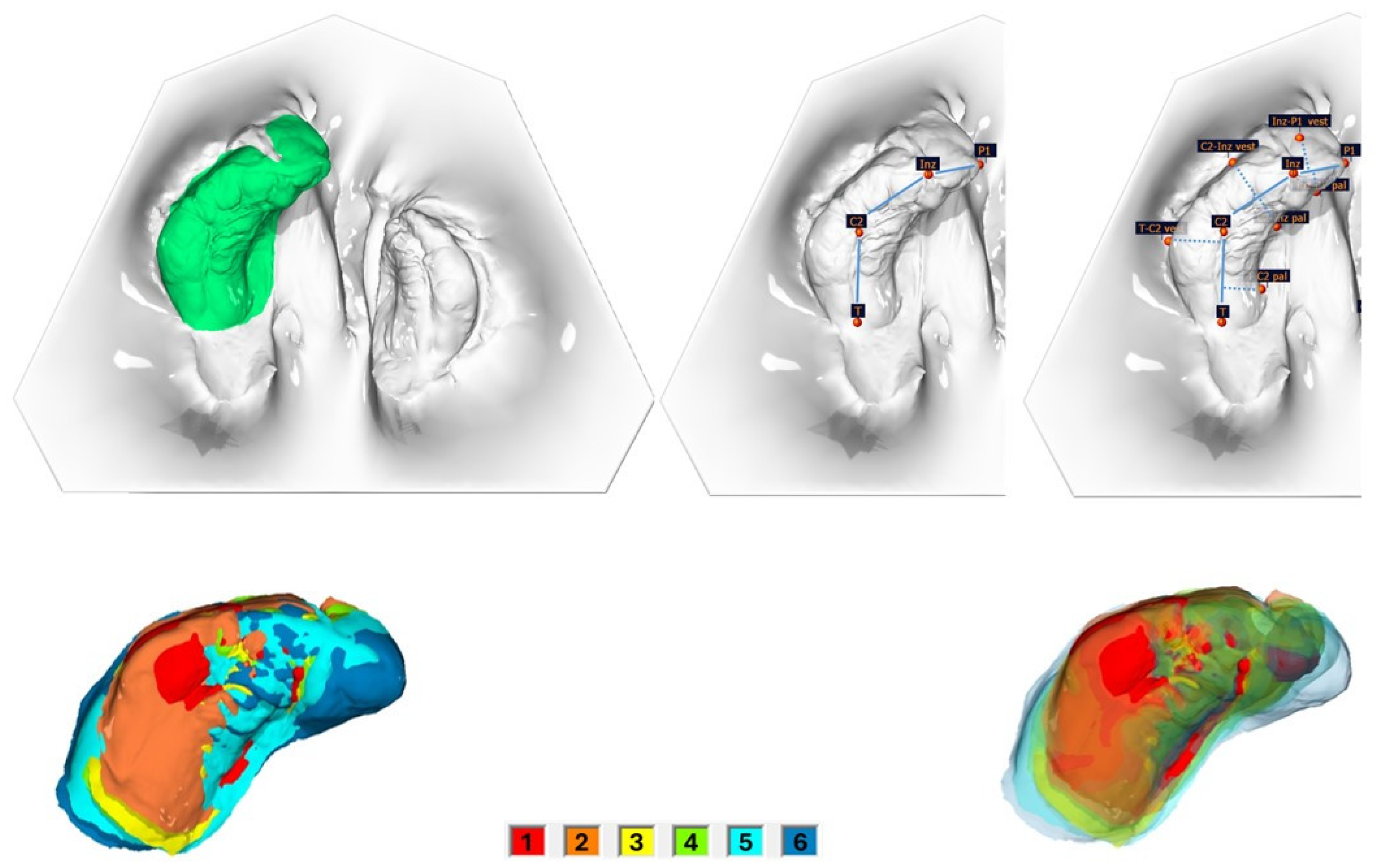
3.1. Quantitative Analysis
3.2. Qualitative Analysis
3.2.1. Transversal Changes Between Segments
3.2.2. Segmental Length and Width of the Segments
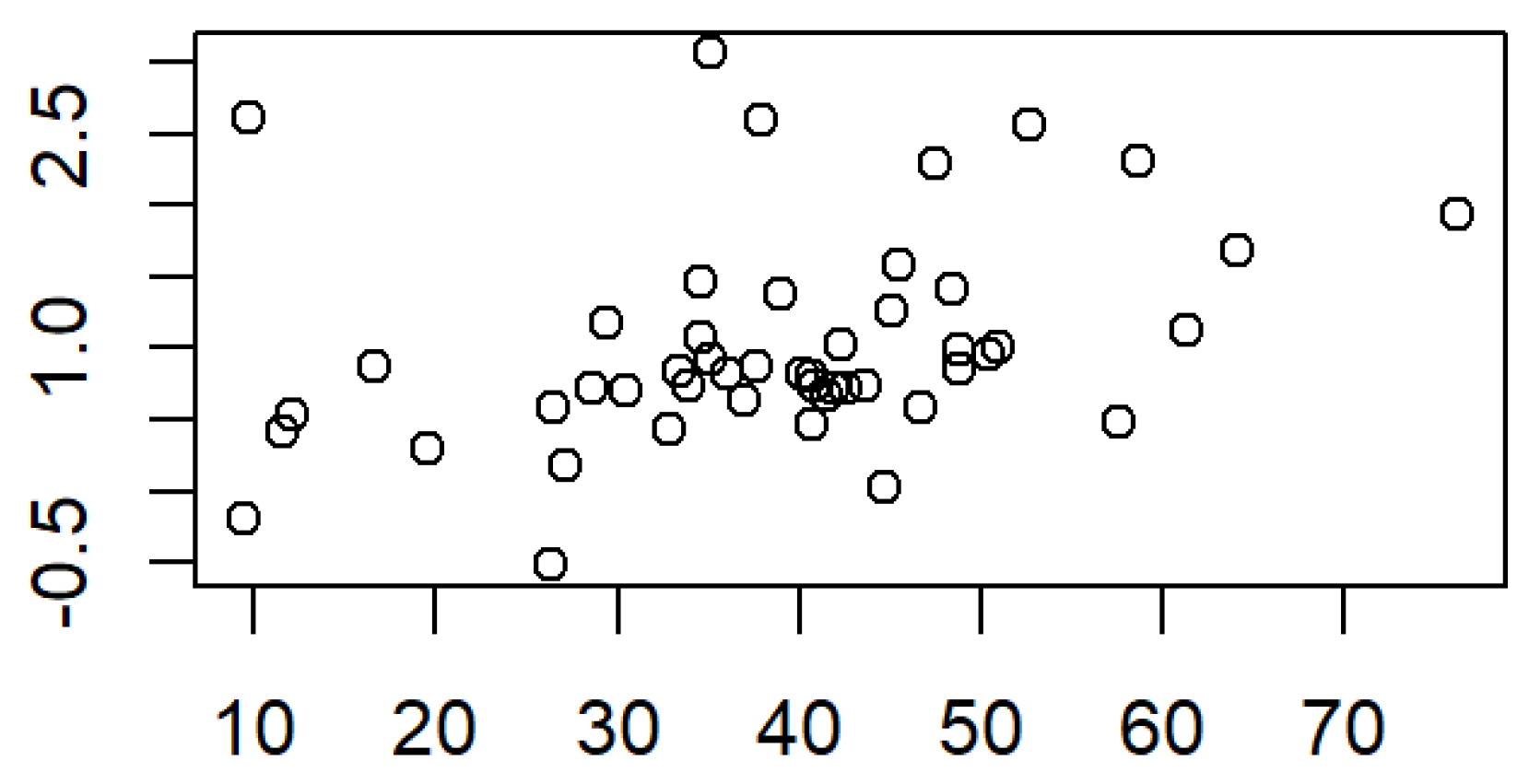
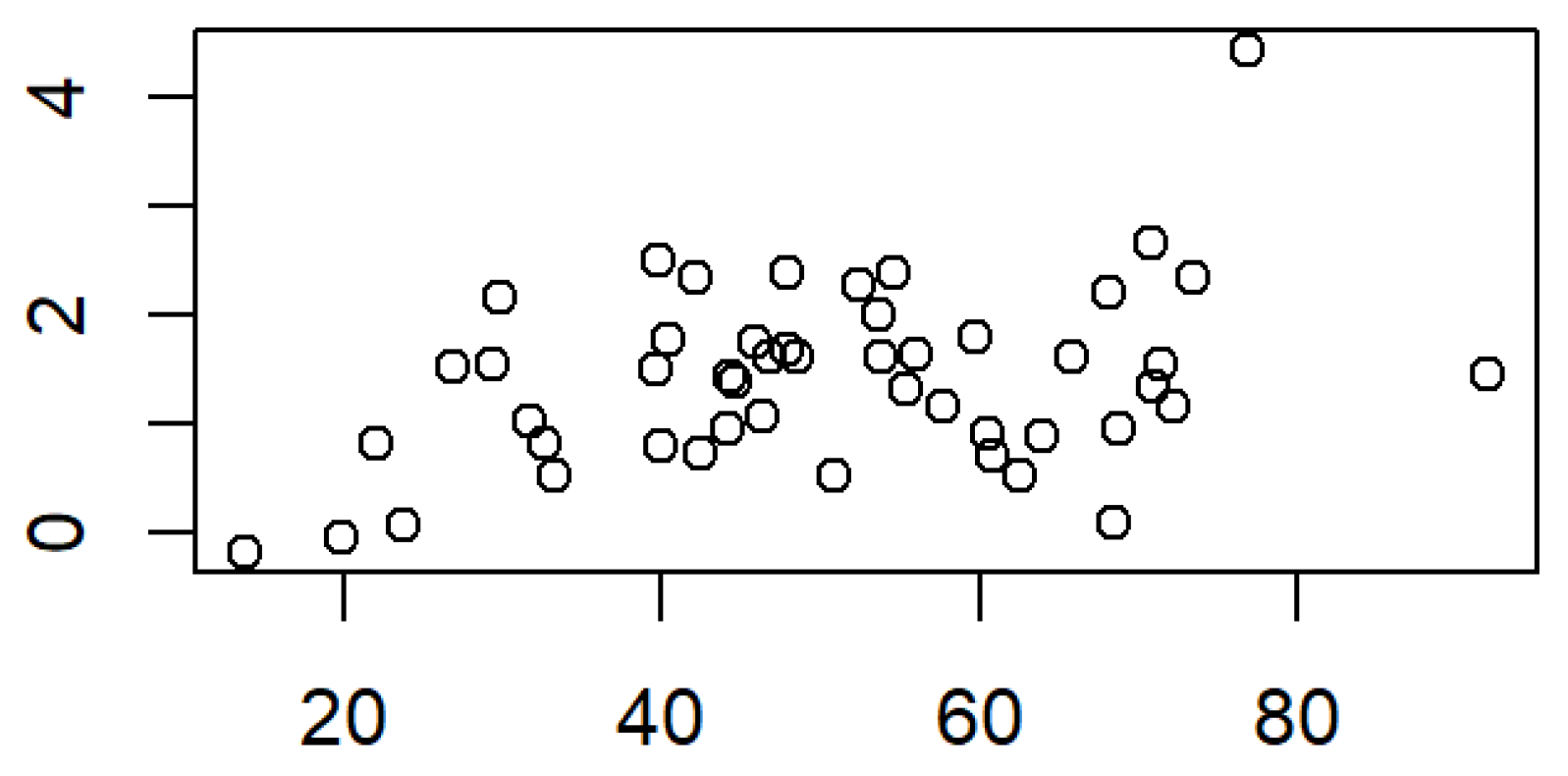
3.2.3. Correlation Between Surface and Segmental Length and Width
3.3. Angle Measurements
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| UCLP | Unilateral Cleft Lip and Palate |
| PSIO | Pre-Surgical Infant Orthopedics |
References
- Rahimov, F.; Jugessur, A.; Murray, J.C. Genetics of nonsyndromic orofacial clefts. Cleft Palate Craniofacial J. 2012, 49, 73–91. [Google Scholar] [CrossRef]
- Ambrosio, E.C.P.; Sforza, C.; De Menezes, M.; Gibelli, D.; Codari, M.; Carrara, C.F.C.; Machado, M.; Oliveira, T.M. Longitudinal morphometric analysis of dental arch of children with cleft lip and palate: 3D stereophotogrammetry study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 126, 463–468. [Google Scholar] [CrossRef]
- Sofi-Mahmudi, A.; Shamsoddin, E.; Khademioore, S.; Khazaei, Y.; Vahdati, A.; Tovani-Palone, M.R. Global, regional, and national survey on burden and Quality of Care Index (QCI) of orofacial clefts: Global burden of disease systematic analysis 1990–2019. PLoS ONE 2025, 20, e0317267. [Google Scholar] [CrossRef]
- Freitas, J.A.; das Neves, L.T.; de Almeida, A.L.; Garib, D.G.; Trindade-Suedam, I.K.; Yaedú, R.Y.; Lauris Rde, C.; Soares, S.; Oliveira, T.M.; Pinto, J.H. Rehabilitative treatment of cleft lip and palate: Experience of the Hospital for Rehabilitation of Craniofacial Anomalies/USP (HRAC/USP)—Part 1: Overall aspects. J. Appl. Oral. Sci. 2012, 20, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Kozelj, V. Changes produced by presurgical orthopedic treatment before cheiloplasty in cleft lip and palate patients. Cleft Palate Craniofacial J. 1999, 36, 515–521. [Google Scholar] [CrossRef][Green Version]
- Kriens, O.; Bertzbach, P. Model analysis of the maxilla in newborn infants with unilateral cheilognathopalatoschisis. Fortschr. Kieferorthop. 1986, 47, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Sillman, J.H. Relationship of maxillary and mandibular gum pads in the newborn infant. Am. J. Orthod. Oral Surg. 1938, 24, 409–424. [Google Scholar] [CrossRef]
- Stöckli, P.W. Application of a quantitative method for arch form evaluation in complete unilateral cleft lip and palate. Cleft Palate J. 1971, 8, 322–341. [Google Scholar]
- Wada, T.; Miyazaki, T. Growth and changes in maxillary arch form in complete unilateral cleft lip and cleft palate children. Cleft Palate J. 1975, 12, 115–130. [Google Scholar]
- Kriens, O. Data-objective diagnosis of infant cleft lip, alveolus, and palate. Morphologic data guiding understanding and treatment concepts. Cleft Palate Craniofacial J. 1991, 28, 157–168. [Google Scholar] [CrossRef]
- Kahl, B. The early treatment of children with cheilognathopalatoschisis—The orthodontic aspects. Fortschr. Kieferorthop. 1990, 51, 218–225. [Google Scholar] [CrossRef] [PubMed]
- De Menezes, M.; Cerón-Zapata, A.M.; López-Palacio, A.M.; Mapelli, A.; Pisoni, L.; Sforza, C. Evaluation of a Three-Dimensional Stereophotogrammetric Method to Identify and Measure the Palatal Surface Area in Children with Unilateral Cleft Lip and Palate. Cleft Palate Craniofacial J. 2016, 53, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Braumann, B.; Keilig, L.; Bourauel, C.; Jäger, A. Three-dimensional analysis of morphological changes in the maxilla of patients with cleft lip and palate. Cleft Palate Craniofacial J. 2002, 39, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Berkowitz, S.; Duncan, R.; Evans, C.; Friede, H.; Kuijpers-Jagtman, A.M.; Prahl-Anderson, B.; Rosenstein, S. Timing of cleft palate closure should be based on the ratio of the area of the cleft to that of the palatal segments and not on age alone. Plast. Reconstr. Surg. 2005, 115, 1483–1499. [Google Scholar] [CrossRef]
