Efficacy and Safety of Nitrous Oxide (N2O) Inhalation Sedation Compared to Other Sedative Agents in Dental Procedures: A Systematic Review with Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Search
2.2. Study Selection
2.3. Definition and Outcome
2.4. Data Extraction and Quality Assessment
2.5. Data Analysis
3. Results
3.1. Study Selection and Characteristics
3.2. Quantitative Synthesis
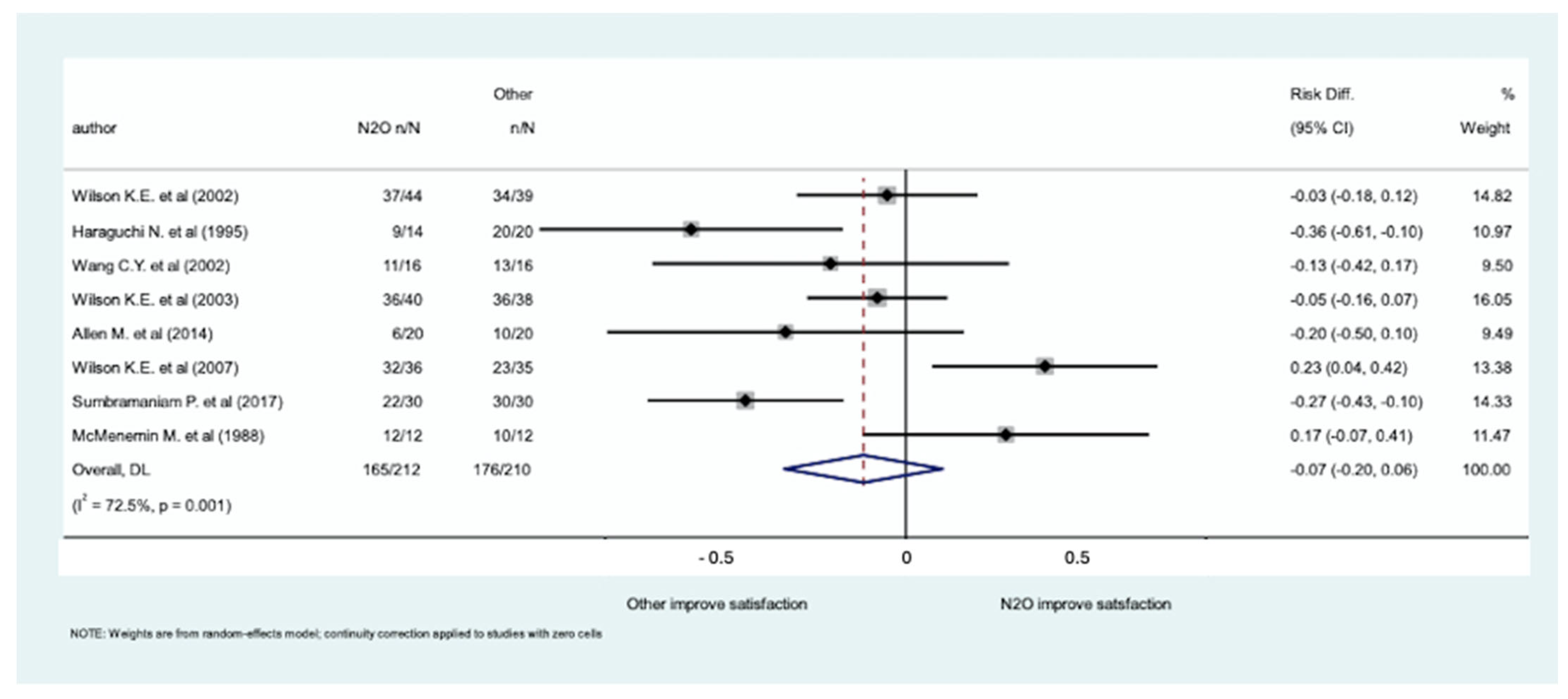
3.2.1. Patient Satisfaction
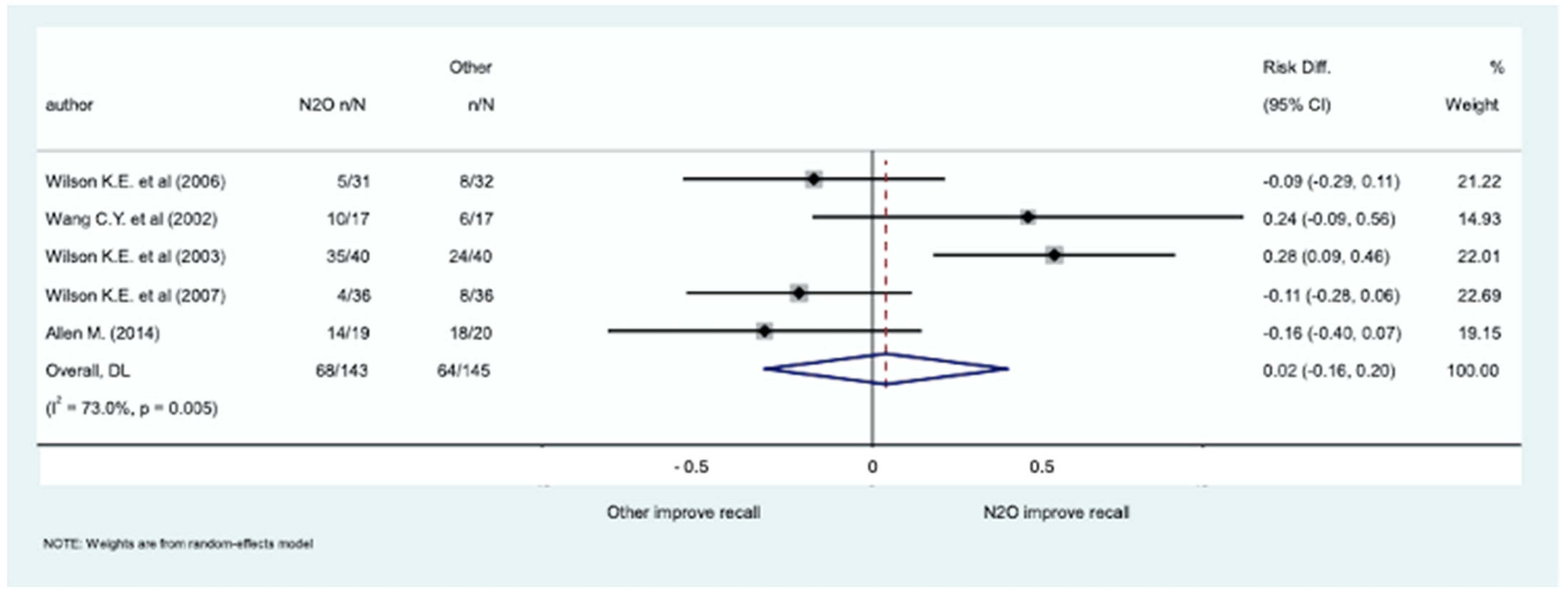
3.2.2. Ability to Recall
3.2.3. Successful Completion of Dental Procedure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pereira-Santos, D.; Brêda-Júnior, M.A.; Ferraz, E.P.; Crippa, G.E.; de Oliveira, F.S.; da Rocha-Barros, V.M. Study comparing midazolam and nitrous oxide in dental anxiety control. J. Craniofac. Surg. 2013, 24, 1636–1639. [Google Scholar] [CrossRef] [PubMed]
- Soldani, F.; Manton, S.; Stirrups, D.R.; Cumming, C.; Foley, J. A comparison of inhalation sedation agents in the management of children receiving dental treatment: A randomized, controlled, cross-over pilot trial. Int. J. Paediatr. Dent. 2010, 20, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Folayan, M.O.; Idehen, E.E.; Ojo, O.O. The modulating effect of culture on the expression of dental anxiety in children: A literature review. Int. J. Paediatr. Dent. 2004, 14, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Ilasrinivasan, J.V.S.; Shyamachalam Mendiretta, P. A Comparative Evaluation of the Sedative Effects of Nitrous Oxide-oxygen Inhalation and Oral Midazolam-Ketamine Combination in Children. Int. J. Clin. Pediatr. Dent. 2018, 11, 399–405. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Milgrom, P.; Newton, J.T.; Boyle, C.; Heaton, L.J.; Donaldson, N. The effects of dental anxiety and irregular attendance on referral for dental treatment under sedation within the National Health Service in London. Community Dent. Oral Epidemiol. 2010, 38, 453–459. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Armfield, J.M.; Stewart, J.F.; Spencer, A.J. The vicious cycle of dental fear: Exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health 2007, 7, 1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abrahamsson, K.H.; Berggren, U.; Hakeberg, M.; Carlsson, S.G. Phobic avoidance and regular dental care in fearful dental patients: A comparative study. Acta Odontol. Scand. 2001, 59, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Schuller, A.A.; Willumsen, T.; Holst, D. Are there differences in oral health and oral health behavior between individuals with high and low dental fear? Community Dent. Oral Epidemiol. 