Thromboembolic Risk After Total Hip Replacement Versus Hemiarthroplasty in Femoral Neck Fracture Patients: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
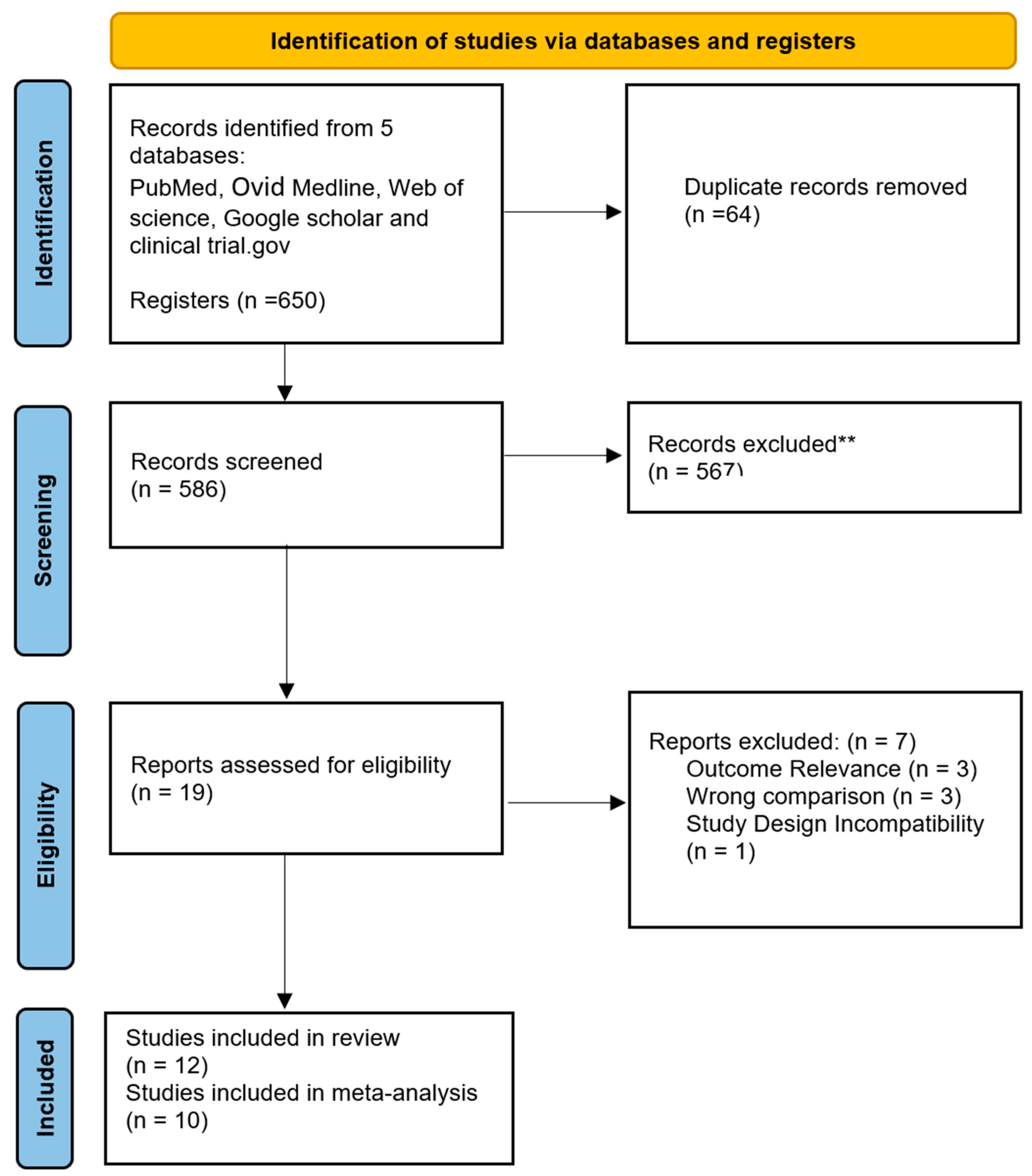
2. Materials and Methods
2.1. Literature Search and Registration
2.2. Study Selection
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. Data Extraction
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Included Studies
3.2. Characteristics of Included Articles
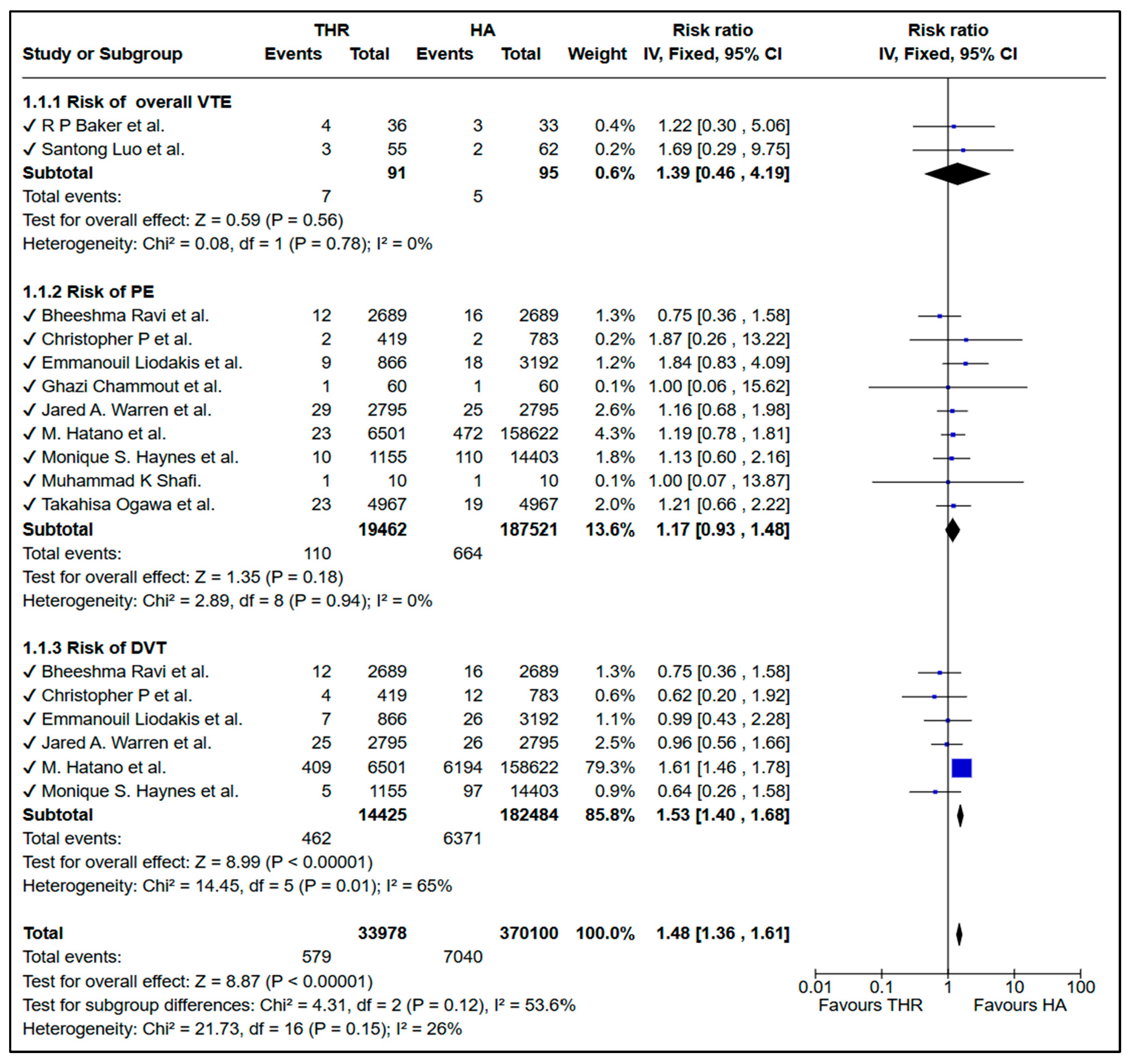
3.3. Risk of VTE Between THR and HA
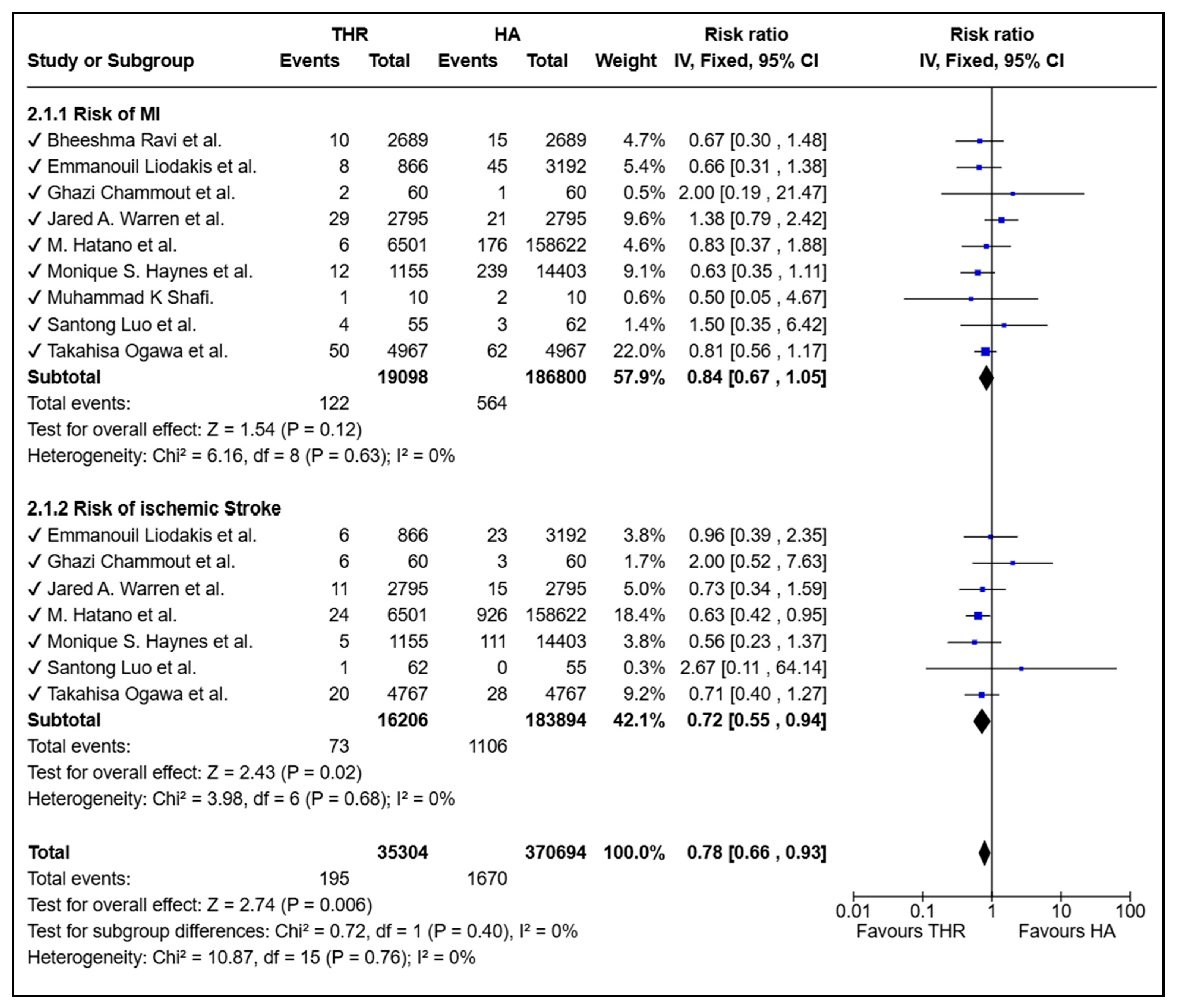
3.4. Risk of Cardiovascular Complications Between THR and HA
3.5. Sensitivity Analysis
3.6. Risk of Bias Assessment
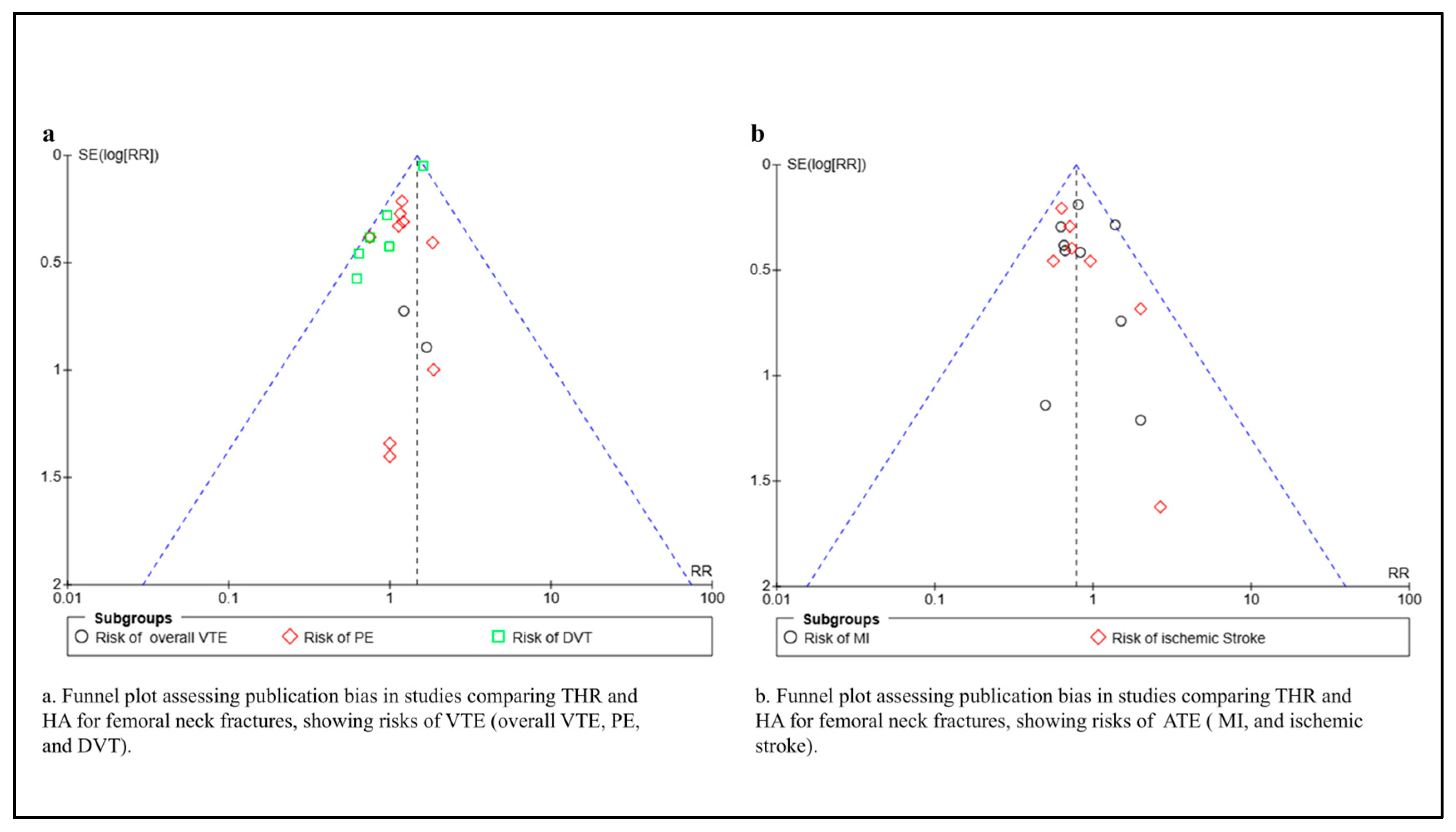
3.7. Publication Bias
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| THR | Total Hip Replacement |
| HA | Hemiarthroplasty |
| VTE | Venous Thromboembolism |
| DVT | Deep Vein Thrombosis |
| PE | Pulmonary Embolism |
| RoB 2 | Risk of Bias 2 (Tool) |
References
- Shehata, S.F.; Altalhiyyah, K.S.; Alqahtani, S.H.; Asiri, A.S.; Alqahtani, F.S.M.; Alfarwan, S.M. Elderly awareness and perception of neck femur fracture in Saudi Arabia. J. Fam. Med. Prim. Care. 2023, 12, 2584–2589. [Google Scholar] [CrossRef]
- Al-Mohrej, O.A.; Alshaalan, F.N.; Aldakhil, S.S.; Rahman, W.A. One-Year Mortality Rates Following Fracture of the Femoral Neck Treated With Hip Arthroplasty in an Aging Saudi Population: A Trauma Center Experience. Geriatr. Orthop. Surg. Rehabil. 2020, 11, 2151459320922473. [Google Scholar] [CrossRef]