- Darvann, T.A.; Hermann, N.V.; Ersbøll, B.K.; Kreiborg, S.; Berkowitz, S. Palatal surface area of maxillary plaster casts—A comparison between two-dimensional and three-dimensional measurements. Cleft Palate Craniofacial J. 2007, 44, 381–390. [Google Scholar] [CrossRef]
- Unnikrishnan, J.; Bakr, M.; Love, R.; Idris, G. The Accuracy of Digital Impressions versus Conventional Impressions in Neonates with Cleft Lip and/or Palate: A Laboratory-Based Study. Children 2024, 11, 827. [Google Scholar] [CrossRef]
- Bruggink, R.; Baan, F.; Kramer, G.; Claessens, C.; Kuijpers-Jagtman, A.M.; Bronkhorst, E.M.; Maal, T.J.J.; Ongkosuwito, E. The effect of lip closure on palatal growth in patients with unilateral clefts. PeerJ 2020, 8, e9631. [Google Scholar] [CrossRef]
- Hoffmannova, E.; Moslerová, V.; Dupej, J.; Borský, J.; Bejdová, Š.; Velemínská, J. Three-dimensional development of the upper dental arch in unilateral cleft lip and palate patients after early neonatal cheiloplasty. Int. J. Pediatr. Otorhinolaryngol. 2018, 109, 1–6. [Google Scholar] [CrossRef]
- Bruggink, R.; Baan, F.; Kramer, G.J.C.; Maal, T.J.J.; Kuijpers-Jagtman, A.M.; Bergé, S.J.; Bronkhorst, E.M.; Ongkosuwito, E.M. Three dimensional maxillary growth modeling in newborns. Clin. Oral Investig. 2019, 23, 3705–3712. [Google Scholar] [CrossRef]
- Bruggink, R.; Baan, F.; Kramer, G.J.C.; Kuijpers-Jagtman, A.M.; Bergé, S.J.; Maal, T.J.J.; Ongkosuwito, E.M. Symmetry of palatal shape during the first year of life in healthy infants. Clin. Oral Investig. 2021, 25, 1069–1076. [Google Scholar] [CrossRef]
- Rando, G.M.; Ambrosio, E.C.P.; Jorge, P.K.; Sforza, C.; Menezes, M.; de Almeida, A.; Soares, S.; Dalben, G.S.; Tonello, C.; Carrara, C.F.C.; et al. Three-Dimensional Anthropometric Analysis of the Effect of Lip Reconstructive Surgery on Children with Cleft Lip and Palate at Three Different Times. Children 2024, 11, 824. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Jorge, P.K.; Ambrosio, E.C.P.; Machado, M.; Oliveira, T.M.; de Almeida, A.; Soares, S. A Narrative Review on Non-Invasive Diagnostic Tools for the Analysis of Dental Arches in Orofacial Cleft Patients. Children 2022, 9, 1533. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.H.; Son, W.S. Difference in alveolar molding effect and growth in the cleft segments: 3-dimensional analysis of unilateral cleft lip and palate patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Neuschulz, J.; Schaefer, I.; Scheer, M.; Christ, H.; Braumann, B. Maxillary reaction patterns identified by three-dimensional analysis of casts from infants with unilateral cleft lip and palate. J. Orofac. Orthop. 2013, 74, 275–286. [Google Scholar] [CrossRef]
- Yu, Q.; Gong, X.; Wang, G.M.; Yu, Z.Y.; Qian, Y.F.; Shen, G. A novel technique for presurgical nasoalveolar molding using computer-aided reverse engineering and rapid prototyping. J. Craniofacial Surg. 2011, 22, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.; Yao, C.A.; Magee, W.; Chai, G.; Zhang, Y. Presurgical nasoalveolar molding for cleft lip and palate: The application of digitally designed molds. Plast. Reconstr. Surgery 2015, 135, 1007e–1015e. [Google Scholar] [CrossRef]
- Christensen, G.J. Will digital impressions eliminate the current problems with conventional impressions? J. Am. Dent. Assoc. 2008, 139, 761–763. [Google Scholar] [CrossRef]
- Braumann, B.; Keilig, L.; Stellzig-Eisenhauer, A.; Bourauel, C.; Bergé, S.; Jäger, A. Patterns of maxillary alveolar arch growth changes of infants with unilateral cleft lip and palate: Preliminary findings. Cleft Palate Craniofacial J. 2003, 40, 363–372. [Google Scholar] [CrossRef]
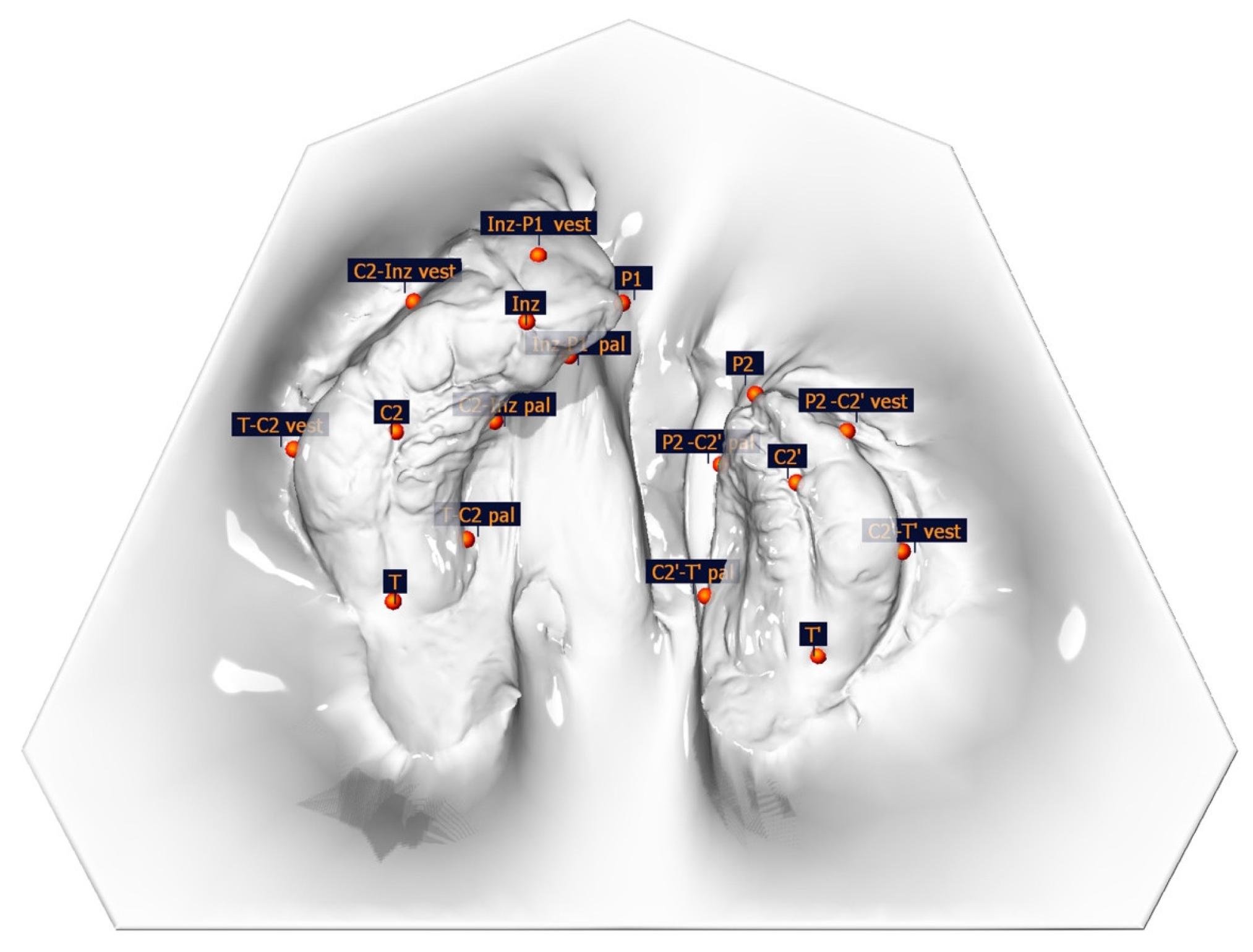


| Measuring Point | Description of the Anatomical Position | |
|---|---|---|
| Anatomical points | Inz | Intersection of the crest of the alveolar ridge and the line drawn from the labial frenulum to the incisive papilla |
| P1/P2 | Cleft edge of the crest of the alveolar ridge, large/small segment | |
