Prevalence of Severe Hypercholesterolemia and Familial Hypercholesterolemia Phenotype in Patients with Acute Coronary Syndrome
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Di Cesare, M.; Perel, P.; Taylor, S.; Kabudula, C.; Bixby, H.; Gaziano, T.A.; McGhie, D.V.; Mwangi, J.; Pervan, B.; Narula, J.; et al. The Heart of the World. Glob. Heart 2024, 19, 11. [Google Scholar] [CrossRef]
- Ralapanawa, U.; Sivakanesan, R. Epidemiology and the Magnitude of Coronary Artery Disease and Acute Coronary Syndrome: A Narrative Review. J. Epidemiol. Glob. Health 2021, 11, 169. [Google Scholar] [CrossRef]
- Johansson, S.; Rosengren, A.; Young, K.; Jennings, E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: A systematic review. BMC Cardiovasc. Disord. 2017, 17, 53. [Google Scholar] [CrossRef] [PubMed]
- Tušek-Bunc, K.; Petek, D. Comorbidities and characteristics of coronary heart disease patients: Their impact on health-related quality of life. Health Qual. Life Outcomes 2016, 14, 159. [Google Scholar] [CrossRef]
- Libby, P.; Buring, J.E.; Badimon, L.; Hansson, G.K.; Deanfield, J.; Bittencourt, M.S.; Tokgözoğlu, L.; Lewis, E.F. Atherosclerosis. Nat. Rev. Dis. Primer 2019, 5, 56. [Google Scholar] [CrossRef]
- Lechner, K.; Von Schacky, C.; McKenzie, A.L.; Worm, N.; Nixdorff, U.; Lechner, B.; Kränkel, N.; Halle, M.; Krauss, R.M.; Scherr, J. Lifestyle factors and high-risk atherosclerosis: Pathways and mechanisms beyond traditional risk factors. Eur. J. Prev. Cardiol. 2020, 27, 394–406. [Google Scholar] [CrossRef] [PubMed]
