Artificial Intelligence in Cardiopulmonary Resuscitation
Abstract
1. Introduction
2. Methodology
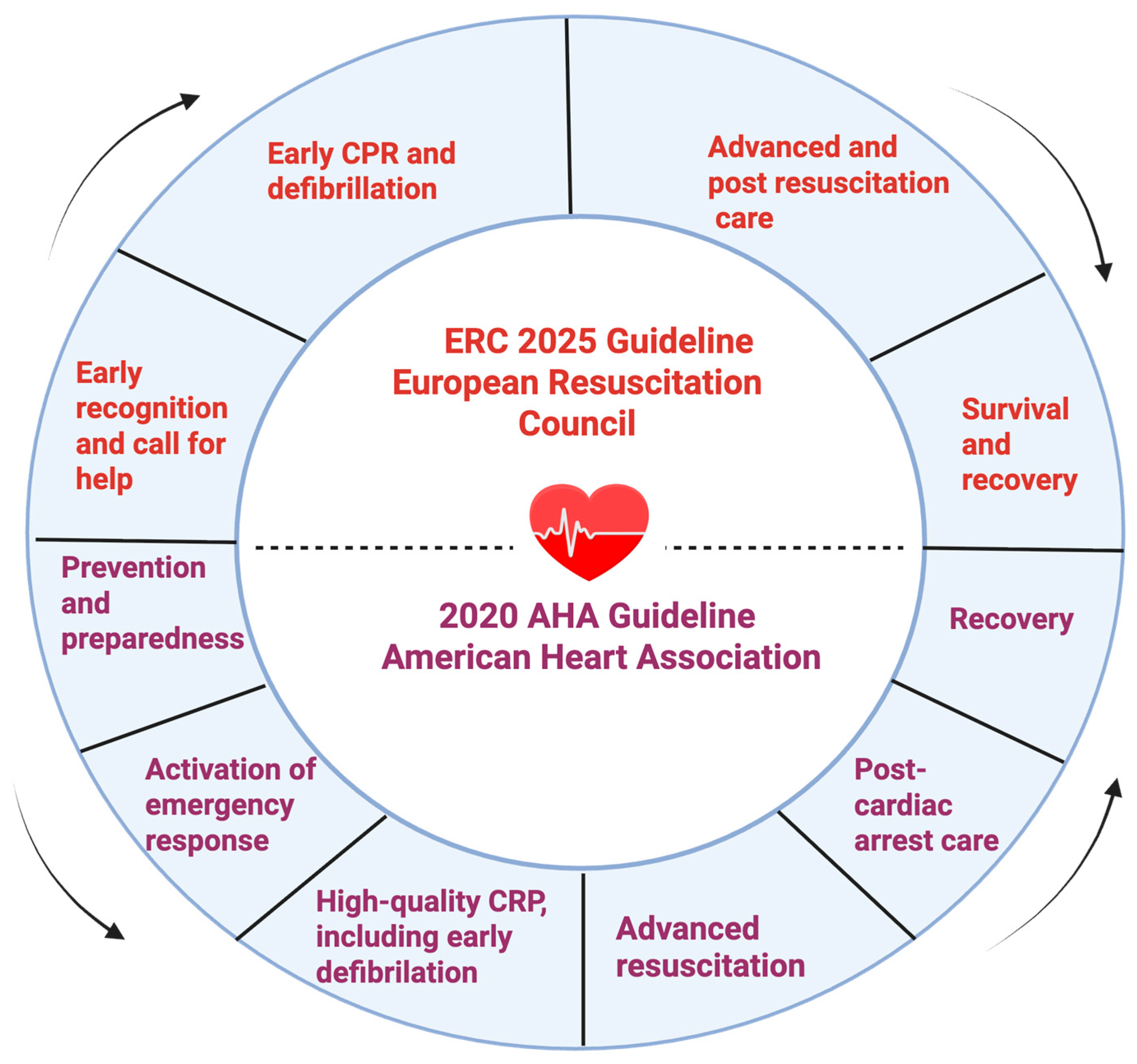
3. Chain of Survival
- -
- Prevention and preparedness;
- -
- Activation of the emergency response system;
- -
- High-quality CPR, including early defibrillation;
- -
- Advanced resuscitation interventions;
- -
- Post-cardiac arrest care;
- -
- Recovery.