| C2/C2′ | Intersection of the gingival groove and the lateral sulcus (large/small segment) | |
| T/T’ | The most distal point of the gingival groove (Tuberosity points) | |
| T-C2 vest | The most vestibular point perpendicular to the line T-C2 (large segment) | |
| T-C2 pal | The most palatal point perpendicular to the line T-C2 (large segment) | |
| C2-Inz vest | The most vestibular point perpendicular to the line C2-Inz (large segment) | |
| C2-Inz pal | The most palatal point perpendicular to the line C2-Inz (large segment) | |
| Inz-P1 vest | The most vestibular point perpendicular to the line Inz-P1 (large segment) | |
| Inz-P1 pal | The most palatal point perpendicular to the line Inz-P1 (large segment) | |
| P2-C2′ vest | The most vestibular point perpendicular to the line P2-C2′ (small segment) | |
| P2-C2′ pal | The most palatal point perpendicular to the line P2-C2′ (small segment) | |
| C2′-T’ vest | The most vestibular point perpendicular to the line C2′-T’ (small segment) | |
| C2′-T’ pal | The most palatal point perpendicular to the line C2′-T’ (small segment) | |
| Constructed points | M | Center of the line connecting T and T’ |
| A | Perpendicular projection of Inz to the line T-T’ | |
| Measuring distance | Description | |
| Alveolar cleft width | P-P’ | The line connecting P and P’; real cleft width |
| Anterior and posterior arch width | C2-C2′ | Distance C2-C2′ |
| T-T’ | Distance T-T′ | |
| C2-M | Distance point C2 to the midpoint of line TT′ (large segment) | |
| C2′-M | Distance point C2′ to the midpoint of line TT′ (small segment) | |
| Segment length measurements | T-C2 | Distal alveolar ridge length of the large segment |
| C2-Inz | Medial alveolar ridge length of the large segment | |
| Inz-P1 | Mesial alveolar ridge length of the large segment | |
| P2-C2′ | Mesial alveolar ridge length of the small segment | |
| C2′-T’ | Distal alveolar ridge length of the small segment | |
| AKL (T-C2-Inz-P1) | Total alveolar ridge length large segment | |
| AKL’ (P2-C2′-T’) | Total alveolar ridge length small segment | |
| Segment width measurements | T-C2 vest—T-C2 pal | Distance from the most vestibular and the most palatal point perpendicular to the distance T-C2 (large segment)/distal alveolar ridge width of the large segment |
| C2-Inz vest—Inz pal | Distance from the most vestibular and the most palatal point to the distance C2-Inz (large segment)/medial alveolar ridge width of the large segment | |
| Inz-P1 vest—Inz-P1 pal | Distance from the most vestibular and the most palatal point to the distance Inz-P1 (large segment)/mesial alveolar ridge width of the large segment | |
| C2′-P2 vest—C2′-P2 pal | Distance from the most vestibular and the most palatal point to the distance C2′-P2 (small segment)/mesial alveolar ridge width of the small segment | |
| T’-C2′ vest—T’-C2′ pal | Distance from the most vestibular and the most palatal point to the distance T′-C2′ (small segment)/distal alveolar ridge width of the small segment | |
| Angle measurements | MIA | Angle between Inz-A and Inz-M |
| C2-T-T’ | Curvature of the distal alveolar ridge area (large segment) | |
| T-C2-Inz | Curvature of the medial alveolar ridge area (large segment) | |
| C2-Inz-P1 | Curvature of the mesial alveolar ridge area (large segment) | |
| P2-C2′-T’ | Curvature of the mesial alveolar ridge area (small segment) | |
| C2′-T-T’ | Curvature of the distal alveolar ridge area (small segment) |
| Type of Stratification | Measurement Time | N | Mean/Median | SD/IQR | p-Value | ||
|---|---|---|---|---|---|---|---|
| Total surface area | monthly (mm2) | 49 | 89.01 | 27.20 | <0.001 * | ||
| monthly (%) | 49 | 8.56 | 0.0276 | <0.001 * | |||
| overall (mm2) | 49 | 363.23 | 157.15 | <0.001 * | |||
| overall increase (%) | 49 | 34.89 | 0.1549 | <0.001 * | |||
| Small segment | monthly (mm2) | 49 | 38.69 | 13.91 | <0.001 * | ||
| monthly (%) | 49 | 9.50 | 0.0357 | <0.001 * | |||
