High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair
Abstract
1. Introduction
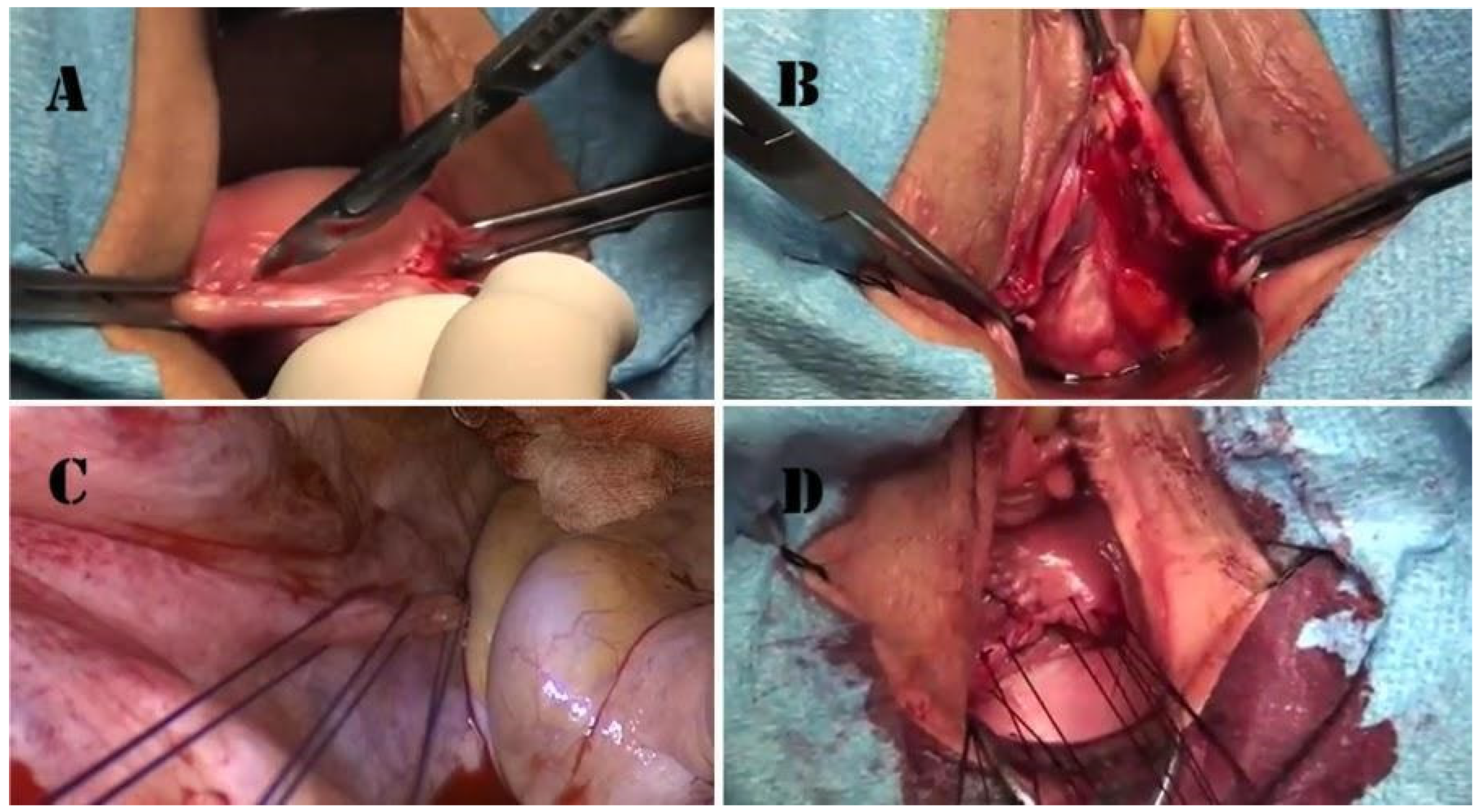
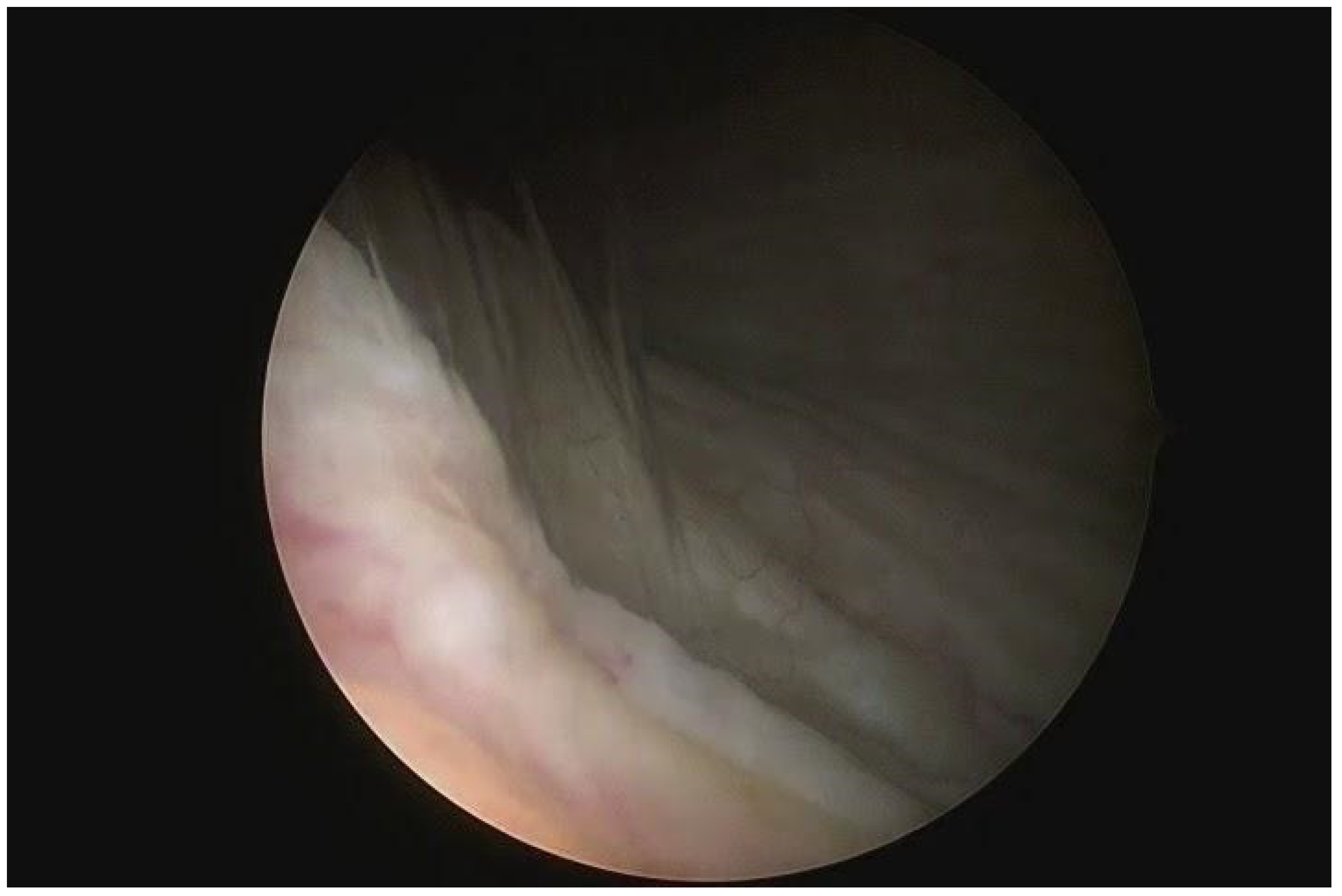
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Altman, D.; Falconer, C.; Cnattingius, S.; Granath, F. Pelvic organ prolapse surgery following hysterectomy on benign indications. Am. J. Obstet. Gynecol. 2008, 198, 572.e1–572.e6. [Google Scholar] [CrossRef]
- Slieker-ten Hove, M.C.; Pool-Goudzwaard, A.L.; Eijkemans, M.J.; Steegers-Theunissen, R.P.; Burger, C.W.; Vierhout, M.E. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2009, 20, 1037–1045. [Google Scholar] [CrossRef]
- Brunes, M.; Ek, M.; Drca, A.; Söderberg, M.; Bergman, I.; Warnqvist, A.; Johannesson, U. Vaginal vault prolapse and recurrent surgery: A nationwide observational cohort study. Acta Obstet. Gynecol. Scand. 2022, 101, 542–549. [Google Scholar] [CrossRef]
- Deo, G.; Bernasconi, D.P.; Cola, A.; Palmieri, S.; Spelzini, F.; Milani, R.; Manodoro, S.; Frigerio, M. Long-term outcomes and five-year recurrence-free survival curves after native-tissue prolapse repair. Int. J. Gynaecol. Obstet. 2019, 147, 238–245. [Google Scholar] [CrossRef]
- Manodoro, S.; Frigerio, M.; Cola, A.; Spelzini, F.; Milani, R. Risk factors for recurrence after hysterectomy plus native-tissue repair as primary treatment for genital prolapse. Int. Urogynecol. J. 2018, 29, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Manodoro, S.; Spelzini, F.; Cesana, M.C.; Frigerio, M.; Maggioni, D.; Ceresa, C.; Penati, C.; Sicuri, M.; Fruscio, R.; Nicolini, G.; et al. Histologic and metabolic assessment in a cohort of patients with genital prolapse: Preoperative stage and recurrence investigations. Minerva Ginecol. 2017, 69, 233–238. [Google Scholar] [CrossRef]
- Robinson, D.; Thiagamoorthy, G.; Cardozo, L. Post-hysterectomy vaginal vault prolapse. Maturitas 2018, 107, 39–43. [Google Scholar] [CrossRef]
- Vermeulen, C.K.M.; Veen, J.; Adang, C.; van Leijsen, S.A.L.; Coolen, A.L.W.M.; Bongers, M.Y. Pelvic organ prolapse after laparoscopic hysterectomy compared with vaginal hysterectomy: The POP-UP study. Int. Urogynecol. J. 2021, 32, 841–850. [Google Scholar] [CrossRef]