3.1. Prevention and Preparedness
3.2. Early Recognition and Activation of the Emergency Medical System
3.3. Basic Life Support (BLS) with High-Quality Chest Compressions and Early Defibrillation
3.4. Advanced Life Support (ALS)
3.5. Post-Resuscitation Care
3.6. Recovery
4. Integrative and Cross-Domain Approaches in Resuscitation Science
5. Education and Training in AI-Enhanced Resuscitation
6. Limitations and Future Perspectives
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavoans, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142 (Suppl. S2), S366–S468. [Google Scholar]
- Kiguchi, T.; Okubo, M.; Nishiyama, C.; Maconochie, I.; Ong, M.E.H.; Kern, K.B.; Wyckoff, M.H.; McNally, B.; Christensen, E.F.; Tjelmeland, I.; et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation 2020, 152, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Nishiyama, C.; Kiguchi, T.; Okubo, M.; Alihodžić, H.; Al-Araji, R.; Baldi, E.; Beganton, F.; Booth, S.; Bray, J.; Christensen, E.; et al. Three-year trends in out-of-hospital cardiac arrest across the world: Second report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation 2023, 186, 109757. [Google Scholar] [CrossRef]
- Gräsner, J.T.; Herlitz, J.; Tjelmeland, I.B.M.; Wnent, J.; Masterson, S.; Lilja, G.; Bein, B.; Bottiger, B.W.; Rosell-Ortiz, F.; Nolan, J.P.; et al. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe. Resuscitation 2021, 161, 61–79. [Google Scholar] [CrossRef]
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M.; Lavonas, E.J.; Magid, D.J. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142 (Suppl. S2), S337–S357. [Google Scholar] [CrossRef]
- Islam, S.; Rjoub, G.; Elmekki, H.; Bentahar, J.; Pedrycz, W.; Cohen, R. Machine learning innovations in CPR: A comprehensive survey on enhanced resuscitation techniques. Artif. Intell. Rev. 2025, 58, 233. [Google Scholar] [CrossRef] [PubMed]
- Zace, D.; Semeraro, F.; Schnaubelt, S.; Montomoli, J.; Ristagno, G.; Fijačko, N.; Gamberini, L.; Bignami, E.G. Artificial intelligence in resuscitation: A scoping review. Resusc. Plus 2025, 24, 100973. [Google Scholar] [CrossRef]
- Isasi, I.; Jaureguibeitia, X.; Alonso, E.; Elola, A.; Aramendi, E.; Wik, L. Artificial Intelligence for Multiclass Rhythm Analysis for Out-of-Hospital Cardiac Arrest During Mechanical Cardiopulmonary Resuscitation. Mathematics 2025, 13, 1251. [Google Scholar] [CrossRef]
- Lee, S.; Lee, K.S.; Park, H.J.; Han, K.S.; Song, J.; Lee, S.W.; Kim, S.J. A Comparative Study of Convolutional Neural Network and Recurrent Neural Network Models for the Analysis of Cardiac Arrest Rhythms During Cardiopulmonary Resuscitation. Appl. Sci. 2025, 15, 4148. [Google Scholar] [CrossRef]
- Shen, C.P.; Freed, B.C.; Walter, D.P.; Perry, J.C.; Barakat, A.F.; Elashery, A.R.A.; Shah, K.S.; Kutty, S.; McGillion, M.; Siong Ng, F.; et al. Convolution Neural Network Algorithm for Shockable Arrhythmia Classification Within a Digitally Connected Automated External Defibrillator. J. Am. Heart Assoc. 2023, 12, e026974. [Google Scholar] [CrossRef] [PubMed]
- Krishnamurti, C.; Mrutu, S. Artificial Intelligence in Cardiac Emergencies: A Review. Indian J. Clin. Cardiol. 2025, 6, 148–154. [Google Scholar] [CrossRef]
- Schnaubelt, S.; Monsieurs, K.G.; Fijacko, N.; Veigl, C.; Al-Hilali, Z.; Atiq, H.; Bigham, B.L.; Eastwood, K.; Ko, Y.C.; Matsuyama, T.; et al. International facets of the ‘chain of survival’ for out-of-hospital and in-hospital cardiac arrest—A scoping review. Resusc. Plus 2024, 19, 100689. [Google Scholar] [CrossRef]
- Srivats, S.; Zghyer, F.; Shahrori, Z.; Albert, C.; Al-Khatib, S.M.; Chugh, S.; Etheridge, S.P.; Goldberger, Z.D.; Gopinathannair, R.; Lakkireddy, D.; et al. Sudden cardiac arrest: Limitations in risk-stratification and treatment, and the potential for digital technologies and artificial intelligence to improve prediction and outcomes. Prog. Cardiovasc. Dis. 2025, 91, 144–166. [Google Scholar] [CrossRef] [PubMed]
- Prasad, S.; Ayhan, I.; Mohammed, D.; Kalafat, E.; Khalil, A. Longitudinal twin growth discordance patterns and adverse perinatal outcomes. Am. J. Obstet. Gynecol. 2025, 233, 73.e1–73.e14. [Google Scholar] [CrossRef] [PubMed]
- Gebran, A.; Vapsi, A.; Maurer, L.R.; El Moheb, M.; Naar, L.; Thakur, S.S.; Sinyard, R.; Daye, D.; Velmahos, G.C.; Bertsimas, D.; et al. POTTER-ICU: An artificial intelligence smartphone-accessible tool to predict the need for intensive care after emergency surgery. Surgery 2022, 172, 470–475. [Google Scholar] [CrossRef] [PubMed]
- El Hechi, M.; Gebran, A.; Bouardi, H.T.; Maurer, L.R.; El Moheb, M.; Zhuo, D.; Dunn, J.; Bertsimas, D.; Velmahos, G.C.; Kaafarani, H.M. Validation of the artificial intelligence–based trauma outcomes predictor (TOP) in patients 65 years and older. Surgery 2022, 171, 1687–1694. [Google Scholar] [CrossRef]
- Chen, K.W.; Wang, Y.C.; Liu, M.H.; Tsai, B.Y.; Wu, M.Y.; Hsieh, P.H.; Wei, J.T.; Shih, E.S.; Shiao, Y.T.; Hwang, M.J.; et al. Artificial intelligence-assisted remote detection of ST-elevation myocardial infarction using a mini-12-lead electrocardiogram device in prehospital ambulance care. Front. Cardiovasc. Med. 2022, 9, 1001982. [Google Scholar]
- Lewandowski, M. A Review of the Commercially Available ECG Detection and Transmission Systems—The Fuzzy Logic Approach in the Prevention of Sudden Cardiac Arrest. Micromachines 2021, 12, 1489. [Google Scholar] [CrossRef]
- Chang, H.K.; Wu, C.T.; Liu, J.H.; Jang, J.S.R. Using Machine Learning Algorithms in Medication for Cardiac Arrest Early Warning System Construction and Forecasting. In Proceedings of the 2018 Conference on Technologies and Applications of Artificial Intelligence (TAAI) Taichung, Taichung, Taiwan, 30 November–2 December 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 1–4. Available online: https://ieeexplore.ieee.org/document/8588466/ (accessed on 18 October 2025).