| overall (mm2) | 49 | 158.33 | 78.48 | <0.001 * | |||
| overall increase (%) | 49 | 39.00 | 0.2025 | <0.001 * | |||
| Large segment | monthly (mm2) | 49 | 50.32 | 16.85 | <0.001 * | ||
| monthly (%) | 49 | 8.01 | 0.0290 | <0.001 * | |||
| overall (mm2) | 49 | 204.90 | 87.50 | <0.001 * | |||
| overall increase (%) | 49 | 32.43 | 0.1404 | <0.001 * | |||
| Segment type | LS—SS | monthly (mm2) | 49 | 11.62 | 14.66 | <0.001 *,A | |
| monthly (%) | 49 | −1.49 | 0.0322 | <0.001 *,A | |||
| overall (mm2) | 49 | 46.57 | 54.16 | <0.001 *,A | |||
| overall increase (%) | 49 | −6.57 | 0.1300 | <0.001 *,A | |||
| Cleft side | TS | L | monthly (mm2) | 32 | 89.93 | 24.47 | 0.77 **,B |
| R | monthly (mm2) | 17 | 87.29 | 32.46 | |||
| L | overall (mm2) | 32 | 389.10 | 156.62 | 0.11 **,B | ||
| R | overall (mm2) | 17 | 314.53 | 150.66 | |||
| SS | L | monthly (mm2) | 32 | 39.47 | 11.85 | 0.64 **,B | |
| R | monthly (mm2) | 17 | 37.24 | 17.46 | |||
| L | overall (mm2) | 32 | 171.10 | 75.02 | 0.13 **,B | ||
| R | overall (mm2) | 17 | 134.27 | 81.41 | |||
| LS | L | monthly (mm2) | 32 | 50.46 | 15.28 | 0.94 **,B | |
| R | monthly (mm2) | 17 | 50.04 | 19.97 | |||
| L | overall (mm2) | 32 | 217.99 | 89.56 | 0.14 **,B | ||
| R | overall (mm2) | 17 | 180.25 | 80.25 | |||
| Gender | TS | M | monthly (mm2) | 39 | 91.60 | 27.42 | 0.18 **,C |
| F | monthly (mm2) | 10 | 78.93 | 25.06 | |||
| M | overall (mm2) | 39 | 368.11 | 155.46 | 0.69 **,C | ||
| F | overall (mm2) | 10 | 344.18 | 170.78 | |||
| SS | M | monthly (mm2) | 39 | 40.49 | 14.25 | 0.04 **,C | |
| F | monthly (mm2) | 10 | 31.68 | 10.31 | |||
| M | overall (mm2) | 39 | 164.25 | 81.16 | 0.25 **,C | ||
| F | overall (mm2) | 10 | 135.24 | 65.49 | |||
| LS | M | monthly (mm2) | 39 | 51.10 | 16.93 | 0.53 **,C | |
| F | monthly (mm2) | 10 | 47.25 | 17.01 | |||
| M | overall (mm2) | 39 | 203.86 | 82.61 | 0.89 **,C | ||
| F | overall (mm2) | 10 | 208.93 | 109.53 | |||
| Type of Stratification | N | Mean | SD | p-Value | |
|---|---|---|---|---|---|
| Total surface increase compared to the first measurement | month 1 (mm2) | 29 | 124.75 | 50.83 | <0.001 * |
| month 1 (%) | 29 | 0.1218 | 0.0511 | <0.001 * | |
| month 2 (mm2) | 25 | 225.77 | 67.26 | <0.001 * | |
| month 2 (%) n | 25 | 0.2190 | 0.0685 | <0.001 * | |
| month 3 (mm2) | 31 | 293.68 | 102.99 | <0.001 * | |
| month 3 (%) | 31 | 0.2871 | 0.1066 | <0.001 * | |
| month 4 (mm2) | 28 | 359.49 | 102.59 | <0.001 * | |
| month 4 (%) | 28 | 0.3371 | 0.0994 | <0.001 * | |
| month 5 (mm2) | 15 | 488.67 | 99.44 | <0.001 * | |
| month 5 (%) | 15 | 0.4556 | 0.1022 | <0.001 * | |
| month 6 (mm2) | 9 | 437.29 | 140.49 | <0.001 * | |
| month 6 (%) | 9 | 0.4354 | 0.1407 | <0.001 * | |
| Total surface increase compared to the previous month | month 1 (mm2) | 27 | 107.09 | 40.26 | <0.001 * |
| month 1 (%) | 27 | 0.1034 | 0.0389 | <0.001 * | |
| month 2 (mm2) | 19 | 105.33 | 34.69 | <0.001 * | |
| month 2 (%) n | 19 | 0.0913 | 0.0286 | <0.001 * | |
| month 3 (mm2) | 17 | 135.39 | 35.64 | <0.001 * | |
| month 3 (%) | 17 | 0.1111 | 0.0326 | <0.001 * | |
| month 4 (mm2) | 15 | 104.79 | 0.0773 | <0.001 * | |
| month 4 (%) | 15 | 0.0729 | 0.0416 | <0.001 * | |
| month 5 (mm2) | 9 | 109.05 | 58.31 | <0.001 * | |
| month 5 (%) | 9 | 0.0766 | 0.0472 | <0.01 * | |
| month 6 (mm2) | 3 | 87.62 | 0.0227 | <0.03 * | |
| month 6 (%) | 3 | 0.0581 | 0.0129 | <0.02 * | |
| Surface increase small segment compared to the first measurement | month 1 (mm2) | 29 | 58.26 | 27.69 | <0.001 * |
| month 1 (%) | 29 | 0.1453 | 0.0708 | <0.001 * | |
| month 2 (mm2) | 25 | 104.30 | 35.32 | <0.001 * | |
| month 2 (%) n | 25 | 0.2562 | 0.0883 | <0.001 * | |
| month 3 (mm2) | 31 | 133.38 | 57.09 | <0.001 * | |
| month 3 (%) | 31 | 0.3308 | 0.1472 | <0.001 * | |
| month 4 (mm2) | 29 | 155.00 | 59.38 | <0.001 * | |
| month 4 (%) | 29 | 0.3761 | 0.1478 | <0.001 * | |
| month 5 (mm2) | 15 | 227.94 | 50.54 | <0.001 * | |
