1. Introduction
Dry eye disease (DED) is a multifactorial condition characterized by a persistently unstable or insufficient tear film that causes discomfort, visual impairment, ocular surface epitheliopathy, inflammation, and neurosensory abnormalities. The global prevalence of DED varies widely, ranging from 5% to 50%, as reported by studies conducted in the United States, Australia, and several countries in Asia [
1,
2]. In Saudi Arabia, two published studies reported prevalence rates of 49.5% and 74.9%, respectively [
3,
4].
Environmental factors, including climate conditions, air pollution, and digital device use, also contribute significantly to DED development. A comprehensive review by demonstrated that temperature, humidity, and air pollutants significantly impact tear film stability and ocular surface health globally [
5]. Low relative humidity has been consistently associated with increased tear evaporation, decreased tear stability, and worsened DED symptoms in controlled studies [
6]. Additionally, the widespread use of digital devices has emerged as a significant risk factor, with a recent systematic review and dose-response meta-analysis by Ha et al. reporting that each additional hour of daily digital screen time was associated with 21% higher odds of myopia, with this relationship following a sigmoidal pattern that suggests potential harm beyond one hour of daily exposure [
7].
Several factors influence the development of DED, including systemic disorders, environmental and sociodemographic factors, and iatrogenic causes such as medications or surgical procedures [
8,
9,
10]. DED presents with symptoms ranging from ocular discomfort, a key indicator of disease progression and treatment response, to unstable tear films, epitheliopathy, corneal disease, and conjunctival disease. These symptoms can eventually lead to visual and functional impairment [
11]. In severe cases, DED can result in ocular pathologies such as ulceration, scarring, infectious keratitis, and ultimately, blindness [
10].
Considering the relatively high prevalence of DED, studies have indicated that dry eye disease (DED) has a significant influence on the quality of life [
12]. According to the World Health Organization (WHO), quality of life is defined as an individual’s subjective evaluation of their standing in life, considering the cultural and value systems of their environment. It encompasses their aspirations, expectations, norms, and worries, all within the context of their goals and values [
13]. Many treatment approaches for DED require long-term management, often integrating dry eye treatment regimens into daily routines, which can burden individuals affected by the disease [
12].
Symptoms of DED, including discomfort, blurred vision, and sensitivity to light, have been shown to reduce work efficiency and productivity [
14]. Furthermore, DED is associated with psychological stress, anxiety, and depression, with many affected individuals having a history of seeking psychological counseling [
15]. In light of the significant impact of DED on ocular health and quality of life, this study aimed to examine the relationship between dry eye disease and quality of life, identify influential factors, and estimate the prevalence of DED in Saudi Arabia.
2. Materials and Methods
2.1. Study Design and Setting
This cross-sectional study explored the prevalence of dry eye disease (DED), its determinants, and its impact on quality of life (QoL) among adults in Saudi Arabia. Cross-sectional designs are particularly well-suited for capturing prevalence and associated risk factors at a specific point in time, allowing for an efficient assessment of population health behaviors and outcomes [
16]. Data collection encompassed multiple variables relevant to the population of Saudi Arabia, offering valuable insights about DED prevalence and characteristics in the nation.
2.2. Data Collection Tools
The data collection tool was developed through a review of validated instruments designed to measure dry eye disease (DED) and quality of life (QoL). Experts in ophthalmology and public health were consulted to ensure the questionnaire’s relevance and cultural suitability for the Saudi Arabian context. The final instrument comprised 49 questions, structured into three main sections: demographics, the ocular surface disease index (OSDI), and the Arabic version of the World Health Organization Quality of Life (WHOQOL-BREF).
The first section focused on demographic data, covering variables such as age, gender, employment status, education level, monthly income, residency, and geographical area. The second section was the OSDI—an established measure for assessing DED severity—containing 12 questions administered in Arabic. Participants’ responses were scored from 0 to 100 and classified as normal (0–12), mild (13–22), moderate (23–32), or severe (33–100) [
17,
18]. The third section incorporated the Arabic version of the WHOQOL-BREF questionnaire, which has 26 items to evaluate physical, psychological, social, and environmental dimensions of QoL. Higher scores indicate a better quality of life, and conversely, lower scores indicate a poorer quality of life [
19,
20].