- Luo, S.; Qin, W.; Yu, L.; Luo, R.; Liang, W. Total hip arthroplasty versus hemiarthroplasty in the treatment of active elderly patients over 75 years with displaced femoral neck fractures: A retrospective study. BMC Musculoskelet. Disord. 2023, 24, 745. [Google Scholar] [CrossRef] [PubMed]
- Metcalfe, D.; Judge, A.; Perry, D.C.; Gabbe, B.; Zogg, C.K.; Costa, M.L. Total hip arthroplasty versus hemiarthroplasty for independently mobile older adults with intracapsular hip fractures. BMC Musculoskelet. Disord. 2019, 20, 226. [Google Scholar] [CrossRef] [PubMed]
- Voskuijl, T.; Neuhaus, V.; Kinaci, A.; Vrahas, M.; Ring, D. In-Hospital Outcomes after Hemiarthroplasty versus Total Hip Arthroplasty for Isolated Femoral Neck Fractures. Arch. Bone Jt. Surg. 2014, 2, 151–156. [Google Scholar] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Baker, R.P.; Squires, B.; Gargan, M.F.; Bannister, G.C. Total Hip Arthroplasty and Hemiarthroplasty in Mobile, Independent Patients with a Displaced Intracapsular Fracture of the Femoral Neck. J. Bone Jt. Surg. 2006, 88, 2583–2589. [Google Scholar] [CrossRef]
- Miller, C.P.; Buerba, R.A.; Leslie, M.P. Preoperative Factors and Early Complications Associated With Hemiarthroplasty and Total Hip Arthroplasty for Displaced Femoral Neck Fractures. Geriatr. Orthop. Surg. Rehabil. 2014, 5, 73–81. [Google Scholar] [CrossRef]
- Liodakis, E.; Antoniou, J.; Zukor, D.J.; Huk, O.L.; Epure, L.M.; Bergeron, S.G. Major Complications and Transfusion Rates After Hemiarthroplasty and Total Hip Arthroplasty for Femoral Neck Fractures. J. Arthroplast. 2016, 31, 2008–2012. [Google Scholar] [CrossRef]