| month 5 (%) | 15 | 0.5513 | 0.1453 | <0.001 * | |
| month 6 (mm2) | 9 | 182.32 | 75.51 | <0.001 * | |
| month 6 (%) | 9 | 0.4604 | 0.1978 | <0.001 * | |
| Surface increase small segment compared to the previous month | month 1 (mm2) | 27 | 49.17 | 23.99 | <0.001 * |
| month 1 (%) | 27 | 0.1212 | 0.0607 | <0.001 * | |
| month 2 (mm2) | 19 | 51.14 | 18.34 | <0.001 * | |
| month 2 (%) n | 19 | 0.1090 | 0.0359 | <0.001 * | |
| month 3 (mm2) | 17 | 53.84 | 24.11 | <0.001 * | |
| month 3 (%) | 17 | 0.1078 | 0.0485 | <0.001 * | |
| month 4 (mm2) | 15 | 43.38 | 25.89 | <0.001 * | |
| month 4 (%) | 15 | 0.0821 | 0.0505 | <0.001 * | |
| month 5 (mm2) | 10 | 53.48 | 32.58 | <0.001 * | |
| month 5 (%) | 10 | 0.0979 | 0.0756 | <0.01 * | |
| month 6 (mm2) | 3 | 23.76 | 9.94 | 0.05 | |
| month 6 (%) | 3 | 0.0392 | 0.0204 | 0.07 | |
| Surface increase large segment compared to the first measurement | month 1 (mm2) | 29 | 66.48 | 34.57 | <0.001 * |
| month 1 (%) | 29 | 0.1073 | 0.0574 | <0.001 * | |
| month 2 (mm2) | 25 | 121.47 | 38.47 | <0.001 * | |
| month 2 (%) n | 25 | 0.1946 | 0.0639 | <0.001 * | |
| month 3 (mm2) | 31 | 160.29 | 59.58 | <0.001 * | |
| month 3 (%) | 31 | 0.2593 | 0.0982 | <0.001 * | |
| month 4 (mm2) | 28 | 204.79 | 54.07 | <0.001 * | |
| month 4 (%) | 28 | 0.3148 | 0.0873 | <0.001 * | |
| month 5 (mm2) | 16 | 256.36 | 62.01 | <0.001 * | |
| month 5 (%) | 16 | 0.3939 | 0.1007 | <0.001 * | |
| month 6 (mm2) | 9 | 254.97 | 84.78 | <0.001 * | |
| month 6 (%) | 9 | 0.4219 | 0.1371 | <0.001 * | |
| Surface increase large segment compared to the previous month | month 1 (mm2) | 27 | 57.92 | 30.74 | <0.001 * |
| month 1 (%) | 27 | 0.0924 | 0.0485 | <0.001 * | |
| month 2 (mm2) | 19 | 54.19 | 24.46 | <0.001 * | |
| month 2 (%) n | 19 | 0.0794 | 0.0355 | <0.001 * | |
| month 3 (mm2) | 17 | 81.55 | 27.54 | <0.001 * | |
| month 3 (%) | 17 | 0.1144 | 0.0461 | <0.001 * | |
| month 4 (mm2) | 15 | 61.39 | 42.90 | <0.001 * | |
| month 4 (%) | 15 | 0.0742 | 0.0472 | <0.001 * | |
| month 5 (mm2) | 10 | 57.99 | 35.77 | <0.001 * | |
| month 5 (%) | 10 | 0.0678 | 0–0418 | <0.001 * | |
| month 6 (mm2) | 4 | 58.06 | 29.49 | <0.03 * | |
| month 6 (%) | 4 | 0.0684 | 0.0312 | <0.03 * |
| Type of Stratification | Measurement Time | N | Mean/Median | SD/IQR | p-Value | |
|---|---|---|---|---|---|---|
| Cleft width reduction | monthly (mm) | 50 | 0.97 | 0.65 | <0.001 *** | |
| monthly (%) | 50 | 12.10 | 0.0823 | <0.001 * | ||
| overall (mm) | 50 | 3.81 | 2.36 | <0.001 * | ||
| overall (%) | 50 | 45.64 | 0.2883 | <0.001 * | ||
| Cleft side | L | monthly (mm) | 33 | −0.91 | −0.78 | 0.44 ****,A |
| R | monthly (mm) | 17 | −1.03 | 0.47 | ||
| Gender | M | monthly (mm) | 40 | −1.00 | −0.69 | 0.57 ****,B |
| F | monthly (mm) | 10 | −0.78 | −0.45 | ||
| Type of appliance | AP | monthly (mm) | 30 | −1.10 | −0.71 | 0.04 ****,C |
| PP | monthly (mm) | 20 | −0.75 | −0.53 | ||
| Type of Stratification | Measurement Time | N | Mean/Median | SD/IQR | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| C2-C2′ | descriptive | monthly (mm) | 50 | −0.01 | 0.61 | 0.50 * | ||
| Cleft side | L | monthly (mm) | 33 | −0.0023 | 0.63 | 0.86 **,A | ||
| R | monthly (mm) | 17 | −0.04 | 0.60 | ||||
| Gender | M | monthly (mm) | 40 | −0.06 | 0.65 | 0.15 **,B | ||
| F | monthly (mm) | 10 | 0.18 | 0.39 | ||||
| Type of appliance | AP | monthly (mm) | 30 | −0.04 | 0.59 | 0.69 **,C | ||
| PP | monthly (mm) | 20 | 0.02 | 0.66 | ||||
| T-T’ | descriptive | monthly (mm) | 50 | 0.14 | 0.59 | 0.08 * | ||
| Cleft side | L | monthly (mm) | 33 | 0.12 | 0.50 | 0.63 **,A | ||
| R | monthly (mm) | 17 | 0.21 | 0.73 | ||||
| Gender | M | monthly (mm) | 40 | 0.12 | 0.62 | 0.43 **,B | ||
| F | monthly (mm) | 10 | 0.26 | 0.45 | ||||
| Type of appliance | AP | monthly (mm) | 30 | 0.08 | 0.59 | 0.38 ****,C | ||
| PP | monthly (mm) | 20 | 0.16 | 2.22 | ||||
| C2-M/ C2′-M | descriptive | LS | monthly (mm) | 50 | −0.09 | 0.44 | 0.17 * | |
| SS | monthly (mm) | 50 | 0.07 | 0.35 | 0.18 * | |||