2.3. Data Collection Process
Data collection was conducted entirely online from June to August 2024. During this period, the research team distributed the questionnaires through widely used social media platforms (WhatsApp, Twitter, Telegram, and others). Although no formal training was required for data collectors, the study team received internal briefings to maintain a consistent approach in addressing participant inquiries and clarifying any survey items. Quality control measures were upheld by utilizing validated questionnaires—namely; the ocular surface disease index (OSDI) and the WHOQOL-BREF—for assessing dry eye disease (DED) severity and quality of life (QoL); respectively. Additionally, routine checks were performed to identify and resolve duplicate or incomplete submissions in a timely manner.
Convenience sampling was utilized to recruit adults (18+) residing in Saudi Arabia who signed the informed consent without further restrictions. Individuals who did not meet these criteria (e.g., minors or non-residents) were excluded. As with many survey-based studies on health conditions, participants experiencing DED symptoms may have been more inclined to respond to the survey due to personal relevance, potentially influencing prevalence estimates. This common phenomenon in cross-sectional surveys was taken into account during data interpretation. Participants received clear instructions and could reach out for clarification at any time, ensuring accurate responses and a reliable dataset. This online approach capitalized on the widespread use of social media in Saudi Arabia, enabling a broad coverage of diverse demographic groups while minimizing barriers to participation.
2.4. Study Size
Sample size estimation for the current cross-sectional study was based on the following statistical formula:
where:
is the sample size in terms of the number of participants to be selected;
is the sample design effect;
is the statistic that defines the desired level of confidence;
is an estimate of the key indicator (in this case, dry eye disease prevalence) to be measured by the survey;
is a multiplier to account for the anticipated rate of non-response;
is the margin of error to be attained.
In this study, a total of 1062 participants was determined based on the following assumptions. First, the -statistic of 1.96 corresponded to a 95% level of confidence. The design effect () was set at 2 due to the absence of empirical data suggesting an alternative value. A 20% proportion was applied as the non-response multiplier (). The level of was set at 50% to ensure the largest possible sample size given the unknown prevalence of dry eye disease (DED). Lastly, a margin of error () of 5% was adopted. Although the questionnaire was distributed online through convenience sampling, these parameters served as a methodological guide to capture a representative snapshot of DED prevalence and its impact on quality of life (QoL) among adults in Saudi Arabia.
2.5. Data Analysis
Statistical data analysis was conducted using RStudio (version 4.2.3, R Foundation for Statistical Computing, Vienna, Austria). The main variable in this study was the OSDI score, which was analyzed to determine its relationship with various predictors and the outcome of interest. The predictor variables were divided into two main categories: (1) sociodemographic characteristics, including age, gender, nationality, education level, income, occupation, and marital status; and (2) health-related parameters, such as body mass index (BMI), smoking status, and chronic conditions (diabetes, hypertension, thyroid disease, and dyslipidemia). The outcome variables of interest included the four domains of quality of life (QoL)—physical; psychological; social; and environmental health—assessed using the WHOQOL-BREF questionnaire.
Our analysis began with an overview of the sample characteristics. Categorical variables were described using frequencies and percentages, while continuous variables were summarized with mean values and standard deviations (SDs). The normality of continuous data were evaluated using the Shapiro–Wilk test and visual inspection of Q-Q plots. Multiple linear regression models were then employed to explore the adjusted relationships between dry eye disease (DED) scores and the QoL domains, taking into account the identified predictor variables. The associations were quantified using regression coefficients (β), 95% confidence intervals (CI), and p-values. Statistical significance was determined with a p-value threshold below 0.05.
4. Discussion
This study aimed to investigate the relationship between DED and QoL, identify contributing risk factors, and estimate the prevalence of DED in Saudi Arabia. Our results show that several factors are implicated in the development of DED. In this study, chronic diseases showed a significant correlation with DED. As mentioned, higher OSDI scores were found in those with a history of thyroid illness, hypertension, and diabetes mellitus (DM). These findings emphasize the necessity of considering ocular complications in the management plans of such patients.