2003, 31, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Dionne, R.A.; Gordon, S.M.; McCullagh, L.M.; Phero, J.C. Assessing the need for anesthesia and sedation in the general population. J. Am. Dent. Assoc. 1998, 129, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Ashley, P.; Anand, P.; Andersson, K. Best clinical practice guidance for conscious sedation of children undergoing dental treatment: An EAPD policy document. Eur. Arch. Paediatr. Dent. 2021, 22, 989–1002. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mishra, N.; Birmiwal, K.G.; Pani, N.; Raut, S.; Sharma, G.; Rath, K.C. Sedation in oral and maxillofacial day care surgery: A comparative study between intravenous dexmedetomidine and midazolam. Natl. J. Maxillofac. Surg. 2016, 7, 178–185. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shapira, J.; Kupietzky, A.; Kadari, A.; Fuks, A.B.; Holan, G. Comparison of oral midazolam with and without hydroxyzine in the sedation of pediatric dental patients. Pediatr. Dent. 2004, 26, 492–496. [Google Scholar] [PubMed]
- Gazal, G.; Fareed, W.M.; Zafar, M.S.; Al-Samadani, K.H. Pain and anxiety management for pediatric dental procedures using various combinations of sedative drugs: A review. Saudi Pharm. J. 2016, 24, 379–385. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jockusch, J.; Sobotta, B.A.J.; Nitschke, I. Outpatient dental care for people with disabilities under general anaesthesia in Switzerland. BMC Oral Health 2020, 20, 225. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choi, J.; Doh, R.M. Dental treatment under general anesthesia for patients with severe disabilities. J. Dent. Anesth. Pain. Med. 2021, 21, 87–98. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mozafar, S.; Bargrizan, M.; Golpayegani, M.V.; Shayeghi, S.; Ahmadi, R. Comparison of nitrous oxide/midazolam and nitrous oxide/promethazine for pediatric dental sedation: A randomized, cross-over, clinical trial. Dent. Res. J. 2018, 15, 411–419. [Google Scholar] [PubMed] [PubMed Central]
- Ramazani, N. Different Aspects of General Anesthesia in Pediatric Dentistry: A Review. Iran. J. Pediatr. 2016, 26, e2613. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- American Academy of Pediatric Dentistry. Policy on patient safety. In The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2022; pp. 176–180. [Google Scholar]
- Galeotti, A.; Garret Bernardin, A.; D’Antò, V.; Ferrazzano, G.F.; Gentile, T.; Viarani, V.; Cassabgi, G.; Cantile, T. Inhalation Conscious Sedation with Nitrous Oxide and Oxygen as Alternative to General Anesthesia in Precooperative, Fearful, and Disabled Pediatric Dental Patients: A Large Survey on 688 Working Sessions. Biomed Res. Int. 2016, 2016, 7289310. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ashley, P.F.; Chaudhary, M.; Lourenço-Matharu, L. Sedation of children undergoing dental treatment. Cochrane Database Syst. Rev. 2018, 12, Cd003877. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Evers, A.S.C.C.M.; Balser, J.R. General anesthetics. In Goodman and Gilman’s the Pharmacological Basis of Therapeutics, 11th ed.; Brunton, L.L., Lazo, J.S., Parker, K.L., Eds.; McGraw-Hill: New York, NY, USA, 2006. [Google Scholar]
