Abnormal Uterine Bleeding Among Rural Adolescent Schoolgirls: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
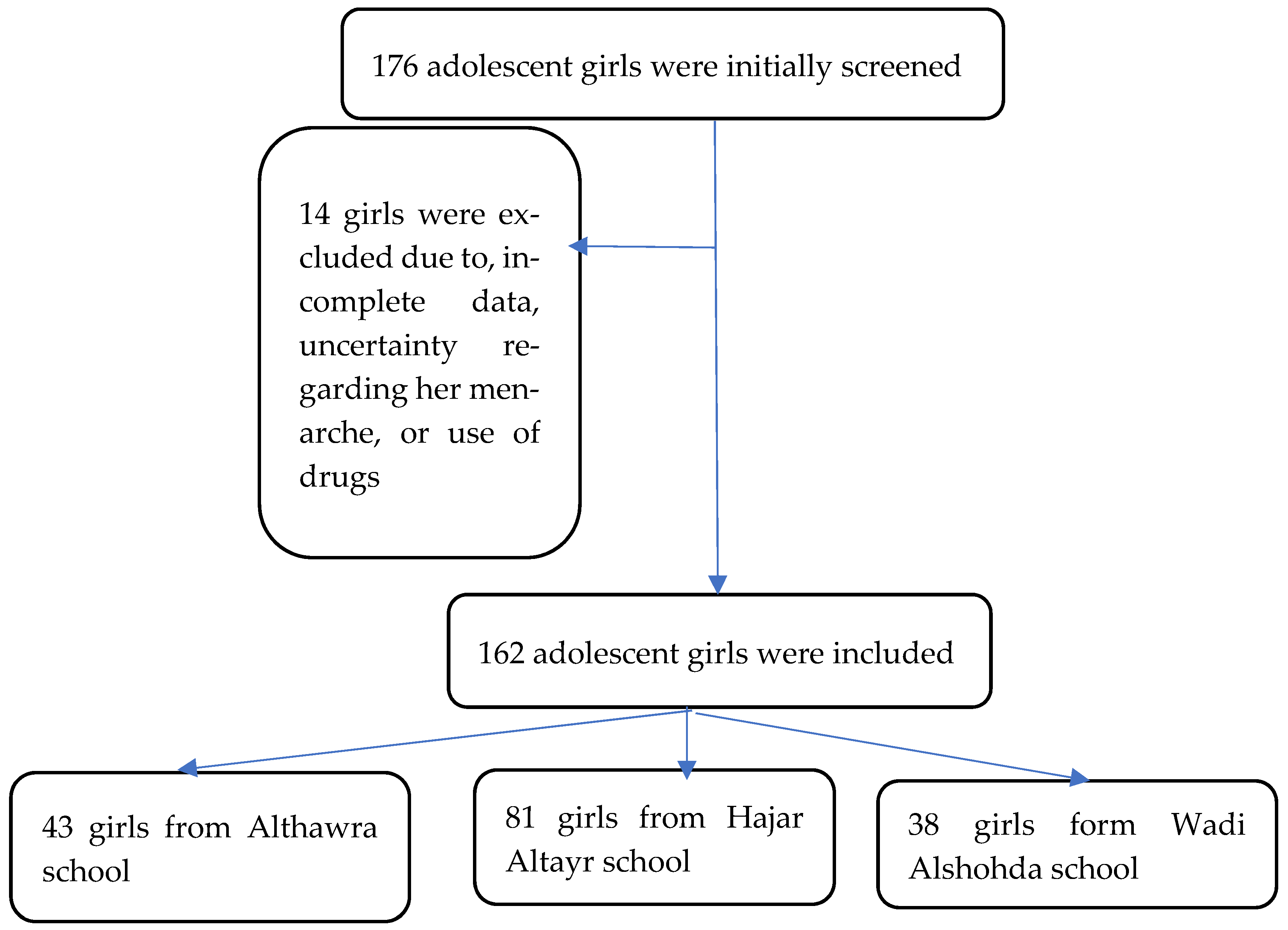
2.1. Sampling and Recruitment
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Definitions
2.5. Sample Size
2.6. Statistical Analysis
3. Results
3.1. Demographic and Social Characteristics of Participants
3.2. Menstrual Patterns and Disturbances
3.3. Factors Associated with AUB
4. Discussion
Strengths and Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Munro, M.G.; Critchley, H.O.D.; Fraser, I.S.; Haththotuwa, R.; Kriplani, A.; Bahamondes, L.; Füchtner, C.; Tonye, R.; Archer, D.; Abbott, J.; et al. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int. J. Gynecol. Obstet. 2018, 143, 393–408. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. Committee opinion no. 557: Management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women. Obstet. Gynecol. 2013, 121, 891–896. [Google Scholar] [CrossRef] [PubMed]
- Mittiku, Y.M.; Mekonen, H.; Wogie, G.; Tizazu, M.A.; Wake, G.E. Menstrual irregularity and its associated factors among college students in Ethiopia, 2021. Front. Glob. Women’s Health 2022, 3, 917643. [Google Scholar] [CrossRef]
- Demeke, E.; Zeru, A.B.; Tesfahun, E.; Mohammed, W.B. Effect of menstrual irregularity on academic performance of undergraduate students of Debre Berhan University: A comparative cross sectional study. PLoS ONE 2023, 18, e0280356. [Google Scholar] [CrossRef] [PubMed]
- Zeru, A.B.; Gebeyaw, E.D.; Ayele, E.T. Magnitude and associated factors of menstrual irregularity among undergraduate students of Debre Berhan University, Ethiopia. Reprod. Health 2021, 18, 101. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, A.; Dietrich, J.E. Abnormal Uterine Bleeding in the Adolescent. Obstet. Gynecol. 2020, 135, 615–621. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 128: Diagnosis of Abnormal Uterine Bleeding in Reproductive-Aged Women. Obstet. Gynecol. 2012, 120, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Yaşa, C.; Uğurlucan, F.G. Approach to abnormal uterine bleeding in adolescents. J. Clin. Res. Pediatr. Endocrinol. 2020, 12, 1–6. [Google Scholar] [CrossRef]
- Motta, T.; Laganà, A.S.; Valenti, G.; La Rosa, V.L.; Noventa, M.; Vitagliano, A.; Chiofalo, B.; Rapisarda, A.M.; Rossetti, D.; Vitale, S.G. Differential diagnosis and management of abnormal uterine bleeding in adolescence. Minerva Ginecol. 2017, 69, 618–630. [Google Scholar] [CrossRef]
- Crankshaw, T.L.; Strauss, M.; Gumede, B. Menstrual health management and schooling experience amongst female learners in Gauteng, South Africa: A mixed method study. Reprod. Health 2020, 17, 48. [Google Scholar] [CrossRef]
