Effects of a Postural Hammock in People with Chronic Neck Pain and Chronic Low Back Pain: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
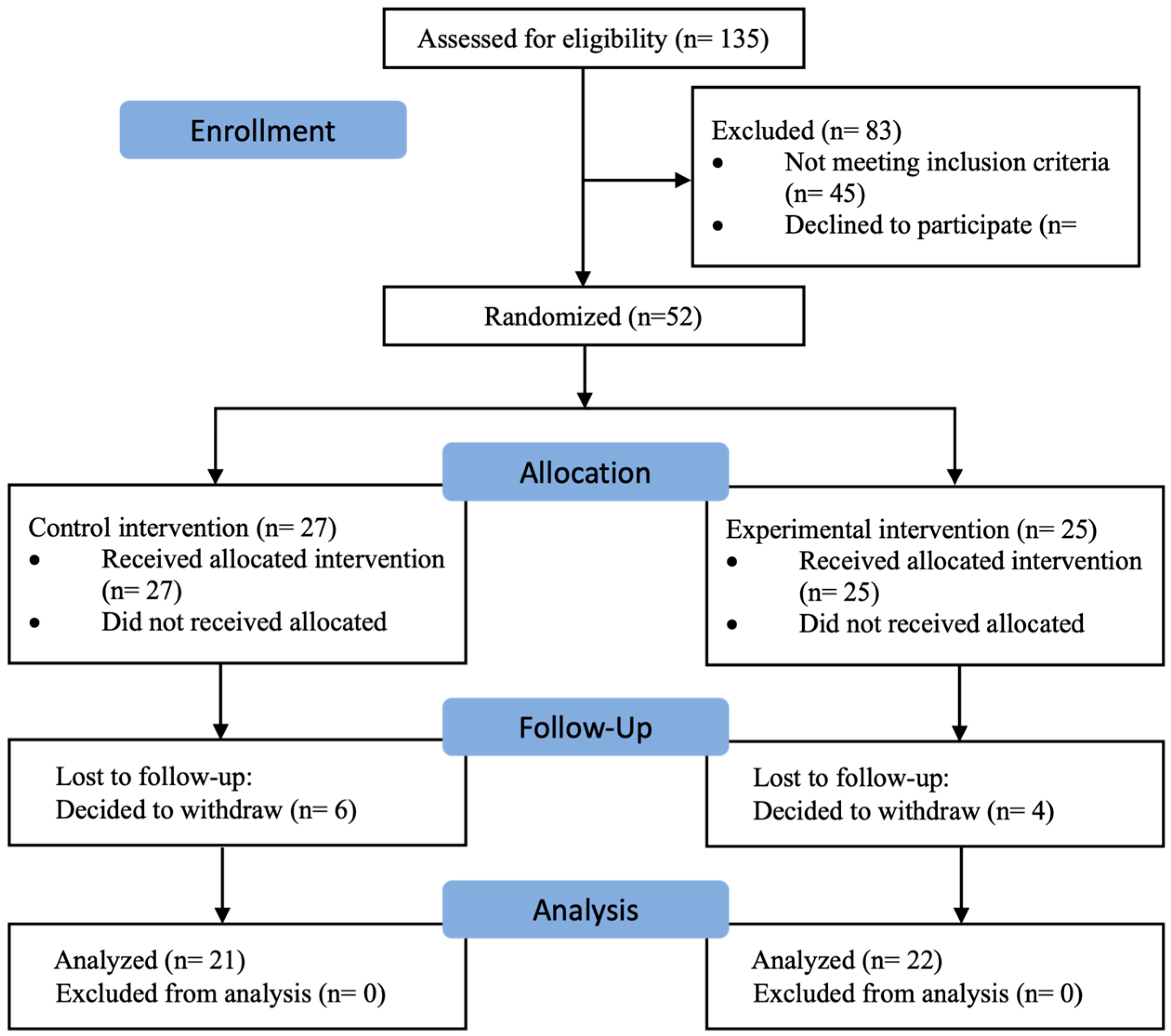
2.1. Study Design
2.2. Participants
2.3. Randomization and Allocation Process
2.4. Intervention
2.5. Variables and Measurement Instruments
2.6. Sample Size Calculation
2.7. Data Analysis
3. Results
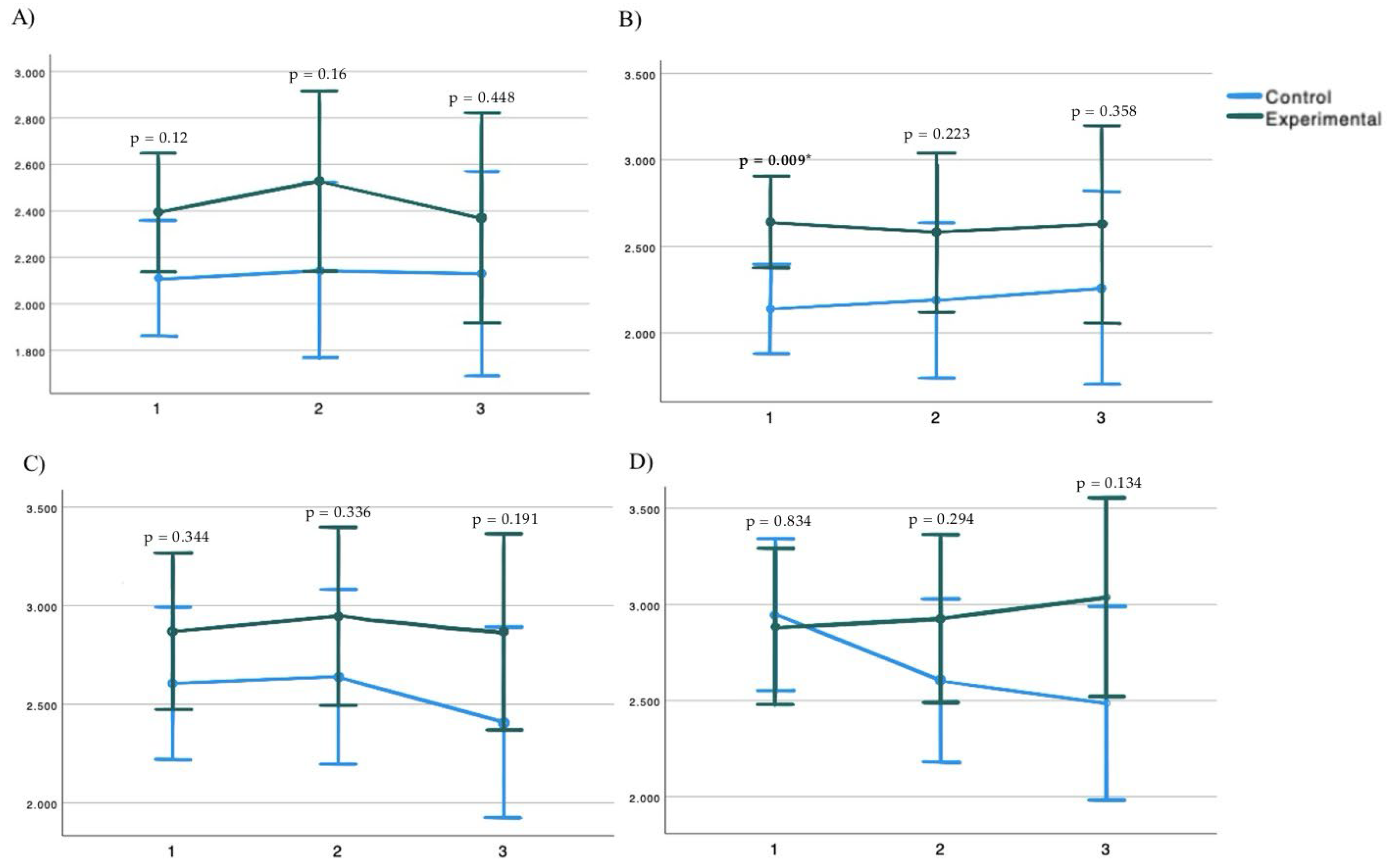
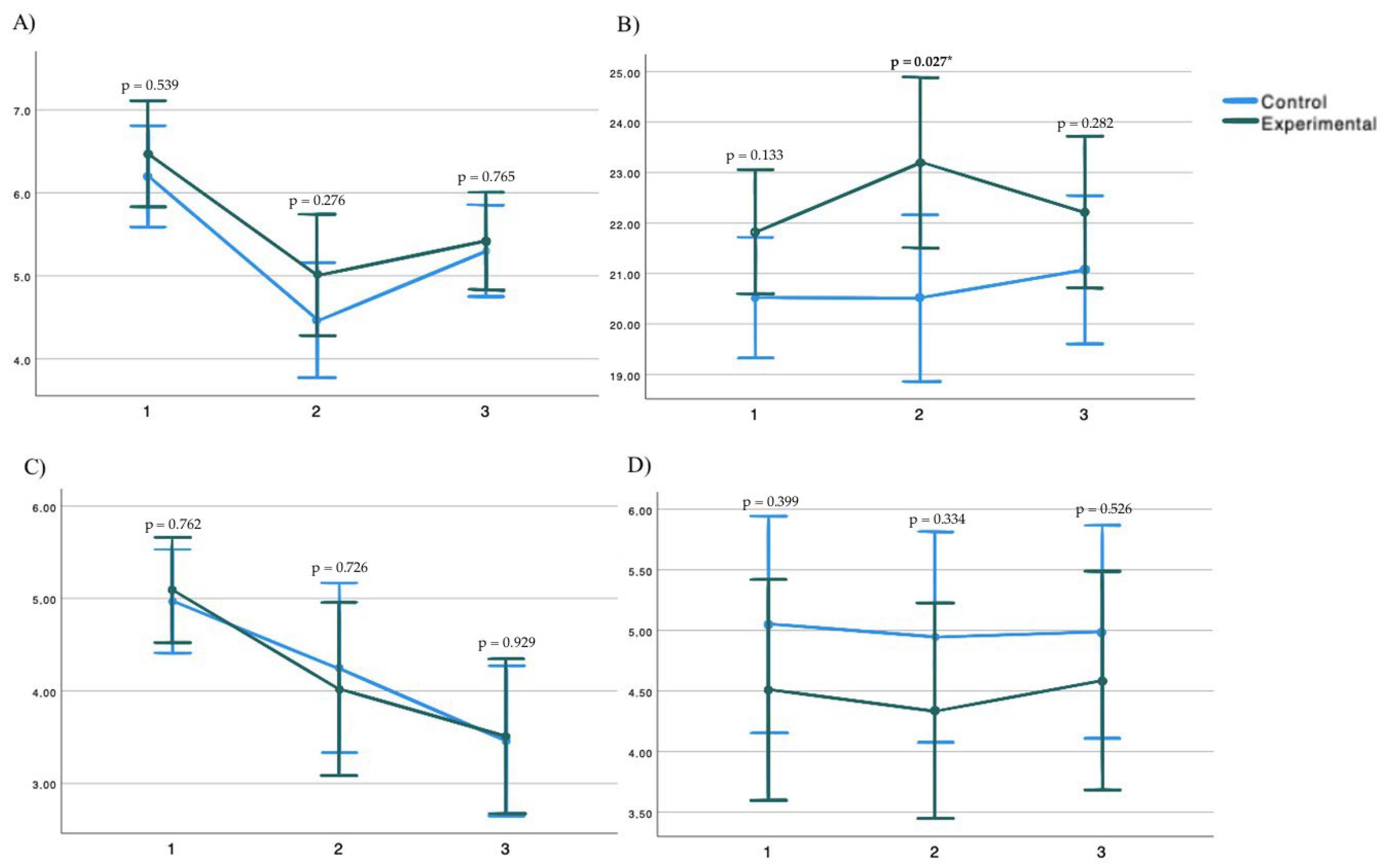
3.1. Group-Time Interaction Analysis
3.2. Within-Subjects’ Analysis
4. Discussion
4.1. Implications for Rehabilitation
4.2. Study Strengths and Limitations
4.3. On the Other Hand, Several Study Limitations Have Been Identified
4.4. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Briggs, A.M.; Woolf, A.D.; Dreinhöfer, K.; Homb, N.; Hoy, D.G.; Kopansky-Giles, D.; March, L. Reducing the Global Burden of Musculoskeletal Conditions. Bull. World Health Organ. 2018, 96, 366. [Google Scholar] [CrossRef] [PubMed]
- Lavin, R.A.; Pappagallo, M.; Kuhlemeier, K.V. Cervical Pain: A Comparison of Three Pillows. Arch. Phys. Med. Rehabil. 1997, 78, 193–198. [Google Scholar] [CrossRef]
- IHME Viz Hub. WHO Rehabilitation Need Estimator. Available online: https://vizhub.healthdata.org/rehabilitation/ (accessed on 15 July 2023).