- Olive, M.K.; Owens, G.E. Current monitoring and innovative predictive modeling to improve care in the pediatric cardiac intensive care unit. Transl. Pediatr. 2018, 7, 120–128. [Google Scholar] [CrossRef]
- Thorn, S.; Güting, H.; Maegele, M.; Gruen, R.L.; Mitra, B. Early Identification of Acute Traumatic Coagulopathy Using Clinical Prediction Tools: A Systematic Review. Medicina 2019, 55, 653. [Google Scholar] [CrossRef]
- Kim Jhyun Cho, E.Y.; Choi, Y.; Won, J.Y.; Cheon, S.H.; Kim, Y.A.; Lee, K.B.; Kim, K.J.; Kim, H.G.; Sim, T. Deep Learning–Based Early Warning Systems in Hospitalized Patients at Risk of Code Blue Events and Length of Stay: Retrospective Real-World Implementation Study. JMIR Med. Inform. 2025, 13, e72232. [Google Scholar]
- Oberdier, M.T.; Neri, L.; Orro, A.; Carrick, R.T.; Nobile, M.S.; Jaipalli, S.; Khan, M.; Diciotti, S.; Borghi, C.; Halperin, H.R. Sudden cardiac arrest prediction via deep learning electrocardiogram analysis. Eur. Heart J.—Digit. Health 2025, 6, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Ghasad, P.P.; Vegivada, J.V.S.; Kamble, V.M.; Bhurane, A.A.; Santosh, N.; Sharma, M.; Tan, R.S.; Acharya, U.R. A systematic review of automated prediction of sudden cardiac death using ECG signals. Physiol. Meas. 2025, 46, 01TR01. [Google Scholar] [CrossRef]
- Dores, H.; Dinis, P.; Viegas, J.M.; Freitas, A. Preparticipation Cardiovascular Screening of Athletes: Current Controversies and Challenges for the Future. Diagnostics 2024, 14, 2445. [Google Scholar] [CrossRef]
- Scquizzato, T.; Gamberini, L.; Semeraro, F. How technology can save lives in cardiac arrest. Curr. Opin. Crit. Care 2022, 28, 250–255. [Google Scholar] [CrossRef]
- Byrsell, F.; Claesson, A.; Ringh, M.; Svensson, L.; Jonsson, M.; Nordberg, P.; Forsberg, S.; Hollenberg, J.; Nord, A. Machine learning can support dispatchers to better and faster recognize out-of-hospital cardiac arrest during emergency calls: A retrospective study. Resuscitation 2021, 162, 218–226. [Google Scholar] [CrossRef]
- Blomberg, S.N.; Christensen, H.C.; Lippert, F.; Ersbøll, A.K.; Torp-Petersen, C.; Sayre, M.R.; Kudenchuk, P.J.; Folke, F. Effect of Machine Learning on Dispatcher Recognition of Out-of-Hospital Cardiac Arrest During Calls to Emergency Medical Services: A Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2032320. [Google Scholar] [CrossRef]
- Chin, K.C.; Hsieh, T.C.; Chiang, W.C.; Chien, Y.C.; Sun, J.T.; Lin, H.Y.; Hsieh, M.J.; Yang, C.W.; Chen, A.Y.; Huei-Ming Ma, M. Early recognition of a caller’s emotion in out-of-hospital cardiac arrest dispatching: An artificial intelligence approach. Resuscitation 2021, 167, 144–150. [Google Scholar] [CrossRef]
- Zicari, R.V.; Brusseau, J.; Blomberg, S.N.; Christensen, H.C.; Coffee, M.; Ganapini, M.B.; Gerke, S.; Gilbert, T.; Hikman, E.; Hildt, E.; et al. On Assessing Trustworthy AI in Healthcare. Machine Learning as a Supportive Tool to Recognize Cardiac Arrest in Emergency Calls. Front. Hum. Dyn. 2021, 3, 673104. [Google Scholar] [CrossRef]
- Blomberg, S.N.; Folke, F.; Ersbøll, A.K.; Christensen, H.C.; Torp-Pedersen, C.; Sayre, M.R.; Counts, C.R.; Lippert, F.K. Machine learning as a supportive tool to recognize cardiac arrest in emergency calls. Resuscitation 2019, 138, 322–329. [Google Scholar] [CrossRef]
- Zhong, Z.; Li, W.; Zhou, L.; Liu, L. Factors influencing the performance of cardiopulmonary resuscitation by lay rescuers: A qualitative study based on the Theory of Planned Behavior. PLoS ONE 2025, 20, e0327439. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.P.; Jonsson, M.; Böttiger, B.W.; Rott, N. Telephone cardiopulmonary resuscitation, first responder systems, cardiac arrest centers, and global campaigns to save lives. Curr. Opin. Crit. Care 2023, 29, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Brown, G.; Conway, S.; Ahmad, M.; Adegbie, D.; Patel, N.; Myneni, V.; Alradhawi, M.; Kumar, N.; Obaid, D.R.; Pimenta, D.; et al. Role of artificial intelligence in defibrillators: A narrative review. Open Heart 2022, 9, e001976. [Google Scholar] [CrossRef]
- Hellenthal, K.E.M.; Porschen, C.; Wnent, J.; Lange, M. Evolving role of point-of-care ultrasound in prehospital emergency care: A narrative review. Scand. J. Trauma. Resusc. Emerg. Med. 2025, 33, 126. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Jung, S.; Park, J.H.; Cho, H.; Moon, S.; Lee, S. Artificial intelligence for predicting shockable rhythm during cardiopulmonary resuscitation: In-hospital setting. Resuscitation 2024, 202, 110325. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Yoon, H.; Yeon Kang, S.; Joon Jo, I.; Heo, S.; Chang, H.; Parc, J.E.; Lee, G.; Kim, T.; Hwang, S.Y.; et al. Artificial intelligence-based evaluation of carotid artery compressibility via point-of-care ultrasound in determining the return of spontaneous circulation during cardiopulmonary resuscitation. Resuscitation 2024, 202, 110302. [Google Scholar] [CrossRef]
- Spacek, R.; Weiss, V.; Kavalkova, P.; Jiravsky, O.; Barcak, J.; Belohlavek, J. Age as a Mortality Predictor in ECPR Patients. Medicina 2024, 60, 1444. [Google Scholar] [CrossRef]
