Abstract
Background and Objectives: Immediate implant placement in the esthetic zone presents challenges in maintaining peri-implant tissues due to post-extraction remodeling. Bone grafting has been proposed to support tissue preservation and improve esthetic outcomes. This article reviews the role of grafting in clinical studies and case reports. Materials and Methods: A literature search on PubMed and Google Scholar identified studies focusing on immediate implant placement with grafting. The search strategy included articles from 2012 to 2025, in English, from peer-reviewed journals. Results: Implant survival is possible without grafting in ideal cases, but grafting is often essential in patients with thin biotypes or esthetic demands. Technique and material selection are critical. The socket shield technique shows promise in preserving buccal tissues despite its complexity. Case reports demonstrated stable soft tissues and favorable esthetic outcomes. Conclusions: Grafting should be tailored to the clinical situation. While not always necessary, it is often crucial in compromised sites to ensure long-term esthetic success. Current literature supports predictable outcomes with appropriate grafting protocols.
1. Introduction
Immediate implant placement encompasses a variety of techniques, each defined by specific procedural variations tailored to clinical and anatomical circumstances. These approaches are primarily categorized based on three critical clinical decisions: (1) soft tissue management, specifically whether to perform a flapless or flap-based surgical approach; (2) the treatment of the fresh extraction socket, including drilling protocols for achieving primary implant stability; and (3) the timing of provisional restoration placement, also known as immediate provisionalization [1].
The selection of the most appropriate technique is multifactorial, relying on a comprehensive assessment of the patient’s anatomical features, the integrity of the extraction site, and the desired esthetic and functional outcomes [2,3]. The initial decision—whether to perform a flapless procedure or raise a mucoperiosteal flap—is pivotal. A flapless approach preserves the periosteal blood supply and reduces postoperative morbidity, whereas flap elevation offers improved access, visibility, and facilitates bone augmentation when needed [4,5,6]. Following this, achieving primary implant stability involves strategic implant positioning, often by engaging the apical or palatal bone. Grafting materials may be employed to enhance osseointegration and support the peri-implant tissues in cases where a gap remains between the implant and socket walls [7,8].
The decision to place an immediate provisional restoration depends on the quality of primary stability achieved. When sufficient stability is confirmed, immediate provisionalization can help preserve the soft tissue contours and provide instant esthetic benefits. Conversely, a delayed approach may be preferred in situations where initial stability is inadequate, allowing for undisturbed soft tissue healing prior to prosthetic placement [9].
Given the complexity and technique-sensitive nature of these decisions, a comprehensive understanding of each approach is crucial for achieving predictable esthetic and functional success. This paper will therefore provide a narrative review of the current immediate implant placement techniques
2. Materials and Methods
The literature search was performed in two different databases (Google Scholar and PubMed). The following filters were used for Google Scholar: Articles from 2012 to 2025, in English. Systematic reviews, meta-analysis, studies in animals (canine, rats, and rabbits were excluded), and the search strategy was the following: “immediate implant placement” AND “bone grafting”–“systematic review”–meta-analysis–animal–canine–rat–rabbit. The search strategy for PubMed was as follows: (“Immediate Dental Implant Loading” (Mesh)) OR “immediate implant placement” (tiab) OR “immediate implantation” (tiab) OR “post-extraction implant” (tiab) OR “fresh socket” (tiab)) AND (“Bone Transplantation” (Mesh) OR “Alveolar Ridge Augmentation” (Mesh)) OR “bone graft” (tiab) OR “bone grafting” (tiab) OR “socket grafting” (tiab) OR “ridge preservation” (tiab) OR “guided bone regeneration” (tiab)) NOT (“systematic review” (Publication Type) OR “meta-analysis” (Publication Type) OR (animals (MeSH) NOT humans (MeSH))). The search excluded systematic reviews and meta-analyses, in vitro studies, and studies in animals or in vitro and ex vivo studies. A manual search was made from the cited articles and found other 14 articles. The details of the search and selection of the articles are shown in Figure 1.