- Becker, D.E.; Rosenberg, M. Nitrous oxide and the inhalation anesthetics. Anesth. Prog. 2008, 55, 124–130; quiz 131–132. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, C.; Davies, M.F.; Guo, T.Z.; Maze, M. The analgesic action of nitrous oxide is dependent on the release of norepinephrine in the dorsal horn of the spinal cord. Anesthesiology 1999, 91, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Emmanouil, D.E.; Quock, R.M. Advances in understanding the actions of nitrous oxide. Anesth. Prog. 2007, 54, 9–18. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sanders, R.D.; Weimann, J.; Maze, M. Biologic effects of nitrous oxide: A mechanistic and toxicologic review. Anesthesiology 2008, 109, 707–722. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wilson, K.E.; Welbury, R.R.; Girdler, N.M. A randomised, controlled, crossover trial of oral midazolam and nitrous oxide for paediatric dental sedation. Anaesthesia 2002, 57, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Haraguchi, N.; Furusawa, H.; Takezaki, R.; Oi, K. Inhalation sedation with sevoflurane: A comparative study with nitrous oxide. J. Oral Maxillofac. Surg. 1995, 53, 24–26; discussion 26–27. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.Y.; Chiu, C.L.; Har, K.O.; Chan, C.; Rahman, Z.A.A. A comparative study of sevoflurane sedation with nitrous oxide sedation for dental surgery. Int. J. Oral Maxillofac. Surg. 2002, 31, 506–510. [Google Scholar] [CrossRef]
- Allen, M.; Thompson, S. An equivalence study comparing nitrous oxide and oxygen with low-dose sevoflurane and oxygen as inhalation sedation agents in dentistry for adults. Br. Dent. J. 2014, 217, E18. [Google Scholar] [CrossRef]
- Wilson, K.E.; Welbury, R.R.; Girdler, N.M. Comparison of transmucosal midazolam with inhalation sedation for dental extractions in children. A randomized, cross-over, clinical trial. Acta Anaesthesiol. Scand. 2007, 51, 1062–1067. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, P.; Babu Kl, G.; Lakhotia, D. Evaluation of nitrous oxide-oxygen and triclofos sodium as conscious sedative agents. J. Indian Soc. Pedod. Prev. Dent. 2017, 35, 156–161. [Google Scholar] [CrossRef] [PubMed]
- McMenemin, I.M.; Parbrook, G.D. Comparison of the Effects of Subanaesthetic Concentrations of Isoflurane or Nitrous Oxide in Volunteers. Br. J. Anaesth. 1988, 60, 56–63. [Google Scholar] [CrossRef]
