Comparative Assessment of Point Shear Wave Elastography (pSWE) and Two-Dimensional Shear Wave Elastography (2D-SWE) in the Diagnostic Evaluation of Simple Liver Cysts and Liver Hemangiomas
Abstract
1. Introduction
2. Objective
3. Materials and Methods
3.1. Patients with Liver Hemangiomas-31
3.2. Statistical Analysis
4. Results
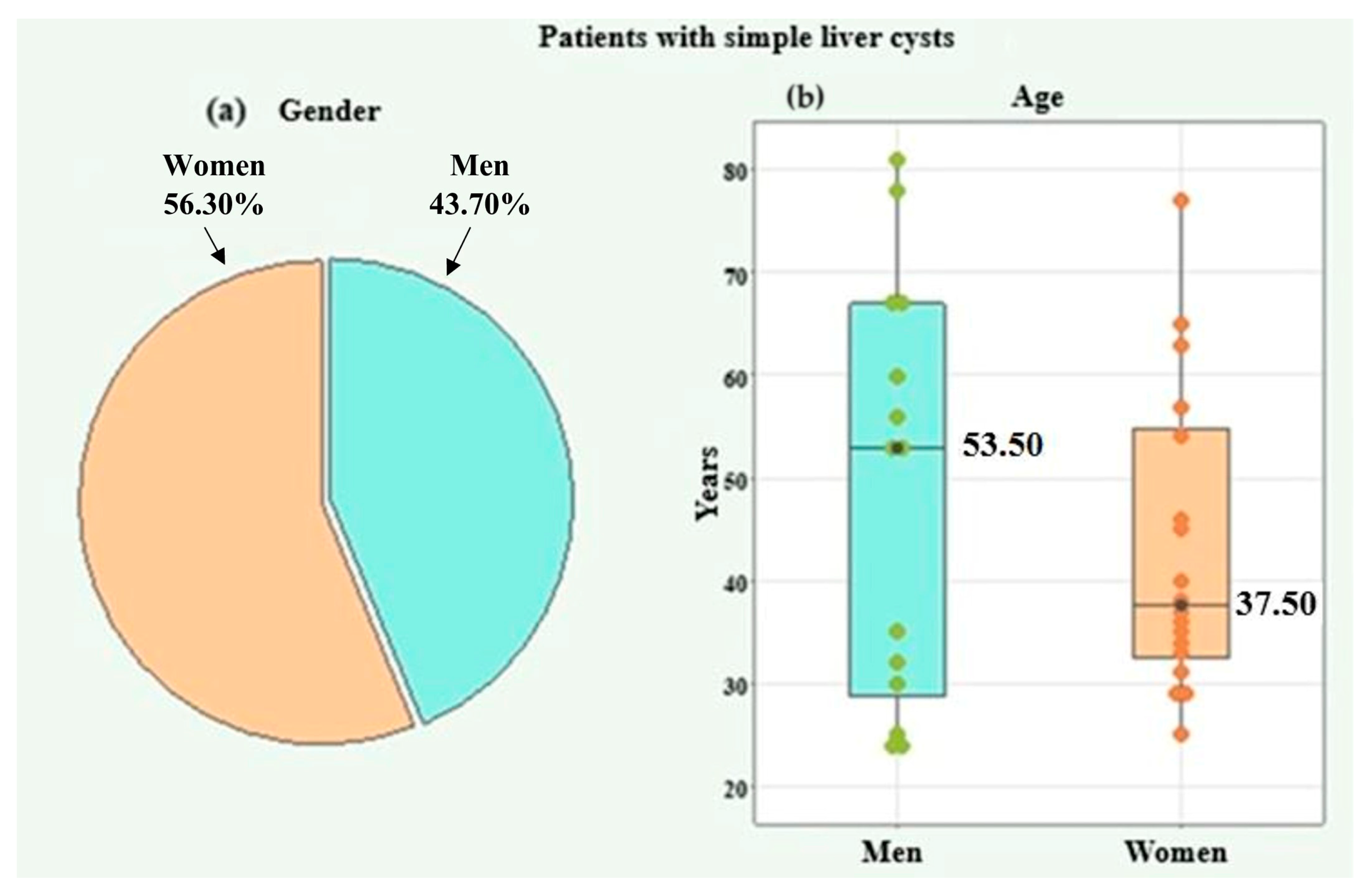
4.1. Information on Patients with Simple Liver Cysts
4.1.1. Basic Information on Patients with Simple Liver Cysts
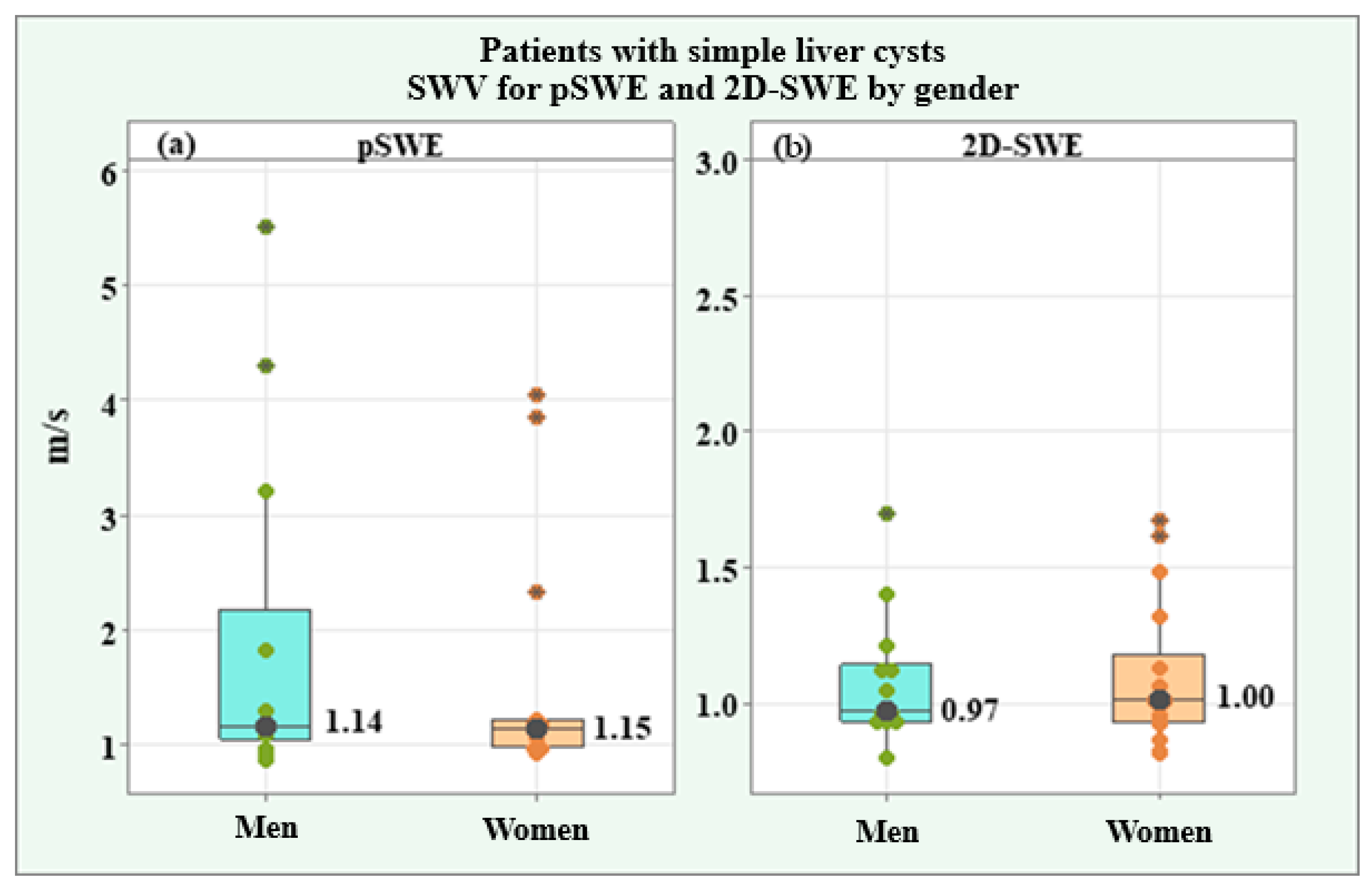