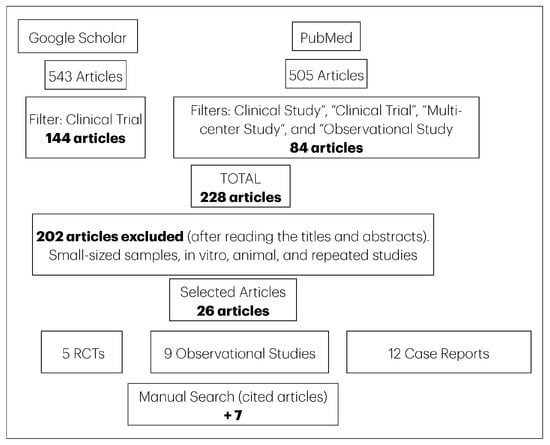
Figure 1.
Flowchart illustrating the search strategy and selection process for the articles.
Two independent reviewers were involved in screening and data extraction. The research question was “Does immediate implant placement with bone augmentation in post-extraction sockets with buccal bony defects of ≥5 mm in the esthetic zone lead to comparable or superior peri-implant hard and soft tissue outcomes, esthetics, and patient satisfaction over a 5-year period, compared to delayed implant placement after alveolar ridge preservation?” This research question compares two non-randomized interventions (immediate vs. delayed implant placement) for which a randomized controlled trial (RCT) would be unethical or impractical.
Confounding Factors
Initial Bone and Tissue Conditions: The baseline state of the patient’s bone and soft tissue is a significant confounder. Differences in buccal bone thickness, the size and type of the bony defect, and the atient’s gingival tissue phenotype (biotype) could all affect the outcome, regardless of the intervention chosen. For example, a thicker gingival biotype is associated with more favorable esthetic outcomes and less recession.
Patient Health and Habits: Systemic health and patient habits can influence healing and long-term implant success. Factors such as uncontrolled diabetes, smoking (especially heavy smoking more than 20 cigarettes per day), and parafunctional habits like bruxism are all known to negatively impact treatment outcomes.
Surgical Technique and Operator Experience: The skill and experience of the surgeon affects the result, particularly for a technically sensitive procedure like immediate implant placement. Key aspects include the atraumatic extraction of the tooth to preserve bone, the proper positioning of the implant, and the careful execution of bone grafting and soft tissue procedures. A flapless approach versus a flap elevation is another technical difference that could influence outcomes.
Implant and Grafting Material Characteristics: The type of implant used, including its design (e.g., tapered, platform-switched, micro threaded surface), length, and diameter, can influence primary stability and long-term bone maintenance. The choice of bone grafting material (e.g., xenograft, allograft) and whether a membrane is used also plays a role in bone regeneration and stability.
Prosthetic Protocol: How and when the definitive restoration is placed can affect the final soft and hard tissue contours. The timing of provisionalization, the type of restoration (e.g., screw-retained vs. cement-retained), and the occlusal load on the implant can all be confounding factors. For instance, excess cement in a cement-retained restoration can lead to bone loss and inflammation.
3. Results
Comprehensive Review Outcome
The risk of bias (RoB) analysis for a selection of clinical studies on immediate implant placement was made using Cochrane Risk of Bias (ROBINS-I), used for Randomized Controlled Trials (RCTs). The purpose of this analysis is to evaluate the methodological quality of each study and determine the level of confidence in their reported outcomes.
Table 1 summarizes the study characteristics of observational studies from 2012 to 2025 on immediate implant placement studies.

Table 1.
Study characteristics of selected observational studies (2012 to 2025) on immediate implant placement studies [10,11,12,13,14,15,16,17,18,19].
Table 2 describes the overall risk of bias for each study and provides a brief justification for the assessment, highlighting the key factors that influence each study’s internal validity.

Table 2.
Risk of bias analysis of selected RCTs (2012 to 2025) on immediate implant placement studies [20,21,22,23,24,25,26,27,28,29,30].
