Sex Differences in the In-Hospital Mortality of Patients with Acute Myocardial Infarction: A Cross-Sectional Study in 36 Hospitals Across Germany
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Study Population
2.3. Study Outcome and Covariables
2.4. Statistical Analyses
3. Results
3.1. Baseline Characteristics
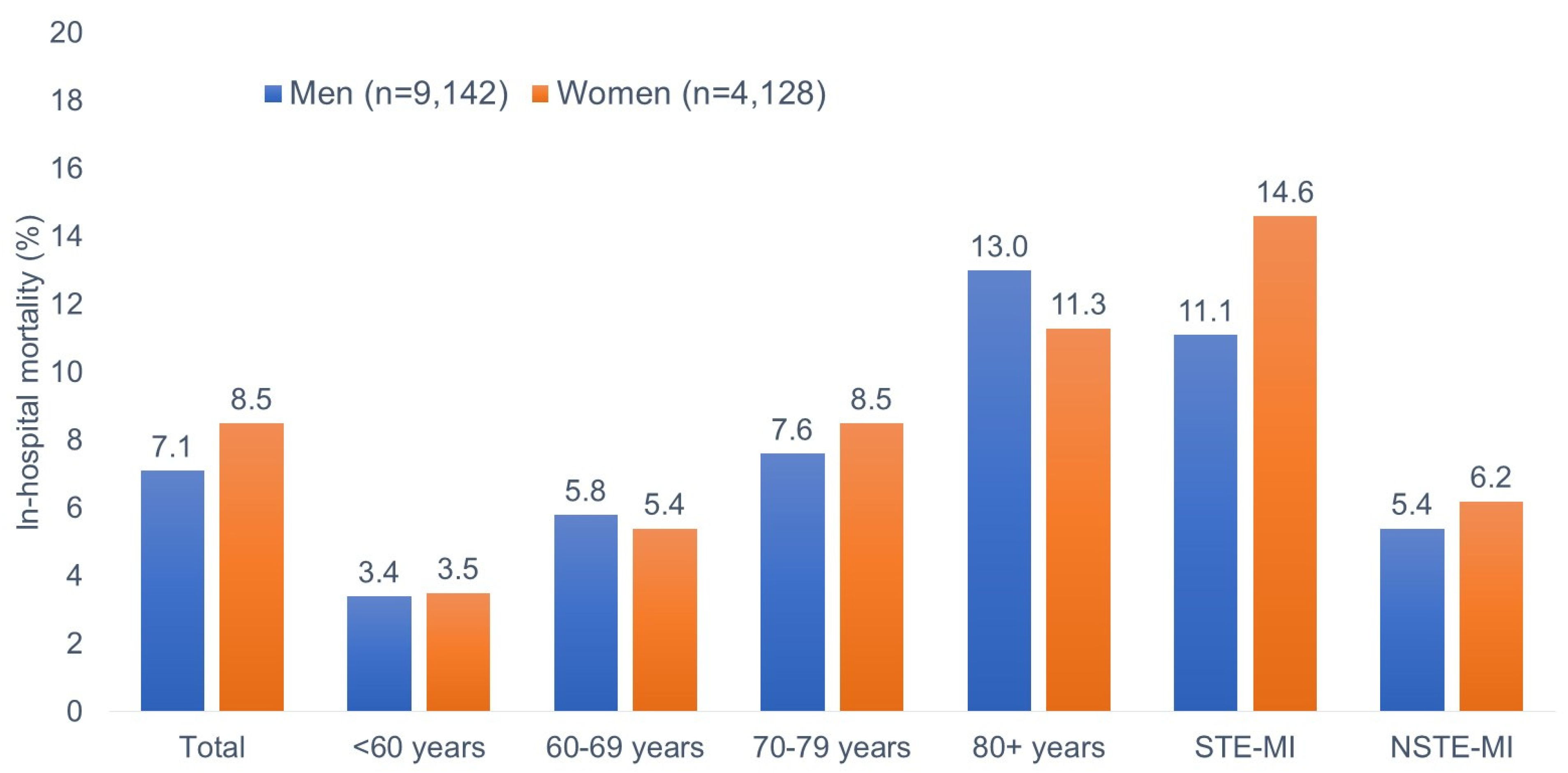
3.2. Prevalence of In-Hospital Mortality
3.3. Association Between Female Sex and In-Hospital Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martin, S.S.; Aday, A.W.; Allen, N.B.; Almagro, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Bansal, N.; Beaton, A.Z.; et al. 2025 Heart Disease and Stroke Statistics: A Report of US and Global Data from the American Heart Association. Circulation 2025, 151, e41–e660. [Google Scholar] [CrossRef] [PubMed]
- Zuin, M.; Rigatelli, G.; Temporelli, P.; Di Fusco, S.A.; Colivicchi, F.; Pasquetto, G.; Bilato, C. Trends in acute myocardial infarction mortality in the European Union, 2012–2020. Eur. J. Prev. Cardiol. 2023, 30, 1758–1771. [Google Scholar] [CrossRef] [PubMed]
- de Miguel-Yanes, J.M.; Jiménez-García, R.; Hernandez-Barrera, V.; de Miguel-Díez, J.; Muñoz-Rivas, N.; Méndez-Bailón, M.; Pérez-Farinós, N.; López-Herranz, M.; Lopez-De-Andres, A. Sex Differences in the Incidence and Outcomes of Acute Myocardial Infarction in Spain, 2016–2018: A Matched-Pair Analysis. J. Clin. Med. 2021, 10, 1795. [Google Scholar] [CrossRef] [PubMed]
- DeFilippis, E.M.; Collins, B.L.; Singh, A.; Biery, D.W.; Fatima, A.; Qamar, A.; Berman, A.N.; Gupta, A.; Cawley, M.; Wood, M.J.; et al. Women who experience a myocardial infarction at a young age have worse outcomes compared with men: The Mass General Brigham YOUNG-MI registry. Eur. Heart J. 2020, 41, 4127–4137. [Google Scholar] [CrossRef] [PubMed]
- Shah, T.; Haimi, I.; Yang, Y.; Gaston, S.; Taoutel, R.; Mehta, S.; Lee, H.J.; Zambahari, R.; Baumbach, A.; Henry, T.D.; et al. Meta-Analysis of Gender Disparities in In-hospital Care and Outcomes in Patients with ST-Segment Elevation Myocardial Infarction. Am. J. Cardiol. 2021, 147, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Cenko, E.; Yoon, J.; Bergami, M.; Gale, C.P.; Vasiljevic, Z.; Vavlukis, M.; Kedev, S.; Miličić, D.; Dorobantu, M.; Badimon, L.; et al. Coronary revascularization and sex differences in cardiovascular mortality after myocardial infarction in 12 high and middle-income European countries. Eur. Heart J. Qual. Care Clin. Outcomes 2024, qcae035. [Google Scholar] [CrossRef]
- Alkhouli, M.; Alqahtani, F.; Jneid, H.; Al Hajji, M.; Boubas, W.; Lerman, A. Age-Stratified Sex-Related Differences in the Incidence, Management, and Outcomes of Acute Myocardial Infarction. Mayo Clin. Proc. 2021, 96, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Kuehnemund, L.; Koeppe, J.; Feld, J.; Wiederhold, A.; Illner, J.; Makowski, L.; Gerß, J.; Reinecke, H.; Freisinger, E. Gender differences in acute myocardial infarction-A nationwide German real-life analysis from 2014 to 2017. Clin. Cardiol. 2021, 44, 890–898. [Google Scholar] [CrossRef] [PubMed]