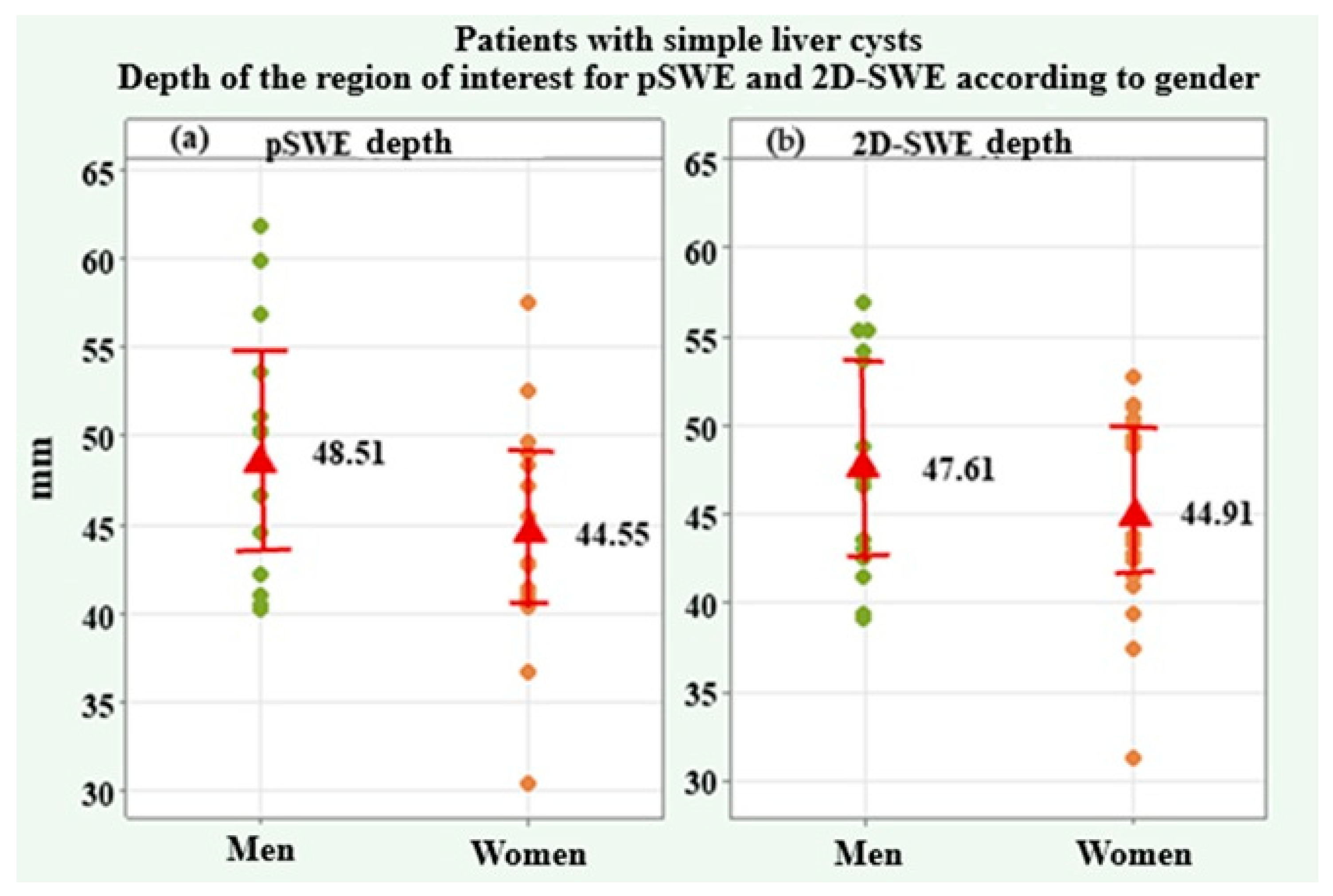
4.1.2. SWV and Depth of the Region of Interest Values for pSWE and 2D-SWE in Patients with Simple Liver Cysts
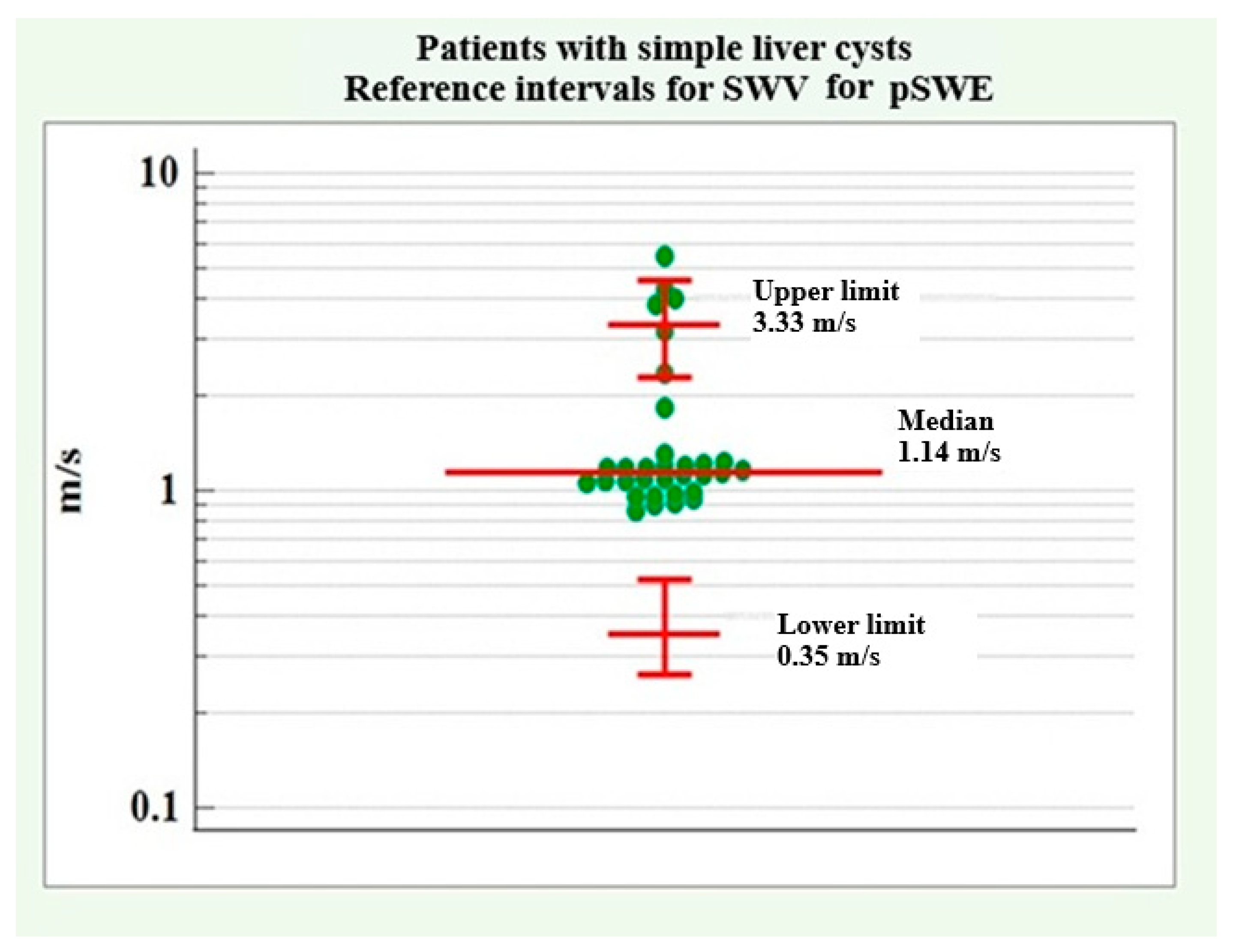
4.1.3. SWV Reference Intervals for pSWE in Patients with Simple Liver Cysts
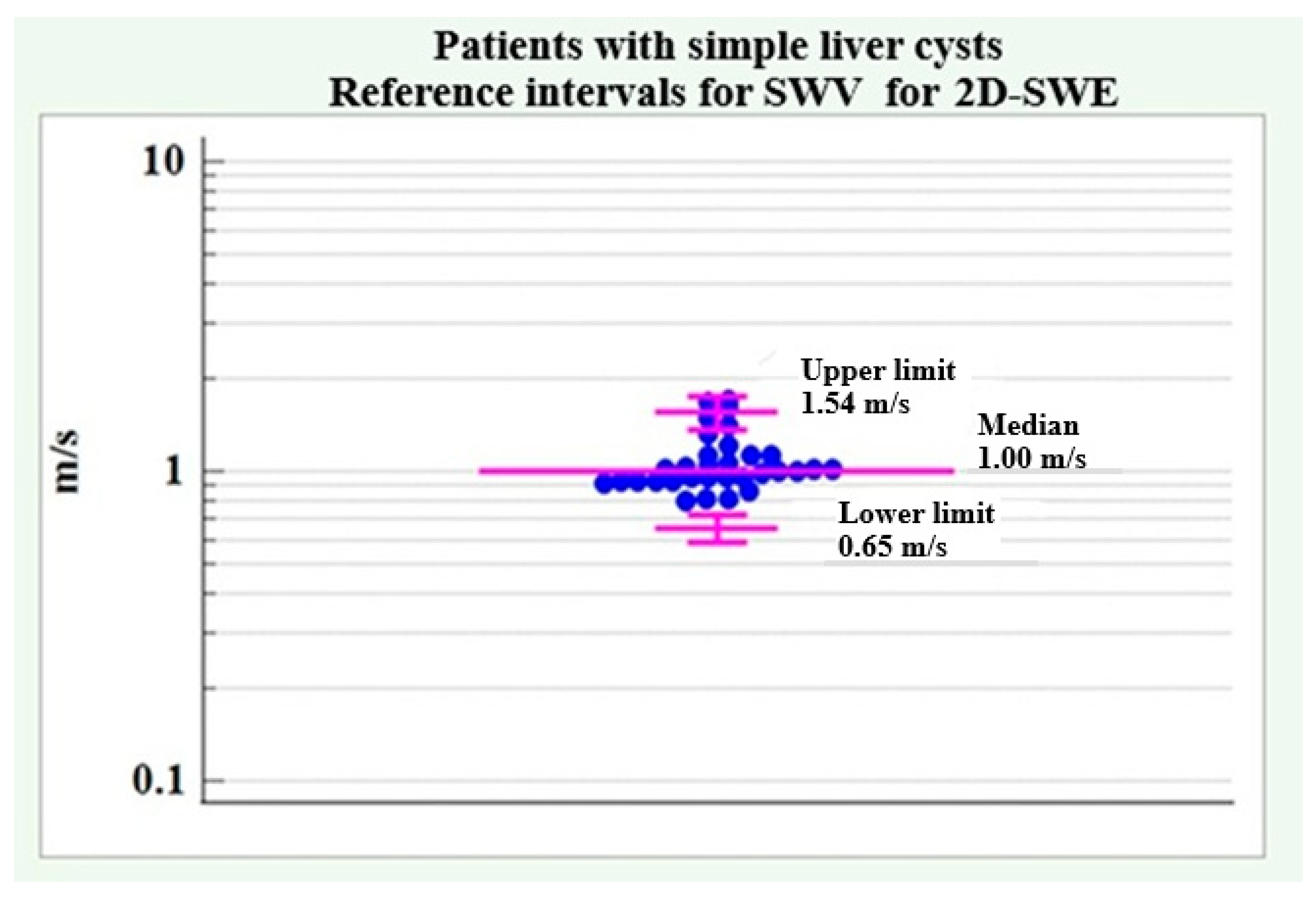
4.1.4. SWV Reference Intervals for 2D-SWE in Patients with Simple Liver Cysts
4.1.5. Summary of the Main Trends Regarding Patients with Simple Liver Cysts
- Demographic and clinical data for patients with simple liver cysts showed significant differences between men and women regarding:
- -
- GG with significantly higher values in men compared with women.
- -
- Alcohol use and smoking, with a significantly higher relative proportion in male patients. The results are summarized in Table 5.
- No significant difference was found between the two genders regarding the SWV values for pSWE and 2D-SWE in patients with simple liver cysts.
- The following reference ranges for SWV for pSWE and 2D-SWE were determined for patients with simple liver cysts. The results are summarized in Table 6.