An analysis of the ‘Risk of Bias’ column reveals a prevalence of ‘Low risk’ classifications in 9 out of 13 studies. Conversely, only 4 studies were categorized as having a ‘Moderate risk’ of bias. This distribution suggests a general adherence to robust methodological practices within the reviewed studies, aimed at minimizing inherent biases. Based on the “Random Sequence Generation” column in the provided data, a few studies used sophisticated computer-generated randomization lists [20,21,22,23]. One single study indicated random assignment without explicitly detailing the generation method, which mentions that patients were “randomly assigned” but does not explicitly state the method beyond the computer-generated list for allocation [20]. Two other studies used simple random sequences [21,22], while another used block randomization [23]. Another study used a more rudimentary manual technique—a shuffled deck of cards [24].
4. Discussion
4.1. The Role of Grafting in Hard and Soft Tissue Stability
The rationale for bone grafting during immediate implant placement extends beyond simply filling a void; it is intended to actively influence the healing of both hard and soft tissues to ensure long-term stability and esthetics. The type of graft material and the patient’s pre-existing tissue quality are significant variables that affect the outcome. The interaction between the graft, the implant, and the surrounding biological environment determines whether the tissue volume is maintained, enhanced, or diminished over time.
Observational studies have shed light on how grafting influences tissue healing and dimensional changes. One prospective clinical study found that a history of bone grafting prior to implant placement can positively affect subsequent soft tissue healing [11]. These results suggest augmented sites provide a more favorable environment for peri-implant tissue health. The choice of graft material also plays a role, as a clinical study assessing different bone grafts in immediate implant sites found variations in implant stability, indicating that material properties can influence the osseointegration process [12]. In cases with a thin buccal plate in the anterior maxilla, a case series demonstrated that immediate implant placement with simultaneous buccal bone augmentation led to favorable outcomes at one year, with stable bone and ridge dimensions [13].
These studies underscore the importance of a comprehensive site assessment before deciding on a grafting strategy. In sites with bone loss or a thin buccal plate, not grafting can cause facial recession and gray tissue discoloration from the implant. A case series on immediate implants with facial bone dehiscence found that while the procedure can be successful, the correlation between pre-operative dehiscence and postoperative gingival recession highlights the inherent risks [14]. Therefore, grafting should be viewed not only as corrective but as a proactive step to strengthen the tissue biotype and ensure a stable foundation for the final restoration.
4.2. Immediate Provisionalization and Grafting in the Esthetic Zone
The decision to place an immediate provisional restoration and to graft the peri-implant gap is a critical step in achieving predictable esthetic outcomes [15,16]. This approach is particularly relevant in the esthetic zone, where the preservation of soft tissue architecture is important. The literature provides several examples of high success rates when combining these techniques, though the protocols and materials vary. The primary goals are to support the facial tissues, prevent gingival recession, and maintain the natural emergence profile of the restoration from the outset of treatment [17].
Evidence from prospective case series supports the viability of this combined approach. In 110 implants placed without graft material (selected based on sufficient bone beyond the root apex and absence of pathology), survival over 5 years was very high, with only five failures [18]. These results demonstrate predictability. A study involving 27 patients who received immediately placed and provisionalized implants with bone grafting in the esthetic zone reported predictable success and survival, highlighting the importance of 3D implant positioning and a non-functional, screw-retained provisional [19]. Similarly, another case series involving 15 patients who received immediate implants with provisional restoration demonstrated stable changes in hard and soft tissues over a 23.2-month follow-up [19]. These results reinforce the technique’s reliability when strict clinical protocols are followed. Furthermore, a study focusing on peri-implant bone response after immediate placement and provisionalization also found favorable outcomes, suggesting this protocol can maintain bone levels effectively in the esthetic zone [20].
These findings suggest that, when primary stability is achieved, immediate provisionalization with bone grafting is an effective strategy for managing peri-implant tissues. The provisional crown acts as a scaffold for the healing gingiva, while the bone graft helps to fill the residual gap and support the facial bone plate, mitigating the risk of resorption and subsequent tissue collapse. However, as noted in a retrospective study analyzing treatment for labial soft tissue recession, the use of mineralized allograft for guided bone regeneration can be an effective method to address and prevent such esthetic complications, emphasizing that grafting is a key component for long-term tissue stability [21,22].