- Ramathuba, D.U. Menstrual knowledge and practices of female adolescents in Vhembe district, Limpopo Province, South Africa. Curationis 2015, 38, 6. [Google Scholar] [CrossRef]
- UNESCO. Puberty Education and Mentsrual Hygiene Management. Lancet 2014, 1, 1330–1331. [Google Scholar]
- Elmaoğulları, S.; Aycan, Z. Abnormal Uterine Bleeding in Adolescents. J. Clin. Res. Pediatr. Endocrinol. 2018, 10, 191. [Google Scholar] [CrossRef] [PubMed]
- Bennett, A.R.; Gray, S.H. What to do when she’s bleeding through: The recognition, evaluation, and management of abnormal uterine bleeding in adolescents. Curr. Opin. Pediatr. 2014, 26, 413–419. [Google Scholar] [CrossRef]
- Sani, K.; Lachyan, A.S.; Simon, N.H. Systematic Review on Prevalence of Menstrual Disorders Among Women. Int. J. Recent Sci. Res. 2021, 12, 1525–41527. [Google Scholar] [CrossRef]
- Shiferaw, M.T.; Wubshet, M.; Tegabu, D. Menstrual problems and associated factors among students of Bahir Dar University, Amhara National Regional State, Ethiopia: A cross-sectional survey. Pan Afr. Med. J. 2014, 17, 246. [Google Scholar] [CrossRef] [PubMed]
- Hossam, H.; Fahmy, N.; Khidr, N.; Marzouk, T. The Relationship between Menstrual Cycle Irregularity and Body Mass Index among Secondary Schools Pupils. J. Nurs. Health Sci. 2016, 5, 48–52. [Google Scholar] [CrossRef]
- Abdelmoty, H.I.; Youssef, M.A.; abdallah, S.; Abdel-Malak, K.; Hashish, N.M.; Samir, D.; Abdelbar, M.; Hosni, A.N.; Abd-El Ghafar, M.; Khamis, Y.; et al. Menstrual patterns and disorders among secondary school adolescents in Egypt. A cross-sectional survey. BMC Womens. Health 2015, 15, 70. [Google Scholar] [CrossRef]
- Abbasi, S.; Naz, S.; Khalid, S.; Bukhari, A. Menstrual Pattern and Common Menstrual Disorders among Adolescent Girls. Pak. J. Med. Health Sci. 2022, 16, 1031–1033. [Google Scholar] [CrossRef]
- Sharma, S.; Deuja, S.; Saha, C.G. Menstrual pattern among adolescent girls of Pokhara Valley: A cross sectional study. BMC Women. Health 2016, 16, 74. [Google Scholar] [CrossRef]
- Agarwal, A.; Venkat, A. Questionnaire Study on Menstrual Disorders in Adolescent Girls in Singapore. J. Pediatr. Adolesc. Gynecol. 2009, 22, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Marques, P.; Madeira, T.; Gama, A. Menstrual cycle among adolescents: Girls’ awareness and influence of age at menarche and overweight. Rev. Paul. Pediatr. 2022, 40, e2020494. [Google Scholar] [CrossRef]
- Pitangui, A.C.R.; Gomes, M.R.d.A.; Lima, A.S.; Schwingel, P.A.; Albuquerque, A.P.d.S.; de Araújo, R.C. Menstruation Disturbances: Prevalence, Characteristics, and Effects on the Activities of Daily Living among Adolescent Girls from Brazil. J. Pediatr. Adolesc. Gynecol. 2013, 26, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Saeed, M.; Mohammed, A. Influence of Socioeconomic Status in the Age at the of Menarche and Duration of Menstrual Bleeding. Mater. Sociomed. 2011, 23, 195. [Google Scholar] [CrossRef] [PubMed]
