Total Thyroidectomy with Harmonic Scalpel Combined with Gelatin Thrombin Hemostatic: A Focus on the Elderly Population—A Multicentric Study
Abstract
1. Introduction
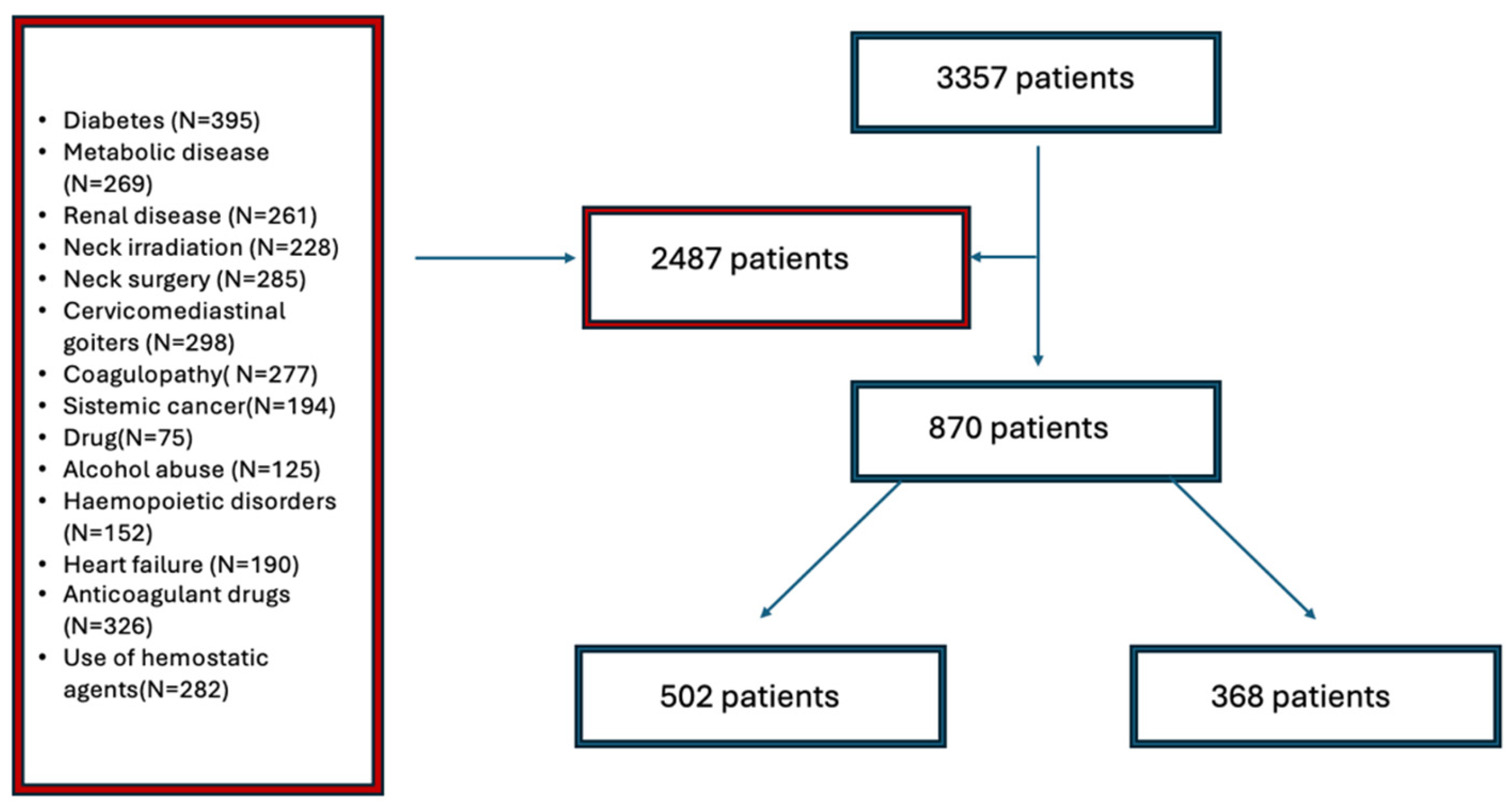
2. Materials and Methods
2.1. Study Design
2.2. Study Setting and Study Population
2.3. Surgical Techniques
- -
- Dissection and ligation of vascular pedicles were performed using the HS;
- -
- Gelatin–thrombin was applied after the thyroidectomy, particularly in the Gruber and Sappey ligaments, with the aim of avoiding electrocautery injuries to recurrent nerves.
