Influence of Prosthetic Emergence Profile on Peri-Implant Marginal Bone Stability: A Comprehensive Review
Abstract
1. Introduction
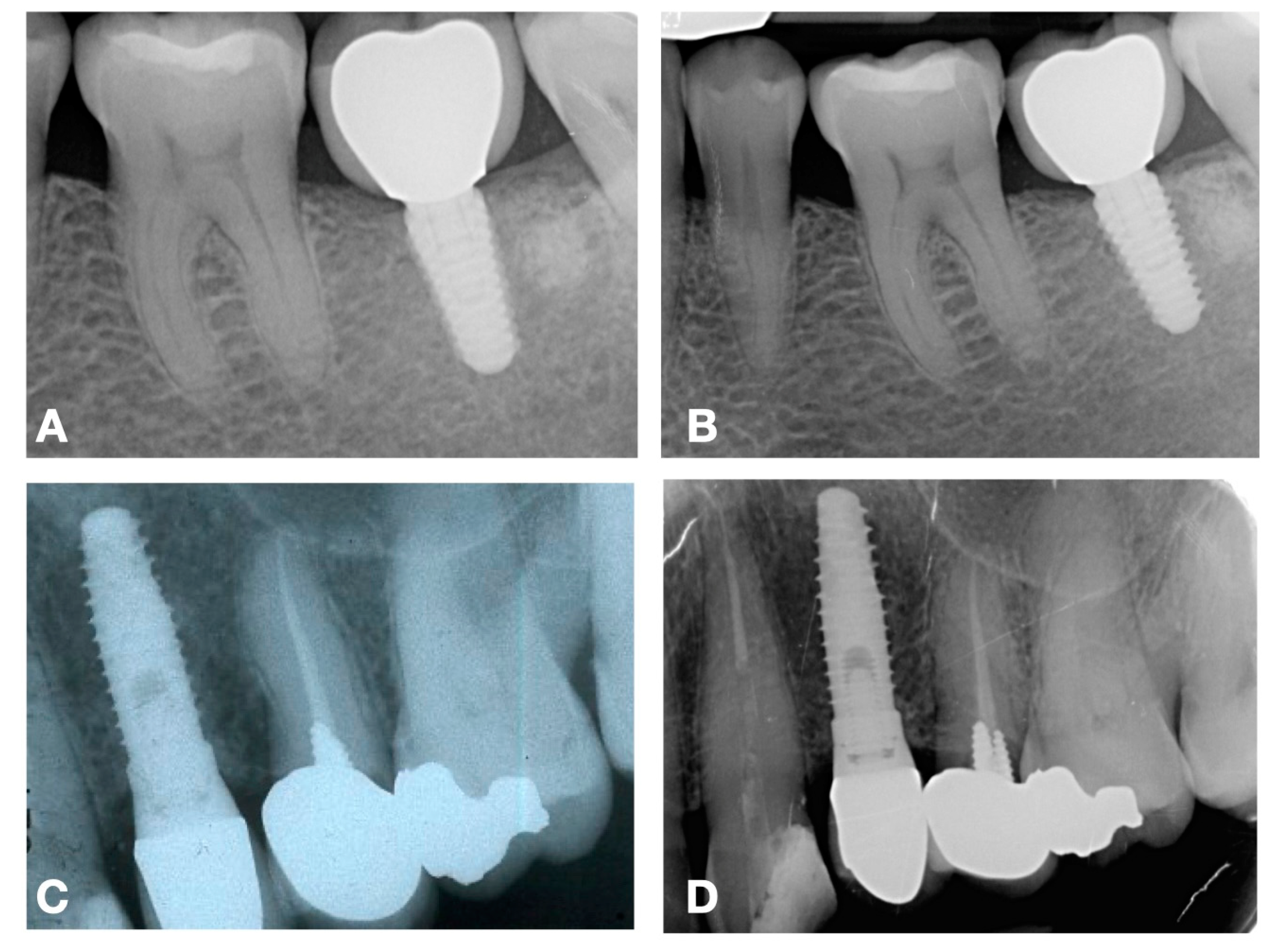
2. Features of Different Prosthetic Emergence Profiles
3. Assessing Marginal Bone Level
4. Implications in Patient Treatments Outcomes
5. Implications for Clinicians
6. Evidence from the Literature
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fu, J.H.; Lee, A.; Wang, H.L. Influence of tissue biotype on implant esthetics. Int. J. Oral Maxillofac. Implant. 2011, 26, 499–508. [Google Scholar]
- Insua, A.; Monje, A.; Wang, H.; Miron, R.J. Basis of bone metabolism around dental implants during osseointegration and peri-implant bone loss. J. Biomed. Mater. Res. A 2017, 105, 2075–2089. [Google Scholar] [CrossRef]
- Bambini, F.; Pellecchia, M.; Memè, L.; Santarelli, A.; Emanuelli, M.; Procaccini, M.; Muzio, L.L. Anti-Inflammatory Cytokines in Peri-Implant Soft Tissues: A Preliminary Study on Humans Using CDNA Microarray Technology. Eur. J. Inflamm. 2007, 5, 121–127. [Google Scholar] [CrossRef]
- Linkevicius, T.; Puisys, A.; Steigmann, M.; Vindasiute, E.; Linkeviciene, L. Influence of Vertical Soft Tissue Thickness on Crestal Bone Changes Around Implants with Platform Switching: A Comparative Clinical Study. Clin. Implant. Dent. Relat. Res. 2015, 17, 1228–1236. [Google Scholar] [CrossRef]
- Linkevicius, T.; Apse, P.; Grybauskas, S.; Puisys, A. Influence of Thin Mucosal Tissues on Crestal Bone Stability Around Implants With Platform Switching: A 1-year Pilot Study. J. Oral Maxillofac. Surg. 2010, 68, 2272–2277. [Google Scholar] [CrossRef]
- Monje, A.; Suarez, F.; Galindo-Moreno, P.; García-Nogales, A.; Fu, J.; Wang, H. A systematic review on marginal bone loss around short dental implants (<10 mm) for implant-supported fixed prostheses. Clin. Oral Implant. Res. 2014, 25, 1119–1124. [Google Scholar] [CrossRef]
- Berglundh, T.; Lindhe, J. Dimension of the periimplant mucosa. J. Clin. Periodontol. 1996, 23, 971–973. [Google Scholar] [CrossRef]
- Patzelt, S.B.M.; Spies, B.C.; Kohal, R.J. CAD/CAM-fabricated implant-supported restorations: A systematic review. Clin. Oral Implant. Res. 2015, 26, 77–85. [Google Scholar] [CrossRef]
- dos Reis, I.N.R.; Chamma-Wedemann, C.N.; de Oliveira Silva, I.A.; Spin-Neto, R.; Sesma, N.; da Silva, E.V.F. Clinical outcomes of digital scans versus conventional impressions for implant-supported fixed complete arch prostheses: A systematic review and meta-analysis. J. Prosthet. Dent. 2023, in press. [Google Scholar] [CrossRef]
- Nassani, L.M.; Bencharit, S.; Schumacher, F.; Lu, W.E.; Resende, R.; Fernandes, G.V.O. The Impact of Technology Teaching in the Dental Predoctoral Curriculum on Students’ Perception of Digital Dentistry. Dent. J. 2024, 12, 75. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, I.; Berglundh, T.; Lindhe, J. The mucosal barrier following abutment dis/reconnection. J. Clin. Periodontol. 1997, 24, 568–572. [Google Scholar] [CrossRef]