- Swift, S. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am. J. Obstet. Gynecol. 2000, 183, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Mant, J.; Painter, R.; Vessey, M. Epidemiology of genital prolapse: Observations from the Oxford family planning association study. BJOG 1997, 104, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Marchianni, M.; Bracco, G.L.; Checcucci, V.; Carabaneanu, A.; Coccia, E.M.; Mecacci, F.; Scarselli, G. True incidence of vaginal vault prolapse: Thirteen years of experience. J. Reprod. Med. 1999, 44, 678–684. [Google Scholar]
- Coolen, A.W.M.; van IJsselmuiden, M.N.; van Oudheusden, A.M.J.; Veen, J.; van Eijndhoven, H.W.F.; Mol, B.W.J.; Roovers, J.P.; Bongers, M.Y. Laparoscopic sacrocolpopexy versus vaginal sacrospinous fixation for vaginal vault prolapse, a randomized controlled trial: SALTO-2 trial, study protocol. BMC Womens Health 2017, 17, 52. [Google Scholar] [CrossRef] [PubMed]
- Brubaker, L.; Maher, C.; Jacquetin, B.; Rajamaheswari, N.; von Theobald, P.; Norton, P. Surgery for pelvic organ prolapse. Female Pelvic Med. Reconstr. Surg. 2010, 16, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Nygaard, I.E.; McCreery, R.; Brubaker, L.; Connolly, A.; Cundiff, G.; Weber, A.M.; Zyczynski, H.; Pelvic Floor Disorders Network. Abdominal sacrocolpopexy: A comprehensive review. Obstet. Gynecol. 2004, 104, 805–823. [Google Scholar] [CrossRef] [PubMed]
- Hilger, W.S.; Poulson, M.; Norton, P.A. Long-term results of abdominal sacrocolpopexy. Am. J. Obstet. Gynecol. 2003, 189, 1606–1610. [Google Scholar] [CrossRef] [PubMed]
- Price, N.; Jackson, S.R. Advances in laparoscopic techniques in pelvic reconstructive surgery for prolapse and incontinence. Maturitas 2009, 62, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Paraiso, M.F.; Falcone, T.; Walters, M.D. Laparoscopic surgery for enterocele, vaginal apex prolapse and rectocele. Int. Urogynecol. J. Pelvic Floor Dysfunct 1999, 10, 223–229. [Google Scholar] [CrossRef]
- Geller, E.J.; Parnell, B.A.; Dunivan, G.C. Pelvic floor function before and after robotic sacrocolpopexy: One year outcomes. J. Minim. Gynecol. 2011, 18, 322–327. [Google Scholar] [CrossRef]