- Pirillo, A.; Casula, M.; Olmastroni, E.; Norata, G.D.; Catapano, A.L. Global epidemiology of dyslipidaemias. Nat. Rev. Cardiol. 2021, 18, 689–700. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; De Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, 25. [Google Scholar] [CrossRef]
- Julius, U. Lipoprotein apheresis in the management of severe hypercholesterolemia and of elevation of lipoprotein(a): Current perspectives and patient selection. Med. Devices Evid. Res. 2016, 9, 349–360. [Google Scholar] [CrossRef]
- Song, Y.; Liu, J.; Zhao, K.; Gao, L.; Zhao, J. Cholesterol-induced toxicity: An integrated view of the role of cholesterol in multiple diseases. Cell Metab. 2021, 33, 1911–1925. [Google Scholar] [CrossRef]
- Yanai, H.; Yoshida, H. Secondary dyslipidemia: Its treatments and association with atherosclerosis. Glob. Health Med. 2021, 3, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Leal, L.G.; Hoggart, C.; Jarvelin, M.; Herzig, K.; Sternberg, M.J.E.; David, A. A polygenic biomarker to identify patients with severe hypercholesterolemia of polygenic origin. Mol. Genet. Genomic Med. 2020, 8, e1248. [Google Scholar] [CrossRef]
- Beheshti, S.O.; Madsen, C.M.; Varbo, A.; Nordestgaard, B.G. Worldwide Prevalence of Familial Hypercholesterolemia. J. Am. Coll. Cardiol. 2020, 75, 2553–2566. [Google Scholar] [CrossRef] [PubMed]
- Gencer, B.; Nanchen, D. Identifying familial hypercholesterolemia in acute coronary syndrome. Curr. Opin. Lipidol. 2016, 27, 375–381. [Google Scholar] [CrossRef]