- Kazeminasab, S.; Nejadghaderi, S.A.; Amiri, P.; Pourfathi, H.; Araj-Khodaei, M.; Sullman, M.J.; Kolahi, A.-A.; Safiri, S. Neck Pain: Global Epidemiology, Trends and Risk Factors. BMC Musculoskelet. Disord. 2022, 23, 26. [Google Scholar] [CrossRef]
- Mazaheri-Tehrani, S.; Arefian, M.; Abhari, A.P.; Riahi, R.; Vahdatpour, B.; Mahdavi, S.B.; Kelishadi, R. Sedentary Behavior and Neck Pain in Adults: A Systematic Review and Meta-Analysis. Prev. Med. 2023, 175, 107711. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.L.; de Luca, K.; Haile, L.M.; Steinmetz, J.D.; Culbreth, G.T.; Cross, M.; Kopec, J.; Ferreira, P.H.; Blyth, F.M.; Buchbinder, R.; et al. Global, Regional, and National Burden of Low Back Pain, 1990–2020, its Attributable Risk Factors, and Projections to 2050: A Systematic Analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e316–e329. [Google Scholar] [CrossRef]
- Nieminen, L.K.; Pyysalo, L.M.; Kankaanpää, M.J. Prognostic Factors for Pain Chronicity in Low Back Pain: A Systematic Review. Pain Rep. 2021, 6, e897. [Google Scholar] [CrossRef]
- Nielens, H.; Van Zundert, J.; Mairiaux, P.; Gailly, J.; Van Den Hecke, N.; Mazina, D.; Camberlin, C.; Bartholomeeusen, S.; De Gauquier, K.; Paulus, D.; et al. Chronic Low Back Pain. Good Clinical Practice (GCP). PM&R. 2006. Available online: https://link.springer.com/article/10.1007/s00586-018-5673-2 (accessed on 15 July 2023).
- Joseph, L.; Vasanthan, L.; Standen, M.; Kuisma, R.; Paungmali, A.; Pirunsan, U.; Sitilertpisan, P. Causal Relationship between the Risk Factors and Work-Related Musculoskeletal Disorders among Professional Drivers: A Systematic Review. Hum. Factors 2023, 65, 62–85. [Google Scholar] [CrossRef]
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Buchbinder, R.; Blyth, F.; Woolf, A.; Vos, T. A Systematic Review of the Global Prevalence of Low Back Pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Hartvigsen, J.; Hancock, M.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Sieper, J.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; et al. What Low Back Pain Is and Why We Need to Pay Attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Melman, A.; Lord, H.J.; Coombs, D.; Zadro, J.; Maher, C.G.; Machado, G.C. Global Prevalence of Hospital Admissions for Low Back Pain: A Systematic Review with Meta-Analysis. BMJ Open 2023, 13, e069517. [Google Scholar] [CrossRef]
- Fatoye, F.; Gebrye, T.; Mbada, C.E.; Useh, U. Clinical and Economic Burden of Low Back Pain in Low- and Middle-Income Countries: A Systematic Review. BMJ Open 2023, 13, e064119. [Google Scholar] [CrossRef] [PubMed]
- Infosalus. Dolor de Espalda, Culpable de la Mitad de las Bajas Laborales. Infosalus. 7 September 2015. Available online: https://www.infosalus.com/salud-investigacion/noticia-dolor-espalda-culpable-mitad-bajas-laborales-20150907112615.html (accessed on 9 February 2025).