- Nordseth, T.; Eftestøl, T.; Aramendi, E.; Kvaløy, J.T.; Skogvoll, E. Extracting physiologic and clinical data from defibrillators for research purposes to improve treatment for patients in cardiac arrest. Resusc. Plus 2024, 18, 100611. [Google Scholar] [CrossRef]
- Alrawashdeh, A.; Alkhatib, Z.I. Incidence and outcomes of in-hospital resuscitation for cardiac arrest among paediatric patients in Jordan: A retrospective observational study. BMJ Paediatr Open 2024, 8, e003013. [Google Scholar] [CrossRef]
- Rawshani, A.; Hessulf, F.; Deminger, J.; Sultanian, P.; Gupta, V.; Lundgren, P.; Mohammed, M.; Alchay, M.A.; Dioland, T.; Gryska, E.; et al. Prediction of neurologic outcome after out-of-hospital cardiac arrest: An interpretable approach with machine learning. Resuscitation 2024, 202, 110359. [Google Scholar] [CrossRef]
- Kawai, Y.; Kogeichi, Y.; Yamamoto, K.; Miyazaki, K.; Asai, H.; Fukushima, H. Explainable artificial intelligence-based prediction of poor neurological outcome from head computed tomography in the immediate post-resuscitation phase. Sci. Rep. 2023, 13, 5759. [Google Scholar] [CrossRef]
- Leon, M. Revolutionizing Donor Heart Procurement: Innovations and Future Directions for Enhanced Transplantation Outcomes. J. Cardiovasc. Dev. Dis. 2024, 11, 235. [Google Scholar] [CrossRef]
- Ogawara, T.; Usui, A.; Homma, N.; Funayama, M. Diagnosing Drowning in Postmortem CT Images Using Artificial Intelligence. Tohoku J. Exp. Med. 2023, 259, 65–75. [Google Scholar] [CrossRef]
- Shin, S.J.; Bae, H.S.; Moon, H.J.; Kim, G.W.; Cho, Y.S.; Lee, D.W.; Jeong, D.K.; Kim, H.J.; Lee, H.J. Evaluation of optimal scene time interval for out-of-hospital cardiac arrest using a deep neural network. Am. J. Emerg. Med. 2023, 63, 29–37. [Google Scholar] [CrossRef]
- Kim, J.W.; Ha, J.; Kim, T.; Yoon, H.; Hwang, S.Y.; Jo, I.J.; Shin, T.G.; Sim, M.S.; Cha, W.C. Developing a Time-Adaptive Prediction Model for Out-of-Hospital Cardiac Arrest: Nationwide Cohort Study in Korea. J. Med. Internet Res. 2021, 23, e28361. [Google Scholar] [CrossRef]
- Dumas, F.; Bougouin, W.; Cariou, A. Cardiac arrest: Prediction models in the early phase of hospitalization. Curr. Opin. Crit. Care 2019, 25, 204–210. [Google Scholar] [CrossRef]
- Goyal, A.; Puttaswamy, D.; Kadam, E.; Maheshwari, S.; Hurjkaliani, S.; Goyal, P.; Thakkar, K.; Shah, V.; Daoud, M.; Mahalwar, G. Telemedicine for the detection and management of in-hospital and out-of-hospital sudden cardiac arrest: Status quo and quo vadis. Am. Heart J. Plus Cardiol. Res. Pract. 2025, 59, 100600. [Google Scholar] [CrossRef] [PubMed]
- Fijačko, N.; Schnaubelt, S.; Nadkarni, V.M.; Metličar, Š.; Greif, R. Analyzing resuscitation conference content through the lens of the chain of survival. Resusc. Plus 2025, 23, 100951. [Google Scholar] [CrossRef]
- Wei, S.; Guo, X.; He, S.; Zhang, C.; Chen, Z.; Chen, J.; Huang, Y.; Zhang, F.; Liu, Q. Application of Machine Learning for Patients with Cardiac Arrest: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2025, 27, e67871. [Google Scholar] [CrossRef] [PubMed]
- Lapostolle, F.; Agostinucci, J.M.; Petrovic, T.; Feral-Pierssens, A.L. Cardiac Arrest: Can Technology Be the Solution? J. Clin. Med. 2025, 14, 972. [Google Scholar] [CrossRef] [PubMed]
- Fortunov, R.M.; Cabacungan, E.; Barry, J.S.; Jagarapu, J. Artificial intelligence and informatics in neonatal resuscitation. Semin. Perinatol. 2024, 48, 151992. [Google Scholar] [CrossRef]
- Rietchel, L.J.; Belfiore, E.B.R.; Sigala, M.E.M.; D’Empaire, P.P. Point-of-Care Ultrasound in Trauma and the Evolving Role of the Anesthesiologist: A Narrative Review of Emerging Topic Trends. Curr. Anesthesiol. Rep. 2024, 15, 2. [Google Scholar] [CrossRef]
- Shao, Y.; Yang, Z.; Chen, W.; Zhang, Y. Implementing an intelligent diagnosis and treatment system for in-hospital cardiac arrest in the Utstein style: A multi-center case study. J. Transl. Med. 2024, 2, 996. [Google Scholar] [CrossRef] [PubMed]
- Nádasi, E.; Héder, M. The future of medicine or a threat? Artificial intelligence representation in Chicago Med. Humanit. Soc. Sci. Commun. 2024, 11, 1346. [Google Scholar] [CrossRef]
- Semeraro, F.; Schnaubelt, S.; Malta Hansen, C.; Bignami, E.G.; Piazza, O.; Monsieurs, K.G. Cardiac arrest and cardiopulmonary resuscitation in the next decade: Predicting and shaping the impact of technological innovations. Resuscitation 2024, 200, 110250. [Google Scholar] [CrossRef] [PubMed]
- Birkun, A.A. Misinformation on resuscitation and first aid as an uncontrolled problem that demands close attention: A brief scoping review. Public Health 2024, 228, 147–149. [Google Scholar] [CrossRef]
- Plodr, M.; Chalusova, E. Current trends in the management of out of hospital cardiac arrest (OHCA). Biomed. Pap. Med. Fac. Univ. Palacky. Olomouc Czech Repub. 2024, 168, 105–116. [Google Scholar] [CrossRef]
- Aqel, S.; Syaj, S.; Al-Bzour, A.; Abuzanouneh, F.; Al-Bzour, N.; Ahmad, J. Artificial Intelligence and Machine Learning Applications in Sudden Cardiac Arrest Prediction and Management: A Comprehensive Review. Curr. Cardiol. Rep. 2023, 25, 1391–1396. [Google Scholar] [CrossRef]
- Piliuk, K.; Tomforde, S. Artificial intelligence in emergency medicine. A systematic literature review. Int. J. Med. Inform. 2023, 180, 105274. [Google Scholar] [CrossRef]