- Cinquini, C.; Parisi, E.; Baldi, N.; Miccoli, M.; Alfonsi, F.; Barone, A. Esthetic Outcomes of Immediately Placed Implants with Convergent Transmucosal Profile: A Retrospective Single-Cohort Study. Int. J. Oral Maxillofac. Implant. 2024, 1–20. [Google Scholar] [CrossRef]
- Siegenthaler, M.; Strauss, F.J.; Gamper, F.; Hämmerle, C.H.F.; Jung, R.E.; Thoma, D.S. Anterior implant restorations with a convex emergence profile increase the frequency of recession: 12-month results of a randomized controlled clinical trial. J. Clin. Periodontol. 2022, 49, 1145–1157. [Google Scholar] [CrossRef]
- Linkevicius, T.; Apse, P. Influence of abutment material on stability of peri-implant tissues: A systematic review. Int. J. Oral Maxillofac. Implant. 2018, 23, 449–456. [Google Scholar]
- Finne, K.; Rompen, E.; Toljanic, J. Prospective multicenter study of marginal bone level and soft tissue health of a one-piece implant after two years. J. Prosthet. Dent. 2007, 97, S79–S85. [Google Scholar] [CrossRef]
- Mattheos, N.; Janda, M.; Acharya, A.; Pekarski, S.; Larsson, C. Impact of design elements of the implant supracrestal complex (ISC) on the risk of peri-implant mucositis and peri-implantitis: A critical review. Clin. Oral Implant. Res. 2021, 32, 181–202. [Google Scholar] [CrossRef]
- Bambini, F.; Orilisi, G.; Quaranta, A.; Memè, L. Biological Oriented Immediate Loading: A New Mathematical Implant Vertical Insertion Protocol, Five-Year Follow-Up Study. Materials 2021, 14, 387. [Google Scholar] [CrossRef]
- Da Silva, D.M.; Castro, F.; Martins, B.; Fraile, J.F.; Fernandes, J.C.H.; Fernandes, G.V.O. The influence of the gingival phenotype on implant survival rate and clinical parameters: A systematic review. Evid. Based Dent. 2025. [Google Scholar] [CrossRef]
- Cinquini, C.; Marchio, V.; Di Donna, E.; Alfonsi, F.; Derchi, G.; Nisi, M.; Barone, A. Histologic Evaluation of Soft Tissues around Dental Implant Abutments: A Narrative Review. Materials 2022, 15, 3811. [Google Scholar] [CrossRef]
- Furuhashi, A.; Ayukawa, Y.; Atsuta, I.; Rakhmatia, Y.D.; Koyano, K. Soft Tissue Interface with Various Kinds of Implant Abutment Materials. J. Clin. Med. 2021, 10, 2386. [Google Scholar] [CrossRef]
- Fuda, S.; Martins, B.G.d.S.; Castro, F.C.d.; Heboyan, A.; Gehrke, S.A.; Fernandes, J.C.H.; Mello-Moura, A.C.V.; Fernandes, G.V.O. Marginal Bone Level and Clinical Parameter Analysis Comparing External Hexagon and Morse Taper Implants: A Systematic Review and Meta-Analysis. Diagnostics 2023, 13, 1587. [Google Scholar] [CrossRef]
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implant. 1986, 1, 11–25. [Google Scholar]
- Esposito, M.; Hirsch, J.M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants, (II). Etiopathogenesis. Eur. J. Oral Sci. 1998, 106, 721–764. [Google Scholar] [CrossRef]