- -
- Dissection and ligation of vascular pedicles were performed using ligatures, sutures, and electrocautery;
- -
- Bleeding not responsive to surgical hemostasis, particularly in the Gruber and Sappey ligaments, was treated solely with electrocautery or ligation. Patients who were enrolled in the control group (A), who were not treated with hemostatic agents, but who received them following the development of complications, were also excluded from the study.
2.4. Outcomes Measure
- -
- A cervical ultrasound, performed using a 7–13 Hz linear probe (Esaote, MyLab™ X5, Genova, Italy) at 48 h and 7 days after surgery to detect potential hematoma or seroma. Sonographers reported the transversal, longitudinal, and cranio-caudal diameters in millimeters in case of detection.
- -
- In the event of dysphonic voice incidence, laryngoscopy was performed before the discharge.
- -
- Clinical examinations after 3 months by an experienced endocrine surgeon.
2.5. Study Endpoints
2.6. Statistical Analysis
3. Results
3.1. Study Population
3.2. Primary Outcomes
3.3. HS (Harmonic Scalpel), TT (Total Thyroidectomy), and mL (Milliliters)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smith, R.B.; Coughlin, A. Thyroidectomy Hemostasis. Otolaryngol. Clin. N. Am. 2016, 49, 727–748. [Google Scholar] [CrossRef] [PubMed]
- Branca, J.J.V.; Lascialfari Bruschi, A.; Pilia, A.M.; Carrino, D.; Guarnieri, G.; Gulisano, M.; Pacini, A.; Paternostro, F. The Thyroid Gland: A Revision Study on Its Vascularization and Surgical Implications. Medicina 2022, 58, 137. [Google Scholar] [CrossRef] [PubMed]
- Garas, G.; Okabayashi, K.; Ashrafian, H.; Shetty, K.; Palazzo, F.; Tolley, N.; Darzi, A.; Athanasiou, T.; Zacharakis, E. Which hemostatic device in thyroid surgery? A network meta-analysis of surgical technologies. Thyroid 2013, 23, 1138–1150. [Google Scholar] [CrossRef]
- Materazzi, G.; Caravaglios, G.; Matteucci, V.; Aghababyan, A.; Miccoli, M.; Miccoli, P. The impact of the Harmonic FOCUS™ on complications in thyroid surgery: A prospective multicenter study. Updates Surg. 2013, 65, 295–299. [Google Scholar] [CrossRef]
- Docimo, G.; Filograna Pignatelli, M.; Ferrandes, S.; Monaco, A.; Calisti, F.; Ruggiero, R.; Tolone, S.; Lucido, F.S.; Brusciano, L.; Parisi, S.; et al. Role of Absorbable Polysaccharide Hemostatic Powder in the Prevention of Bleeding and Wound Events after Thyroid Surgery. J. Clin. Med. 2023, 12, 5684. [Google Scholar] [CrossRef]
- Testini, M.; Marzaioli, R.; Lissidini, G.; Lippolis, A.; Logoluso, F.; Gurrado, A.; Lardo, D.; Poli, E.; Piccinni, G. The effectiveness of FloSeal matrix hemostatic agent in thyroid surgery: A prospective, randomized, control study. Langenbecks Arch. Surg. 2009, 394, 837–842. [Google Scholar] [CrossRef]