- Chammout, G.; Kelly-Pettersson, P.; Hedbeck, C.J.; Stark, A.; Mukka, S.; Sköldenberg, O. HOPE-Trial: Hemiarthroplasty Compared with Total Hip Arthroplasty for Displaced Femoral Neck Fractures in Octogenarians. JBJS Open Access 2019, 4, e0059. [Google Scholar] [CrossRef]
- Warren, J.A.; Sundaram, K.; Anis, H.K.; Piuzzi, N.S.; Higuera, C.A.; Kamath, A.F. Total Hip Arthroplasty Outperforms Hemiarthroplasty in Patients Aged 65 Years and Older: A Propensity-Matched Study of Short-Term Outcomes. Geriatr. Orthop. Surg. Rehabil. 2019, 10, 2151459319876854. [Google Scholar] [CrossRef] [PubMed]
- Ravi, B.; Pincus, D.; Khan, H.; Wasserstein, D.; Jenkinson, R.; Kreder, H.J. Comparing Complications and Costs of Total Hip Arthroplasty and Hemiarthroplasty for Femoral Neck Fractures. J. Bone Jt. Surg. 2019, 101, 572–579. [Google Scholar] [CrossRef]
- Haynes, M.S.; Ondeck, N.T.; Ottesen, T.D.; Malpani, R.; Rubin, L.E.; Grauer, J.N. Perioperative Outcomes of Hemiarthroplasty Versus Total Hip Arthroplasty for Geriatric Hip Fracture: The Importance of Studying Matched Populations. J. Arthroplasty 2020, 35, 3188–3194. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Yoshii, T.; Moriwaki, M.; Morishita, S.; Oh, Y.; Miyatake, K.; Nazarian, A.; Shiba, K.; Okawa, A.; Fushimi, K.; et al. Association between Hemiarthroplasty vs. Total Hip Arthroplasty and Major Surgical Complications among Patients with Femoral Neck Fracture. J. Clin. Med. 2020, 9, 3203. [Google Scholar] [CrossRef]