4.2. Information on Patients with Liver Hemangiomas
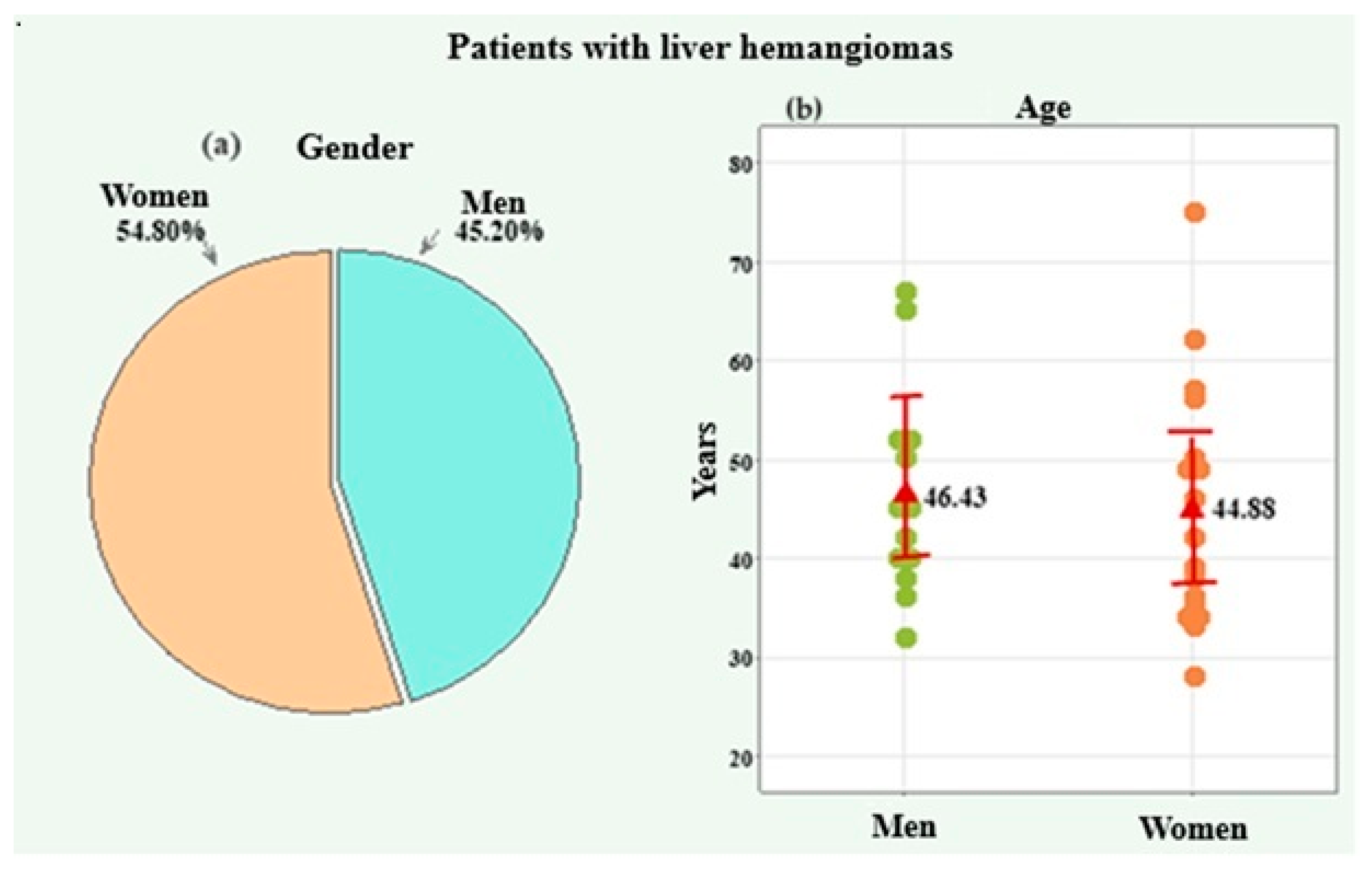
4.2.1. Background Information on Patients with Liver Hemangiomas
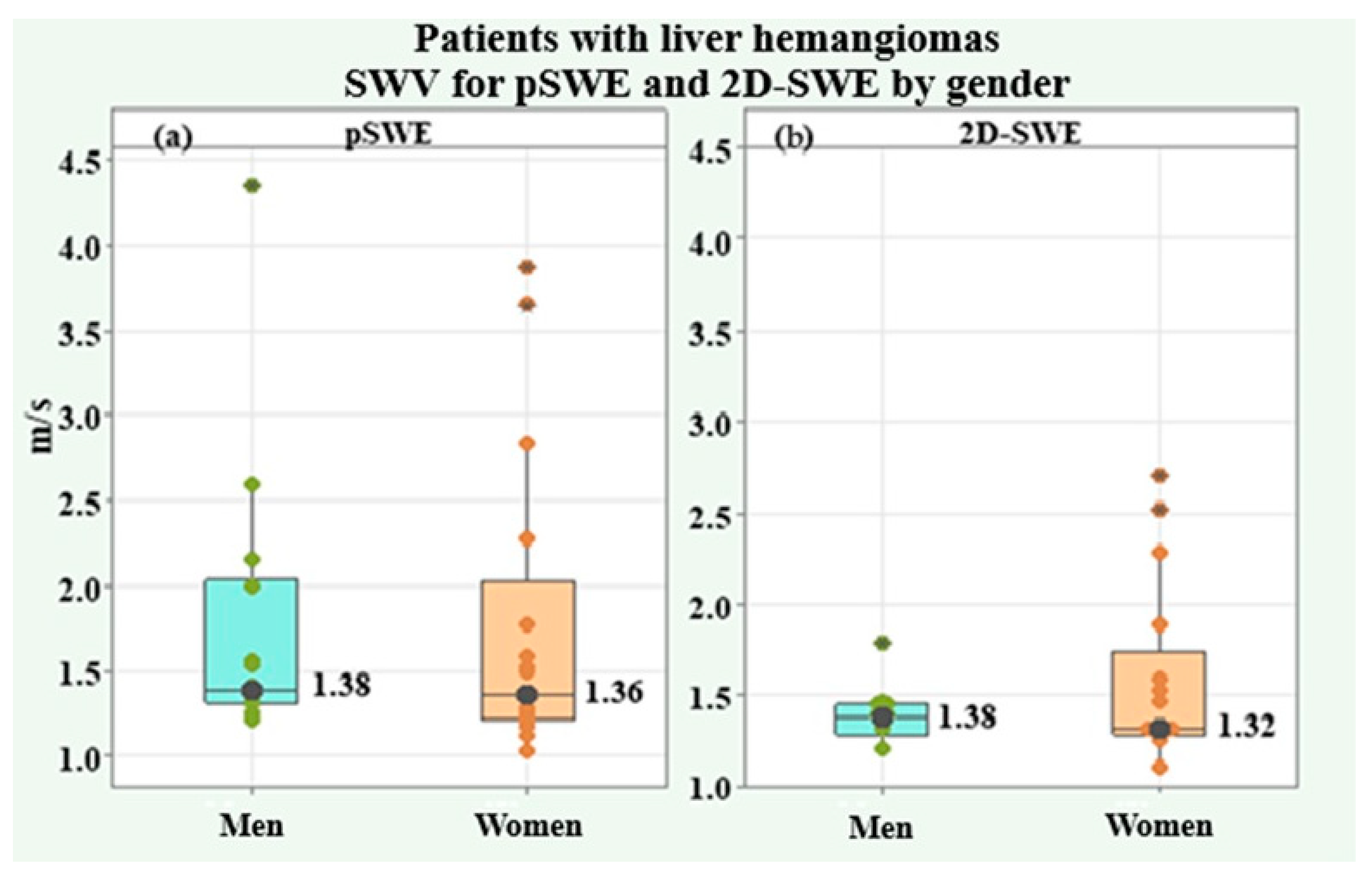
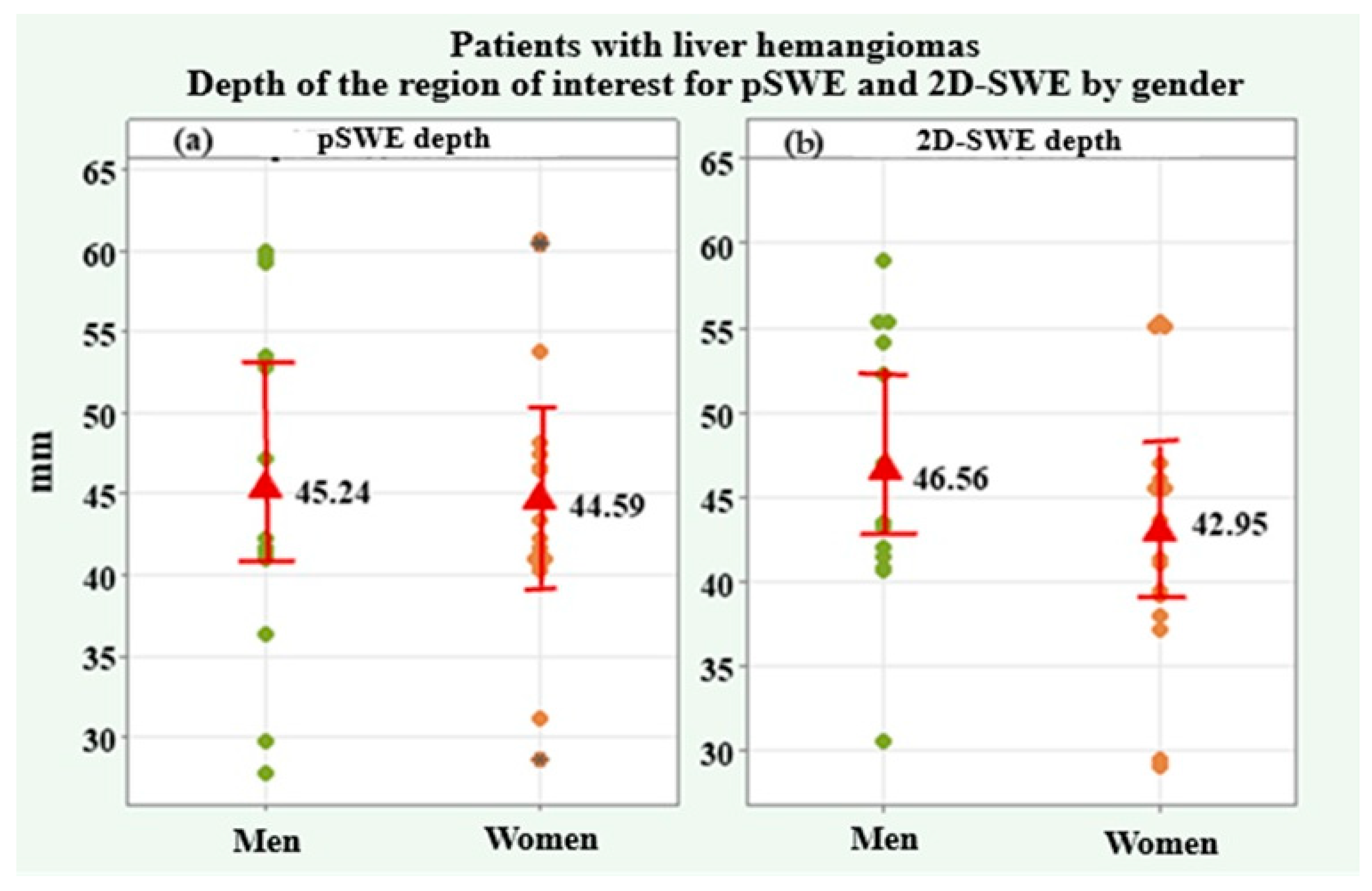
4.2.2. SWV and Depth of the Region of Interest Values for pSWE and 2D-SWE in Patients with Liver Hemangiomas
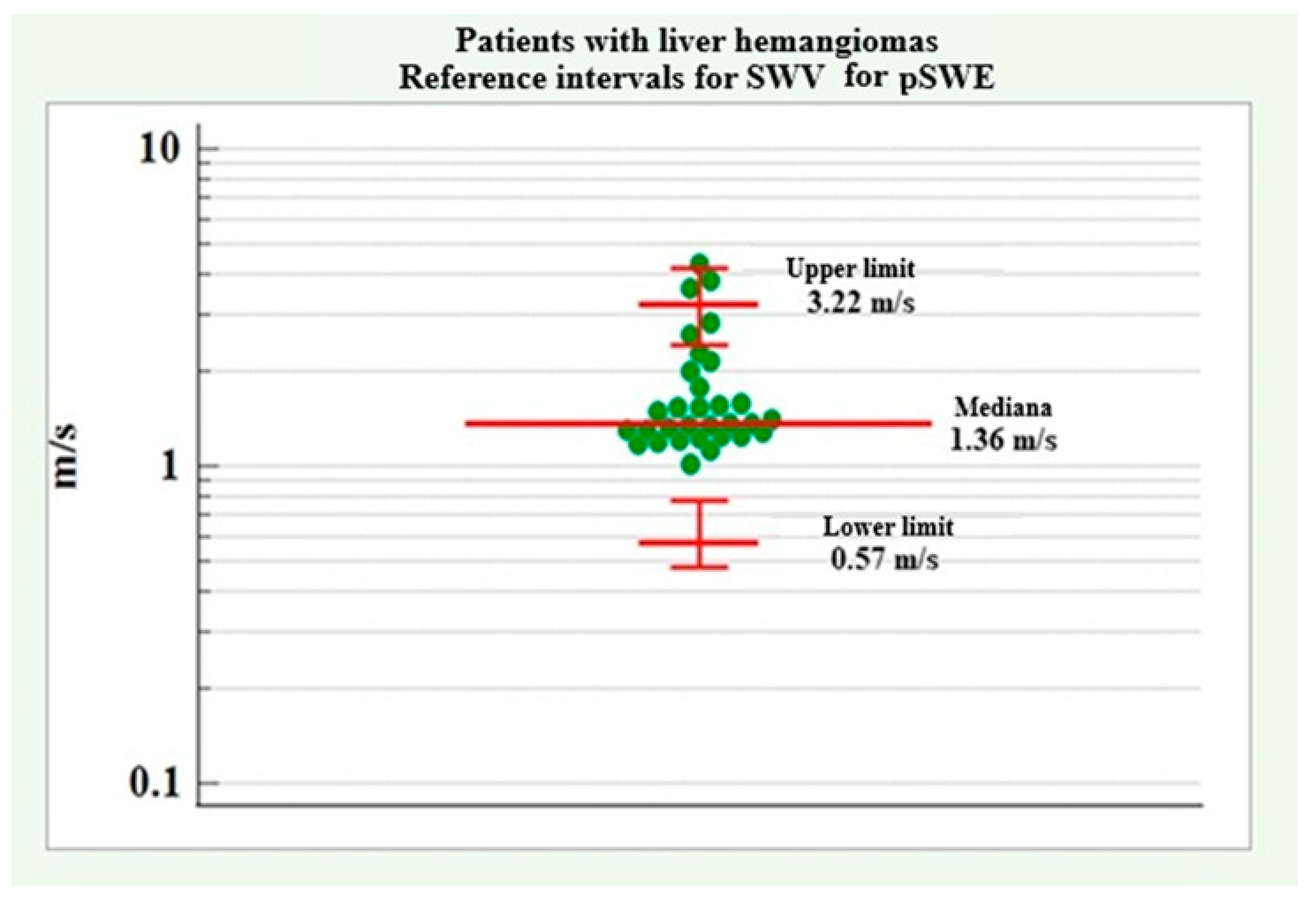
4.2.3. Reference Intervals of SWV for pSWE in Patients with Liver Hemangiomas
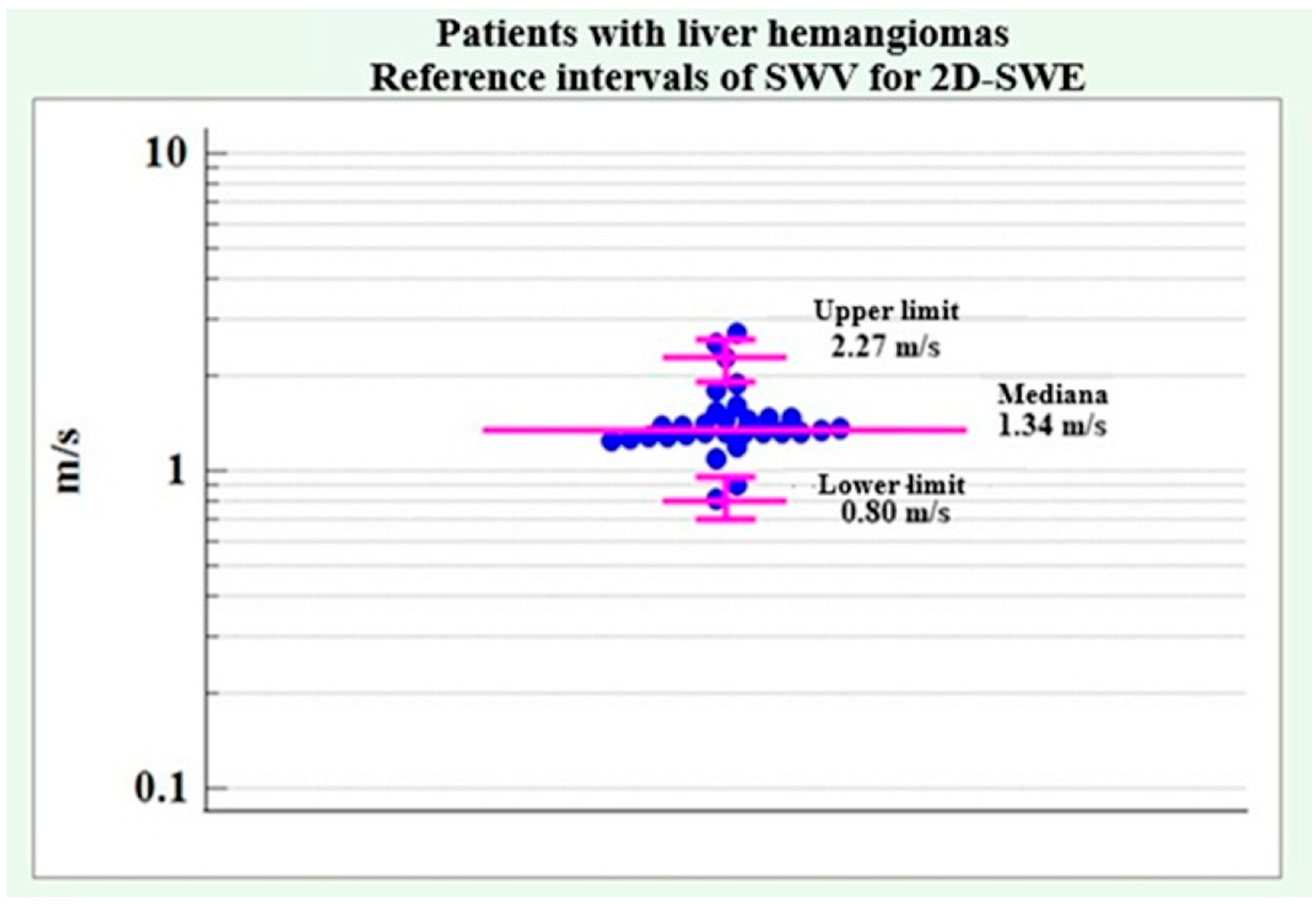
4.2.4. SWV Reference Intervals for 2D-SWE in Patients with Liver Hemangiomas
4.2.5. Summary of Main Trends Regarding Patients with Liver Hemangiomas
- Demographic and clinical data for patients with liver hemangiomas did not show any significant differences between men and women, except for alcohol consumption, which showed a significantly higher relative proportion in male patients. The results are summarized in Table 9.
- No significant difference was found between the two genders regarding SWV values for pSWE and 2D-SWE in patients with liver hemangiomas.
- The following reference ranges of SWV for pSWE and 2D-SWE were determined in patients with liver hemangiomas. The results are summarized in Table 10.
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| pSWE | Point shear wave elastography |
| 2D-SWE | Two-dimensional shear wave elastography |
References
- Doyley, M.M.; Parker, K.J. Elastography: General Principles and Clincial Applications. Ultrasound Clin. 2014, 9, 1–11. [Google Scholar] [CrossRef]
- Garra, B. Elastography history principles and technique comparisson. Abdom. Radiol. 2015, 40, 680–697. [Google Scholar] [CrossRef]
- Dietrich, C.F.; Bamber, J.; Berzigotti, A.; Bota, S.; Cantisani, V.; Castera, L.; Cosgrove, D.; Ferraioli, G.; Friedrich-Rust, M.; Gilja, O.H.; et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Long Version). Ultraschall Med. 2017, 38, e16–e47. [Google Scholar] [CrossRef] [PubMed]
- Gennisson, J.L.; Deffieux, T.; Fink, M.; Tanter, M. Ultrasound elastography: Principles and techniques. Diagn. Interv. Imaging 2013, 94, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Bamber, J.; Cosgrove, D.; Dietrich, C.F.; Fromageau, J.; Bojunga, J.; Calliada, F.; Piscaglia, F. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: Basic principles and technology. Ultraschall Med.-Eur. J. Ultrasound 2013, 34, 169–184. [Google Scholar] [CrossRef]
- Tang, A.; Cloutier, G.; Szeverenyi, N.M.; Sirlin, C.B. Ultrasound Elastography and MR Elastography for Assessing Liver Fibrosis: Part 1, Principles and Techniques. Am. J. Roentgenol. 2015, 205, 22–32. [Google Scholar] [CrossRef]
- Bruni, A.; Dell’Anna, G.; Samanta, J.; Fanizza, J.; Mandarino, F.V.; Dhar, J.; Facciorusso, A.; Annese, V.; Massironi, S.; Malesci, A.; et al. Advances in Endo-Hepatology: The Role of Endoscopic Ultrasound in the Management of Portal Hypertension. Diagnostics 2025, 15, 967. [Google Scholar] [CrossRef]