- Ghandour, R.; Stigum, H.; Giacaman, R.; Fjeld, H.; Holmboe-Ottesen, G. Menstrual characteristics and dysmenorrhea among Palestinian adolescent refugee camp dwellers in the West Bank and Jordan: A cross-sectional study. 2023; preprint. [Google Scholar] [CrossRef]
- Arafa, A.E.; Senosy, S.A.; Helmy, H.K.; Mohamed, A.A. Prevalence and patterns of dysmenorrhea and premenstrual syndrome among Egyptian girls (12–25 years). Middle East Fertil. Soc. J. 2018, 23, 486–490. [Google Scholar] [CrossRef]
- Amu, E.O.; Bamidele, J.O. Prevalence of menstrual disorders among adolescent girls in Osogbo, South Western Nigeria. Int. J. Adolesc. Med. Health 2014, 26, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Zegeye, D.T.; Megabiaw, B.; Mulu, A. Age at menarche and the menstrual pattern of secondary school adolescents in northwest Ethiopia. BMC Womens. Health 2009, 9, 29. [Google Scholar] [CrossRef] [PubMed]
- Adam, A.M.; Fadlalmola, H.A.; Mosaad, H.K. Menstrual Disorders Among Nursing Students at Al Neelain University, Khartoum State. Sudan J. Med. Sci. 2020, 15, 199–214. [Google Scholar] [CrossRef]
- Sen, L.C.; Annee, I.J.; Akter, N.; Fatha, F.; Mali, S.K.; Debnath, S. Study on relationship between obesity and menstrual disorders. Asian J. Med. Biol. Res. 2018, 4, 259–266. [Google Scholar] [CrossRef]
- Munro, M.G.; Mast, A.E.; Powers, J.M.; Kouides, P.A.; O’Brien, S.H.; Richards, T.; Lavin, M.; Levy, B.S. The relationship between heavy menstrual bleeding, iron deficiency, and iron deficiency anemia. Am. J. Obstet. Gynecol. 2023, 229, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Derman, R.J.; Patted, A. Overview of iron deficiency and iron deficiency anemia in women and girls of reproductive age. Int. J. Gynecol. Obstet. 2023, 162, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Sooki, Z.; Shariati, M.; Chaman, R.; Khosravi, A.; Effatpanah, M.; Keramat, A. The Role of Mother in Informing Girls About Puberty: A Meta-Analysis Study. Nurs. Midwifery Stud. 2016, 5, e30360. [Google Scholar] [CrossRef]
- Afsari, A.; Mirghafourvand, M.; Valizadeh, S.; Abbasnezhadeh, M.; Galshi, M.; Fatahi, S. The effects of educating mothers and girls on the girls’ attitudes toward puberty health: A randomized controlled trial. Int. J. Adolesc. Med. Health 2015, 29, 20150043. [Google Scholar] [CrossRef]
| Variable | Mean (Standard Deviation) |
|---|---|
| Age, years | 15.78 (1.25) |
| Body mass index, kg/m2 | 19.90 (3.36) |
| Gynecological age, years | 2.28 (1.37) |
| Hemoglobin level, g/dL | 12.58 (1.25) |
| Manses Duration, days | 5.23 (1.38) |
| Frequency (proportion) | |
| Mother’s educational level | |
| Illiterate | 43 (26.5) |
| Basic | 100 (61.7) |