4.3. Socket Shield Technique as an Alternative to Complete Extraction
An alternative approach to conventional immediate implant placement is the socket shield technique (SST), which involves retaining the buccal portion of the root to preserve the periodontal ligament and, consequently, the buccal bone plate. This technique was developed to counteract the physiological bone remodeling and resorption that typically follows tooth extraction. By leaving the labial root fragment in situ, the blood supply from the periodontal ligament is maintained, which is thought to provide a more stable biological environment for the peri-implant tissues [23].
Despite its potential benefits, the socket shield technique requires meticulous execution and is associated with a steep learning curve. The clinician must be proficient in sectioning the root without damaging the buccal plate and placing the implant in the correct three-dimensional position relative to the retained root fragment. Complications such as infection, failure of the shield to integrate, or exposure of the shield can occur. Therefore, although SST provides a strong biological rationale for ridge preservation, its use should be limited to experienced clinicians and carefully selected cases where the benefits outweigh the risks [24].
4.4. Insights from Randomized Clinical Evidence
RCTs provide the highest level of evidence for evaluating clinical interventions. Several RCTs have investigated the efficacy of bone grafting in immediate implant placement. These studies offer more definitive insights into whether grafting provides a clinically significant benefit compared to non-grafted sites. The evidence, however, is not entirely conclusive and often depends on the specific clinical scenario, outcome measures, and follow-up duration.
In contrast, a different randomized trial employing “dual zone grafting” with a mix of autogenous and xenogeneic bone reported that this technique significantly improved tissue volume and esthetic outcomes. This discrepancy suggests that the grafting technique and material choice are critical variables [28].
One RCT evaluating grafting in sites with a thin labial plate found that adding a xenograft yielded only a minimal, statistically insignificant increase in horizontal bone width after one year compared with ungrafted sites [29]. One RCT comparing immediate versus early implant placement in the esthetic area found that both treatments can yield successful outcomes, suggesting that clinicians have some flexibility in timing, though immediate placement offers the benefit of a shorter treatment period [31,32,33]. Grafting during immediate placement may offer minor improvements in horizontal gap fill and soft-tissue esthetics in the anterior zone, but evidence of significant volumetric preservation is inconsistent (~0.2 mm difference).
4.5. Limitations of the Review
This narrative review has several limitations. The search strategy was not as exhaustive as that of a systematic review and was limited to two databases, which may have resulted in the omission of some relevant studies. The heterogeneity among the included studies in terms of methodology, follow-up duration, and outcome measures makes direct comparisons difficult and limits the ability to draw definitive, overarching conclusions. The constraints here outlined directly qualify the strength of the discussion’s conclusions, revealing the unreliable foundation of the evidence. The discussion uses a limited, non-exhaustive selection of studies, which means its inferences may be based on incomplete information. This raises the possibility that other studies not included in the review could contradict or significantly alter the findings, making the conclusions about the benefits of grafting tentative rather than definitive. For example, while the text mentions “high success rates,” this observation might be skewed if a broader, more representative sample of the literature were examined.
The heterogeneity of the included studies further undermines the reliability of the discussion’s inferences. The studies referenced varied widely in their methods, follow-up times, and outcome measures, making direct comparisons difficult. This inconsistency makes it impossible to draw a single, strong conclusion about grafting’s effectiveness. The inference that the grafting technique and material are critical variables is a logical one, but it remains a qualified statement because the underlying evidence is too inconsistent to support a definitive conclusion.
5. Conclusions
Integrating bone grafting into immediate implant placement protocols is beneficial for achieving predictable and stable aesthetic outcomes, especially in the challenging anterior maxilla. Although implants may survive in certain cases without grafting, the evidence suggests that bone grafts help preserve alveolar bone dimensions and support peri-implant soft tissues. This is critical for long-term success. The chosen technique—whether flapped or flapless, the type of graft material, and the use of immediate provisionalization—must be customized to the patient’s specific anatomical and clinical needs. A comprehensive approach that combines digital planning, atraumatic surgery, soft tissue augmentation, and precise prosthetic management is essential for success in complex aesthetic cases.