- Delitto, A.; George, S.Z.; Van Dillen, L.R.; Whitman, J.M.; Sowa, G.; Godges, J.J.; Shekelle, P.; Denninger, T.R.; Beneciuk, J.M.; Bishop, M.D.; et al. Low Back Pain. J. Orthop. Sports Phys. Ther. 2012, 42, 1–57. [Google Scholar] [CrossRef] [PubMed]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global Estimates of the Need for Rehabilitation Based on the Global Burden of Disease Study 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Corp, N.; Mansell, G.; Stynes, S.; Wynne-Jones, G.; Morsø, L.; Hill, J.C.; van der Windt, D.A. Evidence-Based Treatment Recommendations for Neck and Low Back Pain across Europe: A Systematic Review of Guidelines. Eur. J. Pain 2021, 25, 275–295. [Google Scholar] [CrossRef]
- Zaina, F.; Côté, P.; Cancelliere, C.; Di Felice, F.; Donzelli, S.; Rauch, A.; Verville, L.; Negrini, S.; Nordin, M. A Systematic Review of Clinical Practice Guidelines for Persons with Non-Specific Low Back Pain with and without Radiculopathy: Identification of Best Evidence for Rehabilitation to Develop the WHO’s Package of Interventions for Rehabilitation. Arch. Phys. Med. Rehabil. 2023, 104, 1913–1927. [Google Scholar] [CrossRef]
- Yuan, Q.L.; Guo, T.M.; Liu, L.; Sun, F.; Zhang, Y.G. Traditional Chinese medicine for neck pain and low back pain: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0117146. [Google Scholar] [CrossRef]
- Noori, S.A.; Rasheed, A.; Aiyer, R.; Jung, B.; Bansal, N.; Chang, K.V.; Ottestad, E.; Gulati, A. Therapeutic ultrasound for pain management in chronic low back pain and chronic neck pain: A systematic review. Pain Med. 2020, 21, 1482–1493. [Google Scholar] [CrossRef]
- Cashin, A.G.; Wand, B.M.; O’Connell, N.E.; Lee, H.; Rizzo, R.R.; Bagg, M.K.; O’Hagan, E.; McAuley, J.H. Pharmacological treatments for low back pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2023, 4, CD013815. [Google Scholar] [CrossRef]
- Kazeminia, M.; Rajati, F.; Rajati, M. The Effect of Pelvic Floor Muscle-Strengthening Exercises on Low Back Pain: A Systematic Review and Meta-Analysis on Randomized Clinical Trials. Neurol. Sci. 2023, 44, 859–872. [Google Scholar] [CrossRef]
- Fernández-Rodríguez, R.; Álvarez-Bueno, C.; Cavero-Redondo, I.; Torres-Costoso, A.; Pozuelo-Carrascosa, D.P.; Reina-Gutiérrez, S.; Pascual-Morena, C.; Martínez-Vizcaíno, V. Best Exercise Options for Reducing Pain and Disability in Adults with Chronic Low Back Pain: Pilates, Strength, Core-Based, and Mind-Body. A Network Meta-Analysis. J. Orthop. Sports Phys. Ther. 2022, 52, 505–521. [Google Scholar] [CrossRef]
- Zhu, F.; Zhang, M.; Wang, D.; Hong, Q.; Zeng, C.; Chen, W. Yoga Compared to Non-Exercise or Physical Therapy Exercise on Pain, Disability, and Quality of Life for Patients with Chronic Low Back Pain: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2020, 15, e0238544. [Google Scholar] [CrossRef]
- Paolucci, T.; Attanasi, C.; Cecchini, W.; Marazzi, A.; Capobianco, S.V.; Santilli, V. Chronic low back pain and postural rehabilitation exercise: A literature review. J. Pain Res. 2018, 12, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Grooten, W.J.A.; Boström, C.; Dedering, Å.; Halvorsen, M.; Kuster, R.P.; Nilsson-Wikmar, L.; Olsson, C.B.; Rovner, G.; Tseli, E.; Rasmussen-Barr, E. Summarizing the Effects of Different Exercise Types in Chronic Low Back Pain—A Systematic Review of Systematic Reviews. BMC Musculoskelet. Disord. 2022, 23, 801. [Google Scholar] [CrossRef]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Malmivaara, A.; van Tulder, M.W. Exercise Therapy for Chronic Low Back Pain. Cochrane Database Syst. Rev. 2021, 9, CD009790. [Google Scholar] [CrossRef]
- Owen, P.J.; Miller, C.T.; Mundell, N.L.; Verswijveren, S.J.; Tagliaferri, S.D.; Brisby, H.; Bowe, S.J.; Belavy, D.L. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br. J. Sports Med. 2019, 54, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Petrucci, G.; Papalia, G.F.; Russo, F.; Vadalà, G.; Piredda, M.; De Marinis, M.G.; Papalia, R.; Denaro, V. Psychological Approaches for the Integrative Care of Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 19, 60. [Google Scholar] [CrossRef] [PubMed]
- Quentin, C.; Bagheri, R.; Ugbolue, U.C.; Coudeyre, E.; Pélissier, C.; Descatha, A.; Menini, T.; Bouillon-Minois, J.-B.; Dutheil, F. Effect of Home Exercise Training in Patients with Nonspecific Low-Back Pain: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8430. [Google Scholar] [CrossRef]
