Effects of Vape Use on Oral Health: A Review of the Literature
Abstract
1. Introduction
2. Objectives
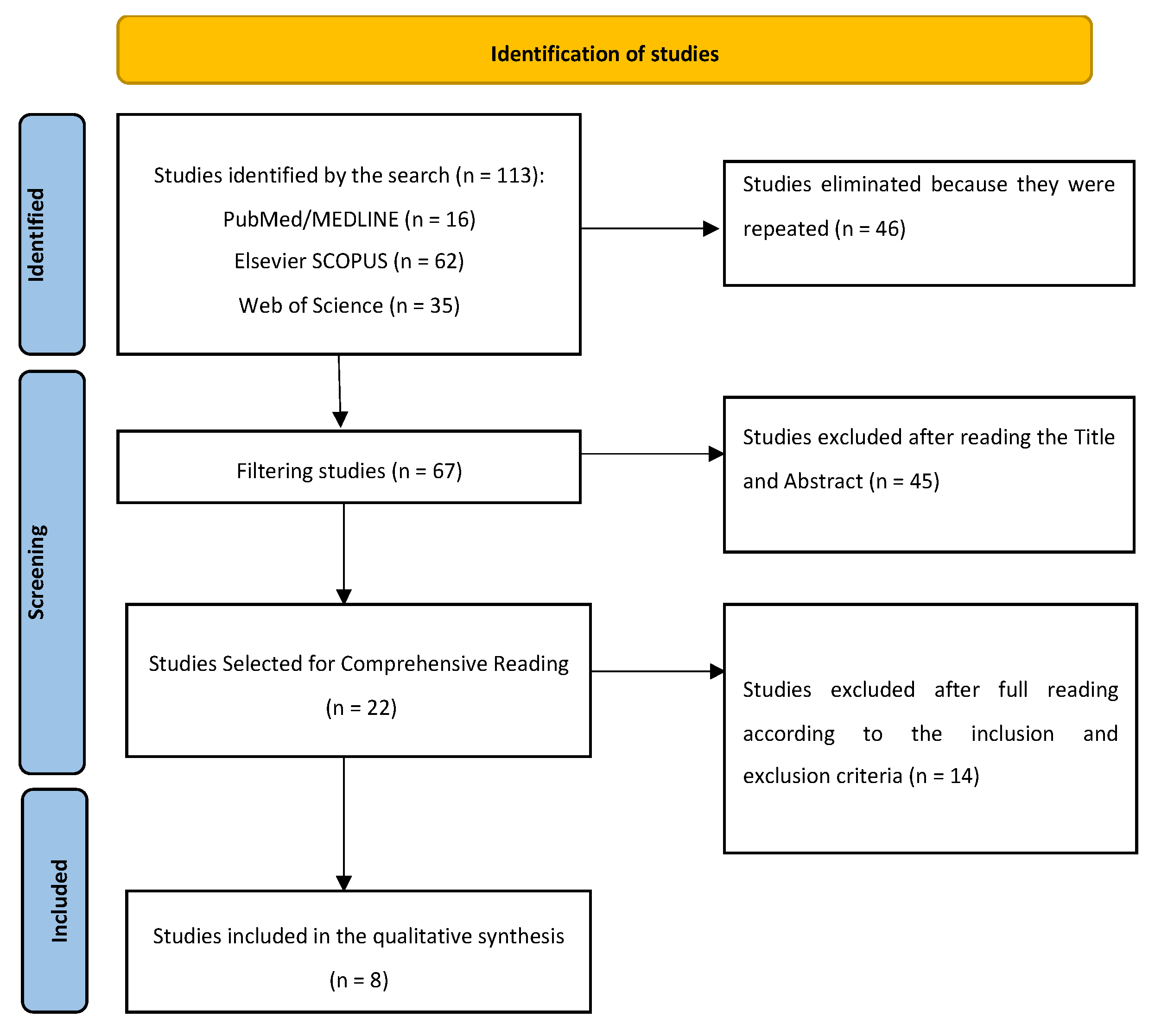
3. Materials and Methods
- Search Strategy
- Inclusion Criteria
- Exclusion Criteria
- Study Selection and Data Collection
4. Results
Description of the Studies
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ebersole, J.; Samburova, V.; Son, Y.; Cappelli, D.; Demopoulos, C.; Capurro, A.; Pinto, A.; Chrzan, B.; Kingsley, K.; Howard, K.; et al. Harmful chemicals emitted from electronic cigarettes and potential deleterious effects in the oral cavity. Tob. Induc. Dis. 2020, 8, 18–41. [Google Scholar] [CrossRef]
- Hang, H.; Dobson, R.; McCool, J. How young people in Aotearoa perceive vaping and the associated oral health risks. N. Z. Med. J. 2023, 136, 28–42. [Google Scholar]
- Fairchild, R.; Setarehnejad, A. Erosive potential of commonly available vapes: A cause for concern? Br. Dent. J. 2021, 231, 487–491. [Google Scholar] [CrossRef]
- Martell, K.M.; Boyd, L.D.; Giblin-Scanlon, L.J.; Vineyard, J. Knowledge, attitudes, and practices of young adults regarding the impact of electronic cigarette use on oral health. J. Am. Dent. Assoc. 2020, 151, 903–911. [Google Scholar] [CrossRef] [PubMed]
- Sharma, K.; Jha, R.K. Impact of Vaping on Lungs: An Indian Prospect. Cureus 2023, 4, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Almeida-da-Silva, C.C.F.; Dakafay, H.M.; O’Brien, K.; Montierth, D.; Xiao, N.; Ojcius, D.M. Effects of electronic cigarette aerosol exposure on oral and systemic health. Biomed. J. 2021, 44, 252–259. [Google Scholar] [CrossRef]
- WHO Reports Progress in the Fight against Tobacco Epidemic. Available online: https://www.who.int/news/item/27-07-2021-who-reports-progress-in-the-fight-against-tobacco-epidemic (accessed on 27 July 2021).
- Vaping to Quit Smoking. Available online: https://www.nhs.uk/better-health/quit-smoking/vaping-to-quit-smoking/ (accessed on 7 April 2019).
- Figueredo, C.A.; Abdelhay, N.; Figueredo, C.M.; Catunda, R.; Gibson, M.P. The impact of vaping on periodontitis: A systematic review. Clin. Exp. Dent. Res. 2021, 7, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Krishnan-Sarin, S.; Morean, M.; Kong, G.; Bold, K.W.; Camenga, D.R.; Cavallo, D.A.; Simon, P.; Ran Wu, R. E-Cigarettes and “Dripping” Among High-School Youth. Pediatrics 2017, 1, 139–143. [Google Scholar]
- Lidón-Moyano, C.; Martínez-Sánchez, J.M.; Fu, M.; Ballbè, M.; Martín-Sánchez, J.C.; Fernández, E. Prevalence and profile of electronic cigarette use in Spain. Gac Sanit. 2016, 30, 432–437. [Google Scholar] [CrossRef]
- Bello, S.S. Lung damage associated with the use of e-cigarette-vapes. Rev. Chil. Dis. Breathe 2020, 36, 115–121. [Google Scholar]
- Peruga, A.; Martínez, C.; Fu, M.; Ballbè, M.; Tigova, O.; Carnicer-Pont, D.; Fernández, E. Current e-cigarette use among high school students who have never smoked. Gac Sanit. 2022, 36, 433–438. [Google Scholar] [CrossRef]