- Carrigan, A.; Roberts, N.; Han, J.; John, R.; Khan, U.; Sultani, A.; Austin, E.E. The Digital Hospital: A Scoping Review of How Technology Is Transforming Cardiopulmonary Care. Heart Lung Circ. 2023, 32, 1057–1068. [Google Scholar] [CrossRef]
- Moon, H.J.; Shin, Y.J.; Cho, Y.S. Identification of out-of-hospital cardiac arrest clusters using unsupervised learning. Am. J. Emerg. Med. 2022, 62, 41–48. [Google Scholar] [CrossRef]
- Batey, N.; Henry, C.; Garg, S.; Wagner, M.; Malhotra, A.; Valstar, M.; Smith, T.; Sharkey, D. The newborn delivery room of tomorrow: Emerging and future technologies. Pediatr. Res. 2024, 96, 586–594. [Google Scholar] [CrossRef] [PubMed]
- Rajagopalan, B.; Shen, W.K.; Patton, K.; Kutyifa, V.; Di Biase, L.; Al-Ahmad, A.; Natale, A.; Gopinathannair, R.; Lakkireddy, D. Surviving sudden cardiac arrest—Successes, challenges, and opportunities. J. Interv. Card. Electrophysiol. 2022, 64, 567–571. [Google Scholar] [CrossRef] [PubMed]
- Narayan, S.M.; Wang, P.J.; Daubert, J.P. New Concepts in Sudden Cardiac Arrest to Address an Intractable Epidemic. J. Am. Coll. Cardiol. 2019, 73, 70–88. [Google Scholar] [CrossRef] [PubMed]
- Kitapcioglu, D.; Aksoy, M.E.; Ozkan, A.E.; Usseli, T.; Cabuk Colak, D.; Torun, T. Enhancing Immersion in Virtual Reality–Based Advanced Life Support Training: Randomized Controlled Trial. JMIR Serious Games 2025, 13, e68272. [Google Scholar] [CrossRef]
- Constable, M.D.; Zhang, F.X.; Conner, T.; Monk, D.; Rajsic, J.; Ford, C.; Park, L.J.; Platt, A.; Porteous, D.; Grierson, L.; et al. Advancing healthcare practice and education via data sharing: Demonstrating the utility of open data by training an artificial intelligence model to assess cardiopulmonary resuscitation skills. Adv. Health Sci. Educ. 2025, 30, 15–35. [Google Scholar] [CrossRef]
| Reference | Objective | Methodology | Key Findings | Relevance to Prevention and Preparedness |
|---|---|---|---|---|
| Kim et al., 2025 [22] | To evaluate changes in clinical outcomes following implementation of VitalCare (an AI-based early warning system) and validate algorithmic performance | Retrospective analysis of 30,785 inpatient cases using electronic health record data from general wards and ICUs | The AI-based model showed strong predictive capacity for major in-hospital adverse events by providing early warnings to clinicians | Demonstrates how AI early-warning systems enhance preparedness, optimize human resource use, and improve workflow efficiency in hospital settings |
| Oberdier et al., 2025 [23] | To predict sudden cardiac arrest (SCA) using short 12-lead ECG segments and deep convolutional neural networks | Analysis of public ECG datasets (10 s recordings) from 221 SCA and 1046 control subjects, including demographic and temporal variables | Deep learning achieved promising accuracy in SCA prediction; performance improved as ECGs were recorded closer to the event. QRS complex data were the most influential features | Highlights the feasibility of AI-based ECG analysis for pre-event risk detection and its potential to improve individualized preventive screening |
| Ghasad et al., 2025 [24] | Systematic review of automated sudden cardiac death (SCD) prediction models developed between 2011–2023 | Analysis of ML/DL algorithms (KNN, SVM, decision trees, random forest, CNNs) using databases such as MIT-BIH SCD Holter | Machine and deep learning methods achieved up to 97% accuracy, predicting SCD 30–70 min before onset. However, performance depends on training data size and multimodal integration | Confirms that advanced AI models can anticipate SCD with high precision but emphasizes the need for larger datasets and real-time clinical implementation |
| Dores et al., 2024 [25] | To review methodologies and challenges in preparticipation screening of athletes to prevent SCD | Narrative review integrating literature on digital screening, ECG interpretation, and AI-enhanced cardiology | AI and digital tools could improve early detection of cardiac abnormalities in athletes, addressing current gaps in manual screening | Underlines the need for ethical and regulatory frameworks to integrate AI safely into preventive cardiology and sports medicine |
| Ghebran et al., 2022 [15] | To develop an interpretable AI model predicting postoperative ICU requirement in emergency surgery | Optimal classification tree (OCT) algorithm trained on 464,861 cases from the ACS NSQIP database (2007–2017) | The Predictive OpTimal Trees in Emergency Surgery Risk ICU tool accurately predicted postoperative critical care need (C-statistic ≈ 0.89) | Demonstrates AI’s ability to improve perioperative preparedness, ICU triage, and early postoperative intervention to reduce preventable mortality |
| Chen et al., 2022 [17] | To implement real-time AI-assisted detection of STEMI in prehospital 12-lead ECGs | CNN-LSTM model used by EMTs in 14 AI-equipped fire stations; 362 ECGs analyzed, compared to physician interpretation | AI achieved 99% accuracy (AUC 0.997) and reduced ECG-to-feedback time from 113 s to 37 s, enabling earlier reperfusion | Proves that AI can enhance prehospital preparedness and minimize delays in STEMI treatment through rapid and autonomous triage |