| Cleft side | LS | L | monthly (mm) | 33 | −0.11 | 0.46 | 0.52 **,A | |
| R | monthly (mm) | 17 | −0.03 | 0.40 | ||||
| SS | L | monthly (mm) | 33 | 0.11 | 0.33 | 0.29 **,A | ||
| R | monthly (mm) | 17 | −0.01 | 0.38 | ||||
| Gender | LS | M | monthly (mm) | 40 | −0.11 | -0.45 | 0.42 **,B | |
| F | monthly (mm) | 10 | 0.01 | 0.39 | ||||
| SS | M | monthly (mm) | 40 | 0.04 | 0.37 | 0.21 **,B | ||
| F | monthly (mm) | 10 | 0.17 | 0.25 | ||||
| Type of appliance | LS | AP | monthly (mm) | 30 | −0.09 | 0.39 | 1.0 **,C | |
| PP | monthly (mm) | 20 | −0.09 | 0.51 | ||||
| SS | AP | monthly (mm) | 30 | 0.04 | 0.36 | 0.51 **,C | ||
| PP | monthly (mm) | 20 | 0.11 | 0.35 | ||||
| Type of Stratification | Measurement Time | N | Mean/ Median | SD/IQR | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| Segment length measurements | ||||||||
| LS | AKL | descriptive | monthly (mm) | 49 | 1.55 | 0.82 | <0.001 *** | |
| monthly (%) | 49 | 0.0480 | 0.0370 | <0.001 *** | ||||
| Cleft side | L | monthly (mm) | 32 | 1.52 | 0.68 | 0.16 ****,A | ||
| R | monthly (mm) | 17 | 1.17 | 0.74 | ||||
| Gender | M | monthly (mm) | 39 | 1.48 | 0.82 | 0.93 ****,B | ||
| F | monthly (mm) | 10 | 1.42 | 0.78 | ||||
| Type | AP | monthly (mm) | 29 | 1.67 | 1.23 | 0.52 ****,C | ||
| PP | monthly (mm) | 20 | 1.38 | 0.53 | ||||
| Inz-P1 | descriptive | monthly (mm) | 49 | 0.31 | 0.62 | <0.001 *** | ||
| monthly (%) | 49 | 0.0466 | 0.1292 | <0.001 *** | ||||
| C2-Inz | descriptive | monthly (mm) | 49 | 0.44 | 0.46 | <0.001 * | ||
| monthly (%) | 49 | 0.0405 | 0.0424 | <0.001 * | ||||
| T-C2 | descriptive | monthly (mm) | 49 | 0.79 | 0.66 | <0.001 *** | ||
| monthly (%) | 49 | 0.0662 | 0.0630 | <0.001 *** | ||||
| SS | AKL’ | descriptive | monthly (mm) | 49 | 1.02 | 0.74 | <0.001 *** | |
| monthly (%) | 49 | 0.0521 | 0.0393 | <0.001 *** | ||||
| Cleft side | L | monthly (mm) | 32 | 0.98 | 0.65 | 0.78 ****,A | ||
| R | monthly (mm) | 17 | 1.10 | 0.90 | ||||
| Gender | M | monthly (mm) | 39 | 1.07 | 0.81 | 0.57 ****,B | ||
| F | monthly (mm) | 10 | 0.83 | 0.31 | ||||
| Type | AP | monthly (mm) | 29 | 1.24 | 0.77 | 0.006 ****,C | ||
| PP | monthly (mm) | 20 | 0.70 | 0.56 | ||||
| P2-C2′ | descriptive | monthly (mm) | 49 | 0.46 | 0.51 | <0.001 *** | ||
| monthly (%) | 49 | 0.0607 | 0.0667 | <0.001 *** | ||||
| C2′-T′ | descriptive | monthly (mm) | 49 | 0.56 | 0.57 | <0.001 *** | ||
| monthly (%) | 49 | 0.0500 | 0.0532 | <0.001 *** | ||||
| Segment width measurements | ||||||||
| LS | B.AKL | descriptive | monthly (mm) | 49 | 1.41 | 0.82 | <0.001 *** | |
| monthly (%) | 49 | 0.0463 | 0.0277 | <0.001 * | ||||
| Cleft side | L | monthly (mm) | 32 | 1.41 | 0.62 | 0.99 **,A | ||
| R | monthly (mm) | 17 | 1.41 | 1.13 | ||||
| Gender | M | monthly (mm) | 39 | 1.47 | 0.88 | 0.12 ****,B | ||
| F | monthly (mm) | 10 | 1.15 | 0.49 | ||||
| Type | AP | monthly (mm) | 29 | 1.41 | 0.91 | 0.57 ****,C | ||
| PP | monthly (mm) | 20 | 1.42 | 0.71 | ||||
| B.Inz-P1 | descriptive | monthly (mm) | 49 | 0.23 | 0.42 | <0.001 *** | ||
| monthly (%) | 49 | 0.0346 | 0.0670 | <0.001 *** | ||||
| B.C2-Inz | descriptive | monthly (mm) | 49 | 0.46 | 0.40 | <0.001 * | ||
| monthly (%) | 49 | 0.0483 | 0.0427 | <0.001 * | ||||
| B.T-C2 | descriptive | monthly (mm) | 49 | 0.72 | 0.32 | <0.001 * | ||
| monthly (%) | 49 | 0.0556 | 0.0289 | <0.001 *** | ||||
| SS | B.AKL’ | descriptive | monthly (mm) | 49 | 1.05 | 0.80 | <0.001 *** | |
| monthly (%) | 49 | 0.0468 | 0.0368 | <0.001 *** | ||||
| Cleft side | L | monthly (mm) | 32 | 0.97 | 0.57 | 0.40 ****,A | ||
| R | monthly (mm) | 17 | 1.21 | 1.11 | ||||
| Gender | M | monthly (mm) | 39 | 1.06 | 0.83 | 0.71 ****,B | ||
| F | monthly (mm) | 10 | 1.00 | 0.68 | ||||
| Type | AP | monthly (mm) | 29 | 1.14 | 0.70 | 0.58 ****,C | ||
| PP | monthly (mm) | 20 | 0.93 | 0.93 | ||||
| B.P2-C2‘ | descriptive | monthly (mm) | 49 | 0.50 | 0.36 | 0.001 *** | ||
| monthly (%) | 49 | 0.0551 | 0.0377 | 0.001 * | ||||