- Holliday, R.; Chaffee, B.W.; Jakubovics, N.S.; Kist, R.; Preshaw, P.M. Electronic Cigarettes and Oral Health. J. Dent. Res. 2021, 100, 906–913. [Google Scholar] [CrossRef]
- Cichońska, D.; Kusiak, A.; Kochańska, B.; Ochocińska, J.; Świetlik, D. Influence of Electronic Cigarettes on Selected Physicochemical Properties of Saliva. Int. J. Environ. Res. Public Health 2022, 19, 3314. [Google Scholar] [CrossRef] [PubMed]
- Javed, F.; Abduljabbar, T.; Vohra, F.; Malmstrom, H.; Rahman, I.; Romanos, G.E. Comparison of periodontal parameters and self-perceived oral symptoms among cigarette smokers, individuals vaping electronic cigarettes, and never-smokers. J. Periodontol. 2017, 88, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Ghazali, A.F.; Ismail, A.F.; Faisal, G.G.; Halil, M.H.M.; Daud, A. Oral health of smokers and e-cigarette users: A case-control study. J. Int. Dent. Med. Res. 2018, 11, 428–432. [Google Scholar]
- Ye, D.; Gajendra, S.; Lawyer, G.; Jadeja, N.; Pishey, D.; Pathagunti, S. Inflammatory biomarkers, and growth factors in saliva and gingival crevicular fluid of e-cigarette users, cigarette smokers, and dual smokers: A pilot study. J. Periodontol. 2020, 91, 1274–1283. [Google Scholar] [CrossRef] [PubMed]
- Jeong, W.; Choi, D.W.; Kim, Y.K.; Lee, H.J.; Lee, S.A.; Park, E.C.; Jang, S.I. Associations of electronic and conventional cigarette use with periodontal disease in South Korean adults. J. Periodontol. 2020, 91, 55–64. [Google Scholar] [CrossRef]
- Vemulapalli, A.; Mandapati, S.R.; Kotha, A.; Aryal, S. Association between vaping and untreated caries A cross-sectional study of National Health and Nutrition Examination Survey 2017–2018 data. J. Am. Dent. Assoc. 2021, 152, 720–729. [Google Scholar] [CrossRef]
- Irusa, K.F.; Finkelman, M.; Magnuson, B.; Donovan, T.; Eisen, S.E. A comparison of the caries risk between patients who use vapes or electronic cigarettes and those who do not: A cross-sectional study. J. Am. Dent. Assoc. 2022, 153, 1179–1183. [Google Scholar] [CrossRef]
- Ramenzoni, L.L.; Schneider, A.; Fox, S.C.; Meyer, M.; Meboldt, M.; Attin, T.; Schmidlin, P.R. Cytotoxic and Inflammatory Effects of Electronic and Traditional Cigarettes on Oral Gingival Cells Using a Novel Automated Smoking Instrument: An In Vitro Study. Toxics 2022, 6, 179. [Google Scholar] [CrossRef]
- Xu, C.P.; Palazzolo, D.L.; Cuadra, G.A. Mechanistic Effects of E-Liquids on Biofilm Formation and Growth of Oral Commensal Streptococcal Communities: Effect of Flavoring Agents. Dent. J. 2022, 10, 85. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.S.; Clark, P.; Brinkman, M.C.; Saxena, D. Novel Nicotine Delivery Systems. Adv. Dent. Res. 2019, 30, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Heller, Z.A.; Ms, E.C.A.; Dmd, J.E.P. Implications of Electronic Cigarettes on the Safe Administration of Sedation and General Anesthesia in the Outpatient Dental Setting. Anesth Prog. 2022, 69, 41–52. [Google Scholar] [CrossRef]