- Wilson, K.E.; Girdler, N.M.; Welbury, R.R. A comparison of oral midazolam and nitrous oxide sedation for dental extractions in children. Anaesthesia 2006, 61, 1138–1144. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.E.; Girdler, N.M.; Welbury, R.R. Randomized, controlled, cross-over clinical trial comparing intravenous midazolam sedation with nitrous oxide sedation in children undergoing dental extractions. Br. J. Anaesth. 2003, 91, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Lahoud, G.Y.; Averley, P.A. Comparison of sevoflurane and nitrous oxide mixture with nitrous oxide alone for inhalation conscious sedation in children having dental treatment: A randomised controlled trial. Anaesthesia 2002, 57, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Hulland, S.A.; Freilich, M.M.; Sàndor, G.K. Nitrous oxide-oxygen or oral midazolam for pediatric outpatient sedation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 93, 643–646. [Google Scholar] [CrossRef] [PubMed]


| Participants | Intervention | Comparison | Outcomes | Study Design |
|---|---|---|---|---|
| Adult and pediatric patients undergoing dental procedures | N2O inhalation sedation | Any sedative medication or placebo or no medication | Patient satisfaction; recall; success; adverse events | Cross-sectional, case–control, cohort, and RCTs |
| Author (Publ. Year) [Ref.] | N. of Patients Enrolled | N. of Patients Treated with N2O | N. of Patients Treated with Other Medications | Other Medication | Study Design | Adults/ Children | Patient Satisfaction Evaluation |
|---|---|---|---|---|---|---|---|
| Wilson K.E. et al. (2002) [29] | 83 | 44 | 39 | Oral midazolam | RCT crossover | Children | Questionnaire: pleasant, acceptable, and unpleasant |
| Haraguchi N. et al. (1995) [30] | 34 | 14 | 20 | Sevoflurane | RCT | Adults | Questionnaire: odour, general opinion, and would have same inhalation again |
| Wang C.Y. et al. (2002) [31] | 32 | 16 | 16 | Sevoflurane | RCT crossover | Adults | Patient intraoperative feeling VAS (0 = pleasant; 10 = unpleasant) |
| Wilson K.E. et al. (2003) [29] | 78 | 40 | 38 | Intravenous midazolam | RCT crossover | Children | Questionnaire: pleasant, acceptable, and unpleasant; preferred type of sedation |
| Allen M. et al. (2014) [32] | 40 | 20 | 20 | Sevoflurane | RCT | Adults | Questionnaire: pleasant and not pleasant |
| Wilson K.E. et al. (2007) [33] | 71 | 36 | 35 | Sublingual midazolam | RCT crossover | Adolescents | Questionnaire: how they felt about sedarion, what they liked or disliked, and preferred type of sedation |
| Sumbramaniam P. et al. (2017) [34] | 60 | 30 | 30 | Oral triclofos sodium | RCT | Children | Patient’s acceptance of route of administration |