Moreover, our findings also raise questions regarding the relationship between DED, QoL, and chronic illness. As seen, thyroid diseases can significantly impact patients’ QoL, raising concerns regarding the possible synergistic effect of DED and chronic diseases on QoL, regardless of whether DED was precipitated by the chronic disease.
Regarding occupation as a risk factor, our results show that students scored higher OSDI scores than those not working. These conclusions underline the critical nature of occupational status as a risk factor, which can be important to consider when assessing for DED.
Another noteworthy finding is the statistical significance of sex as a risk factor for DED, with men having significantly lower OSDI scores than women, indicating a lower risk for DED in males. Interestingly, our results also showed that men had higher physical health scores (QoL domain), further emphasizing our conclusions regarding the relation between DED and physical health.
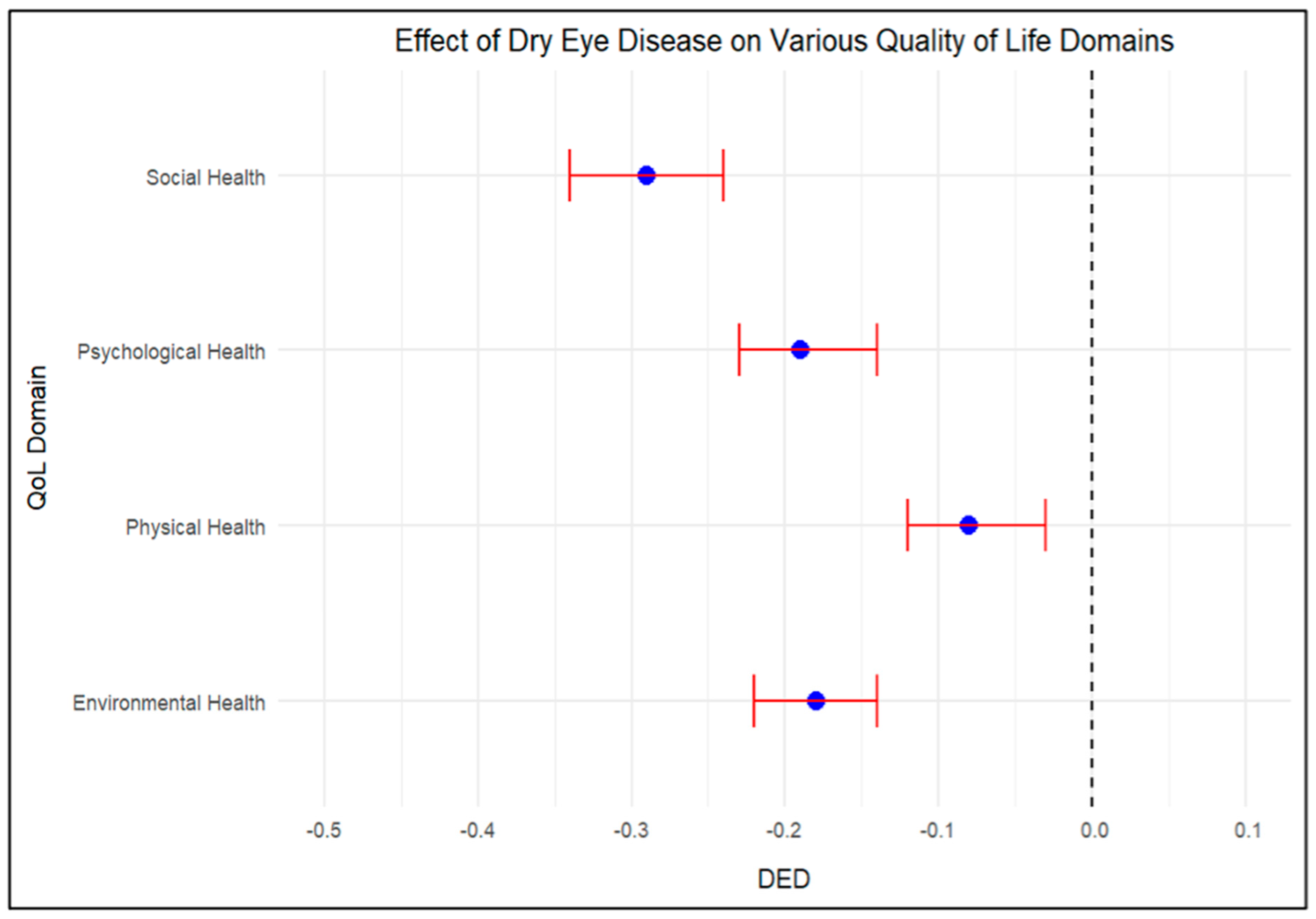
These findings naturally lead to a discussion of QoL, as our results demonstrate a negative correlation between DED and QoL in all its domains. In
Table 6, we notice that there is an increase in DED severity among participants with poorer physical health scores. DED may impair physical activity, potentially leading to reduced physical health. It is important to note that dyslipidemia was also associated with poorer physical health scores. With dyslipidemia being closely associated with physical activity, consideration for DED in such patients is vital.