- Pang, J.; Hu, M.; Lin, J.; Miida, T.; Nawawi, H.M.; Park, J.E.; Wu, X.; Ramli, A.S.; Kim, N.T.; Kwok, S.; et al. An enquiry based on a standardised questionnaire into knowledge, awareness and preferences concerning the care of familial hypercholesterolaemia among primary care physicians in the Asia-Pacific region: The “Ten Countries Study”. BMJ Open 2017, 7, e017817. [Google Scholar] [CrossRef]
- Kutkiene, S.; Petrulioniene, Z.; Laucevicius, A.; Cerkauskiene, R.; Staigyte, J.; Saulyte, A.; Petrulionyte, E.; Gargalskaite, U.; Skiauteryte, E.; Matuzeviciene, G.; et al. Lipid profile evaluation and severe hypercholesterolaemia screening in the middle-aged population according to nationwide primary prevention programme in Lithuania. Atherosclerosis 2018, 277, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Wulff, A.B.; Mortensen, M.B.; Nordestgaard, B.G. Low-density lipoprotein cholesterol cannot be too low after a myocardial infarction. J. Intern. Med. 2023, 294, 540–542. [Google Scholar] [CrossRef]
- Balci, B. The Modification of Serum Lipids after Acute Coronary Syndrome and Importance in Clinical Practice. Curr. Cardiol. Rev. 2012, 7, 272–276. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Van Driel, M.L.; Morledge, M.D.; Ulep, R.; Shaffer, J.P.; Davies, P.; Deichmann, R. Interventions to improve adherence to lipid-lowering medication. Cochrane Database Syst. Rev. 2016, 2021, 20. [Google Scholar] [CrossRef]
- Wang, Y.; Xu, D. Effects of aerobic exercise on lipids and lipoproteins. Lipids Health Dis. 2017, 16, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.J.; Park, S.; Han, K.; Lee, S. Cardiovascular Risk and Treatment Outcomes in Severe Hypercholesterolemia: A Nationwide Cohort Study. J. Am. Heart Assoc. 2022, 11, e024379. [Google Scholar] [CrossRef] [PubMed]