- Wattiez, A.; Mashiach, R.; Donoso, M. Laparoscopic repair of vaginal vault prolapse. Curr. Opin. Obstet. Gynecol. 2003, 15, 315–319. [Google Scholar] [CrossRef]
- Klauschie, J.L.; Cornella, J.L. Surgical treatment of vaginal vault prolapse: A historic summary and review of outcomes. Female Pelvic Med. Reconstr. Surg. 2012, 18, 10–17. [Google Scholar] [CrossRef]
- Collins, S.; Lewicky-Gaupp, C. Pelvic Organ Prolapse. Gastroenterol. Clin. N. Am. 2022, 51, 177–193. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.; Feiner, B.; Baessler, K.; Christmann-Schmid, C.; Haya, N.; Marjoribanks, J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst. Rev. 2016, 2, CD012079. [Google Scholar] [CrossRef] [PubMed]
- Cola, A.P.; Marino, G.; Milani, R.; Barba, M.; Volontè, S.; Spelzini, F.; Manodoro, S.; Frigerio, M. Native-tissue prolapse repair: Efficacy and adverse effects of uterosacral ligaments suspension at 10-year follow up. Int. J. Gynecol. Obstet. 2022, 159, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Schimpf, M.O.; Abed, H.; Sanses, T.; White, A.B.; Lowenstein, L.; Ward, R.M.; Sung, V.W.; Balk, E.M.; Murphy, M.; Society of Gynecologic Surgeons Systematic Review Group. Graft and Mesh Use in Transvaginal Prolapse Repair: A Systematic Review. Obstet. Gynecol. 2016, 128, 81–91. [Google Scholar] [CrossRef]
- Sederl, J. Zur Operation des Prolapses der blind endigenden Schiede [Surgery in prolapse of a blind-end vagina]. Geburtshilfe Frauenheilkd. 1958, 18, 824–828. (In German) [Google Scholar]
- Yazdany, T.; Wong, K.; Bhatia, N.N. Sacrospinous ligament fixation for pelvic organ prolapse in the era of vaginal mesh kits. Curr. Opin. Obstet. Gynecol. 2011, 23, 391–395. [Google Scholar] [CrossRef]
- Milani, R.; Frigerio, M.; Manodoro, S. Transvaginal sacrospinous ligament fixation for posthysterectomy vaginal vault prolapse repair. Int. Urogynecol. J. 2017, 28, 1103–1105. [Google Scholar] [CrossRef]
- Leron, E.; Erez, O.; Shwarzmam, P.; Baessler, K. Sacrospinous ligament fixation (SSLF): An old method with new horizons. Arch. Gynecol. Obstet. 2022, 305, 1379–1382. [Google Scholar] [CrossRef]