- Krämer, C.; Meisinger, C.; Kirchberger, I.; Heier, M.; Kuch, B.; Thilo, C.; Linseisen, J.; Amann, U. Epidemiological trends in mortality, event rates and case fatality of acute myocardial infarction from 2004 to 2015: Results from the KORA MI registry. Ann. Med. 2021, 53, 2142–2152. [Google Scholar] [CrossRef] [PubMed]
- Nichols, M.; Townsend, N.; Scarborough, P.; Rayner, M. Cardiovascular disease in Europe: Epidemiological update. Eur. Heart J. 2013, 34, 3028–3034. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Padial, L.; Fernández-Pérez, C.; Bernal, J.L.; Anguita, M.; Sambola, A.; Fernández-Ortiz, A.; Elola, F.J. Differences in in-hospital mortality after STEMI versus NSTEMI by sex. Eleven-year trend in the Spanish National Health Service. Rev. Esp. Cardiol. Engl. Ed. 2021, 74, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Ye, G.; Pattisapu, V.K.; Wang, P.; Cheng, L.; Yao, S.; Hao, H. Sex Differences and Temporal Trends in Revascularization and Outcomes of ST-Elevation Myocardial Infarction in Older Adults in the United States. Arch. Med. Res. 2022, 53, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Elbadawi, A.; Elgendy, I.Y.; Megaly, M.; Ogunbayo, G.O.; Krittanawong, C.; Tamis-Holland, J.E.; Ballantyne, C.M.; Khalid, M.U.; Virani, S.; et al. Age-Stratified Sex Disparities in Care and Outcomes in Patients With ST-Elevation Myocardial Infarction. Am. J. Med. 2020, 133, 1293–1301.e1. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhang, Y.; Cheng, Q.; Qi, D.; Wang, X.; Zhu, Z.; Li, M.; Zhang, J.; Hu, D.; Gao, C.; et al. Sex Disparity in Characteristics, Management, and In-Hospital Outcomes of Patients with ST-Segment Elevated Myocardial Infarction: Insights from Henan STEMI Registry. Cardiol. Res. Pract. 2022, 2022, 2835485. [Google Scholar] [CrossRef] [PubMed]
- Hassani, N.S.; Mozafarybazargany, M.; Pirdehghan, R.; Sepahvandi, R.; Khodaprast, Z.; Karimi, F.; Rahimi, F.; Zakani, A.; Mardi, P.; Kamipoor, Z.; et al. The Outcome of ST-elevation Myocardial Infarction by Sex: A Retrospective Cohort Study. Futur. Cardiol. 2023, 19, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Stehli, J.; Dinh, D.; Dagan, M.; Duffy, S.J.; Brennan, A.; Smith, K.; Andrew, E.; Nehme, Z.; Reid, C.M.; Lefkovits, J.; et al. Sex Differences in Prehospital Delays in Patients with ST-Segment-Elevation Myocardial Infarction Undergoing Percutaneous Coronary Intervention. J. Am. Heart Assoc. 2021, 10, e019938. [Google Scholar] [CrossRef] [PubMed]
- Blümel, M.; Spranger, A.; Achstetter, K.; Maresso, A.; Busse, R. Germany: Health System Review. Health Syst. Transit. 2020, 22, 1–272. [Google Scholar] [PubMed]
- Pilarczyk, K.; Boeken, U.; Russ, M.; Briegel, J.; Buerke, M.; Geppert, A.; Janssens, U.; Kelm, M.; Michels, G.; Schlitt, A.; et al. Second Edition of the German–Austrian S3 Guideline “Infarction-Related Cardiogenic Shock: Diagnosis, Monitoring and Treatment”. Hearts 2024, 5, 142–164. [Google Scholar] [CrossRef]
