Association Between Perinasal Uptake on Radioactive Iodine Whole-Body Scan and Nasolacrimal Duct Obstruction
Abstract
1. Introduction
2. Methods
2.1. Study Subjects
2.2. Data Analysis
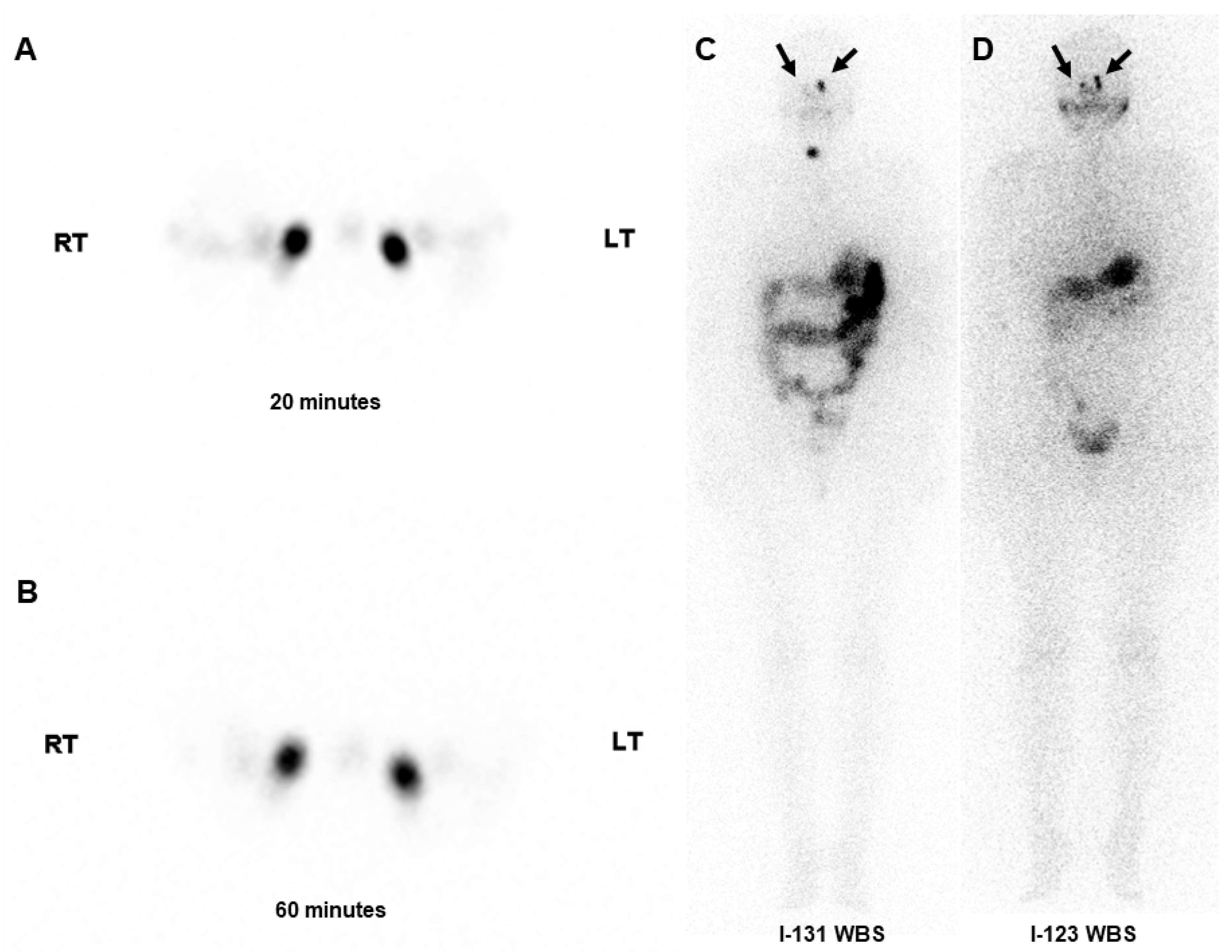
2.2.1. I-131 and I-123 Whole-Body Scans
2.2.2. Lacrimal Drainage System
A. Dacryoscintigraphy
B. Ophthalmic Examination
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics and Examination Results
3.2. Association Between WBS and Dacryoscintigraphy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef]
- Mazzaferri, E.L.; Jhiang, S.M. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am. J. Med. 1994, 97, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Mazzaferri, E.L.; Jhiang, S.M. Differentiated thyroid cancer long-term impact of initial therapy. Trans. Am. Clin. Climatol. Assoc. 1995, 106, 151–168, discussion 168–170. [Google Scholar] [PubMed]
- Mazzaferri, E.L. An overview of the management of papillary and follicular thyroid carcinoma. Thyroid 1999, 9, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.K.; Youn, H.W.; Kang, J.H.; Lee, H.Y.; Kang, K.W. Sodium iodide symporter and the radioiodine treatment of thyroid carcinoma. Nucl. Med. Mol. Imaging 2010, 44, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Koca, G.; Singar, E.; Akbulut, A.; Yazihan, N.; Yumuşak, N.; Demir, A.; Korkmaz, M. The effect of resveratrol on radioiodine therapy-associated lacrimal gland damage. Curr. Eye Res. 2021, 46, 398–407. [Google Scholar] [CrossRef] [PubMed]
- Yartsev, V.D.; Solodkiy, V.A.; Fomin, D.K.; Borisenko, T.E.; Atkova, E.L. Clinical and demographic characteristics of tearing in patients after radioiodine ablation for differentiated thyroid cancer. Curr. Eye Res. 2021, 46, 1320–1324. [Google Scholar] [CrossRef] [PubMed]
- Solans, R.; Bosch, J.A.; Galofré, P.; Porta, F.; Roselló, J.; Selva-O’Callagan, A.; Vilardell, M. Salivary and lacrimal gland dysfunction (sicca syndrome) after radioiodine therapy. J. Nucl. Med. 2001, 42, 738–743. [Google Scholar] [PubMed]
- Sun, G.E.; Hatipoglu, B. Epiphora after radioactive iodine ablation for thyroid cancer. Thyroid 2013, 23, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Rahmanipour, E.; Askari, E.; Ghorbani, M.; Mirzaei, M.; Rahimi, B.; Daskareh, M.; Mirshahvalad, S.A. Eye-related adverse events after I-131 radioiodine therapy: A systematic review of the current literature. Endocr. Pract. 2024, 30, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Bakheet, S.M.; Hammami, M.M. False-positive radioiodine whole-body scan in thyroid cancer patients due to unrelated pathology. Clin. Nucl. Med. 1994, 19, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Bakheet, S.M.; Hammami, M.M.; Hemidan, A.; Powe, J.E.; Bajaafar, F. Radioiodine secretion in tears. J. Nucl. Med. 1998, 39, 1452–1454. [Google Scholar] [PubMed]