Author Contributions
Conceptualization, C.A.J. and G.G.-P.; methodology, F.A. and M.A.A.; software, S.R.-R.; validation, F.F., K.I.A. and N.G.F.; formal analysis, F.A.; investigation, C.A.J. and M.A.A.; resources, F.A. and G.G.-P.; data curation, M.A.A. and S.R.-R.; writing—original draft preparation, F.A. and C.A.J.; writing—review and editing, N.G.F. and M.A.A.; visualization, S.R.-R. and M.A.A.; supervision, K.I.A. and G.G.-P.; project administration, K.I.A. and F.F.; funding acquisition, K.I.A. and N.G.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
K. I. Afrashtehfar thanks the Universität Bern for partially supporting the open access publication of this work.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Levine, R.A.; Ganeles, J.; Gonzaga, L.; Kan, J.K.; Randel, H.; Evans, C.D.; Chen, S.T. 10 keys for successful esthetic-zone single immediate implants. Compend. Contin. Educ. Dent. 2017, 38, 248–260. [Google Scholar] [PubMed]
- Vasiljevic, M.; Selakovic, D.; Rosic, G.; Stevanovic, M.; Milanovic, J.; Arnaut, A.; Milanovic, P. Anatomical factors of the anterior and posterior maxilla affecting immediate implant placement based on cone beam computed tomography analysis: A narrative review. Diagnostics 2024, 14, 1697. [Google Scholar] [CrossRef]
- De Angelis, N.; Signore, A.; Alsayed, A.; Hai Hock, W.; Solimei, L.; Barberis, F.; Amaroli, A. Immediate implants in the aesthetic zone: Is socket shield technique a predictable treatment option? A narrative review. J. Clin. Med. 2021, 10, 4963. [Google Scholar] [CrossRef]
- Liñares, A.; Dopico, J.; Magrin, G.; Blanco, J. Critical review on bone grafting during immediate implant placement. Periodontol. 2000 2023, 93, 309–326. [Google Scholar] [CrossRef]
- Sanz-Sánchez, I.; Sanz-Martín, I.; Ortiz-Vigón, A.; Molina, A.; Sanz, M. Complications in bone-grafting procedures: Classification and management. Periodontol. 2000 2022, 88, 86–102. [Google Scholar] [CrossRef] [PubMed]
- Blanco, J.; Caramês, J.; Quirynen, M. A narrative review on the use of autologous platelet concentrates during alveolar bone augmentation: Horizontal (simultaneous/staged) & vertical (simultaneous/staged). Periodontol. 2000 2025, 97, 236–253. [Google Scholar] [CrossRef] [PubMed]
- Jebelli, M.S.H.; Yari, A.; Nikparto, N.; Cheperli, S.; Asadi, A.; Darehdor, A.A.; Nezanimia, S.; Drotaj, D.; Mehraban, S.H.; Hakim, L.K. Tissue engineering innovations to enhance osseointegration in immediate dental implant loading: A narrative review. Cell Biochem. Funct. 2024, 42, e3974. [Google Scholar] [CrossRef]
- Sghaireen, M.G.; Shrivastava, D.; Alnusayri, M.O.; Alahmari, A.D.; Aldajani, A.M.; Srivastava, K.C.; Alam, M.K. Bone grafts in dental implant management: A narrative review. Curr. Pediatr. Ver. 2023, 19, 15–20. [Google Scholar] [CrossRef] [PubMed]
- de Araújo Nobre, M.; Salvado, F.; Correia, J.A.; Teixeira, M.C.F.; Coutinho, F.A. Long-term outcome of dental implants in immediate function inserted on autogenous grafted bone. J. Clin. Med. 2022, 12, 261. [Google Scholar] [CrossRef]
- Amato, F.; Cracknell, T.J. Single-Tooth Immediate Placement and Provisionalization with Subcrestally Angulated Implants in Sites with Hard and Soft Tissue Facial Dehiscence in the Esthetic Zone: An Observational Study with 2 to 5 Years of Follow-up. Int. J. Periodontics Restor. Dent. 2022, 42, e133–e142. [Google Scholar] [CrossRef]