- Shaha, A.R. Thyroidectomy in the Eldery. Eur. J. Surg. Oncol. 2019, 45, 299–300. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Sorensen, J.R.; Watt, T.; Cramon, P.; Døssing, H.; Hegedüs, L.; Bonnema, S.J.; Godballe, C. Quality of life after thyroidectomy in patients with nontoxic nodular goiter: A prospective cohort study. Head Neck 2017, 39, 2232–2240. [Google Scholar] [CrossRef]
- Ruggiero, R.; Pirozzi, R.; Gualtieri, G.; Terracciano, G.; Parisi, S.; Nesta, G.; Gazeneo, L.; Lanza Volpe, M.; Rinaldi, S.; Docimo, L. Overview on surgical management of papillary thyroid microcarcinoma. G. Chir. 2019, 40, 81–87. [Google Scholar]
- Sugitani, I.; Nagaoka, R.; Saitou, M.; Sen, M.; Kazusaka, H.; Matsui, M.; Abe, T.; Ito, R.; Toda, K. Long-term outcomes of active surveillance for low-risk papillary thyroid carcinoma: Progression patterns and tumor calcification. World J. Surg. 2025, 49, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Joseph, K.R.; Edirimanne, S.; Eslick, G.D. Thyroidectomy for thyroid cancer in the elderly: A meta-analysis. Eur. J. Surg. Oncol. 2019, 45, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Wojtczak, B.; Aporowicz, M.; Kaliszewski, K.; Bolanowski, M. Consequences of bleeding after thyroid surgery—analysis of 7805 operations performed in a single center. Arch. Med. Sci. 2018, 14, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Promberger, R.; Ott, J.; Kober, F.; Koppitsch, C.; Seemann, R.; Freissmuth, M.; Hermann, M. Risk factors for postoperative bleeding after thyroid surgery. Br. J. Surg. 2012, 99, 373–379. [Google Scholar] [CrossRef]
- Finnerty, B.M.; Gray, K.D.; Ullmann, T.M.; Zarnegar, R.; Fahey, T.J., 3rd; Beninato, T. Frailty is More Predictive than Age for Complications After Thyroidectomy for Multinodular Goiter. World J. Surg. 2020, 44, 1876–1884. [Google Scholar] [CrossRef]
- Fassas, S.; Mamidi, I.; Lee, R.; Pasick, L.; Benito, D.A.; Thakkar, P.; Joshi, A.S.; Goodman, J.F. Postoperative Complications After Thyroidectomy: Time Course and Incidence Before Discharge. J. Surg. Res. 2021, 260, 210–219. [Google Scholar] [CrossRef]
- Ruggiero, R.; Docimo, L.; Tolone, S.; De Palma, M.; Musella, M.; Pezzolla, A.; Gubitosi, A.; Parmeggiani, D.; Pirozzi, R.; Gili, S.; et al. Effectiveness of an advanced hemostatic pad combined with harmonic scalpel in thyroid surgery: A prospective study. Int. J. Surg. 2016, 28, 17–21. [Google Scholar] [CrossRef]
- Revelli, L.; Damiani, G.; Bianchi, C.B.; Vanella, S.; Ricciardi, W.; Raffaelli, M.; Lombardi, C.P. Complications in thyroid surgery. Harmonic Scalpel, Harmonic Focus versus Conventional Hemostasis: A meta-analysis. Int. J. Surg. 2016, 28 (Suppl. S1), S22–S32. [Google Scholar] [CrossRef]