- Al-Qahtani, K.H.; Al Asiri, M.; Tunio, M.A.; Aljohani, N.J.; Bayoumi, Y.; Munir, I.; AlAyoubi, A. Nasolacrimal duct obstruction following radioactive iodine-131 therapy in differentiated thyroid cancers: Review of 19 cases. Clin. Ophthalmol. 2014, 8, 2479–2484. [Google Scholar] [PubMed]
- Ali, M.J. Iodine-131 therapy and nasolacrimal duct obstructions: What we know and what we need to know. Ophthal. Plast. Reconstr. Surg. 2016, 32, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.T.; Chen, W.; Chen, Q.; Cole, H.A.; Bischoff, L.A.; Jessop, A.C.; Sobel, R.K. Factors associated with radioactive iodine therapy-acquired nasolacrimal duct obstruction. Endocr. Pract. 2022, 28, 1210–1215. [Google Scholar] [CrossRef] [PubMed]
- Fedorov, A.A.; Atkova, E.L.; Yartsev, V.D. Secondary acquired nasolacrimal duct obstruction as a specific complication of treatment with radioactive iodine (morphological study). Ophthal. Plast. Reconstr. Surg. 2020, 36, 250–253. [Google Scholar] [CrossRef] [PubMed]
- da Fonseca, F.L.; Yamanaka, P.K.; Kato, J.M.; Matayoshi, S. Lacrimal system obstruction after radioiodine therapy in differentiated thyroid carcinomas: A prospective comparative study. Thyroid 2016, 26, 1761–1767. [Google Scholar] [CrossRef] [PubMed]
- Fard-Esfahani, A.; Gholamrezanezhad, A.; Mirpour, S.; Tari, A.S.; Saghari, M.; Beiki, D.; Sichani, B.F.; Eftekhari, M. Assessment of the accuracy of lacrimal scintigraphy based on a prospective analysis of patients’ symptomatology. Orbit 2008, 27, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.J.; Vyakaranam, A.R.; Rao, J.E.; Prasad, G.; Reddy, P.V. Iodine-131 therapy and lacrimal drainage system toxicity: Nasal localization studies using whole body nuclear scintigraphy and SPECT-CT. Ophthal. Plast. Reconstr. Surg. 2017, 33, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Sakahara, H.; Yamashita, S.; Suzuki, K.; Imai, M.; Kosugi, T. Visualization of nasolacrimal drainage system after radioiodine therapy in patients with thyroid cancer. Ann. Nucl. Med. 2007, 21, 525–527. [Google Scholar] [CrossRef] [PubMed]
| Variable | Results |
|---|---|
| Sex, n | |
| Men | 10 |
| Women | 27 |
| Mean age, years (range) | 50 (22–74) |
| Mean RAI dose, mCi (range) | 75 (30–150) |
| Abnormal RAI WBS uptakes | |
| Perinasal uptake (+), % (eyes) | |
| I-131 WBS | 11 (8) |
| I-123 WBS | 20 (15) |
| Nasal uptake (+), % (eyes) | |
| I-131 WBS | 8 (60) |
| I-123 WBS | 100 (74) |
| Abnormal dacryoscintigraphy, % (eyes) | 32 (24) |
| Abnormal ophthalmic examination, % (eyes) | |
| Nasolacrimal duct obstruction | 16 (12) |
| Ocular dryness | 41 (30) |
| Epiphora | 15 (11) |
| Punctal stenosis | 12 (9) |