- Kim, B.; Yim, J. Core Stability and Hip Exercises Improve Physical Function and Activity in Patients with Non-Specific Low Back Pain: A Randomized Controlled Trial. Tohoku J. Exp. Med. 2020, 251, 193–206. [Google Scholar] [CrossRef]
- Suh, J.H.; Kim, H.; Jung, G.P.; Ko, J.Y.; Ryu, J.S. The Effect of Lumbar Stabilization and Walking Exercises on Chronic Low Back Pain: A Randomized Controlled Trial. Medicine 2019, 98, e16173. [Google Scholar] [CrossRef]
- Castagnoli, C.; Cecchi, F.; Del Canto, A.; Paperini, A.; Boni, R.; Pasquini, G.; Vannetti, F.; Macchi, C. Effects in short and long term of global postural reeducation (GPR) on chronic low back pain: A controlled study with one-year follow-up. Sci World J. 2015, 2015, 271436. [Google Scholar] [CrossRef]
- Moher, D.; Schulz, K.F.; Altman, D.G.; CONSORT Group (Consolidated Standards of Reporting Trials). The CONSORT Statement: Revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001, 285, 1987–1991. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Erueti, C.; Glasziou, P.P. Better reporting of interventions: Template for Intervention Description and Replication (TIDIER) checklist and guide. BMJ 2013, 348, g1687. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction With Life Scale. J. Pers. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Fairbank, J.C.; Couper, J.; Davies, J.B.; O’Brien, J.P. The Oswestry Low Back Pain Disability Questionnaire. Physiotherapy 1980, 66, 271–273. [Google Scholar]
- Walton, D.M.; Macdermid, J.C.; Nielson, W.; Teasell, R.W.; Chiasson, M.; Brown, L. Reliability, Standard Error, and Minimum Detectable Change of Clinical Pressure Pain Threshold Testing in People with and without Acute Neck Pain. J. Orthop. Sports Phys. Ther. 2011, 41, 644–650. [Google Scholar] [CrossRef]
- Chiarotto, A.; Maxwell, L.J.; Ostelo, R.W.; Boers, M.; Tugwell, P.; Terwee, C.B. Measurement Properties of Visual Analogue Scale, Numeric Rating Scale, and Pain Severity Subscale of the Brief Pain Inventory in Patients With Low Back Pain: A Systematic Review. J. Pain 2019, 20, 245–263. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CpGs), short Form-36 bodily pain scale (SF-36 BPs), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar]
- Prushansky, T.; Dvir, Z.; Defrin-Assa, R. Reproducibility indices applied to cervical pressure pain threshold measurements in healthy subjects. Clin. J. Pain 2004, 20, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Hui, S.C.; Yuen, P.Y. Validity of the Modified Back-Saver Sit-and-Reach Test: A Comparison with Other Protocols. Med. Sci. Sports Exerc. 2000, 32, 1655–1659. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.; Silva, A.J.; Oliveira, J. Minimal clinically important difference for the sit-and-reach test in patients with low back pain. Eur. Spine J. 2012, 21, 1763–1768. [Google Scholar]
- Tousignant, M.; Poulin, L.; Marchand, S.; Viau, A.; Place, C. The Modified-Modified Schober Test for Range of Motion Assessment of Lumbar Flexion in Patients with Low Back Pain: A Study of Criterion Validity, Intra- and Inter-Rater Reliability and Minimum Metrically Detectable Change. Disabil. Rehabil. 2005, 27, 553–559. [Google Scholar] [CrossRef]
- Chou, L.W.; Wang, C.H. Minimal clinically important difference of the modified Schober test in patients with low back pain. J. Rehabil. Res. Dev. 2003, 40, 43–48. [Google Scholar]
- Hengeveld, E.; Banks, K. Maitland’s Peripheral Manipulation; Elsevier Health Sciences: New York, NY, USA, 2013. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 29.0.2.0; IBM Corp: Armonk, NY, USA, 2023. [Google Scholar]
- Field, A. Discovering Statistics with IBM SPSS Statistics; Sage: Newbury Park, CA, USA, 2013. [Google Scholar]
- Van Breukelen, G.J.P. ANCOVA versus Change from Baseline: More Power in Randomized Studies, More Bias in Nonrandomized Studies [Corrected]. J. Clin. Epidemiol. 2006, 59, 920–925. [Google Scholar] [CrossRef]
- Sanzarello, I.; Merlini, L.; Rosa, M.A.; Perrone, M.; Frugiuele, J.; Faldini, C.; Borghi, R.; Vaienti, E. Central Sensitization in Chronic Low Back Pain: A Narrative Review. J. Back Musculoskelet. Rehabil. 2016, 29, 625–633. [Google Scholar] [CrossRef]