- Gheonea, D.I.; Saftoiu, A.; Ciurea, T.; Gorunescu, F.; Iordache, S.; Popescu, G.L.; Belciug, S.; Gorunescu, M.; Sandulescu, L. Real-time sonoelastography in the diagnosis of diffuse liver diseases. World J. Gastroenterol. 2010, 16, 1720–1726. [Google Scholar] [CrossRef] [PubMed]
- Gheorghe, L.; Iacob, S.; Gheorghe, C. Real-time sonoelastography-a new application in the field of liver disease. J. Gastrointestin. Liver Dis. 2008, 17, 469–474. [Google Scholar]
- Kapoor, A.; Kapoor, A.; Mahajan, G.; Sidhu, B.S.; Lakhanpal, V.P. Real-time elastography in differentiating metastatic from nonmetastatic liver nodules. Ultrasound Med. Biol. 2011, 37, 207–213. [Google Scholar] [CrossRef]
- Tohno, E.; Ueno, E. Current improvements in breast ultrasound, with a special focus on elastography. Breast Cancer 2008, 15, 200–204. [Google Scholar] [CrossRef]
- Itoh, A.; Ueno, E.; Tohno, E.; Kamma, H.; Takahashi, H.; Shiina, T.; Yamakawa, M.; Matsumura, T. Breast disease: Clinical application of US elastography for diagnosis. Radiology 2006, 239, 341–350. [Google Scholar] [CrossRef]
- Cepeha, C.M.; Borlea, A.; Paul, C.; Velea, I.; Stoian, D. Shear-Wave Elastography in Diffuse Thyroid Diseases. In Elastography—Applications in Clinical Medicine; InTech Open: London, UK, 2022; p. 197. [Google Scholar] [CrossRef]
- Uchida, H.; Hirooka, Y.; Itoh, A.; Kawashima, H.; Hara, K.; Nonogaki, K.; Kasugai, T.; Ohno, E.; Ohmiya, N.; Niwa, Y.; et al. Feasibility of tissue elastography using transcutaneous ultrasonography for the diagnosis of pancreatic diseases. Pancreas 2009, 38, 17–22. [Google Scholar] [CrossRef]
- Kawada, N.; Tanaka, S.; Uehara, H.; Takakura, R.; Katayama, K.; Fukuda, J.; Matsuno, N.; Takenaka, A.; Ishikawa, O. Feasibility of second-generation transabdominal ultrasound-elastography to evaluate solid pancreatic tumors: Preliminary report of 36 cases. Pancreas 2012, 41, 978–980. [Google Scholar] [CrossRef]
- Tsutsumi, M.; Miyagawa, T.; Matsumura, T.; Kawazoe, N.; Ishikawa, S.; Shimokama, T.; Shiina, T.; Miyanaga, N.; Akaza, H. The impact of real-timetissue elasticity imaging (elastography) on the detection of prostate cancer: Clinicopathological analysis. Int. J. Clin. Oncol. 2007, 12, 250–255. [Google Scholar] [CrossRef]
- Săftoiu, A.; Vilmann, P.; Hassan, H.; Gorunescu, F. Analysis of endoscopic ultrasound elastography used for characterisation and differentiation of benign and malignant lymph nodes. Ultraschall Med. 2006, 27, 535–542. [Google Scholar] [CrossRef]