- Suarez, J.C.; Arguelles, W.; Saxena, A.; Rivera, P.; Parris, D.; Veledar, E. Hemiarthroplasty vs. Total Hip Arthroplasty for Femoral Neck Fractures: 2010–2017 Trends in Complication Rates. J. Arthroplast. 2020, 35, S262–S267. [Google Scholar] [CrossRef]
- Shafi, M.K.; Buzdar, M.I.; Mahmood, S.; Khan, M.A.; Mubeen, F. Comparison of Hemiarthroplasty and Total Hip Arthroplasty in Elderly Patients with Displaced Femoral Neck Fractures. Pak. J. Med. Health Sci. 2022, 16, 547–549. [Google Scholar] [CrossRef]
- Hatano, M.; Sasabuchi, Y.; Isogai, T.; Ishikura, H.; Tanaka, T.; Tanaka, S.; Yasunaga, H. Increased early complications after total hip arthroplasty compared with hemiarthroplasty in older adults with a femoral neck fracture. Bone Jt. J. 2024, 106-B, 986–993. [Google Scholar] [CrossRef]
- Peng, W.; Bi, N.; Zheng, J.; Xi, N. Does total hip arthroplasty provide better outcomes than hemiarthroplasty for the femoral neck fracture? A systematic review and meta-analysis. Chin. J. Traumatol. 2020, 23, 356–362. [Google Scholar] [CrossRef]
- Li, X.; Luo, J. Hemiarthroplasty compared to total hip arthroplasty for the treatment of femoral neck fractures: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2021, 16, 172. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Wang, Y.; Chen, J. Total Hip Arthroplasty Versus Hemiarthroplasty for Displaced Femoral Neck Fractures: Meta-analysis of Randomized Trials. Clin. Orthop. Relat. Res. 2012, 470, 2235–2243. [Google Scholar] [CrossRef] [PubMed]
- Blomfeldt, R.; Törnkvist, H.; Eriksson, K.; Söderqvist, A.; Ponzer, S.; Tidermark, J. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint. Surg. Br. 2007, 89-B, 160–165. [Google Scholar] [CrossRef] [PubMed]