| McMenemin M. et al. (1988) [35] | 24 | 12 | 12 | Isoflurane | Prospective crossover trial | Adults | VAS scale of level of sedation and mood; pleasant or unpleasant |
| Author (Publ. Year) [Ref.] | N. of Patients Enrolled | N. of Patients Treated with N2O | N. of Patients Treated with Other Medications | Other Medication | Study Design | Adults/ Children |
|---|---|---|---|---|---|---|
| Wilson K.E. et al. (2006) [36] | 63 | 31 | 32 | Oral midazolam | RCT crossover | Children |
| Wang C.Y. et al. (2002) [31] | 34 | 17 | 17 | Sevoflurane | RCT crossover | Adults |
| Wilson K.E. et al. (2003) [37] | 80 | 40 | 40 | Intravenous midazolam | RCT crossover | Children |
| Wilson K.E. et al. (2007) [33] | 72 | 36 | 36 | Sublingual midazolam | RCT crossover | Adolescents |
| Allen M. (2014) [32] | 39 | 19 | 20 | Sevoflurane | RCT | Adults |
| Author (Publ. Year) [Ref.] | N. of Patients Enrolled | N. of Patients Treated with N2O | N. of Patients Treated with Other Medications | Other Medication | Study Design | Adults/ Children |
|---|---|---|---|---|---|---|
| Lahoud G.Y. et al. (2002) [38] | 411 | 170 | 241 | Sevoflurane + N2O | RCT | Children |
| Hulland S.A. et al. (2002) [39] | 1112 | 326 | 786 | Oral midazolam | RCT | Children |
| Soldani F. et al. (2010) [2] | 55 | 29 | 26 | N2O + sevoflurane | RCT crossover | Children |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piccialli, F.; Fiore, M.; Giurazza, R.; Falso, F.; Simeon, V.; Chiodini, P.; Russo, D.; Laino, L. Efficacy and Safety of Nitrous Oxide (N2O) Inhalation Sedation Compared to Other Sedative Agents in Dental Procedures: A Systematic Review with Meta-Analysis. Medicina 2025, 61, 929. https://doi.org/10.3390/medicina61050929
Piccialli F, Fiore M, Giurazza R, Falso F, Simeon V, Chiodini P, Russo D, Laino L. Efficacy and Safety of Nitrous Oxide (N2O) Inhalation Sedation Compared to Other Sedative Agents in Dental Procedures: A Systematic Review with Meta-Analysis. Medicina. 2025; 61(5):929. https://doi.org/10.3390/medicina61050929
Chicago/Turabian StylePiccialli, Francesca, Marco Fiore, Roberto Giurazza, Fabrizio Falso, Vittorio Simeon, Paolo Chiodini, Diana Russo, and Luigi Laino. 2025. "Efficacy and Safety of Nitrous Oxide (N2O) Inhalation Sedation Compared to Other Sedative Agents in Dental Procedures: A Systematic Review with Meta-Analysis" Medicina 61, no. 5: 929. https://doi.org/10.3390/medicina61050929
APA StylePiccialli, F., Fiore, M., Giurazza, R., Falso, F., Simeon, V., Chiodini, P., Russo, D., & Laino, L. (2025). Efficacy and Safety of Nitrous Oxide (N2O) Inhalation Sedation Compared to Other Sedative Agents in Dental Procedures: A Systematic Review with Meta-Analysis. Medicina, 61(5), 929. https://doi.org/10.3390/medicina61050929