| Tear film break-up time | 96 (71) * |
| Schirmer’s test | 25 (18/72) † |
| Punctate keratopathy | 51 (38) |
| Tear meniscus height | 35 (26) |
| Variable | I-131 WBS | I-123 WBS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Perinasal Uptake | Nasal Uptake | Perinasal Uptake | Nasal Uptake | |||||||||
| No | Yes | p * | No | Yes | p * | No | Yes | p * | No | Yes | p * | |
| Dacryoscintigraphy | <0.001 | 0.03 | <0.001 | NA | ||||||||
| Normal | 50 | 0 | 13 | 37 | 46 | 4 | 0 | 50 | ||||
| Abnormal | 16 | 8 | 1 | 23 | 13 | 11 | 0 | 24 | ||||
| Punctal stenosis | 0.58 | 0.36 | 1.0 | NA | ||||||||
| No | 57 | 8 | 11 | 54 | 52 | 13 | 0 | 65 | ||||
| Yes | 9 | 0 | 3 | 6 | 7 | 3 | 0 | 9 | ||||
| NLDO | 1.0 | 0.44 | 0.44 | NA | ||||||||
| No | 55 | 7 | 13 | 49 | 48 | 14 | 0 | 62 | ||||
| Yes | 11 | 1 | 1 | 11 | 11 | 1 | 0 | 12 | ||||
| Epiphora | 1.0 | 0.11 | 0.22 | NA | ||||||||
| No | 56 | 7 | 14 | 49 | 52 | 11 | 0 | 63 | ||||
| Yes | 10 | 1 | 0 | 11 | 7 | 4 | 0 | 11 | ||||
| Dryness | 0.13 | 0.16 | 0.02 | NA | ||||||||
| No | 37 | 7 | 6 | 38 | 31 | 13 | 0 | 44 | ||||
| Yes | 29 | 1 | 8 | 22 | 28 | 2 | 0 | 30 | ||||
| Tear film break-up time | 1.0 | 0.18 | 1.0 | NA | ||||||||
| Normal | 7 | 1 | 3 | 5 | 7 | 1 | 0 | 5 | ||||
| Abnormal | 57 | 7 | 11 | 53 | 50 | 14 | 0 | 64 | ||||
| Schirmer’s test | 0.67 | 0.74 | 0.1 | NA | ||||||||
| Normal | 17 | 1 | 4 | 14 | 17 | 1 | 0 | 18 | ||||
| Abnormal | 47 | 7 | 10 | 44 | 40 | 14 | 0 | 54 | ||||
| Punctate keratopathy | 0.15 | 0.91 | 0.68 | NA | ||||||||
| Normal | 30 | 6 | 7 | 29 | 28 | 8 | 0 | 36 | ||||
| Abnormal | 36 | 2 | 7 | 31 | 31 | 7 | 0 | 38 | ||||
| Tear meniscus height | 1.0 | 1.0 | 1.0 | NA | ||||||||
| Normal | 65 | 8 | 14 | 59 | 58 | 15 | 0 | 73 | ||||
| Abnormal | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, M.; Lee, H.; Park, N.R.; Lee, J.-H.; Park, S.H. Association Between Perinasal Uptake on Radioactive Iodine Whole-Body Scan and Nasolacrimal Duct Obstruction. Medicina 2025, 61, 1165. https://doi.org/10.3390/medicina61071165
Seo M, Lee H, Park NR, Lee J-H, Park SH. Association Between Perinasal Uptake on Radioactive Iodine Whole-Body Scan and Nasolacrimal Duct Obstruction. Medicina. 2025; 61(7):1165. https://doi.org/10.3390/medicina61071165
Chicago/Turabian StyleSeo, Minjung, Hongje Lee, Na Ri Park, Ju-Hyang Lee, and Seol Hoon Park. 2025. "Association Between Perinasal Uptake on Radioactive Iodine Whole-Body Scan and Nasolacrimal Duct Obstruction" Medicina 61, no. 7: 1165. https://doi.org/10.3390/medicina61071165
APA StyleSeo, M., Lee, H., Park, N. R., Lee, J.-H., & Park, S. H. (2025). Association Between Perinasal Uptake on Radioactive Iodine Whole-Body Scan and Nasolacrimal Duct Obstruction. Medicina, 61(7), 1165. https://doi.org/10.3390/medicina61071165