DED severity was also negatively correlated with psychological health scores. The chronic nature of DED may play a significant role in its association with poorer psychological health, especially in the presence of other significant risk factors for poorer psychological health, like being single. DEDs negative impact on these two domains demonstrates the multidimensional nature of its impact on QoL.
Moreover,
Table 6 demonstrates a strong association between higher DED scores and poorer social health, emphasizing the negative effects of DED on patients’ social functioning and relationships. Notably, higher BMI and cigarette smoking were linked to lower social health, suggesting that these factors may exacerbate the social difficulties faced by individuals with DED. In contrast, being married was associated with better social health, likely reflecting the protective role of social support in mitigating the disease’s adverse effects.
Similarly,
Table 6 reveals a significant correlation between increasing DED severity and declines in environmental health, indicating that DED restricts individuals’ ability to interact with and adapt to their surroundings. These limitations may include difficulties in tolerating bright environments, outdoor activities, or exposure to dust and pollutants, all contributing to a decline in environmental health. The presence of thyroid disease was associated with even poorer environmental outcomes, potentially reflecting the combined effects of thyroid disorders and DED on patients’ ability to engage with their environment. Conversely, higher income appeared to mitigate the negative effects of DED, contributing to better environmental health, likely due to greater access to resources, healthcare, and treatment options that help address the environmental challenges posed by DED.
Figure 3 summarizes the overall impact of DED across all QoL domains, confirming that DED imposes a substantial burden on physical, psychological, social, and environmental well-being. The most pronounced decline was observed in physical health, followed by social, psychological, and environmental health, suggesting that the chronic discomfort and functional limitations associated with DED have far-reaching consequences across multiple aspects of life. These findings highlight the need to address not only the clinical management of DED but also its broader psychosocial and environmental impacts to improve patients’ overall quality of life.