- Marchio, V.; Derchi, G.; Cinquini, C.; Miceli, M.; Gabriele, M.; Alfonsi, F.; Barone, A. Tissue level implants in healthy versus medically compromised patients: A cohort comparative study. Minerva Stomatol. 2020, 69, 295–301. [Google Scholar] [CrossRef]
- De Bruyn, H.; Vandeweghe, S.; Ruyffelaert, C.; Cosyn, J.; Sennerby, L. Radiographic evaluation of modern oral implants with emphasis on crestal bone level and relevance to peri-implant health. Periodontology 2000 2013, 62, 256–270. [Google Scholar] [CrossRef]
- Campi, M.; Leitão-Almeida, B.; Pereira, M.; Shibli, J.A.; Levin, L.; Fernandes, J.C.H.; Fernandes, G.V.O.; Borges, T. Immediate implant placement in damaged extraction sockets: A systematic review and meta-analysis of randomized controlled trials. Quintessence Int. 2025, 56, 34–45. [Google Scholar] [CrossRef]
- Carmagnola, D.; Araújo, M.; Berglundh, T.; Albrektsson, T.; Lindhe, J. Bone tissue reaction around implants placed in a compromised jaw. J. Clin. Periodontol. 1999, 26, 629–635. [Google Scholar] [CrossRef]
- Ong, C.T.T.; Ivanovski, S.; Needleman, I.G.; Retzepi, M.; Moles, D.R.; Tonetti, M.S.; Donos, N. Systematic review of implant outcomes in treated periodontitis subjects. J. Clin. Periodontol. 2008, 35, 438–462. [Google Scholar] [CrossRef]
- Wu, X.; Shi, J.; Buti, J.; Lai, H.; Tonetti, M.S. Buccal bone thickness and mid-facial soft tissue recession after various surgical approaches for immediate implant placement: A systematic review and network meta-analysis of controlled trials. J. Clin. Periodontol. 2023, 50, 533–546. [Google Scholar] [CrossRef]
- Donati, M.; Ekestubbe, A.; Lindhe, J.; Wennström, J.L. Marginal bone loss at implants with different surface characteristics—A 20-year follow-up of a randomized controlled clinical trial. Clin. Oral Implant. Res. 2018, 29, 480–487. [Google Scholar] [CrossRef]
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant placement post extraction in esthetic single tooth sites: When immediate, when early, when late? Periodontology 2000 2017, 73, 84–102. [Google Scholar] [CrossRef]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H. Peri-implantitis. J. Periodontol. 2018, 89, S267–S290. [Google Scholar] [CrossRef]
- Herrera, D.; Berglundh, T.; Schwarz, F.; Chapple, I.; Jepsen, S.; Sculean, A.; Kebschull, M.; Papapanou, P.N.; Tonetti, M.S.; Sanz, M.; et al. Prevention and treatment of peri-implant diseases—The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2023, 50, 4–76. [Google Scholar] [CrossRef]
- Renvert, S.; Polyzois, I. Risk indicators for peri-implant mucositis: A systematic literature review. J. Clin. Periodontol. 2015, 42, S172–S186. [Google Scholar] [CrossRef]
- Suárez-López del Amo, F.; Lin, G.; Monje, A.; Galindo-Moreno, P.; Wang, H. Influence of Soft Tissue Thickness on Peri-Implant Marginal Bone Loss: A Systematic Review and Meta-Analysis. J. Periodontol. 2016, 87, 690–699. [Google Scholar] [CrossRef]
- Sheridan, R.A.; Decker, A.M.; Plonka, A.B.; Wang, H.L. The Role of Occlusion in Implant Therapy. Implant Dent. 2016, 25, 829–838. [Google Scholar] [CrossRef]