- Ślósarz, D.; Poniewierka, E.; Neubauer, K.; Kempiński, R. Ultrasound elastography in the assessment of the intestinal changes in inflammatory bowel disease: Systematic review. J. Clin. Med. 2021, 10, 4044. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, O.; Sakuma, J.; Kawakami, Y.; Suzuki, K.; Fukubayashi, T. Effect of exercise-induced muscle damage on muscle hardness evaluated by ultrasound real-time tissue elastography. Springerplus 2015, 4, 308. [Google Scholar] [CrossRef]
- Bota, S.; Herkner, H.; Sporea, I.; Salzl, P.; Sirli, R.; Neghina, A.M.; Peck-Radosavljevic, M. Meta-analysis: ARFI elastography versus transient elastography for the evaluation of liver fibrosis. Liver Int. 2013, 33, 113847. [Google Scholar] [CrossRef] [PubMed]
- Bruno, C.; Minniti, S.; Bucci, A.; Pozzi Mucelli, R. ARFI: From basic principles to clinical applications in diffuse chronic disease—A review. Insights Imaging 2016, 7, 735–746. [Google Scholar] [CrossRef] [PubMed]
- Iglesias-Garcia, J.; Domínguez-Muñoz, J.E.; Castiñeira-Alvariño, M.; Luaces-Regueira, M.; Lariño-Noia, J. Quantitative elastography associated with endoscopic ultrasound for the diagnosis of chronic pancreatitis. J. Endosc. 2013, 45, 781–788. [Google Scholar] [CrossRef]
- Oglat, A.A.; Dheyab, M.A. Performance Evaluation of Ultrasonic Imaging System (Part I). J. Med. Ultrasound 2021, 29, 258–263. [Google Scholar] [CrossRef]
- Sigrist, R.M.S.; Liau, J.; Kaffas, A.E.; Chammas, M.C.; Willmann, J.K. Ultrasound Elastography: Review of Techniques and Clinical Applications. Theranostics 2017, 7, 1303–1329. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Lee, J.Y.; Han, J.K.; Choi, B.I. Acoustic radiation force impulse elastography for the evaluation of focal solid hepatic lesions: Preliminary findings. Ultrasound Med. Biol. 2010, 36, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.H.; Wang, S.J.; Xu, H.X.; Sun, L.P.; Zhang, Y.F.; Xu, J.M.; Wu, J.; Fu, H.J.; Xu, X.H. Differentiation of benign and malignant focal liver lesions: Value of virtual touch tissue quantification of acoustic radiation force impulse elastography. Med. Oncol. 2015, 32, 68. [Google Scholar] [CrossRef]
- Heide, R.; Strobel, D.; Bernatik, T.; Goertz, R.S. Characterization of focal liver lesions (FLL) with acoustic radiation force impulse (ARFI) elastometry. Ultraschall Med. 2010, 31, 405–409. [Google Scholar] [CrossRef]
- Choi, B.Y.; Nguyen, M.H. The diagnosis and management of benign hepatic tumors. J. Clin. Gastroenterol. 2005, 39, 401–412. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Wilson, S.R. Differentiation of benign from malignant liver masses with Acoustic Radiation Force Impulse technique. Ultrasound Q. 2011, 27, 217–223. [Google Scholar] [CrossRef]
- Nagolu, H.; Kattoju, S.; Natesan, C.; Krishnakumar, M.; Kumar, S. Role of acoustic radiation forceimpulse elastography in the characterization of focal solid hepaticlesions. J. Clin. Imaging Sci. 2018, 8, 5. [Google Scholar] [CrossRef]
| Values | Total (n = 63) | Male (n = 28) | Female (n = 35) | p |
BMI