| El Hechi et al., 2022 [16] | To validate the Trauma Outcomes Predictor model for geriatric trauma patients using ML-based OCTs | Retrospective cohort of 260,505 patients (aged ≥ 65) from the ACS-TQIP database; model evaluated for mortality and morbidity prediction | Model achieved excellent discrimination (C = 0.83–0.92) and accurately predicted mortality and complications | Reinforces AI’s role in early identification of high-risk trauma patients, enhancing system-level readiness and tailored resource deployment |
| Levandowski et al., 2021 [18] | To develop a rapid response AI-based rescue system (PROTECTOR) for out-of-hospital cardiac arrest detection | Fuzzy logic–based ECG rhythm classifier linked to automatic alarm and geolocation transmission to EMS | The system achieved 100% sensitivity and 97.8% specificity, transmitting alarms and AED maps within seconds | Represents a breakthrough in community-level preparedness, providing immediate detection and automated EMS activation for SCA events |
| Thorn et al., 2019 [21] | To identify and assess predictive models for acute traumatic coagulopathy (ATC) | Systematic review of studies (1998–2018) evaluating prognostic tools using clinical and laboratory variables | Bayesian network models predicted abnormal coagulation (PT > 1.2) with 90% sensitivity and 92% specificit | Demonstrates AI’s potential in trauma risk prediction and prevention, though external validation is still limited |
| Olive et al., 2018 [20] | To discuss challenges in monitoring pediatric cardiac ICU patients and AI’s potential for early decompensation prediction | Narrative review of monitoring data and predictive modeling in PCICU environments | AI and big data analytics can anticipate deterioration by integrating physiological, laboratory, and clinical variables | Highlights AI’s preventive role in pediatric intensive care by enhancing surveillance and anticipating decompensation before critical events |
| Reference | Objective | Methodology | Key Findings | Relevance to EMS Activation |
|---|---|---|---|---|
| Scquizzato et al., 2021 [26] | To review how emerging technologies are being implemented across all steps of the Chain of Survival and their effects on cardiac arrest outcomes | Narrative review summarizing current and future applications of technology (mobile responders, drones, AI dispatchers, wearables) in out-of-hospital and in-hospital cardiac arrest management | Technology now enhances every stage of the Chain of Survival—from prevention and recognition to CPR and defibrillation. Citizen-alert apps, drones delivering AEDs, and AI-based dispatch support improved bystander response and outcomes | Demonstrates that AI and digital tools shorten EMS activation time, improve early recognition, and optimize system coordination across prehospital and in-hospital settings |
| Chin et al., 2021 [29] | To develop an AI model capable of assessing callers’ emotional states during out-of-hospital cardiac arrest (OHCA) emergency calls | Analysis of 337 OHCA audio recordings using Mel-frequency cepstral coefficients and support vector machines (SVM). Performance validated by repeated random sub-sampling cross-validation (RRS-CV) | The AI model classified emotional and cooperative levels with >90% predictive accuracy and 98.6% specificity, even when using only the first 10 s of voice input | Facilitates dispatcher prioritization by identifying emotionally stable callers, allowing focus on high-stress interactions where delayed CPR guidance is more likely |
| Zicari et al., 2021 [30] | To apply the EU “Trustworthy AI” framework (HLEG) to evaluate an ML-based system for recognizing cardiac arrest during emergency calls | Interdisciplinary 1Z-Inspection® involving ethicists, policymakers, technical, and clinical experts; case study based on Copenhagen’s ML-assisted dispatcher system | Highlighted the necessity of human oversight, transparency, and interdisciplinary ethical evaluation in clinical AI deployment | Reinforces that ethically governed AI systems increase trust and reliability in EMS operations, supporting sustainable integration of AI into dispatch systems |
| Byrsell et al., 2021 [27] | To assess whether ML could improve dispatcher recognition of OHCA within the first minute of emergency calls | Observational study analyzing 851 OHCA calls with ML model tuned for multiple false positive rate (FPR) thresholds | ML recognized 36% of OHCAs within the first minute vs. 25% by dispatchers, reducing median recognition time by 28 s (p < 0.001) | Confirms AI’s ability to accelerate OHCA recognition and initiate EMS activation faster, directly enhancing survival chain efficiency |
| Blomberg et al., 2019 [31] | To compare ML performance with human dispatchers in identifying OHCA from recorded emergency calls | Retrospective analysis of 108,607 emergency calls in Copenhagen; ML trained on audio features and validated against dispatcher decisions | ML achieved higher sensitivity (84.1% vs. 72.5%) and shorter recognition times (median 44 s vs. 54 s) | Establishes ML as a decision-support tool that accelerates dispatcher recognition and shortens EMS activation time |