- Ding, Q.; Luo, Q.; Tian, Y.; Zhang, L.; Xie, Q.; Zhou, Y. Occlusal change in posterior implant-supported single crowns and its association with peri-implant bone level: A 5-year prospective study. Clin. Oral Investig. 2022, 26, 4217–4227. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J.A.; Heitz, F.; Lang, N.P. Implant Disease Risk Assessment IDRA–a tool for preventing peri-implant disease. Clin. Oral Implant. Res. 2020, 31, 397–403. [Google Scholar] [CrossRef]
- Yi, Y.; Koo, K.; Schwarz, F.; Ben Amara, H.; Heo, S. Association of prosthetic features and peri-implantitis: A cross-sectional study. J. Clin. Periodontol. 2020, 47, 392–403. [Google Scholar] [CrossRef]
- Inoue, M.; Nakano, T.; Shimomoto, T.; Kabata, D.; Shintani, A.; Yatani, H. Multivariate analysis of the influence of prosthodontic factors on peri-implant bleeding index and marginal bone level in a molar site: A cross-sectional study. Clin. Implant Dent. Relat. Res. 2020, 22, 713–722. [Google Scholar] [CrossRef]
- Caballero, C.; Rodriguez, F.; Cortellari, G.C.; Scarano, A.; Prados-Frutos, J.C.; De Aza, P.N.; Fernandes, G.V.O.; Gehrke, S.A. Mechanical Behavior of Five Different Morse Taper Implants and Abutments with Different Conical Internal Connections and Angles: An In Vitro Experimental Study. J. Funct. Biomater. 2024, 15, 177. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Scarano, A.; Cortellari, G.C.; Fernandes, G.V.O.; Watinaga, S.E.; Bianchini, M.A. Evaluation of Behavior of Castable versus Machined Solid Abutments for Morse Tapper Implant Connection: A Clinical Retrospective Study. Medicina 2023, 59, 1250. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Scarano, A.; Cortellari, G.C.; Fernandes, G.V.O.; Mesquita, A.M.M.; Bianchini, M.A. Marginal Bone Level and Biomechanical Behavior of Titanium-Indexed Abutment Base of Conical Connection Used for Single Ceramic Crowns on Morse-Taper Implant: A Clinical Retrospective Study. J. Funct. Biomater. 2023, 14, 128. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Dedavid, B.A.; de Oliveira Fernandes, G.V. A new design of a multifunctional abutment to morse taper implant connection: Experimental mechanical analysis. J. Mech. Behav. Biomed. Mater. 2021, 116, 104347. [Google Scholar] [CrossRef]
- Lin, I.; Chen, S.; Chang, C.; Chang, J.Z.; Sun, J.; Chang, C. Morphology of Peri-Implant Tissues Around Permanent Prostheses With Various Emergence Angles Following Free Gingival Grafting. J. Prosthodont. 2022, 31, 681–688. [Google Scholar] [CrossRef]
- Montaruli, G.; Dedola, A.; Russo, D.; Zhurakivska, K.; Laino, L.; Mastrangelo, F.; Troiano, G. Prosthesis Emergence Angle Influences Marginal Bone Level for External Connection Implants: A Cross-Sectional Study. Int. J. Periodontics Restor. Dent. 2023, 43, s205–s216. [Google Scholar] [CrossRef]
- Lin, G.; Tran, C.; Brzyska, K.; Kan, J.Y.; Wang, H.L.; Curtis, D.A.; Kao, R.T. The significance of vertical platform discrepancies and splinting on marginal bone levels for adjacent dental implants. Clin. Implant Dent. Relat. Res. 2023, 25, 321–329. [Google Scholar] [CrossRef]