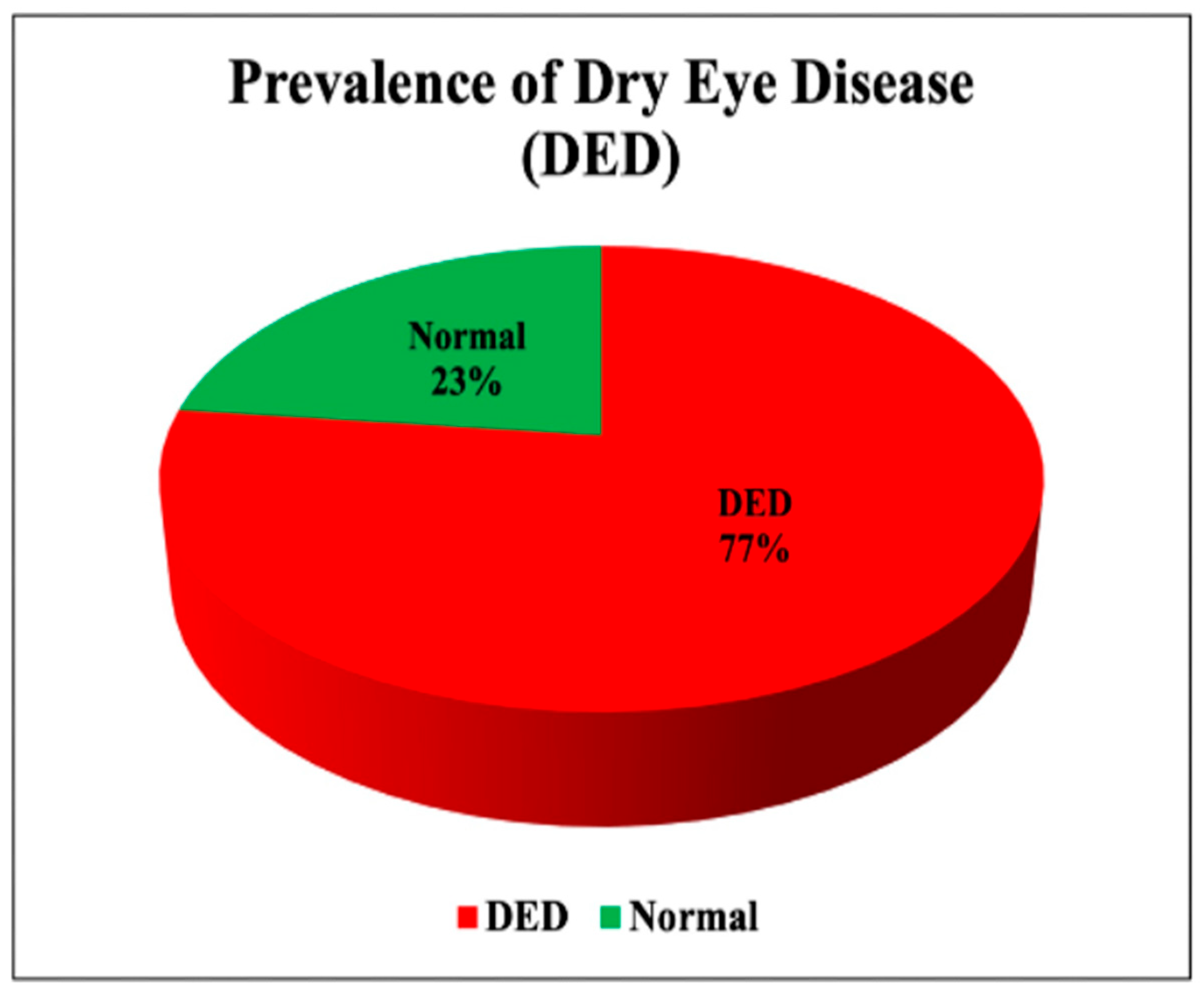
Our finding of 77% DED prevalence is notably higher than global estimates, which typically range from 5 to 50% in general populations [
1,
2]. Several methodological factors may explain this discrepancy. First, online survey distribution may have introduced selection bias, as individuals experiencing DED symptoms might be more motivated to participate. This phenomenon has been observed in other online health surveys, as documented by Toscos et al. [
21], who found that participants excluded from technology-based interventions due to lack of computer/internet access had worse health characteristics and more comorbidities. Second, our study was conducted during summer months in Saudi Arabia, when environmental factors such as higher temperatures, lower humidity, and increased air conditioning use may exacerbate DED symptoms. Van Setten et al. demonstrated that seasonal variation significantly impacts DED, with summer and winter being the two seasons most frequently associated with dry eye complaints (reported by 51% and 43% of patients, respectively) [
22]. Their study of 738 patients across five European countries found that wind (71%), sunshine (60%), and heat (42%) were the most common weather conditions negatively impacting dry eye symptoms.