| Blomberg et al., 2021 [28] | To evaluate ML-assisted dispatcher alerts in real emergency settings and their impact on OHCA recognition | Double-masked, randomized clinical trial including 169,049 emergency calls (Copenhagen, Denmark). ML alerts compared with standard dispatcher protocols | Dispatchers assisted by ML recognized 93.1% of confirmed OHCA vs. 90.5% in controls (p = 0.15). ML alone demonstrated higher sensitivity (85% vs. 77.5%) and faster recognition | Validates the real-world feasibility of AI-assisted dispatch; AI complements human performance by increasing recognition speed and reducing missed cardiac arrests |
| Reference | Objective | Methodology | Key Findings | Relevance |
|---|---|---|---|---|
| Goyal et al., 2025 [48] | To evaluate telemedicine integration in cardiac emergency care | Review | Integrating artificial intelligence enhances telemedicine’s potential by enabling personalized care and predictive analytics | Telemedicine strengthens the “Chain of Survival” for out-of-hospital cardiac arrest through telecommunicator-assisted CPR, boosting bystander CPR rates and survival chances |
| Islam et al., 2025 [6] | To explore the transformative role of ML and AI in cardiopulmonary resuscitation (CPR) | Systematic survey and taxonomy of ML techniques in CPR | ML techniques classified into four CPR-related domains: rhythm analysis, outcome prediction, compression modeling, and ROSC detection; highlighted XAI for model transparency. | Bridges the gap between resuscitation science and advanced ML, providing a structured foundation for innovation in ML-enhanced CPR |
| Fijacko et al., 2025 [49] | To analyze topics and technologies represented at resuscitation conferences | Bibliometric analysis using chain-of-survival framework | “Recognition and prevention” dominated conference abstracts; ML used in 54 (Resuscitation 2024) and 47 (Symposium 2024) studies, but no deep learning applied | Identifies research gaps, showing the underrepresentation of advanced AI methods in current resuscitation science |
| Wei et al., 2025 [50] | To assess ML’s predictive value for cardiac arrest occurrence and outcomes | Systematic review and meta-analysis | ML is a promising tool for predicting cardiac arrest and outcomes such as ROSC and mortality | Supports AI-driven enhancement of traditional prognostic tools for outcome prediction |
| Lapostolle et al., 2025 [51] | To review technological innovations for cardiac arrest management | Perspective review. | Highlighted emerging tools like AI-assisted dispatch, drone AED delivery, and mobile citizen responder apps | Emphasizes prioritizing early links in the Chain of Survival through gamification and education |
| Fortunov R.M. et al., 2024 [52] | To examine the integration of AI and automation in perinatal and resuscitation care | Narrative review | Identified key roles for predictive algorithms and remote monitoring in critical care | Suggests AI as an aid for rapid response and workflow optimization in emergent perinatal scenarios |
| Rietchel et al., 2025 [53] | To discuss point-of-care ultrasound (POCUS) in trauma anesthesiology | Narrative review | Expanding evidence for AI-assisted interpretation of ultrasound during CPR; POCUS use growing globally | Promotes ultrasound accessibility and skill dissemination in low-resource resuscitation environments |
| Shao et al., 2024 [54] | To introduce an intelligent system for diagnosing and treating IHCA | Hybrid model with deep reinforcement learning and virtual data generation | Improved CPR and ROSC outcomes even with incomplete patient data. | Demonstrates AI’s reliability in managing in-hospital cardiac arrest under uncertainty |
| Nadasi et al., 2024 [55] | To analyze how Chicago Med portrays medical AI and influences public perception | Qualitative media content analysis. | Presented both benefits and ethical dilemmas of AI in healthcare, from automation bias to equity issues | Highlights media’s role in shaping public trust and critical thinking about medical AI |
| Semeraro et al., 2024 [56] | To predict future CA management innovations using AI tools | Exploratory literature review with ChatGPT-4 and Gemini Advanced | Predicted adoption of robot CPR, wearable AEDs, and brain–computer interfaces within 3–8 years | Calls for ethical oversight and interdisciplinary collaboration in implementing AI-driven innovations |
| Bikun et al., 2024 [57] | To map misinformation about CPR and first aid | PRISMA-based scoping review | 97.7% of public sources contained misinformation; 25% included harmful or misleading advice | Urges global strategies to detect and prevent misinformation in public CPR education |
| Plodr et al., 2024 [58] | To review current trends in OHCA management | Narrative review | Emphasized improving EMDC information flow and rapid recognition of life-threatening conditions | Reinforces communication efficiency as a determinant of prehospital survival |
| Aquel et al., 2023 [59] | To examine AI and ML in predicting and managing sudden cardiac arrest outcomes | Literature synthesis | AI enhances prediction of shockable rhythms and neurological outcomes; supports real-time feedback. | Collaboration among clinicians, data scientists, and regulators is essential for optimizing AI-based CPR |