- Smilen, S.W.; Saini, J.; Wallach, S.J.; Porges, R.F. The risk of cystocele after sacrospinous ligament fixation. Am. J. Obstet. Gynecol. 1998, 179 Pt 1, 1465–1472. [Google Scholar] [CrossRef]
- Holley, R.L.; Varner, R.E.; Gleason, B.P.; Apffel, L.A.; Scott, S. Recurrent pelvic support defects after sacrospinous ligament fixation for vaginal vault prolapse. J. Am. Coll. Surg. 1995, 180, 444–448. [Google Scholar]
- Inmon, W.B. Pelvic relaxation and repair including prolapse of vagina following hysterectomy. South Med. J. 1963, 56, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Shull, B.L.; Capen, C.V.; Riggs, M.W.; Kuehl, T.J. Bilateral attachment of the vaginal cuff to iliococcygeus fascia: An effective method of cuff suspension. Am. J. Obstet. Gynecol. 1993, 168 Pt 1, 1669–1677. [Google Scholar] [CrossRef] [PubMed]
- Milani, R.; Frigerio, M.; Spelzini, F.; Manodoro, S. Transvaginal iliococcygeus fixation for posthysterectomy vaginal vault prolapse repair. Int. Urogynecol. J. 2017, 28, 1599–1601. [Google Scholar] [CrossRef] [PubMed]
- Milani, R.; Frigerio, M.; Vellucci, F.L.; Palmieri, S.; Spelzini, F.; Manodoro, S. Transvaginal native-tissue repair of vaginal vault prolapse. Minerva Ginecol. 2018, 70, 371–377. [Google Scholar] [CrossRef]
- Webb, M.J.; Aronson, M.P.; Ferguson, L.K.; Lee, R.A. Posthysterectomy vaginal vault prolapse: Primary repair in 693 patients. Obstet. Gynecol. 1998, 92, 281–285. [Google Scholar] [CrossRef]
- Sze, E.H.; Karram, M.M. Transvaginal repair of vault prolapse: A review. Obstet. Gynecol. 1997, 89, 466–475. [Google Scholar] [CrossRef]
- Francis, W.J.; Jeffcoate, T.N. Dyspareunia following vaginal operations. J. Obstet. Gynaecol. Br. Commonw. 1961, 68, 1–10. [Google Scholar] [CrossRef]
- Milani, R.; Manodoro, S.; Cola, A.; Palmieri, S.; Frigerio, M. Transvaginal levator myorrhaphy for posthysterectomy vaginal vault prolapse repair. Int. Urogynecol. J. 2018, 29, 913–915. [Google Scholar] [CrossRef]
- Natale, F.; La Penna, C.; Padoa, A.; Panei, M.; Cervigni, M. High levator myorrhaphy for transvaginal suspension of the vaginal apex: Long-term results. J. Urol. 2008, 180, 2047–2052, discussion 2052. [Google Scholar] [CrossRef]