- Alhajj, M.N.; Al-Maweri, S.A.; Folayan, M.O.; Halboub, E.; Khader, Y.; Omar, R.; Abdullah, G.; Amran, A.G.; Al-Batayneh, O.B.; Celebić, A.; et al. Oral health practices and self-reported adverse effects of E-cigarette use among dental students in 11 countries: An online survey. BMC Oral Health 2022, 67, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Briggs, K.; Bell, C.; Breik, O. What should every dental health professional know about electronic cigarettes? Aust. Dent. J. 2021, 66, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Raj, A.T.; Sujatha, G.; Muruganandhan, J.; Kumar, S.S.; Bharkavi, S.I.; Varadarajan, S.; Shankargouda, P.; Awan, K.H. Reviewing the oral carcinogenic potential of E-cigarettes using the Bradford Hill criteria of causation. Transl. Cancer Res. 2020, 9, 3142–3152. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Hecht, S.S. DNA damage in human oral cells induced by use of e-cigarettes. Anal. Drug Test. 2023, 15, 1189–1197. [Google Scholar] [CrossRef]
- Ramôa, C.P.; Eissenberg, T.; Sahingur, S.E. Increasing popularity of waterpipe tobacco smoking and electronic cigarette use: Implications for oral healthcare. J. Periodontal. Res. 2017, 52, 813–823. [Google Scholar] [CrossRef]
- Ahluwalia, R.; Sharma, K.; Kaur Bindra, P.; Fatima, S. Vaping and oral health. Santosh Univ. J. Health Sci. 2020, 6, 1–4. [Google Scholar]
- Huilgol, P.; Bhatt, S.P.; Biligowda, N.; Wright, N.C.; Wells, J.M. Association of e-cigarette use with oral health: A population based cross-sectional questionnaire study. J. Public Health UK 2019, 41, 354–361. [Google Scholar] [CrossRef]
- Andrikopoulos, G.I.; Farsalinos, K.; Poulas, K. Electronic Nicotine Delivery Systems (ENDS) and Their Relevance in Oral Health. Toxics 2019, 7, 61. [Google Scholar] [CrossRef]
- Silva, G.M.D.; Silva, H.F.V.D.; Campos, I.J.D.O.; Medeiros, E.R.D.; Colares, D.F.; Guedes, T. Assessment of oral changes resulting from the use of electronic cigarettes: Literature review. Res. Soc. Dev. 2021, 8, 10. [Google Scholar] [CrossRef]
- Liu, Y.; Li, R.; Xue, X.; Xu, T.; Luo, Y.; Dong, Q.; Junchao, L.; Jingbo, L.; Yaping, P.; Dongmei, Z. Periodontal disease and Helicobacter pylori infection in oral cavity: A meta-analysis of 2727 participants mainly based on Asian studies. Clin. Oral. Investig. 2020, 24, 2175–2188. [Google Scholar] [CrossRef]
- Bardellini, E.; Amadori, F.; Conti, G.; Majorana, A. Oral mucosal lesions in electronic cigarettes consumers versus former smokers. Acta Odontol. Scand. 2018, 76, 226–228. [Google Scholar] [CrossRef] [PubMed]
- Murthy, V.H. E-Cigarette Use among Youth and Young Adults: A Major Public Health Concern. JAMA Pediatr. 2017, 171, 209–210. [Google Scholar] [CrossRef] [PubMed]
- McCausland, K.; Maycock, B.; Leaver, T.; Jancey, J. The Messages Presented in Electronic Cigarette-Related Social Media Promotions and Discussion: Scoping Review. J. Med. Internet Res. 2019, 5, 21–22. [Google Scholar] [CrossRef] [PubMed]
- Walley, S.C.; Wilson, K.M.; Winickoff, J.P.; Groner, J. A Public Health Crisis: Electronic Cigarettes, Vape, and JUUL. Pediatrics 2019, 143, 6. [Google Scholar] [CrossRef]