| Women (n = 4128) | Men (n = 9142) | p-Value | |
|---|---|---|---|
| Age | |||
| Mean age (SD) | 74.4 (12.3) | 67.7 (12.8) | <0.001 |
| <60 years, n (%) | 651 (13.6) | 2583 (28.3) | <0.001 |
| 60–69 years, n (%) | 729 (17.7) | 2401 (26.3) | |
| 70–79 years, n (%) | 1088 (26.3) | 2158 (23.6) | |
| 80+ years, n (%) | 1750 (42.4) | 2000 (21.9) | |
| MI type, n (%) | |||
| STE-MI | 1208 (29.3) | 3041 (33.3) | <0.001 |
| NSTE-MI | 2920 (70.7) | 6101 (66.7) | |
| Secondary diagnosis, n (%) | |||
| Hypothyroidism | 774 (18.8) | 607 (6.6) | <0.001 |
| Diabetes mellitus | 1168 (28.3) | 2573 (28.1) | 0.859 |
| Lipid metabolism disorders | 1865 (45.2) | 4773 (52.2) | <0.001 |
| Hypokalemia | 570 (13.8) | 871 (9.5) | <0.001 |
| Hypertension | 2567 (62.2) | 5622 (61.5) | 0.450 |
| Chronic ischemic heart disease | 3366 (81.5) | 8374 (91.6) | <0.001 |
| Atrial fibrillation and flutter | 967 (23.4) | 1795 (19.6) | <0.001 |
| Heart failure | 1336 (32.4) | 2778 (30.4) | 0.023 |
| Nonrheumatic valve disorders | 467 (11.3) | 670 (7.3) | <0.001 |
| Atherosclerosis | 224 (5.4) | 469 (5.1) | 0.478 |
| COPD | 282 (6.8) | 484 (5.3) | <0.001 |
| Chronic kidney disease | 728 (17.6) | 1151 (12.6) | <0.001 |
| Multivariable Model | ||
|---|---|---|
| Subgroup | OR for Females Versus Males (95% CIs) | p-Value |
| Total | 0.89 (0.77–1.04) | 0.131 |
| <60 years | 1.10 (0.64–1.89) | 0.739 |
| 60–69 years | 0.90 (061–1.33) | 0.590 |
| 70–79 years | 1.02 (0.76–1.36) | 0.896 |
| 80+ years | 0.79 (0.64–0.97) | 0.027 |
| STE-MI | 0.99 (0.78–1.25) | 0.910 |
| NSTE-MI | 0.84 (0.69–1.03) | 0.094 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kostev, K.; Kaur, N.; Kluge, S.; Konrad, M.; Sedighi, J.; Lüdde, M. Sex Differences in the In-Hospital Mortality of Patients with Acute Myocardial Infarction: A Cross-Sectional Study in 36 Hospitals Across Germany. Medicina 2025, 61, 891. https://doi.org/10.3390/medicina61050891
Kostev K, Kaur N, Kluge S, Konrad M, Sedighi J, Lüdde M. Sex Differences in the In-Hospital Mortality of Patients with Acute Myocardial Infarction: A Cross-Sectional Study in 36 Hospitals Across Germany. Medicina. 2025; 61(5):891. https://doi.org/10.3390/medicina61050891
Chicago/Turabian StyleKostev, Karel, Nimran Kaur, Sabine Kluge, Marcel Konrad, Jamschid Sedighi, and Mark Lüdde. 2025. "Sex Differences in the In-Hospital Mortality of Patients with Acute Myocardial Infarction: A Cross-Sectional Study in 36 Hospitals Across Germany" Medicina 61, no. 5: 891. https://doi.org/10.3390/medicina61050891
APA StyleKostev, K., Kaur, N., Kluge, S., Konrad, M., Sedighi, J., & Lüdde, M. (2025). Sex Differences in the In-Hospital Mortality of Patients with Acute Myocardial Infarction: A Cross-Sectional Study in 36 Hospitals Across Germany. Medicina, 61(5), 891. https://doi.org/10.3390/medicina61050891