- Saadatagah, S.; Alhalabi, L.; Farwati, M.; Zordok, M.; Bhat, A.; Smith, C.Y.; Wood-Wentz, C.M.; Bailey, K.R.; Kullo, I.J. The burden of severe hypercholesterolemia and familial hypercholesterolemia in a population-based setting in the US. Am. J. Prev. Cardiol. 2022, 12, 100393. [Google Scholar] [CrossRef]
- Eid, W.E.; Sapp, E.H.; McCreless, T.; Nolan, J.R.; Flerlage, E. Prevalence and Characteristics of Patients With Primary Severe Hypercholesterolemia in a Multidisciplinary Healthcare System. Am. J. Cardiol. 2020, 132, 59–65. [Google Scholar] [CrossRef]
- Safarova, M.S.; Liu, H.; Kullo, I.J. Rapid identification of familial hypercholesterolemia from electronic health records: The SEARCH study. J. Clin. Lipidol. 2016, 10, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Akioyamen, L.E.; Chu, A.; Genest, J.; Lee, D.S.; Abdel-Qadir, H.; Jackevicius, C.A.; Lawler, P.R.; Sud, M.; Udell, J.A.; Wijeysundera, H.C.; et al. Prevalence and Treatment of Familial Hypercholesterolemia and Severe Hypercholesterolemia in Older Adults in Ontario, Canada. CJC Open 2022, 4, 739–747. [Google Scholar] [CrossRef]
- Pajak, A.; Szafraniec, K.; Polak, M.; Drygas, W.; Piotrowski, W.; Zdrojewski, T.; Jankowski, P. Prevalence of familial hypercholesterolemia: A meta-analysis of six large, observational, population-based studies in Poland. Arch. Med. Sci. 2016, 4, 687–696. [Google Scholar] [CrossRef]
- Canto, J.G.; Kiefe, C.I.; Rogers, W.J.; Peterson, E.D.; Frederick, P.D.; French, W.J.; Gibson, C.M.; Pollack, C.V.; Ornato, J.P.; Zalenski, R.J.; et al. Number of Coronary Heart Disease Risk Factors and Mortality in Patients With First Myocardial Infarction. JAMA 2011, 306, 2120–2127. [Google Scholar] [CrossRef]