- Wójcik, M.; Siatkowski, I. The usefulness of performance matrix tests in locomotor system evaluation of girls attending a ballet school—Preliminary observation. J. Phys. Ther. Sci. 2014, 26, 41–44. [Google Scholar] [CrossRef]
- Chen, S.M.; Liu, M.F.; Cook, J.; Bass, S.; Lo, S.K. Sedentary Lifestyle as a Risk Factor for Low Back Pain: A Systematic Review. Int. Arch. Occup. Environ. Health 2009, 82, 797–806. [Google Scholar] [CrossRef]
- Gross, A.; Kay, T.M.; Paquin, J.P.; Blanchette, S.; Lalonde, P.; Santaguida, P.L.; Christie, T.; Dupont, G.; Graham, N.; Burnie, S.J.; et al. Cervical Overview Group. Exercises for Mechanical Neck Disorders. Cochrane Database Syst. Rev. 2015, 2015, CD004250. [Google Scholar] [CrossRef]
- Areerak, K.; Waongenngarm, P.; Janwantanakul, P. Factors Associated with Exercise Adherence to Prevent or Treat Neck and Low Back Pain: A Systematic Review. Musculoskelet. Sci. Pract. 2012, 52, 102333. [Google Scholar] [CrossRef]
- Andini, F. Risk Factors of Low Back Pain in Workers. J. Major. 2015, 4, 1. [Google Scholar]
- Hignett, S. Work-Related Back Pain in Nurses. J. Adv. Nurs. 1996, 23, 1238–1246. [Google Scholar] [CrossRef] [PubMed]
- Janwantanakul, P.; Pensri, P.; Jiamjarasrangsri, V.; Sinsongsook, T. Prevalence of Self-Reported Musculoskeletal Symptoms among Office Workers. Occup. Med. 2008, 58, 436–438. [Google Scholar] [CrossRef]
- Shariat, A.; Tamrin, S.B.M.; Arumugam, M.; Danaee, M.; Ramasamy, R. Prevalence Rate of Musculoskeletal Discomforts Based on Severity Level among Office Workers. Acta Med. Bulg. 2016, 43, 54–63. [Google Scholar] [CrossRef]
- Russo, F.; Papalia, G.F.; Vadalà, G.; Fontana, L.; Iavicoli, S.; Denaro, V.; Papalia, R. The Effects of Workplace Interventions on Low Back Pain in Workers: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 12614. [Google Scholar] [CrossRef]
- Buranruk, O. A Randomized Clinical Trial of Self-Stretching with and without Mindful Breathing-Immediate Effect on Pressure Pain and Range of Motion in Myofascial Pain Syndrome. J. Bodyw. Mov. Ther. 2022, 32, 29–35. [Google Scholar] [CrossRef]
- Pourahmadi, M.; Hesarikia, H.; Keshtkar, A.; Zamani, H.; Bagheri, R.; Shamsoddini, A.; Ghanjal, A. Effectiveness of Slump Stretching on Low Back Pain: A Systematic Review and Meta-Analysis. Pain Med. 2019, 20, 378–396. [Google Scholar] [CrossRef]
- Kuptniratsaikul, V.; Muaksorn, C.; Koedwan, C.; Suesuwan, O.; Srisomnuek, A. Pain Reduction, Physical Performance, and Psychological Status Compared between Hatha Yoga and Stretching Exercise to Treat Sedentary Office Workers with Mild/Moderate Neck/Shoulder Pain: A Randomized Controlled Non-Inferiority Trial. Complement. Ther. Med. 2023, 79, 102996. [Google Scholar] [CrossRef]
- Parry, S.P.; Coenen, P.; Shrestha, N.; O’Sullivan, P.B.; Maher, C.G.; Straker, L.M. Workplace Interventions for Increasing Standing or Walking for Decreasing Musculoskeletal Symptoms in Sedentary Workers. Cochrane Database Syst Rev. 2019, 11, CD012487. [Google Scholar] [CrossRef]
- Coffeng, J.K.; Hendriksen, I.J.; Duijts, S.F.; Twisk, J.W.; van Mechelen, W.; Boot, C.R. Effectiveness of a Combined Social and Physical Environmental Intervention on Presenteeism, Absenteeism, Work Performance, and Work Engagement in Office Employees. J. Occup. Environ. Med. 2014, 56, 258–265. [Google Scholar] [CrossRef]
- Akagi, R.; Takahashi, H. Acute Effect of Static Stretching on Hardness of the Gastrocnemius Muscle. Med. Sci. Sports Exerc. 2013, 45, 1348–1354. [Google Scholar] [CrossRef] [PubMed]
- Umegaki, H.; Ikezoe, T.; Nakamura, M.; Nishishita, S.; Kobayashi, T.; Ichihashi, N.; Fujita, K.; Tanaka, H. Acute Effects of Static Stretching on the Hamstrings Using Shear Elastic Modulus Determined by Ultrasound Shear Wave Elastography: Differences in Flexibility between Hamstring Muscle Components. Man. Ther. 2015, 20, 610–613. [Google Scholar] [CrossRef]
- Matsuo, S.; Suzuki, S.; Iwata, M.; Banno, Y.; Asai, Y.; Inoue, T.; Tsuchida, W. Acute Effects of Different Stretching Durations on Passive Torque, Mobility, and Isometric Muscle Force. J. Strength Cond. Res. 2013, 27, 3367–3376. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Ikezoe, T.; Takeno, Y.; Ichihashi, N. Time Course of Changes in Passive Properties of the Gastrocnemius Muscle–Tendon Unit during 5 min of Static Stretching. Man. Ther. 2013, 18, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Mottram, S.; Comerford, M. A new perspective on risk assessment. Phys. Ther. Sport 2008, 9, 40–51. [Google Scholar] [CrossRef]