- Abrams, D.; Glasser, A.M.; Pearson, J.; Villanti, A.; Collins, L.K.; Niaura, R.S. Harm Minimization and Tobacco Control: Reframing Societal Views of Nicotine Use to Rapidly Save Lives. Annu. Rev. Public Health 2018, 39, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Bellisario, A.; Bourbeau, K.; Crespo, D.; DeLuzio, N.; Ferro, A.; Sanchez, A.; Jackson, T.; Kunath-Tiburzi, G.; D’Antoni, A.V. An Observational Study of Vaping Knowledge and Perceptions in a Sample of U.S. Adults. Cureu 2020, 24, 12–16. [Google Scholar] [CrossRef]
- Fenech, A.; Baatjes, N.; Gunasuntharam, K. Fifteen-minute consultation: What paediatricians need to know about vaping. Arch. Dis. Child Educ. Pract. Ed. 2022, 20, 22–32. [Google Scholar] [CrossRef]
| Number | Author (Year of Publication) | Full Title | Summary and Conclusions |
|---|---|---|---|
| 1 | Javed et al. (2017) [16] | Comparison of periodontal parameters and self-perceived oral symptoms among cigarettes smokers, individuals vaping electronic cigarettes, and never-smokers | The study compared periodontal parameters and self-perceived oral symptoms between cigarettes smokers, individuals using e-cigarettes, and non-smokers. The study concluded that the periodontal inflammation and self-perceived oral symptoms were poorer among cigarette smokers than among vaping individuals. |
| 2 | Ghazali et al. (2018) [17] | Oral health of smokers and e-cigarette users: A case-control study | The study compares the oral health of cigarette, e-cigarette, and vape smokers and non-smokers. The study concluded that e-cigarettes have potentially detrimental effects on oral health. |
| 3 | Ye et al. (2020) [18] | Inflammatory biomarkers and growth factors in saliva and gingival crevicular fluid of e-cigarette users, cigarette smokers, and dual smokers: A pilot study | The study was on inflammatory biomarkers and growth factors in saliva and crevicular fluid of e-cigarette users, cigarette smokers, and both. In conclusion, smoking/vaping produces significant effects on oral health. |
| 4 | Jeong et al. (2020) [19] | Associations of electronic and conventional cigarette use with periodontal disease in South Korean adults | The study examines the associations of e-cigarette and conventional cigarette use with periodontal disease in South Korean adults. They concluded that smoking and vaping produce incremented rates of periodontal disease. |
| 5 | Velmulapalli et al. (2021) [20] | Association between vaping and untreated caries A cross-sectional study of National Health and Nutrition Examination Survey 2017–2018 data | The study examines the relationship between vaping and the presence of untreated cavities. In conclusion, both vaping and dual smoking are associated with an increased occurrence of untreated caries. |
| 6 | Irusa et al. (2022) [21] | A comparison of the caries risk between patients who use vapes or electronic cigarettes and those who do not: A cross-sectional study | The study deals with the risk of tooth decay associated with vaping. The authors concluded that vaping patients had a higher risk of developing caries. |