| Study (Author, Year) | Study Design | Sample Size (THR/HA) | Age Range | Main Outcomes | VTE Risk |
|---|---|---|---|---|---|
| Baker et al. (2006) [9] | Randomized Controlled Trial (RCT) | (40/41) | >60 years | Better hip scores and walking in THR; more acetabular erosion in HA | PE and DVT RISK is higher in HA group |
| Miller et al. [10] (2014) | Retrospective cohort | (419/783) | >50 years | Shorter hospital stays; minor complications lower in THR | No major difference |
| Liodakis et al. [11] (2016) | Retrospective cohort | (866/3192) | ≥70 years | No major complications difference; higher transfusion in THR | No major difference |
| Chammout et al. [12] (2019) | Prospective Randomized Controlled Trial (RCT) | (60/60) | ≥80 years | No difference in hip function, QoL, or complications | No major difference |
| Warren et al. [13] (2019) | Retrospective matched cohort | (2795/2795) | ≥65 years | Lower mortality, more home discharges in THR | No major difference |
| Ravi et al. [14] (2019) | Retrospective matched cohort | (2689/2689) | ≥60 years | Lower revision rate, higher dislocation in THR | No major difference |
| Haynes et al. [15] (2020) | Retrospective cohort | (1155 /14,403) | ≥70 years | 30-day outcomes (mortality, transfusion) | No major difference |
| Ogawa et al. [16] (2020) | Retrospective matched cohort | (4967/4967) | ≥60 years | Higher dislocation and revision in THR | No major difference |
| Suarez et al. [17] (2020) | Retrospective cohort | (4124/12089) | ≥50 years | THR has had fewer major complications recently | No major difference |