- Tolone, S.; Bondanese, M.; Ruggiero, R.; Gili, S.; Pirozzi, R.; Parisi, S.; Buonomo, N.; Napolitano, V.; Docimo, L.; Docimo, G. Outcomes of sutureless total thyroidectomy in elderly. Int. J. Surg. 2016, 33 (Suppl. S1), S16–S19. [Google Scholar] [CrossRef]
- Sajid, M.S.; Hutson, K.H.; Rapisarda, I.F.; Bonomi, R. Fibrin glue instillation under skin flaps to prevent seroma-related morbidity following breast and axillary surgery. Cochrane Database Syst. Rev. 2013, 5, CD009557. [Google Scholar]
- Pelizzo, M.R.; Sorgato, N.; Isabella Merante Boschin, I.; Marzola, M.C.; Colletti, P.M.; Rubello, D. Does the ultrasound dissector improve parathyroid gland preservation during surgery? Eur. J. Surg. Oncol. 2014, 40, 865–868. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Li, X.; Dong, J.; Sun, W. A comparison of surgical outcomes and complications between hemostatic devices for thyroid surgery: A network meta-analysis. Eur. Arch. Otorhinolaryngol. 2017, 274, 1269–1278. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Wang, C.C.; Wu, C.W.; Lin, Y.C.; Lu, I.C.; Chang, P.Y.; Lien, C.F.; Wang, C.C.; Hwang, T.Z.; Huang, T.Y.; et al. Comparison of Surgical Complications Rates Between LigaSure Small Jaw and Clamp-and-Tie Hemostatic Technique in 1000 Neuro-Monitored Thyroidectomies. Front. Endocrinol. 2021, 12, 638608. [Google Scholar]
- Vrinceanu, D.; Dumitru, M.; Marinescu, A.; Serboiu, C.; Musat, G.; Radulescu, M.; Popa-Cherecheanu, M.; Ciornei, C.; Manole, F. Management of Giant Thyroid Tumors in Patients with Multiple Comorbidities in a Tertiary Head and Neck Surgery Center. Biomedicines 2024, 12, 2204. [Google Scholar] [CrossRef]
| Group A (n502) Floseal + HS TT | Group B (n368) Standard TT | p-Value | |
|---|---|---|---|
| Age (years) ° | 69.2 ± 4.0 | 68.8 ± 6.6 | 0.099 |
| Gender (%) | |||
| -Male | 149 (29.7%) | 95 (25.9%) | 0.176 |
| -Female | 353 (70.3%) | 273 (74.1%) | 0.184 |
| ASA I-II | 450 (89.8%) | 338 (92.1%) | 0.192 |
| ASA III-IV | 52 (10.2%) | 30 (7.9%) | 0.121 |
| BMI (kg/m2) | 23.3 ± 0.6 | 22.5 ± 0.5 | 0.165 |
| Thyroidal disease | |||
| -NORMOFUNCTIONAL NODULES | 242 (48.3%) | 169 (45.9%) | 0.823 |
| Multinodular goiter | 117 (23.3%) | 83 (22.5%) | 0.794 |
| Uninodular goiter | 87 (17.3%) | 65 (17.7%) | 0.898 |
| Follicular adenoma | 32 (6.4%) | 18 (4.9%) | 0.353 |
| Hurthle cell adenoma | 6 (1.3%) | 3 (0.8) | 0.584 |
| -HYPERTHYROID GOITER | 176 (35.0%) | 138 (37.5%) | 0.789 |
| Basedow disease | 132 (26.3%) | 104 (28.3%) | 0.519 |
| Plummer adenoma | 44 (8.8%) | 34 (9.2%) | 0.808 |
| -CARCINOMA | |||
| Papillary | 84 (16.7%) | 71 (19.1%) | 0.768 |
| Follicular | 58 (11.5%) | 50 (13.6%) | 0.368 |
| Medullary | 18 (3.6%) | 14 (3.8%) | 0.865 |
| Anaplastic | 8 (1.6%) | 7 (1.7%) | 0.729 |
| 0 | 0 | - | |
| Preoperative calcemia (mg/dL) ° | 9.2 ± 0.8 | 9.3 ± 0.6 | 0.234 |