| 23.93 (3.50) | 23.07 (3.60) | 24.65 (3.34) | 0.191 t |
GGT
| 38.00 (35.50) | 51.00 (34.77) | 26.00 (29.25) | 0.045 U |
Total bilirubin
| 15.05 (6.10) | 17.45 (8.20) | 14.45 (5.27) | 0.193 U |
Direct bilirubin
| 5.40 (2.15) | 5.95 (2.59) | 4.97 (1.68) | 0.210 t |
ALP
| 58.00 (38.75) | 57.00 (26.75) | 73.50 (38.00) | 0.135 U |
ASAT
| 21.00 (14.75) | 19.50 (13.25) | 22.00 (15.00) | 0.251 U |
ALAT
| 22.50 (18.50) | 27.50 (22.50) | 20.00 (15.50) | 0.283 U |
Cross-sectional area of lesion (mm)
| 29.00 (16.25) | 29.00 (25.25) | 30.00 (12.00) | 0.694 U |
Longitudinal section of lesion (mm)
| 31.50 (14.50) | 32.38 (12.40) | 33.62 (11.63) | 0.750 U |
| Alcohol n (%) | 15 (46.90%) | 12 (85.70%) | 3 (16.70%) | <0.001 f |
| Smoking n (%) | 12 (37.50%) | 10 (71.40%) | 2 (11.10%) | 0.001 f |
| Values | Total (n = 63) | Male (n = 28) | Female (n = 35) | p |
pSWE SWV (m/s)
| 1.14 (0.27) 0.86–5.51 | 1.15 (1.13) 0.86–5.51 | 1.14 (0.23) 0.92–4.04 | 0.613 U |
pSWE depth (mm)
| 46.28 (7.10) 30.34–61.86 | 48.51 (7.50) 40.14–61.86 | 44.55 (6.44) 30.34–57.57 | 0.119 t |
2D-SWE SWV (m/s)
| 1.00 (0.19) 0.80–1.70 | 0.97 (0.21) 0.80–1.70 | 1.00 (0.25) 0.81–1.67 | 0.837 U |
2-D-SWE depth (mm)
| 46.09 (6.07) 31.30–56.90 | 47.61 (6.37) 39.10–56.90 | 44.91 (5.73) 31.30–52.70 | 0.218 t |
| Back-Transformed After Logarithmic Transformation | |
|---|---|
| Number of cases | n = 32 |
| Lower reference limit | 0.86 |
| Upper reference limit | 5.51 |
| Mean | 1.38 |
| Median | 1.14 |
| Shapiro–Wilk test | p = 0.11 |
| Robust method | |
| Lower limit 90% Confidence interval (90% CI) | 0.35 (0.26–0.52) |
| Upper limit 90% Confidence interval (90% CI) | 3.33 (2.28–4.61) |
| Back-Transformed After Logarithmic Transformation | |
|---|---|
| Number of cases | n = 32 |
| Lower reference limit | 0.80 |
| Upper reference limit | 1.70 |
| Mean | 1.06 |
| Median | 1.00 |
| Shapiro–Wilk test | p = 0.32 |
| Robust method | |
| Lower limit 95% Confidence interval (95% CI) | 0.65 (0.59–0.72) |
| Upper limit 95% Confidence interval (95% CI) | 1.54 (1.35–1.75) |
| Male | Female | |
|---|---|---|
| Alcohol | 85.70% | 16.70% |
| Smoking | 71.40% | 11.10% |
| SWV | Median | Upper Limit | Lower Limit |
|---|---|---|---|
| pSWE | 1.14 m/s | 3.33 m/s | 0.35 m/s |
| 2D-SWE | 1.00 m/s | 1.54 m/s | 0.65 m/s |
| Values | Total (n = 63) | Male (n = 28) | Female (n = 35) | p |
BMI
| 22.90 (3.80) | 23.45 (5.20) | 22.80 (4.00) | 0.246 U |
GGT
| 23.00 (15.00) | 23.50 (16.25) | 22.00 (15.50) | 0.769 U |
Total bilirubin
| 13.82 (3.08) | 13.08 (2.85) | 14.42 (3.22) | 0.234 t |
Direct bilirubin
| 4.20 (1.52) | 4.27 (1.48) | 4.15 (1.59) | 0.834 t |
ALP
| 77.00 (23.00) | 76.00 (34.00) | 83.00 (18.50) | 0.377 U |
ASAT
| 25.00 (13.00) | 29.50 (10.50) | 21.00 (10.00) | 0.044 U |
ALAT
| 22.00 (15.00) | 21.50 (11.00) | 23.00 (17.00) | 0.769 U |
Cross-sectional area of lesion (mm)