- Kofina, V.; Demirer, M.; Erdal, B.S.; Eubank, T.D.; Yildiz, V.O.; Tatakis, D.N.; Leblebicioglu, B. Bone grafting history affects soft tissue healing following implant placement. J. Periodontol. 2020, 92, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Jalaluddin, M.; Sathe, S.; Thomas, J.; Haleem, S.; Naik, S.; Shivanna, M.M. Assessment of implant stability in immediate implant placement using different bone grafting materials: A clinical study. J. Pharm Bioallied Sci. 2021, 13 (Suppl. S1), S612–S615. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Li, Z.; Liu, X.; Liu, Q.; Chen, Z.; Sun, Y.; Chen, Z.; Huang, B. Immediate implant placement with buccal bone augmentation in the anterior maxilla with thin buccal plate: A one-year follow-up case series. J. Prosthod. 2021, 30, 473–480. [Google Scholar] [CrossRef]
- Mizuno, K.; Nakano, T.; Shimomoto, T.; Fujita, Y.; Ishigaki, S. The efficacy of immediate implant placement in the anterior maxilla with dehiscence in the facial alveolar bone: A case series. Clin. Implant Dent. Related Res. 2022, 24, 72–82. [Google Scholar] [CrossRef]
- Le, B.; Borzabadi-Farahani, A.; Nielsen, B. Treatment of labial soft tissue recession around dental implants in the esthetic zone using guided bone regeneration with mineralized allograft: A retrospective clinical case series. J. Oral Maxillofac. Surg. 2016, 74, 1552–1561. [Google Scholar] [CrossRef]
- Martin, C.; Thomé, G.; Melo, A.C.M.; Fontão, F.N.G.K. Peri-implant bone response following immediate implants placed in the esthetic zone and with immediate provisionalization—A case series study. Oral Maxillofac. Surg. 2015, 19, 157–163. [Google Scholar] [CrossRef]
- Khzam, N.; Mattheos, N.; Roberts, D.; Bruce, W.L.; Ivanovski, S. Immediate placement and restoration of dental implants in the esthetic region: Clinical case series. J. Esthet. Restor. Dent. 2014, 26, 332–344. [Google Scholar] [CrossRef]
- Atalay, B.; Öncü, B.; Emes, Y.; Bultan, Ö.; Aybar, B.; Yalçin, S. Immediate implant placement without bone grafting: A retrospective study of 110 cases with 5 years of follow-up. Implant. Dent. 2013, 22, 360–365. [Google Scholar] [CrossRef]
- Levin, B.P.; Wilk, B.L. Immediate provisionalization of immediate implants in the esthetic zone: A prospective case series evaluating implant survival, esthetics, and bone maintenance. Compend. Contin. Educ. Dent. 2013, 34, 351–361. [Google Scholar] [PubMed]
- Cardaropoli, D.; Gaveglio, L.; Gherlone, E.; Cardaropoli, G. Soft tissue contour changes at immediate implants: A randomized controlled clinical study. Int. J. Periodontics Restor. Dent. 2014, 34, 631–637. [Google Scholar] [CrossRef]
- Mastrangelo, F.; Gastaldi, G.; Vinci, R.; Troiano, G.; Tettamanti, L.; Gherlone, E.; Muzio, L.L. Immediate postextractive implants with and without bone graft: 3-year follow-up results from a multicenter controlled randomized trial. Implant. Dent. 2018, 27, 638–645. [Google Scholar] [CrossRef]
- Guadilla González, Y.; Benito Garzón, L.; Quispe López, N.; Montero Martín, J. Histologic Outcomes of the Use of Different Biomaterials for Socket Regeneration in Fresh Extraction Sockets: A Split-Mouth Randomized Clinical Trial. Int. J. Oral Maxillofac. Implant. 2022, 37, 1026–1036. [Google Scholar] [CrossRef]
- Gurbuz, E.Z.G.İ.; Ceylan, E. Comparison of a non-grafted socket shield technique with guided bone regeneration in immediate implant placement: A randomized clinical trial. Int. J. Oral Maxillofac. Surg. 2025, 54, 356–364. [Google Scholar] [CrossRef]