| Piliuk et al., 2023 [60] | To review AI applications and challenges in emergency medicine | Systematic review of 380 studies (116 included) | Found isolated, small-scale AI studies with limited generalization | Advocates for unified, human-AI integrated systems across emergency care |
| Carrigan et al., 2023 [61] | To assess the digital hospital model in cardiac and pulmonary care | Scoping review (13 studies) | Wireless ECG telemonitoring improved 24 h survival but not discharge rates | Demonstrates potential benefits of digital infrastructure, requiring robust support systems |
| Moon et al., 2023 [62] | To analyze spatial correlations in OHCA outcomes using ML | Retrospective registry analysis using VAE and DPMM clustering | Identified 8 clusters by geography; transfer to higher-level centers predicted better survival | Provides a data-driven framework for regional optimization of emergency systems |
| Batey et al., 2024 [63] | To apply AI and computer vision in neonatal resuscitation research | Neural network training on neonatal resuscitation videos | Real-time pattern recognition could assist clinicians and improve newborn outcomes | AI-based video feedback may enhance both clinical performance and staff training |
| Rajagopalan et al., 2022 [64] | To review SCA prevention and awareness initiatives | Narrative review | Highlighted campaigns for CPR education and AED access; discussed AI and voice-command CPR aids | Supports technology-enhanced public training and equitable access to life-saving interventions |
| Narayan et al., 2019 [65] | To outline global challenges in sudden cardiac arrest management | Review | Proposed a “Respond–Understand–Predict–Prevent” model integrating AI and open data | Advocates a holistic, policy-oriented approach to SCA prevention and research |
| Limitation | Description/Risks | Suggested Approaches to Address the Limitation |
|---|---|---|
1. Limited generalizability and external validation:
| Many models are trained on small or single-center datasets, reducing applicability across settings | Use multicenter, multinational datasets |
2. Underrepresentation of key demographic or clinical subgroups (bias)
| Certain populations (e.g., elderly, women, minorities, trauma, drowning, pediatrics) are often insufficiently represented, leading to biased predictions | Increase dataset diversity and stratified sampling |
3. Limited interpretability (“black-box” behavior)
| Lack of transparency reduces clinician trust and may hinder adoption; may impair ethical autonomy and informed decision-making | Incorporate explainable AI (XAI) tools |
4. Risk of violating ethical principles (autonomy, beneficence, non-maleficence, justice)
| Algorithmic recommendations may override clinician judgment (autonomy); inaccurate models may harm patients (maleficence); biased models create inequity (justice) | Maintain clinician-in-the-loop decision-making |
5. Heterogeneous definitions of outcomes (survival, neurologic recovery)
| Lack of uniform outcome metrics complicates model comparison and reproducibility | Adhere to standardized definitions |
6. Data quality limitations (missing data, noise, lack of labels)
| Inaccurate or incomplete data degrade model performance and reliability | Implement robust preprocessing and imputation pipelines |
7. Limited real-time feasibility and integration with clinical workflows
| Models may not function adequately during real-time CPR; integration into EMS and hospital systems remains problematic. | Optimize computational efficiency |
8. Human–AI interaction challenges
| Users may misunderstand or misuse AI outputs, affecting safety; risk of over-reliance or under-reliance | Training programs for clinicians and lay responders |
9. Regulatory uncertainty and lack of standardized approval pathways
| Inconsistent regulation across regions impedes safe deployment. | Develop clear regulatory pathways (FDA/EMA) |
10. Limited evidence on long-term outcomes and impact on survival
| Most studies evaluate accuracy metrics, not patient-centered outcomes. | Conduct clinical trials and implementation studies |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puticiu, M.; Pop, F.; Butoi, M.A.; Banicioiu-Covei, M.; Rotaru, L.T.; Blaga, T.; Cimpoesu, D. Artificial Intelligence in Cardiopulmonary Resuscitation. Medicina 2025, 61, 2099. https://doi.org/10.3390/medicina61122099
Puticiu M, Pop F, Butoi MA, Banicioiu-Covei M, Rotaru LT, Blaga T, Cimpoesu D. Artificial Intelligence in Cardiopulmonary Resuscitation. Medicina. 2025; 61(12):2099. https://doi.org/10.3390/medicina61122099
Chicago/Turabian StylePuticiu, Monica, Florica Pop, Mihai Alexandru Butoi, Mihai Banicioiu-Covei, Luciana Teodora Rotaru, Teofil Blaga, and Diana Cimpoesu. 2025. "Artificial Intelligence in Cardiopulmonary Resuscitation" Medicina 61, no. 12: 2099. https://doi.org/10.3390/medicina61122099
APA StylePuticiu, M., Pop, F., Butoi, M. A., Banicioiu-Covei, M., Rotaru, L. T., Blaga, T., & Cimpoesu, D. (2025). Artificial Intelligence in Cardiopulmonary Resuscitation. Medicina, 61(12), 2099. https://doi.org/10.3390/medicina61122099