| Shafi et al. [18] (2022) | Retrospective cohort | (10/10) | >60 years | Fewer complications in THR | No major difference |
| Luo et al. [3] (2023) | Retrospective cohort | (55/62) | >75 years | Better 5-year function and QoL in THR | No major difference |
| Hatano et al. [19] (2024) | Retrospective cohort | (6501/158,622) | >60 years | Lower mortality in THR | Higher DVT in THR |
| Study | Selection | Comparability | Outcome | Total (9/9) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Representative of the Exposed Cohort | Selection of the External Control | Ascertainment of Exposure | Outcome of Interest Does Not Present at the Start of the Study | Comparability of Cohorts | Assessment of Outcomes | Sufficient Follow-Up Time | Adequacy of Follow-Up | |||
| Main Factor | Additional Factor | |||||||||
| Miller et al. 2015 [10] | * | * | * | * | * | * | * | * | 0 | (8/9) |
| Liodakis et al. 2016 [11] | * | * | * | * | * | * | * | 0 | * | (8/9) |
| Ravi et al. 2019 [14] | * | * | * | * | * | * | * | * | * | (9/9) |
| Warren et al. 2019 [13] | * | * | * | * | * | * | * | * | * | (9/9) |
| Ogawa et al. 2020 [16] | * | * | * | * | * | * | * | * | * | (9/9) |
| Suarez et al. 2020 [17] | * | * | * | * | * | * | * | 0 | * | (8/9) |
| Haynes et al. 2020 [15] | * | * | * | * | * | * | * | * | * | (9/9) |
| Shafi et al. 2022 [18] | 0 | * | * | * | * | 0 | * | * | * | (7/9) |
| Luo et al. 2023 [3] | * | * | * | * | * | 0 | * | * | 0 | (7/9) |