| 7 | Ramenzoni et al. (2022) [22] | Cytotoxic and inflammatory effects of electronic and traditional cigarettes on oral gingival cells using a novel automated smoking instrument: An in vitro study | The study investigated the effects of e-cigarettes and traditional cigarettes on oral gingival cells using a novel automated smoking instrument. The conclusions drawn stated that e-cig smoking may contribute to the cell damage of oral tissue and tissue inflammation. |
| 8 | Xu et al. (2022) [23] | Mechanistic effects of e-liquids on biofilm formation and growth of oral commensal streptococcal communities: Effect of flavoring agents | The mechanistic effects of e-liquids on biofilm formation and the growth of oral commensal streptococcal communities were investigated. The findings of the study indicate that flavored e-liquids have a more detrimental impact on the formation and growth of oral commensal bacteria compared to unflavored e-liquids. |
| Number | Author (Year of Publication) | Number of Patients | Gender (M: Male//F: Female) (Number of Cases) | Age (Mean Age/Age Range) |
|---|---|---|---|---|
| 1 | Javed et al. (2017) [16] | 94 | M (94) | Mean age: 39.87 ± 2.17 years |
| 2 | Ghazali et al. (2018) [17] | 120 | M (89)//F (31) | Mean age: 27.66 ± 7.58 |
| 3 | Ye et al. (2020) [18] | 48 | M (24)//F (24) | Mean age: 37.56 ± 13.03 years |
| 4 | Jeong et al. (2020) [19] | 13,551 | M (5715)//F (7836) | Mean age: 29.18 ± 4.24 years |
| 5 | Velmulapalli et al. (2021) [20] | 4618 | M (2234)//F (2384) | Mean age: 41.81 ± 6.11 years |
| 6 | Irusa et al. (2022) [21] | 13,216 | M (6321)//F (6895) | Age range Age: 16–25 years—845 patients Age: 26–40 years—4336 patients Age: >40 years—8014 patients |
| 7 | Ramenzoni et al. (2022) [22] | No data | No data | No data |
| 8 | Xu et al. (2022) [23] | No data | No data | No data |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iacob, A.M.; Escobedo Martínez, M.F.; Barbeito Castro, E.; Junquera Olay, S.; Olay García, S.; Junquera Gutiérrez, L.M. Effects of Vape Use on Oral Health: A Review of the Literature. Medicina 2024, 60, 365. https://doi.org/10.3390/medicina60030365
Iacob AM, Escobedo Martínez MF, Barbeito Castro E, Junquera Olay S, Olay García S, Junquera Gutiérrez LM. Effects of Vape Use on Oral Health: A Review of the Literature. Medicina. 2024; 60(3):365. https://doi.org/10.3390/medicina60030365
Chicago/Turabian StyleIacob, Alin M., Matías F. Escobedo Martínez, Enrique Barbeito Castro, Sonsoles Junquera Olay, Sonsoles Olay García, and Luis Manuel Junquera Gutiérrez. 2024. "Effects of Vape Use on Oral Health: A Review of the Literature" Medicina 60, no. 3: 365. https://doi.org/10.3390/medicina60030365
APA StyleIacob, A. M., Escobedo Martínez, M. F., Barbeito Castro, E., Junquera Olay, S., Olay García, S., & Junquera Gutiérrez, L. M. (2024). Effects of Vape Use on Oral Health: A Review of the Literature. Medicina, 60(3), 365. https://doi.org/10.3390/medicina60030365