| B.C2′-T’ | descriptive | monthly (mm) | 49 | 0.55 | 0.59 | 0.001 *** | ||
| monthly (%) | 49 | 0.0421 | 0.0470 | 0.001 *** | ||||
| Surface Change | Length Change Small Segment | Width Change Small Segment | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Observation Period | N | r | 95% CI | p-Value | r | 95% CI | p-Value | ||
| Small segment | monthly (mm2) | 49 | 0.32 | 0.05–0.55 | 0.02 * | 0.21 | −0.06–0.46 | 0.13 | |
| monthly (%) | 49 | 0.32 | 0.05–0.55 | 0.02 * | 0.21 | −0.07–0.46 | 0.14 | ||
| Cleft side | L | monthly (mm2) | 32 | 0.004 | −0.34–0.35 | 0.98 | 0.39 | 0.05–0.65 | 0.02 * |
| R | monthly (mm2) | 17 | 0.65 | 0.25–0.86 | 0.004 * | 0.12 | −0.38–0.56 | 0.64 | |
| Gender | M | monthly (mm2) | 39 | 0.30 | −0.006–0.569 | 0.05 | 0.20 | −0.11–0.48 | 0.20 |
| F | monthly (mm2) | 10 | 0.34 | −0.36–0.79 | 0.33 | 0.26 | −0.43–0.76 | 0.46 | |
| Surface change | Length change large segment | Width change large segment | |||||||
| observation period | N | r | 95% CI | p value | r | 95% CI | p value | ||
| Large segment | monthly (mm2) | 49 | 0.24 | −0.03–0.49 | 0.08 | 0.36 | 0.09–0.58 | 0.009 * | |
| monthly (%) | 49 | 0.32 | 0.05–0.56 | 0.02 * | 0.42 | 0.16–0.63 | 0.002 * | ||
| Cleft side | L | monthly (mm2) | 32 | −0.008 | −0.35–0.34 | 0.96 | 0.07 | −0.28–0.41 | 0.69 |
| R | monthly (mm2) | 17 | 0.42 | −0.07–0.75 | 0.09 | 0.61 | 0.18–0.84 | 0.008 * | |
| Gender | M | monthly (mm2) | 39 | 0.31 | −0.003–0.57 | 0.05 | 0.44 | 0.15–0.66 | 0.004 * |
| F | monthly (mm2) | 10 | −0.25 | −0.76–0.45 | 0.48 | −0.28 | −0.77–0.41 | 0.42 | |
| Type of Stratification | Measurement Time | N | Mean/ Median | SD/IQR | p Value | |||
|---|---|---|---|---|---|---|---|---|
| LS | P1-TT′Inz | descriptive | monthly (mm) | 50 | 0.02 | 0.43 | 0.47 *** | |
| monthly (%) | 50 | 1.14 | 0.0852 | 0.36 *** | ||||
| Cleft side | L | monthly (mm) | 33 | 0.02 | 0.35 | 0.88 **,A | ||
| R | monthly (mm) | 17 | 0.002 | 0.57 | ||||
| Gender | M | monthly (mm) | 40 | 0.03 | 0.44 | 0.72 **,B | ||
| F | monthly (mm) | 10 | -0.02 | 0.39 | ||||
| Type | AP | monthly (mm) | 30 | 0.12 | 0.36 | 0.06 **,C | ||
| PP | monthly (mm) | 20 | -0.13 | 0.49 | ||||
| C2-TT′Inz | descriptive | monthly (mm) | 50 | 0.24 | 0.25 | <0.001 * | ||
| monthly (%) | 50 | 57.20 | 5.1824 | 0.05 *** | ||||
| Cleft side | L | monthly (mm) | 33 | 0.27 | 0.24 | 0.37 **,A | ||
| R | monthly (mm) | 17 | 0.20 | 0.26 | ||||
| Gender | M | monthly (mm) | 40 | 0.24 | 0.26 | 089 **,B | ||
| F | monthly (mm) | 10 | 0.25 | 0.18 | ||||
| Type | AP | monthly (mm) | 30 | 0.24 | 0.23 | 085 **,C | ||
| PP | monthly (mm) | 20 | 0.25 | 0.27 | ||||
| SS | P2-TT′Inz | descriptive | monthly (mm) | 50 | 0.23 | 0.46 | 0.0002 *** | |
| monthly (%) | 50 | 4.37 | 0.0980 | 0.0002 *** | ||||
| Cleft side | L | monthly (mm) | 33 | 0.26 | 0.37 | 0.58 **,A | ||
| R | monthly (mm) | 17 | 0.16 | 0.68 | ||||
| Gender | M | monthly (mm) | 40 | 0.22 | 0.54 | 0.65 **,B | ||
| F | monthly (mm) | 10 | 0.26 | 0.20 | ||||
| Type | AP | monthly (mm) | 30 | 0.39 | 0.45 | 0.0012 ****,C | ||
| PP | monthly (mm) | 20 | −0.01 | 0.46 | ||||
| C2′-TT′Inz | descriptive | monthly (mm) | 50 | 0.23 | 0.25 | <0.001 *** | ||
| monthly (%) | 50 | 14.17 | 0.4579 | <0.001 *** | ||||
| Cleft side | L | monthly (mm) | 33 | 0.23 | 0.28 | 0.66 ****,A | ||
| R | monthly (mm) | 17 | 0.19 | 0.30 | ||||
| Gender | M | monthly (mm) | 40 | 0.20 | 0.30 | 0.12 ****,B | ||
| F | monthly (mm) | 10 | 0.29 | 0.21 | ||||
| Type | AP | monthly (mm) | 30 | 0.24 | 0.34 | 0.67 ****,C | ||
| PP | monthly (mm) | 20 | 0.18 | 0.17 | ||||
| Type of Stratification | Measurement Time | N | Mean/ Median | SD/IQR | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| Length Measurements | ||||||||
| MIA | descriptive | monthly (mm) | 50 | −1.61 | 1.43 | <0.001 *** | ||
| monthly (%) | 50 | −0.0848 | 0.1152 | <0.001 *** | ||||
| Cleft side | L | monthly (mm) | 33 | −0.09 | 0.13 | 0.26 ****,A | ||
| R | monthly (mm) | 17 | −0.08 | 0.08 | ||||