- Gobbo, S.; Bullo, V.; Bergamo, M.; Duregon, F.; Vendramin, B.; Alberton, C.L.; Battista, F.; Roma, E.; Bocalini, D.S.; Rica, R.L.; et al. Physical Exercise Is Confirmed to Reduce Low Back Pain Symptoms in Office Workers: A Systematic Review of the Evidence to Improve Best Practices in the Workplace. J. Funct. Morphol. Kinesiol. 2019, 4, 43. [Google Scholar] [CrossRef]
- Sowah, D.; Boyko, R.; Antle, D.; Miller, L.; Zakhary, M.; Straube, S. Occupational Interventions for the Prevention of Back Pain: Overview of Systematic Reviews. J. Saf. Res. 2018, 66, 39–59. [Google Scholar] [CrossRef]
- Skelly, A.C.; Chou, R.; Dettori, J.R.; Turner, J.A.; Friedly, J.L.; Ferguson, A.J.R.; Rundell, S.D.; Fu, R.; Brodt, E.D.; Wasson, N.; et al. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update; Agency for Healthcare Research and Quality (US): Rockville MD, USA, 2020. [Google Scholar]
- Falsiroli Maistrello, L.; Zanconato, L.; Palese, A.; Geri, T.; Turolla, A.; Gianola, S.; Dell’isola, A.; Rossettini, G. Perceptions and experiences of individuals with neck pain: A systematic critical review of qualitative studies with meta-summary and meta-synthesis. Phys Ther. 2022, 102, pzac080. [Google Scholar] [CrossRef]
| Parameter | Control (n = 21) | Experimental (n = 22) | p |
|---|---|---|---|
| Gender | 15 women/6 men | 18 women/4 men | |
| Age | 52.73 (10.57) | 55.81 (9.25) | 0.316 |
| Owestry scale | 16.74 (11.51) | 20.29 (12.45) | 0.357 |
| NDI | 24.95 (13.1) | 21 (15.25) | 0.378 |
| SWLS | 25.7 (6.92) | 19.76 (9.47) | 0.028 * |
| PSS | 26.1 (10.68) | 29.71 (6.44) | 0.191 |
| HADS Anxiety | 8.43 (2.77) | 10.2 (3.03) | 0.058 |
| HADS Depression | 8.76 (2.98) | 9.8 (2.35) | 0.225 |
| SF36 Physical Functioning | 75.79 (18.13) | 74.25 (19.49) | 0.8 |
| SF36 Physical Role | 57.89 (40.01) | 48.75 (45.5) | 0.51 |
| SF36 Emotional Role | 77.19 (38.57) | 76.67 (40.61) | 0.967 |
| SF36 Energy | 50.26 (18.06) | 45.75 (16.80) | 0.424 |
| SF36 Emotional well-being | 64.84 (21.32) | 60.6 (16.22) | 0.487 |
| SF36 Social Functioning | 71.84 (27.05) | 73.13 (20.37) | 0.868 |
| SF36 Pain | 53.03 (24.99) | 44.38 (17.01) | 0.212 |
| SF36 General Health | 51.84 (19.16) | 53.42 (18.56) | 0.798 |
| IPAQ-SF, MET-min/week | 2304.37 (1726.59) | 2094.88 (1403.37) | 0.675 |
| IPAQ-SF, category | |||
| High | 47.4% | 23.8% | 0.241 |
| Moderate | 36.8% | 61.9% | 0.241 |
| Low | 15.8% | 14.3% | 0.241 |
| Control vs. Experimental | |||||
|---|---|---|---|---|---|
| Parameter | Control (n = 21) | Experimental (n = 22) | DM | p | CI 95% |
| Right Trapezius PPT 1S | 2.110 (0.124) | 2.392 (0.127) | −0.281 | 0.12 | −0.639, 0.077 |
| Right Trapezius PPT 5S | 2.144 (0.188) | 2.529 (0.192) | −0.385 | 0.16 | −0.928, 0.159 |
| Right Trapezius PPT FU | 2.13 (0.218) | 2.369 (0.223) | −0.24 | 0.448 | −0.871, 0.392 |
| Left Trapezius PPT 1S | 2.138 (0.128) | 2.641 (0.131) | −0.503 | 0.009 * | −0.874, −0.132 |
| Left Trapezius PPT 5S | 2.187 (0.222) | 2.581 (0.227) | −0.394 | 0.223 | −1.039, 0.25 |
| Left Trapezius PPT FU | 2.26 (0.277) | 2.629 (0.283) | −0.369 | 0.358 | −1.173, 0.434 |
| Right Quadratus Lumborum PPT 1S | 2.607 (0.191) | 2.87 (0.196) | −0.263 | 0.344 | −0.817, 0.292 |
| Right Quadratus Lumborum PPT 5S | 2.639 (0.219) | 2.945 (0.224) | −0.306 | 0.336 | −0.941, 0.329 |
| Right Quadratus Lumborum PPT FU | 2.408 (0.241) | 2.868 (0.247) | −0.46 | 0.191 | −1.158, 0.239 |
| Left Quadratus Lumborum PPT 1S | 2.943 (0.197) | 2.884 (0.201) | 0.059 | 0.834 | −0.511, 0.629 |
| Left Quadratus Lumborum PPT 5S | 2.605 (0.211) | 2.927 (0.216) | −0.322 | 0.294 | −0.934, 0.29 |
| Left Quadratus Lumborum PPT FU | 2.487 (0.251) | 3.038 (0.257) | −0.551 | 0.134 | −1.278, 0.176 |
| Modified Schober test 1S | 6.199 (0.302) | 6.471 (0.316) | −271 | 0.539 | −1.157, 0.614 |
| Modified Schober 5S | 4.46 (0.346) | 5.014 (0.363) | −0.554 | 0.276 | −1.569, 0.461 |
| Modified Schober FU | 5.3 (0.276) | 5.42 (0.289) | −0.12 | 0.765 | −0.93, 0.689 |
| SRT 1S | 20,513 (0.595) | 21.82 (0.609) | −1.307 | 0.133 | −3.03, 0.417 |
| SRT 5S | 20,508 (0.819) | 23,201 (0.838) | −2.693 | 0.027 * | −5.064, −0.322 |
| SRT FU | 21,074 (0.728) | 22,213 (0.745) | −1.138 | 0.282 | −3.246, 0.969 |