- Milani, R.; Manodoro, S.; Cola, A.; Bellante, N.; Palmieri, S.; Frigerio, M. Transvaginal uterosacral ligament hysteropexy versus hysterectomy plus uterosacral ligament suspension: A matched cohort study. Int. Urogynecol. J. 2020, 31, 1867–1872. [Google Scholar] [CrossRef]
- Milani, R.; Frigerio, M.; Spelzini, F.; Manodoro, S. Transvaginal uterosacral ligament hysteropexy: A video tutorial. Int. Urogynecol. J. 2017, 28, 789–791. [Google Scholar] [CrossRef]
- Milani, R.; Manodoro, S.; Cola, A.; Palmieri, S.; Reato, C.; Frigerio, M. Transvaginal native-tissue repair of enterocele. Int. Urogynecol. J. 2018, 29, 1705–1707. [Google Scholar] [CrossRef]
- Spelzini, F.; Frigerio, M.; Manodoro, S.; Interdonato, M.L.; Cesana, M.C.; Verri, D.; Fumagalli, C.; Sicuri, M.; Nicoli, E.; Polizzi, S.; et al. Modified McCall culdoplasty versus Shull suspension in pelvic prolapse primary repair: A retrospective study. Int. Urogynecol. J. 2017, 28, 65–71. [Google Scholar] [CrossRef]
- Bump, R.C.; Mattiasson, A.; Bø KBrubaker, L.P.; DeLancey, J.O.; Klarskov, P.; Shull, B.L.; Smith, A.R. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J. Obstet. Gynecol. 1996, 175, 10–17. [Google Scholar] [CrossRef]
- Shull, B.L.; Bachofen, C.; Coates, K.W.; Kuehl, T.J. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am. J. Obstet. Gynecol. 2000, 183, 1365–1373; discussion 1373–1374. [Google Scholar] [CrossRef]
- Cola, A.; Barba, M.; Frigerio, M. Intraoperative ultrasound assessment of ureteral patency during pelvic surgery. Int. Urogynecol. J. 2021, 32, 3313–3315. [Google Scholar] [CrossRef]
- Frigerio, M.; Barba, M.; Marino, G.; Volontè, S.; Cola, A. Intraoperative ultrasound assessment of ureteral patency after uterosacral ligaments apical suspension for prolapse surgical repair: A feasibility study. Int. J. Gynaecol. Obstet. 2023, 163, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Yalcin, I.; Bump, R.C. Validation of two global impression questionnaires for incontinence. Am. J. Obstet. Gynecol. 2003, 189, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Srikrishna, S.; Robinson, D.; Cardozo, L. Validation of the Patient Global Impression of Improvement (PGI-I) for urogenital prolapse. Int. Urogynecol. J. 2010, 21, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Campbell, P.; Cloney, L.; Jha, S. Abdominal Versus Laparoscopic Sacrocolpopexy. Obstet. Gynecol. Surv. 2016, 71, 435–442. [Google Scholar] [CrossRef]