| Gender | M | monthly (mm) | 40 | −1.51 | 1.32 | 0.97 ****,B | ||
| F | monthly (mm) | 10 | −1.99 | 1.83 | ||||
| Type | AP | monthly (mm) | 30 | −0.09 | 0.05 | 0.55 *** | ||
| PP | monthly (mm) | 20 | −0.08 | 0.18 | ||||
| LS | C2-T-T′ | descriptive | monthly (mm) | 50 | −0.49 | 1.53 | 0.03 * | |
| monthly (%) | 50 | −0.0051 | 0.0171 | 0.04 * | ||||
| Cleft side | L | monthly (mm) | 33 | −0.61 | 1.77 | 0.33 **,A | ||
| R | monthly (mm) | 17 | −0.24 | 0.92 | ||||
| Gender | M | monthly (mm) | 40 | −0.51 | 1.55 | 0.46 ****,B | ||
| F | monthly (mm) | 10 | −0.39 | 1.56 | ||||
| Type | AP | monthly (mm) | 30 | −0.38 | 1.39 | 0.60 **,C | ||
| PP | monthly (mm) | 20 | −0.64 | 1.74 | ||||
| T-C2-Inz | descriptive | monthly (mm) | 50 | 8.86 | 65.17 | 0.32 *** | ||
| monthly (%) | 50 | 0.0592 | 0.4333 | 0.36 *** | ||||
| Cleft side | L | monthly (mm) | 33 | 13.24 | 80.25 | 0.50 ****,A | ||
| R | monthly (mm) | 17 | 0.37 | 3.18 | ||||
| Gender | M | monthly (mm) | 40 | 11.44 | 72.81 | 0.27 ****,B | ||
| F | monthly (mm) | 10 | −1.43 | 1.73 | ||||
| Type | AP | monthly (mm) | 30 | 15.13 | 84.08 | 0.35 ****,C | ||
| PP | monthly (mm) | 20 | −0.53 | 2.59 | ||||
| C2-Inz-P1 | descriptive | monthly (mm) | 50 | −1.27 | 3.04 | 0.003 *** | ||
| monthly (%) | 50 | −0.01 | 0.02 | 0.004 *** | ||||
| Cleft side | L | monthly (mm) | 33 | −0.87 | 2.62 | 0.45 ****,A | ||
| R | monthly (mm) | 17 | −2.06 | 3.68 | ||||
| Gender | M | monthly (mm) | 40 | −1.46 | 3.13 | 0.64 ****,B | ||
| F | monthly (mm) | 10 | −0.52 | 2.26 | ||||
| Type | AP | monthly (mm) | 30 | −1.59 | 1.75 | 0.09 ****,C | ||
| PP | monthly (mm) | 20 | −0.80 | 4.32 | ||||
| SS | C2′-T-T′ | descriptive | monthly (mm) | 50 | 0.36 | 1.65 | 0.06 *** | |
| monthly (%) | 50 | 0.0052 | 0.0215 | 0.09 * | ||||
| Cleft side | L | monthly (mm) | 33 | 0.53 | 1.53 | 0.34 **,A | ||
| R | monthly (mm) | 17 | 0.03 | 1.88 | ||||
| Gender | M | monthly (mm) | 40 | 0.34 | 1.80 | 0.79 **,B | ||
| F | monthly (mm) | 10 | 0.45 | 0.93 | ||||
| Type | AP | monthly (mm) | 30 | 0.61 | 1.65 | 0.19 ****,C | ||
| PP | monthly (mm) | 20 | −0.01 | 1.63 | ||||
| P2-C2′-T′ | descriptive | monthly (mm) | 50 | 0.59 | 3.53 | 0.06 *** | ||
| monthly (%) | 50 | 0.0043 | 0.2343 | 0.05 *** | ||||
| Cleft side | L | monthly (mm) | 33 | 1.34 | 2.88 | 0.07 **,A | ||
| R | monthly (mm) | 17 | −0.87 | 4.26 | ||||
| Gender | M | monthly (mm) | 40 | 0.49 | 3,79 | 0.60 ****,B | ||
| F | monthly (mm) | 10 | 0.99 | 2.29 | ||||
| Type | AP | monthly (mm) | 30 | −0.27 | 3.04 | 0.01 ****,C | ||
| PP | monthly (mm) | 20 | 1.89 | 3.89 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bühling, S.; Thedens, C.; Eslami, S.; Plein, N.; Dahmer, I.; Sayahpour, B.; Seifert, L.B.; Sader, R.; Kopp, S. Quantitative and Qualitative Segmental Surface Growth in Infants with Unilateral Cleft Lip and Palate: A Prospective In Vivo Study. Medicina 2025, 61, 1232. https://doi.org/10.3390/medicina61071232
Bühling S, Thedens C, Eslami S, Plein N, Dahmer I, Sayahpour B, Seifert LB, Sader R, Kopp S. Quantitative and Qualitative Segmental Surface Growth in Infants with Unilateral Cleft Lip and Palate: A Prospective In Vivo Study. Medicina. 2025; 61(7):1232. https://doi.org/10.3390/medicina61071232
Chicago/Turabian StyleBühling, Sarah, Cedric Thedens, Sara Eslami, Nicolas Plein, Iulia Dahmer, Babak Sayahpour, Lukas Benedikt Seifert, Robert Sader, and Stefan Kopp. 2025. "Quantitative and Qualitative Segmental Surface Growth in Infants with Unilateral Cleft Lip and Palate: A Prospective In Vivo Study" Medicina 61, no. 7: 1232. https://doi.org/10.3390/medicina61071232
APA StyleBühling, S., Thedens, C., Eslami, S., Plein, N., Dahmer, I., Sayahpour, B., Seifert, L. B., Sader, R., & Kopp, S. (2025). Quantitative and Qualitative Segmental Surface Growth in Infants with Unilateral Cleft Lip and Palate: A Prospective In Vivo Study. Medicina, 61(7), 1232. https://doi.org/10.3390/medicina61071232