- de Oliveira, G.B.; Rebello, I.M.C.; Andrade, K.M.; Araujo, N.S.; Dos Santos, J.N.; Cury, P.R. Evaluation of alveolar process resorption after tooth extraction using the socket shield technique without immediate installation of implants: A randomised controlled clinical trial. Br. J. Oral Maxillofac. Surg. 2021, 59, 1227–1232. [Google Scholar] [CrossRef]
- Happe, A.; Schmidt, A.; Neugebauer, J. Peri-implant soft-tissue esthetic outcome after immediate implant placement in conjunction with xenogeneic acellular dermal matrix or connective tissue graft: A randomized controlled clinical study. J. Esthet. Restor. Dent. 2022, 34, 215–225. [Google Scholar] [CrossRef]
- Perez, A.; Caiazzo, A.; Valente, N.A.; Toti, P.; Alfonsi, F.; Barone, A. Standard vs customized healing abutments with simultaneous bone grafting for tissue changes around immediate implants. 1-year outcomes from a randomized clinical trial. Clin. Implant Dent. Relat. Res. 2020, 22, 42–53. [Google Scholar] [CrossRef]
- Girlanda, F.F.; Feng, H.S.; Corrêa, M.G.; Casati, M.Z.; Pimentel, S.P.; Ribeiro, F.V.; Cirano, F.R. Deproteinized bovine bone derived with collagen improves soft and bone tissue outcomes in flapless immediate implant approach and immediate provisionalization: A randomized clinical trial. Clin. Oral Investig. 2019, 23, 3885–3893. [Google Scholar] [CrossRef]
- Bajaj, V.; Kolte, A.P.; Kolte, R.; Bawankar, P.V. Comparative evaluation of immediate implant placement and provisionalization (IIPP) with and without a concentrated growth factor-enriched bone graft: A randomized controlled trial. Dent. Med. Probl. 2025, 62, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Hamed, M.M.; El-Tonsy, M.M.; Elaskary, A.; Abdelaziz, G.O.; Saeed, S.S.; Elfahl, B.N. Effect of three different grafting materials on immediate implant placement using vestibular socket therapy in class II extraction sockets in the maxillary esthetic zone: A randomized controlled clinical trial. BMC Oral Health 2023, 23, 623. [Google Scholar] [CrossRef] [PubMed]
- El Zahwy, M.; Taha, S.A.A.K.; Mounir, R.; Mounir, M. Assessment of vertical ridge augmentation and marginal bone loss using autogenous onlay vs inlay grafting techniques with simultaneous implant placement in the anterior maxillary esthetic zone: A randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2019, 21, 1140–1147. [Google Scholar] [CrossRef] [PubMed]
- Wanis, R.W.; Hosny, M.M.; El Nahass, H. Clinical evaluation of the buccal aspect around immediate implant using dual zone therapeutic concept versus buccal gap fill to bone level: A randomized controlled clinical trial. Clin. Implant. Dent. Relat. Res. 2022, 24, 307–319. [Google Scholar] [CrossRef] [PubMed]
- Meijer, H.J.; Slagter, K.W.; Gareb, B.; Hentenaar, D.F.; Vissink, A.; Raghoebar, G.M. Immediate single-tooth implant placement in bony defect sites: A 10-year randomized controlled trial. J. Periodontol. 2025, 96, 151–163. [Google Scholar] [CrossRef] [PubMed]
- Puisys, A.; Auzbikaviciute, V.; Vindasiute-Narbute, E.; Pranskunas, M.; Razukevicus, D.; Linkevicius, T. Immediate implant placement vs. early implant treatment in the esthetic area. A 1-year randomized clinical trial. Clin. Oral Implants Res. 2022, 33, 634–655. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).