Furthermore, recent advancements in DED understanding have highlighted its multifactorial nature beyond traditional risk factors. Increasingly recognized contributors include microbiome dysregulation, with research showing that ocular surface inflammation may be triggered by changes in the ocular surface microbiota that influence immune responses [
10]. Altered meibomian gland function has been established as the most common subtype of DED in both clinic and population-based studies, affecting the tear film lipid layer and contributing to tear film instability [
23]. Additionally, neuroinflammatory mechanisms play a critical role in DED pathogenesis, involving bidirectional interactions between the nervous and immune systems, where nerve damage can trigger inflammatory responses while immune cells can affect nerve function through cytokine secretion [
24]. Future studies should incorporate these emerging perspectives to better contextualize prevalence data
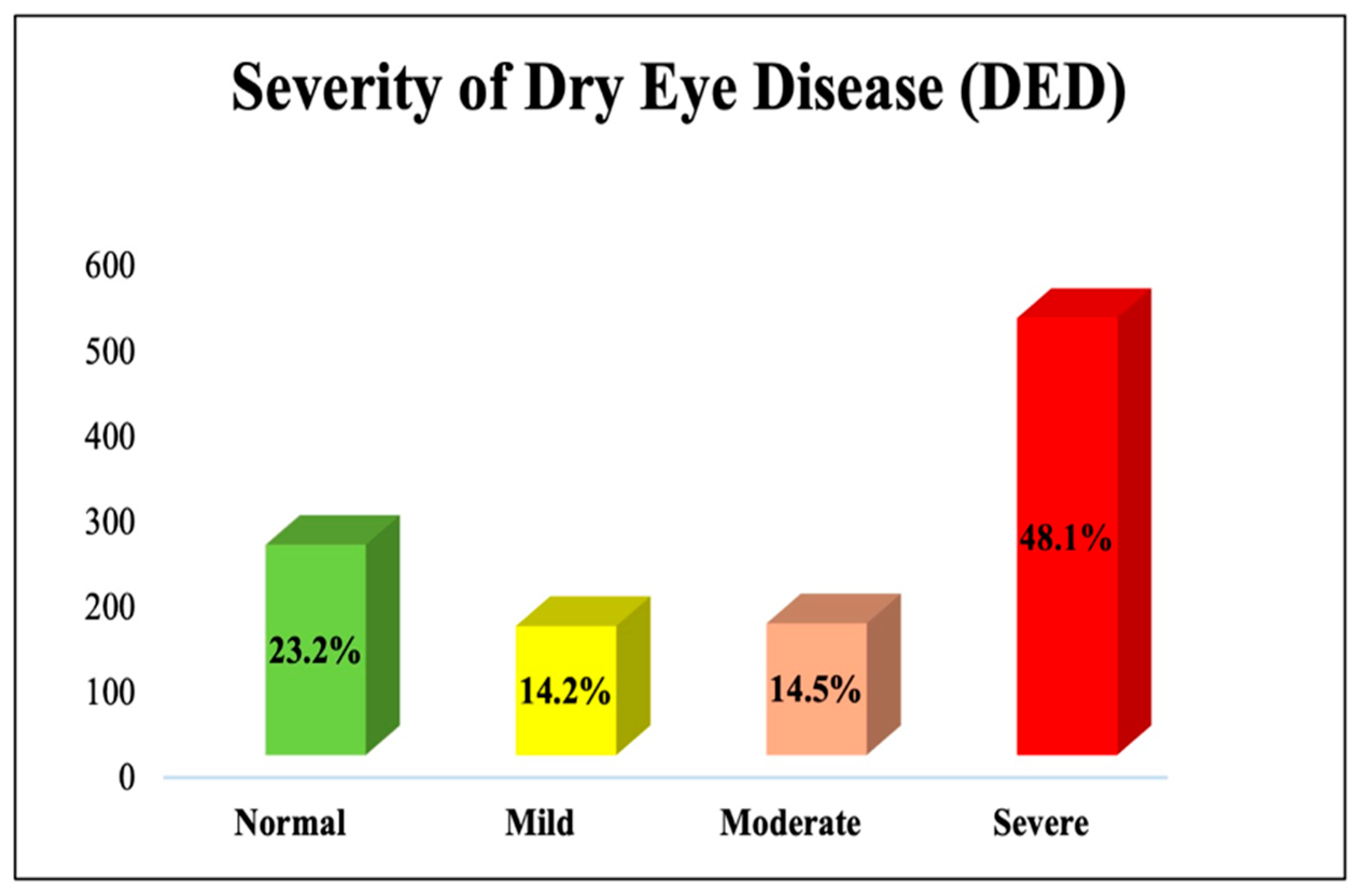
Looking at previously published studies, we can see that most of the conclusions of our study align with theirs. Regarding potential risk factors for DED, a 2022 cross-sectional Saudi study found that DED was more prevalent among females, which is in line with our conclusions. The study also emphasizes our conclusions on the relationship between DED and thyroid diseases, as they found that it increased the risk for DED. On the other hand, we can notice a drastic difference in the prevalence of severe DED, with only 1.7% of their participants having severe DED, in contrast to the significantly higher percentage of our study (48.1%), with both studies using the OSDI scale [
25]. Another Saudi study investigating the prevalence risk factors of DED found that 41.69% is a somewhat similar result to that of our study; however, their conclusions regarding gender, thyroid disease, and diabetes mellitus contradict that of our study, as they found that these factors were not associated with DED. Furthermore, their results show that age significantly correlated with DED, contradicting our conclusions [
26]. Another recent Saudi study with about 4066 participants found the prevalence of severe DED symptoms to be 16.4% and 14.7% of the participants reporting both severe symptoms of DED and a previous diagnosis of DED, contrasting with the 48.1% of our participants reporting severe symptoms. The same study also found that age and being a female correlated with DED, conflicting with our conclusions on age while supporting our conclusions on gender [
4]. Overall, there are inconsistencies across Saudi studies regarding the role of age, diabetes mellitus, thyroid disease, and gender in DED in addition to the variability in the reported prevalence of severe symptoms. Similar inconsistencies are evident in international studies [
27,
28,