- Ong, K.L.; Stafford, L.K.; McLaughlin, S.A.; Boyko, E.J.; Vollset, S.E.; Smith, A.E.; Dalton, B.E.; Duprey, J.; Cruz, J.A.; Hagins, H.; et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. The Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef]
- Lee, C.J.; Park, S.; Han, K.; Lee, S.-H. Impact of Severe Hypercholesterolemia on Cardiovascular Risk in Individuals With or Without Diabetes Mellitus. J. Lipid Atheroscler. 2022, 11, 299. [Google Scholar] [CrossRef]
- Roeters Van Lennep, J.E.; Tokgözoğlu, L.S.; Badimon, L.; Dumanski, S.M.; Gulati, M.; Hess, C.N.; Holven, K.B.; Kavousi, M.; Kayıkçıoğlu, M.; Lutgens, E.; et al. Women, lipids, and atherosclerotic cardiovascular disease: A call to action from the European Atherosclerosis Society. Eur. Heart J. 2023, 44, 4157–4173. [Google Scholar] [CrossRef] [PubMed]
- Klevmoen, M.; Mulder, J.W.C.M.; Roeters Van Lennep, J.E.; Holven, K.B. Sex Differences in Familial Hypercholesterolemia. Curr. Atheroscler. Rep. 2023, 25, 861–868. [Google Scholar] [CrossRef] [PubMed]
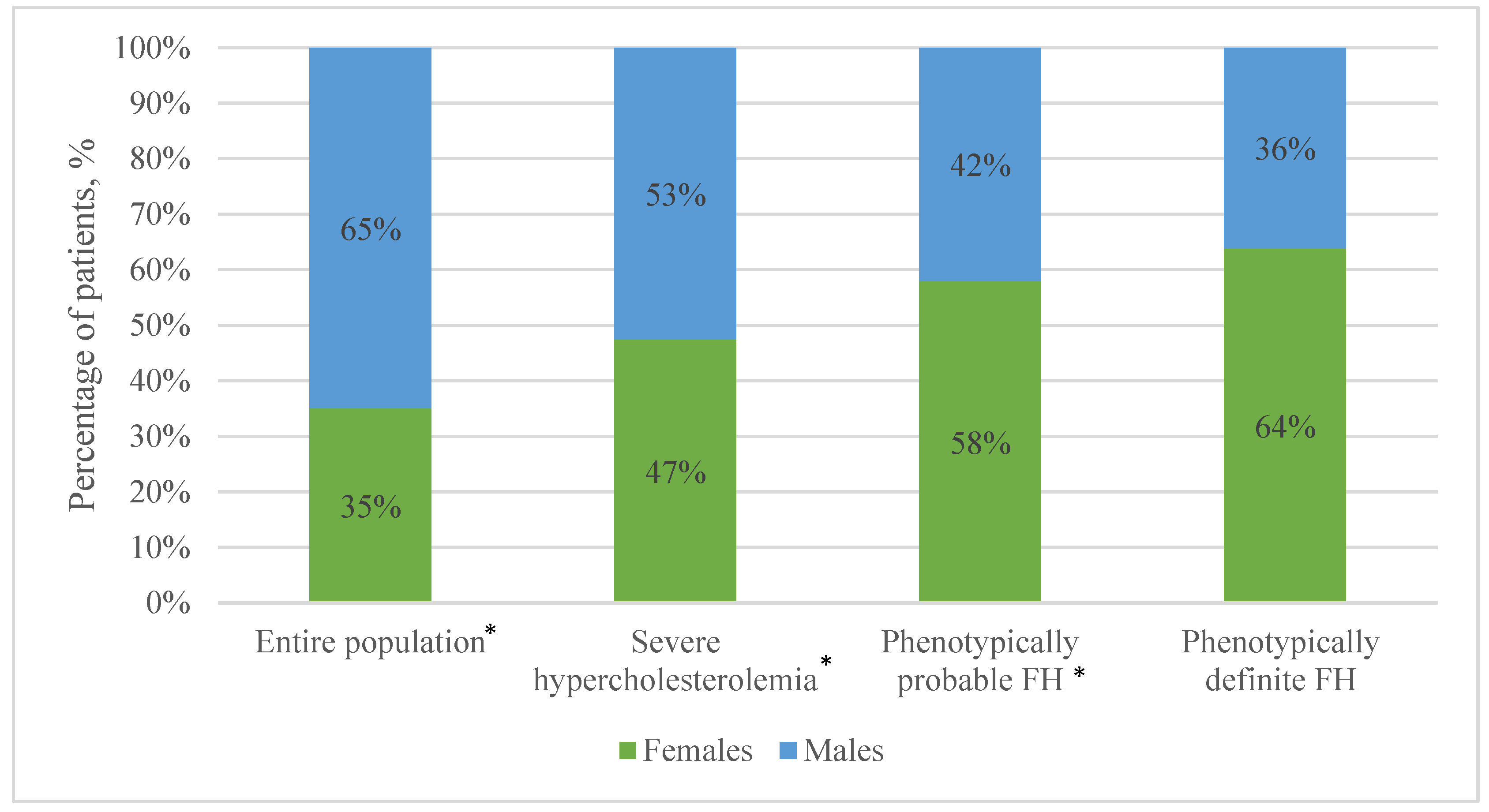
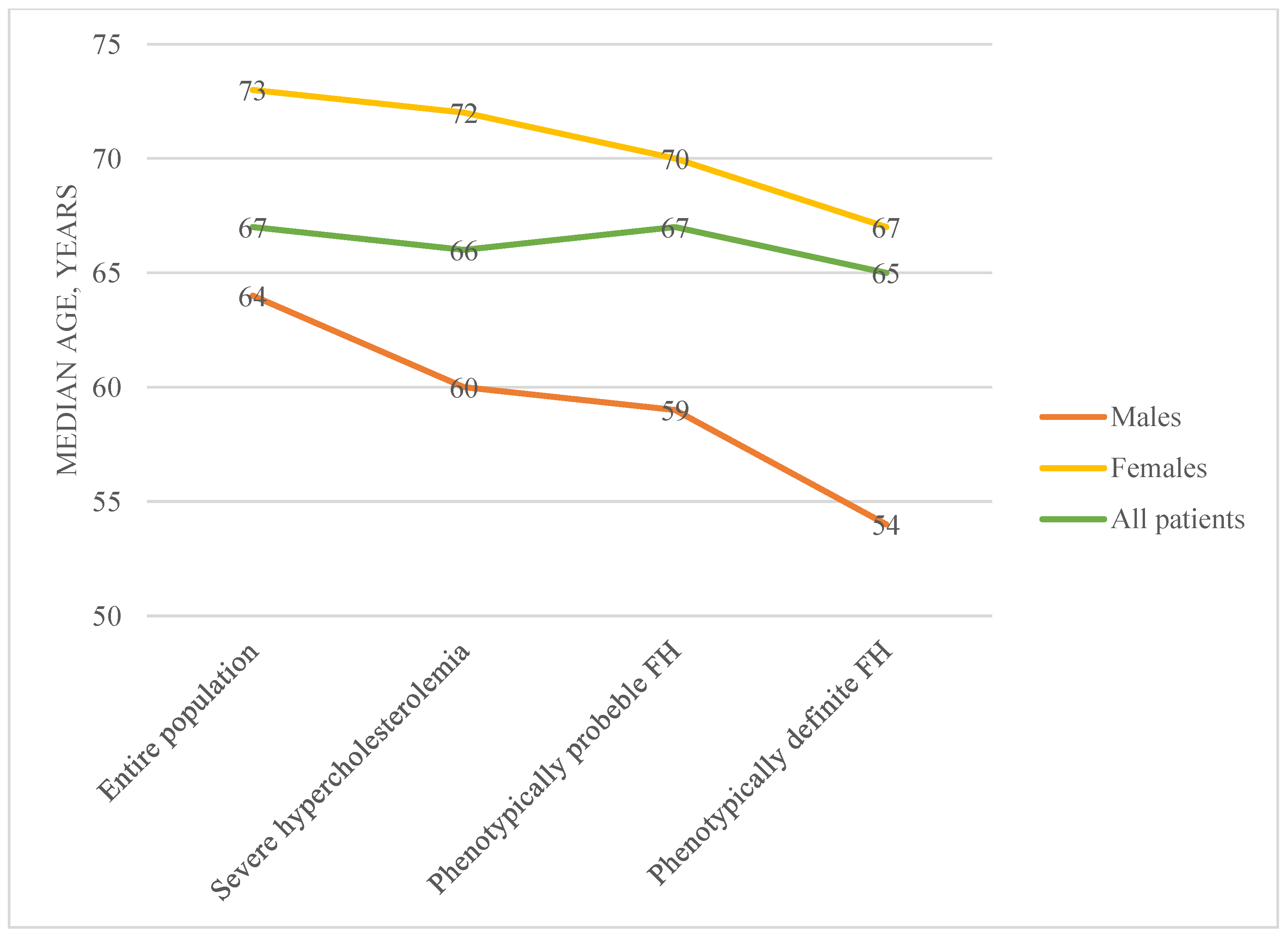
| Study Population | Males | Females | p Value | |
|---|---|---|---|---|
| Total (N) | 34,669 | 22,554 (65.1%) | 12,115 (34.9%) | <0.001 † |
| LDL-C ≥ 4.9 mmol/L (N, %) | 3434 (9.9%) | 1805 (8.0%) | 1629 (13.4%) | <0.001 * |
| LDL-C ≥ 6.5 mmol/L (N, %) | 371 (1.1%) | 157 (0.7%) | 214 (1.8%) | <0.001 * |
| LDL-C ≥ 8.5 mmol/L (N, %) | 36 (0.1%) | 13 (0.1%) | 23 (0.2%) | <0.001 * |
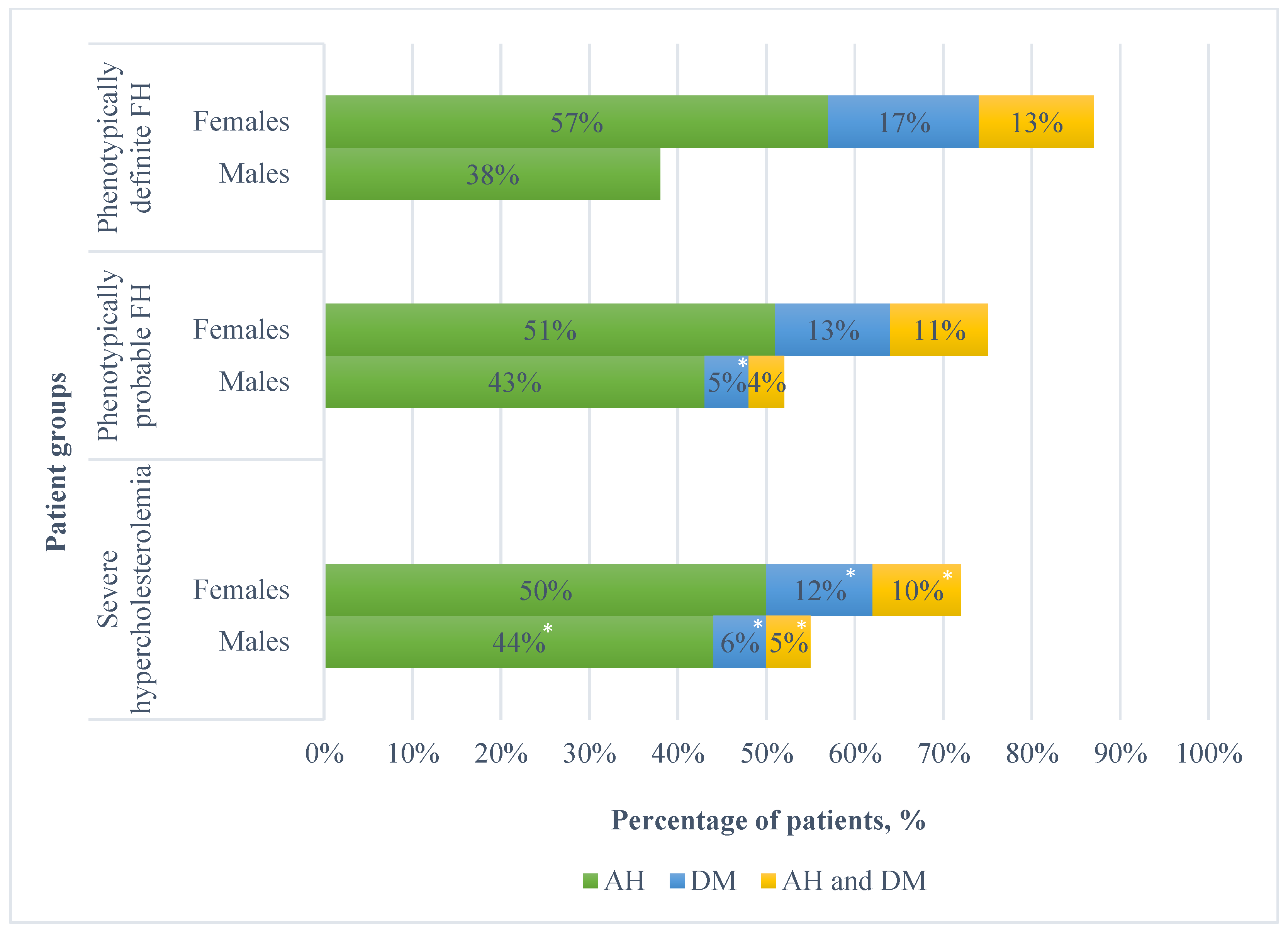