| Cervical VAS 1S | 4.969 (0.277) | 5.088 (2.83) | −0.121 | 0.762 | −0.922, 0.681 |
| Cervical VAS 5S | 4.25 (0.455) | 4.019 (0.466) | 0.23 | 0.726 | −1.087, 1.547 |
| Cervical VAS FU | 3.459 (0.402) | 3.51 (0.412) | −0.052 | 0.929 | −1.216, 1.113 |
| Lumbar VAS 1S | 5.045 (0.442) | 4.504 (0.452) | 0.541 | 0.399 | −0.742, 1.823 |
| Lumbar VAS 5S | 4.942 (0.432) | 4.336 (0.442) | 0.606 | 0.334 | −0.648, 1.861 |
| Lumbar VAS FU | 4.984 (0.437) | 4.583 (0.447) | 0.401 | 0.526 | −0.866, 1.668 |
| Pre vs. 1S | Pre vs. 5S | Pre vs. FU | 5S vs. FU | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DM | p | CI 95% | DM | p | CI 95% | DM | p | CI 95% | DM | p | CI 95% | |
| Right Trapezius PPT control | 0.102 | 1 | −0.247, 0.452 | 0.067 | 1 | −0.457, 0.592 | 0.075 | 1 | −0.561, 0.711 | 0.007 | 1 | −0.536 |
| Right Trapezius PPT Ex | −0.168 | 1 | −0.525, 0.19 | −0.304 | 0.747 | −0.841, 0.233 | −0.137 | 1 | −0.788, 0.515 | 0.167 | 1 | −0.341 |
| Left Trapezius PPT control | 0.176 | 1 | −0.174, 0.526 | 0.142 | 1 | −0.474, 0.759 | 0.065 | 1 | −0.696, 0.827 | −0.077 | 1 | −0.556, 0.403 |
| Left Trapezius PPT Ex | −0.337 | 0.76 | −0.695, 0.022 | −0.293 | 1 | −0.924, 0.338 | −0.336 | 1 | −1.115, 0.443 | −0.043 | 1 | −0.534, 0.448 |
| Right Quadratus Lumborum control | 0.102 | 1 | −0.425, 0.629 | 0.096 | 1 | −0.551, 0.742 | 0.32 | 1 | −0.368, 1.008 | 0.224 | 1 | −0.402, 0.851 |
| Right Quadratus Lumborum Ex | −0.18 | 1 | −0.719, 0.36 | −0.281 | 1 | −0.943, 0.38 | −0.197 | 1 | −0.902, 0.507 | 0.084 | 1 | −0.557, 0.725 |
| Left Quadratus Lumborum control | −0.031 | 1 | −0.581, 0.52 | 0.341 | 1 | −0.347, 1.030 | 0.458 | 0.655 | −0.317, 1.233 | 0.116 | 1 | −0.459, 0.692 |
| Left Quadratus Lumborum Ex | −0.003 | 1 | −0.567, 0.561 | −0.081 | 1 | −0.785, 0.624 | −0.19 | 1 | −0.983, 0.604 | −0.109 | 1 | −0.698, 0.48 |
| Modified Schober test control | −0.468 | 0.829 | −1.327, 0.391 | 1.391 | 1 | −0.155, 2.937 | 0.523 | 1 | −0.721, 1.767 | −0.868 | 0.092 | −1.819, 0.083 |
| Modified Schober test Ex | −0.8 | 0.109 | −1.701, 0.101 | 0.525 | 1 | −1.155, 2.146 | 0.15 | 1 | −1.155, 1.455 | −0.375 | 1 | −1.372, 0.622 |
| SRT control | −1.053 | 0.692 | −2.867, 0.761 | −1.08 | 1 | −3.561, 1.402 | −1.645 | 0.301 | −3.905, 0.614 | −0.566 | 1 | −1.903, 0.771 |
| SRT Ex | −2.167 | 0.014 * | −4.024, −0.31 | −3.514 | 0.003 * | −6.055, −0.974 | −2.526 | 0.025 * | −4.839, −0.213 | 0.988 | 0.312 | −0.38, 2.356 |
| DM | p | CI 95% | DM | P | CI 95% | |||||||
| Cervical VAS control | 0.064 | 1 | −0.816, 943 | 0.834 | 0.868 | −0.721, 2.389 | 1.631 | 0.023 * | 0.154, 3.108 | 0.797 | 0.146 | −0.148, 1.742 |
| Cervical VAS Ex | −0.156 | 1 | −1.056, 0.943 | 0.858 | 0.858 | −0.734, 2.389 | 1.361 | 0.1 | −0.151, 3.108 | 0.503 | 0.941 | −0.464, 1.742 |
| DM | p | CI 95% | DM | p | CI 95% | |||||||
| Lumbar VAS control | −0.477 | 1 | −1.751, 0.917 | −0.403 | 1 | −1.983, 1.176 | −0.419 | 1 | −1.916, 1.078 | −0.015 | 1 | −1.209, 1.179 |
| Lumbar VAS Ex | 0.34 | 1 | −1.025, 1.706 | 0.603 | 1 | −1.014, 2.220 | 0.327 | 1 | −1.205, 1.859 | −0.276 | 1 | −1.498, 0.946 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delfa-De-La-Morena, J.M.; Mijarra-Murillo, J.-J.; Navarro-López, V.; Fernández-Vázquez, D. Effects of a Postural Hammock in People with Chronic Neck Pain and Chronic Low Back Pain: A Randomized Controlled Trial. Medicina 2025, 61, 502. https://doi.org/10.3390/medicina61030502
Delfa-De-La-Morena JM, Mijarra-Murillo J-J, Navarro-López V, Fernández-Vázquez D. Effects of a Postural Hammock in People with Chronic Neck Pain and Chronic Low Back Pain: A Randomized Controlled Trial. Medicina. 2025; 61(3):502. https://doi.org/10.3390/medicina61030502
Chicago/Turabian StyleDelfa-De-La-Morena, José Manuel, Juan-José Mijarra-Murillo, Víctor Navarro-López, and Diego Fernández-Vázquez. 2025. "Effects of a Postural Hammock in People with Chronic Neck Pain and Chronic Low Back Pain: A Randomized Controlled Trial" Medicina 61, no. 3: 502. https://doi.org/10.3390/medicina61030502
APA StyleDelfa-De-La-Morena, J. M., Mijarra-Murillo, J.-J., Navarro-López, V., & Fernández-Vázquez, D. (2025). Effects of a Postural Hammock in People with Chronic Neck Pain and Chronic Low Back Pain: A Randomized Controlled Trial. Medicina, 61(3), 502. https://doi.org/10.3390/medicina61030502