| 31.43 (12.56) | 29.93 (10.23) | 31.24 (12.54) | 0.756 t |
Longitudinal section of lesion (mm)
| 33.07 (11.90) | 30.55 (12.29) | 36.04 (13.59) | 0.252 t |
| Alcohol n (%) | 14 (45.20%) | 10 (71.40%) | 4 (23.50%) | 0.012 f |
| Smoking n (%) | 14 (45.20%) | 7 (50.00%) | 7 (41.20%) | 0.725 f |
| Values | Total (n = 63) | Male (n = 28) | Female (n = 35) | p |
pSWE SWV (m/s)
| 1.36 (0.74) 1.02–4.35 | 1.38 (0.72) 1.21–4.35 | 1.36 (0.81) 1.02–3.87 | 0.544 U |
pSWE depth (mm)
| 44.89 (9.26) 27.80–60.60 | 45.24 (10.52) 27.80–59.96 | 44.59 (8.40) 28.52–60.60 | 0.850 t |
2D-SWE SWV (m/s)
| 1.34 (0.19) 0.82–2.70 | 1.38 (0.17) 0.82–1.79 | 1.32 (0.46) 1.10–2.70 | 0.653 U |
2-D-SWE depth (mm)
| 44.58 (7.93) 29.00–59.00 | 46.56 (7.80) 30.50–59.00 | 42.95 (7.71) 29.00–55.30 | 0.208 t |
| Male | Female | |
|---|---|---|
| Alcohol | 71.40% | 23.50% |
| SWV | Median | Upper Limit | Lower Limit |
|---|---|---|---|
| pSWE | 1.36 m/s | 3.22 m/s | 0.57 m/s |
| 2D-SWE | 1.34 m/s | 2.27 m/s | 0.80 m/s |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nacheva-Georgieva, E.L.; Doykov, D.I.; Hristov, B.K.; Stanchev, D.I.; Todorov, I.S.; Georgiev, Z.G.; Doykova, K.A.; Valova, S.E.; Kraev, K.I.; Uchikov, P.A. Comparative Assessment of Point Shear Wave Elastography (pSWE) and Two-Dimensional Shear Wave Elastography (2D-SWE) in the Diagnostic Evaluation of Simple Liver Cysts and Liver Hemangiomas. Medicina 2025, 61, 1940. https://doi.org/10.3390/medicina61111940
Nacheva-Georgieva EL, Doykov DI, Hristov BK, Stanchev DI, Todorov IS, Georgiev ZG, Doykova KA, Valova SE, Kraev KI, Uchikov PA. Comparative Assessment of Point Shear Wave Elastography (pSWE) and Two-Dimensional Shear Wave Elastography (2D-SWE) in the Diagnostic Evaluation of Simple Liver Cysts and Liver Hemangiomas. Medicina. 2025; 61(11):1940. https://doi.org/10.3390/medicina61111940
Chicago/Turabian StyleNacheva-Georgieva, Emiliya Lyubomirova, Daniel Ilianov Doykov, Bozhidar Krasimirov Hristov, Desislav Ivanov Stanchev, Iliya Stoyanov Todorov, Zhivko Georgiev Georgiev, Katya Angelova Doykova, Siyana Emilova Valova, Krasimir Iliev Kraev, and Petar Angelov Uchikov. 2025. "Comparative Assessment of Point Shear Wave Elastography (pSWE) and Two-Dimensional Shear Wave Elastography (2D-SWE) in the Diagnostic Evaluation of Simple Liver Cysts and Liver Hemangiomas" Medicina 61, no. 11: 1940. https://doi.org/10.3390/medicina61111940
APA StyleNacheva-Georgieva, E. L., Doykov, D. I., Hristov, B. K., Stanchev, D. I., Todorov, I. S., Georgiev, Z. G., Doykova, K. A., Valova, S. E., Kraev, K. I., & Uchikov, P. A. (2025). Comparative Assessment of Point Shear Wave Elastography (pSWE) and Two-Dimensional Shear Wave Elastography (2D-SWE) in the Diagnostic Evaluation of Simple Liver Cysts and Liver Hemangiomas. Medicina, 61(11), 1940. https://doi.org/10.3390/medicina61111940