| Secondary or Higher | 19 (11.7) |
| Mother’s occupation | |
| Housewife | 146 (90.1) |
| Employee | 16 (9.9) |
| Variable | Frequency | Proportion | 95% Confidence Interval |
|---|---|---|---|
| Cycle frequency | |||
| Normal (24–38 days) | 112 | 69.1 | 61.7–75.7 |
| Frequent (<24 days) | 44 | 27.2 | 20.9–34.5 |
| Infrequent (>38 days) | 6 | 3.7 | 1.7–7.8 |
| Menses duration | |||
| Normal (≤8 days) | 158 | 97.5 | 93.8–99.0 |
| Prolonged (>8 days) | 4 | 2.5 | 1.0–6.2 |
| Cycle regularity | |||
| Irregular (variation of 28–10 days) | 72 | 44.4 | 37.0–52.1 |
| Regular (variation of ≤7–9 days) | 90 | 55.6 | 47.9–63.0 |
| Menstrual flow volume | |||
| Heavy | 34 | 21.0 | 15.4–27.9 |
| Normal | 128 | 79.0 | 72.1–84.6 |
| Intermenstrual bleeding | |||
| Yes | 20 | 12.3 | 08.1–18.3 |
| No | 142 | 87.7 | 81.7–91.9 |
| Overall AUB (Presence of at least one abnormal finding) | |||
| No AUB | 57 | 35.2 | 28.3–42.8 |
| Yes AUB | 105 | 64.8 | 57.2–71.7 |
| Variable | Adolescents with No AUB (n = 57) | Adolescents with AUB (n = 105) | |||
|---|---|---|---|---|---|
| Mean (Standard Deviation) | OR (95% CI) | p | |||
| Hemoglobin level, g/dL | 12.63 (1.15) | 12.55 (1.30) | 0.94 (0.70–1.25) | 0.682 | |
| Age, years | 15.61 (1.26) | 15.88 (1.25) | 1.06 (0.76–1.48) | 0.71 | |
| Body mass index, kg/m2 | 19.57 (3.15) | 20.08 (3.46) | 1.04 (0.93–1.15) | 0.434 | |
| Gynecological age, years | 2.04 (1.18) | 2.41 (1.45) | 1.21 (0.87–1.67) | 0.243 | |
| Frequency (percentage) | |||||
| Mother’s occupation | Housewife | 51 (89.5) | 95 (90.5) | Reference | |
| Employee | 6 (10.5) | 10 (9.5) | 0.73 (0.21–2.46) | 0.616 | |
| Mother’s education level | Illiterate or basic | 52 (91.2) | 91 (86.7) | Reference | |
| Secondary or more | 5 (8.8) | 14 (13.3) | 1.73 (0.50–5.91) | 0.381 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salih, Y.; Almutairi, G.S.; Alhumaidi, N.H.; Alhabardi, N.; Adam, I. Abnormal Uterine Bleeding Among Rural Adolescent Schoolgirls: A Cross-Sectional Study. Medicina 2025, 61, 33. https://doi.org/10.3390/medicina61010033
Salih Y, Almutairi GS, Alhumaidi NH, Alhabardi N, Adam I. Abnormal Uterine Bleeding Among Rural Adolescent Schoolgirls: A Cross-Sectional Study. Medicina. 2025; 61(1):33. https://doi.org/10.3390/medicina61010033
Chicago/Turabian StyleSalih, Yasir, Ghaday S. Almutairi, Norah H. Alhumaidi, Nadiah Alhabardi, and Ishag Adam. 2025. "Abnormal Uterine Bleeding Among Rural Adolescent Schoolgirls: A Cross-Sectional Study" Medicina 61, no. 1: 33. https://doi.org/10.3390/medicina61010033
APA StyleSalih, Y., Almutairi, G. S., Alhumaidi, N. H., Alhabardi, N., & Adam, I. (2025). Abnormal Uterine Bleeding Among Rural Adolescent Schoolgirls: A Cross-Sectional Study. Medicina, 61(1), 33. https://doi.org/10.3390/medicina61010033