| DM (N, %) | 4081 (11.8%) | 2244 (9.9%) | 1837 (15.2%) | <0.001 * |
| AH (N, %) | 16,627 (48.0%) | 10,458 (46.4%) | 6169 (50.9%) | <0.001 * |
| DM and AH (N, %) | 3229 (9.3%) | 1743 (7.7%) | 1486 (12.3%) | <0.001 * |
| Median age (years) | 67 | 64 | 73 | <0.001 * |
| Median LDL-C (mmol/L/) | 3.4 | 3.3 | 3.5 | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aliošaitienė, U.; Laucevičius, A.; Smailytė, U.; Rinkūnienė, E.; Puronaitė, R.; Barysienė, J.; Petrulionienė, Ž. Prevalence of Severe Hypercholesterolemia and Familial Hypercholesterolemia Phenotype in Patients with Acute Coronary Syndrome. Medicina 2025, 61, 681. https://doi.org/10.3390/medicina61040681
Aliošaitienė U, Laucevičius A, Smailytė U, Rinkūnienė E, Puronaitė R, Barysienė J, Petrulionienė Ž. Prevalence of Severe Hypercholesterolemia and Familial Hypercholesterolemia Phenotype in Patients with Acute Coronary Syndrome. Medicina. 2025; 61(4):681. https://doi.org/10.3390/medicina61040681
Chicago/Turabian StyleAliošaitienė, Urtė, Aleksandras Laucevičius, Urtė Smailytė, Egidija Rinkūnienė, Roma Puronaitė, Jūratė Barysienė, and Žaneta Petrulionienė. 2025. "Prevalence of Severe Hypercholesterolemia and Familial Hypercholesterolemia Phenotype in Patients with Acute Coronary Syndrome" Medicina 61, no. 4: 681. https://doi.org/10.3390/medicina61040681
APA StyleAliošaitienė, U., Laucevičius, A., Smailytė, U., Rinkūnienė, E., Puronaitė, R., Barysienė, J., & Petrulionienė, Ž. (2025). Prevalence of Severe Hypercholesterolemia and Familial Hypercholesterolemia Phenotype in Patients with Acute Coronary Syndrome. Medicina, 61(4), 681. https://doi.org/10.3390/medicina61040681