| Hatano et al. 2024 [19] | * | * | * | * | * | * | * | * | * | (9/9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hakami, I.A.; Altammar, M.A.; Alaklabi, S.A.; Alotaibi, M.M.; Almunyif, S.N.; Alshuwaier, M.I.; Alobaysi, S.T.; Aldalbahi, S.S.; Alotaibi, A.H.; Alotaibi, M.M.; et al. Thromboembolic Risk After Total Hip Replacement Versus Hemiarthroplasty in Femoral Neck Fracture Patients: A Systematic Review and Meta-Analysis. Medicina 2025, 61, 1929. https://doi.org/10.3390/medicina61111929
Hakami IA, Altammar MA, Alaklabi SA, Alotaibi MM, Almunyif SN, Alshuwaier MI, Alobaysi ST, Aldalbahi SS, Alotaibi AH, Alotaibi MM, et al. Thromboembolic Risk After Total Hip Replacement Versus Hemiarthroplasty in Femoral Neck Fracture Patients: A Systematic Review and Meta-Analysis. Medicina. 2025; 61(11):1929. https://doi.org/10.3390/medicina61111929
Chicago/Turabian StyleHakami, Ibrahim A., Mohammed A. Altammar, Shafi A. Alaklabi, Meshari M. Alotaibi, Saleh N. Almunyif, Mohammed I. Alshuwaier, Sultan T. Alobaysi, Sultan S. Aldalbahi, Abdullah H. Alotaibi, Mohammed M. Alotaibi, and et al. 2025. "Thromboembolic Risk After Total Hip Replacement Versus Hemiarthroplasty in Femoral Neck Fracture Patients: A Systematic Review and Meta-Analysis" Medicina 61, no. 11: 1929. https://doi.org/10.3390/medicina61111929
APA StyleHakami, I. A., Altammar, M. A., Alaklabi, S. A., Alotaibi, M. M., Almunyif, S. N., Alshuwaier, M. I., Alobaysi, S. T., Aldalbahi, S. S., Alotaibi, A. H., Alotaibi, M. M., Alobaysi, O. S., Aladhyani, M. T., & Jareebi, M. A. (2025). Thromboembolic Risk After Total Hip Replacement Versus Hemiarthroplasty in Femoral Neck Fracture Patients: A Systematic Review and Meta-Analysis. Medicina, 61(11), 1929. https://doi.org/10.3390/medicina61111929