| Hypertension | 137 (27.3%) | 107 (29.0%) | 0.562 |
| Smoking | 125 (24.9%) | 90 (24.5%) | 0.880 |
| Cerebrovascular disease | 3 (0.6%) | 4 (1%) | 0.434 |
| Heart ischemic attack | 5 (1.0%) | 2 (0.5%) | 0.460 |
| Group A (n502) Floseal + HS TT | Group B (n368) Standard TT | p-Value | |
|---|---|---|---|
| Drain output after 24 h (mL) ° | 52 ± 25 | 83 ± 28 | 0.002 * |
| Drain output after 48 h (mL) ° | 95 ± 29 | 113 ± 27 | 0.003 * |
| Significant blood loss (%) | 3 (0.6%) | 8 (2.2%) | 0.039 * |
| Reoperation | 2 (0.4%) | 7 (1.9%) | 0.030 * |
| Day of discharge | 3.21 ± 0.75 | 3.48 ± 0.89 | 0.091 |
| Seroma | 9 (1.9%) | 19 (5.1%) | 0.005 * |
| Surgical site infection | 0 | 0 | - |
| Neck hematoma | 7 (1.4%) | 15 (4.3%) | 0.012 * |
| Laryngeal nerve palsy | 1 (0.2%) | 1 (0.3%) | 0.825 |
| Mortality | 0 | 0 | - |
| Post-surgical hypocalcemia (%) | 38 (7.5%) | 42 (11.4%) | 0.052 |
| Group A (n502) Floseal + HS TT | Group B (n368) Standard TT | p-Value | |
|---|---|---|---|
| Operation Time (min) ° | 68.4 ± 37.64 | 75.88 ± 14.78 | 0.031 * |
| Thyroid Volume (mL) ° | 29.97 ± 7.45 | 32.01 ± 3.45 | 0.119 |
| Definitive Pathology | |||
| 199 (39.5%) | 134 (36.4%) | |
| 303 (60.5%) | 234 (63.6%) | 0.677 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parisi, S.; Gambardella, C.; Ruggiero, R.; Docimo, G.; Marotta, V.; Gubitosi, A.; Mongardini, F.M.; D’Orazi, V.; Fisone, F.; Brusciano, L.; et al. Total Thyroidectomy with Harmonic Scalpel Combined with Gelatin Thrombin Hemostatic: A Focus on the Elderly Population—A Multicentric Study. Medicina 2025, 61, 496. https://doi.org/10.3390/medicina61030496
Parisi S, Gambardella C, Ruggiero R, Docimo G, Marotta V, Gubitosi A, Mongardini FM, D’Orazi V, Fisone F, Brusciano L, et al. Total Thyroidectomy with Harmonic Scalpel Combined with Gelatin Thrombin Hemostatic: A Focus on the Elderly Population—A Multicentric Study. Medicina. 2025; 61(3):496. https://doi.org/10.3390/medicina61030496
Chicago/Turabian StyleParisi, Simona, Claudio Gambardella, Roberto Ruggiero, Giovanni Docimo, Vincenzo Marotta, Adelmo Gubitosi, Federico Maria Mongardini, Valerio D’Orazi, Francesca Fisone, Luigi Brusciano, and et al. 2025. "Total Thyroidectomy with Harmonic Scalpel Combined with Gelatin Thrombin Hemostatic: A Focus on the Elderly Population—A Multicentric Study" Medicina 61, no. 3: 496. https://doi.org/10.3390/medicina61030496
APA StyleParisi, S., Gambardella, C., Ruggiero, R., Docimo, G., Marotta, V., Gubitosi, A., Mongardini, F. M., D’Orazi, V., Fisone, F., Brusciano, L., Tolone, S., Docimo, L., & Lucido, F. S. (2025). Total Thyroidectomy with Harmonic Scalpel Combined with Gelatin Thrombin Hemostatic: A Focus on the Elderly Population—A Multicentric Study. Medicina, 61(3), 496. https://doi.org/10.3390/medicina61030496