- Albrektsson, T.; Tengvall, P.; Amengual-Peñafiel, L.; Coli, P.; Kotsakis, G.; Cochran, D.L. Implications of considering peri-implant bone loss a disease, a narrative review. Clin. Implant Dent. Relat. Res. 2022, 24, 532–543. [Google Scholar] [CrossRef]
- Katafuchi, M.; Weinstein, B.F.; Leroux, B.G.; Chen, Y.; Daubert, D.M. Restoration contour is a risk indicator for peri-implantitis: A cross-sectional radiographic analysis. J. Clin. Periodontol. 2018, 45, 225–232. [Google Scholar] [CrossRef]
- Hentenaar, D.; De Waal, Y.; Van Winkelhoff, A.; Raghoebar, G.; Meijer, H. Influence of Cervical Crown Contour on Marginal Bone Loss Around Platform-Switched Bone-Level Implants: A 5-Year Cross-Sectional Study. Int. J. Prosthodont. 2020, 33, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Lops, D.; Romeo, E.; Stocchero, M.; Palazzolo, A.; Manfredi, B.; Sbricoli, L. Marginal Bone Maintenance and Different Prosthetic Emergence Angles: A 3-Year Retrospective Study. J. Clin. Med. 2022, 11, 2014. [Google Scholar] [CrossRef]
- Wang, J.; Tang, Y.; Qiu, L.; Yu, H. Influence of buccal emergence profile designs on peri-implant tissues: A randomized controlled trial. Clin. Implant Dent. Relat. Res. 2022, 24, 329–338. [Google Scholar] [CrossRef]
- Kou, Y.; Li, Q.; Tang, Z. Prosthetic emergence angle in different implant sites and their correlation with marginal bone loss: A retrospective study. J. Dent. Sci. 2023, 18, 534–540. [Google Scholar] [CrossRef]
- Cinquini, C.; Izzetti, R.; Porreca, A.; Iezzi, G.; Nisi, M.; Barone, A. Alveolar ridge preservation and its impact on marginal bone level changes around dental implants: A retrospective, cohort comparative study. Clin. Implant Dent. Relat. Res. 2024, 26, 1162–1171. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Izzetti, R.; Cinquini, C.; Nisi, M.; Covelli, M.; Alfonsi, F.; Barone, A. Influence of Prosthetic Emergence Profile on Peri-Implant Marginal Bone Stability: A Comprehensive Review. Medicina 2025, 61, 517. https://doi.org/10.3390/medicina61030517
Izzetti R, Cinquini C, Nisi M, Covelli M, Alfonsi F, Barone A. Influence of Prosthetic Emergence Profile on Peri-Implant Marginal Bone Stability: A Comprehensive Review. Medicina. 2025; 61(3):517. https://doi.org/10.3390/medicina61030517
Chicago/Turabian StyleIzzetti, Rossana, Chiara Cinquini, Marco Nisi, Michele Covelli, Fortunato Alfonsi, and Antonio Barone. 2025. "Influence of Prosthetic Emergence Profile on Peri-Implant Marginal Bone Stability: A Comprehensive Review" Medicina 61, no. 3: 517. https://doi.org/10.3390/medicina61030517
APA StyleIzzetti, R., Cinquini, C., Nisi, M., Covelli, M., Alfonsi, F., & Barone, A. (2025). Influence of Prosthetic Emergence Profile on Peri-Implant Marginal Bone Stability: A Comprehensive Review. Medicina, 61(3), 517. https://doi.org/10.3390/medicina61030517