29]. Regarding our conclusions on the relationship between DED and QoL, previous studies confirm the negative effect of DED on quality of life; however, no previous study has used the OSDI Questionnaire to assess the severity of DED [
14,
30].
The correlation between DED and chronic diseases can be explained by the systemic inflammatory processes associated with these conditions, which may exacerbate ocular dryness. The greater DED severity observed in men could be linked to differences in occupational exposure, lifestyle, or diagnostic biases. The significant negative impact of DED on QoL, particularly physical health, likely results from the discomfort and limitations it imposes on daily activities. The association between dyslipidemia and poorer physical health highlights the interplay between systemic health conditions and DED. Furthermore, the impact of occupation suggests a complex relationship between physical activity, environmental exposures, and DED symptoms.
The findings highlight the importance of considering DED in the management of chronic diseases and emphasize the need for more targeted interventions that account for both clinical and psychosocial factors. Healthcare providers should incorporate a comprehensive assessment of risk factors, including occupation, sociodemographic status, and comorbidities, when managing DED. Public health efforts should focus on raising awareness of DEDs impact on QoL and encourage lifestyle modifications, such as smoking cessation and weight management, to improve outcomes. Future studies should also investigate the correlation between DED severity classifications and the frequency of symptoms throughout the day, which would provide valuable insights for clinical management and patient education.
This study has several strengths, including a large sample size of 1062 participants and the use of validated tools to assess dry eye disease (DED) severity and quality of life (QoL). The comprehensive analysis of sociodemographic, occupational, and health-related factors provides valuable insights into the multifactorial nature of DED and its broad impact on physical, psychological, social, and environmental well-being. Notably, this is the first nationwide study to explore the association between DED and QoL, filling a critical gap in regional research. However, the cross-sectional design limits the ability to infer causality, and the convenience sampling method may introduce selection bias. Additionally, reliance on self-reported data may lead to recall and response biases. A key limitation was relying exclusively on self-reported symptoms without clinical examination to confirm DED diagnosis. Despite these limitations, this study offers a solid foundation for understanding the impact of DED on QoL and underscores the need for targeted public health interventions and further longitudinal research.