- Zhang, W.; Cheon, W.C.; Zhang, L.; Wang, X.; Wei, Y.; Lyu, C. Comparison of the effectiveness of sacrospinous ligament fixation and sacrocolpopexy: A meta-analysis. Int. Urogynecol. J. 2022, 33, 3–13. [Google Scholar] [CrossRef]
| Age (Years) | 64.8 ± 9.6 |
|---|---|
| Parity (n) | 2.0 ± 0.8 |
| Menopausal status | 45 (95.7%) |
| BMI (Kg/m2) | 27.0 ± 6.1 |
| ASA status 1 | 4 (8.5%) |
| ASA status 2 | 35 (74.5%) |
| ASA status 3 | 8 (17.0%) |
| Indication for previous hysterectomy | 27 (57.4%) Uterovaginal prolapse |
| 20 (42.6%) Other benign indications |
| High Uterosacral Ligaments Suspension | 47 (100%) |
|---|---|
| Anterior repair | 33 (70.2%) |
| Posterior repair | 28 (59.6%) |
| Blood loss (mL) | 184 ± 126 |
| Operative time (min) | 82 ± 26 |
| Intraoperative complications | 0 |
| Postoperative complications | 1 (2.1%) * |
| Anatomic Recurrence | 8 (24.2%) |
|---|---|
| 7 (21.2%) |
| 2 (6.0%) |
| 1 (3.0%) |
| Reoperation | 0 (0%) |
| Postoperative bulging symptoms | 4 (12.1%) |
| PGI-I | 1.6 ± 0.8 |
| Preoperative | Postoperative | p-Value | |
|---|---|---|---|
| Aa | 1.1 ± 1.7 | −1.8 ± 1.2 | <0.001 |
| Ba | 1.3 ± 1.9 | −1.8 ± 1.2 | <0.001 |
| C | 1.2 ± 2.7 | −5.3 ± 2.7 | <0.001 |
| gh | 4.1 ± 0.7 | 3.6 ± 0.6 | <0.001 |
| pb | 2.8 ± 0.5 | 3.1 ± 0.5 | 0.01 |
| tvl | 8.6 ± 1.0 | 8.1 ± 1.2 | 0.004 |
| Ap | −1.7 ± 1.4 | −2.7 ± 0.6 | <0.001 |
| Bp | −1.5 ± 1.6 | −2.7 ± 0.6 | <0.001 |
| Preoperative | Postoperative | p-Value | |
|---|---|---|---|
| Stress urinary incontinence | 16 (34.0%) | 6 (18.2%) | 0.135 |
| Voiding symptoms | 29 (61.7%) | 6 (18.2%) | <0.001 |
| Overactive bladder syndrome | 18 (38.3%) | 10 (30.3%) | 0.486 |
| Constipation | 13 (27.7%) | 11 (33.3%) | 0.626 |
| Bulging symptoms | 47 (100%) | 4 (12.1%) | <0.001 |
| Sexual activity | 15 (31.9%) | 10 (30.3%) | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barba, M.; Cola, A.; Melocchi, T.; De Vicari, D.; Costa, C.; Volontè, S.; Sandullo, L.; Frigerio, M. High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair. Medicina 2024, 60, 320. https://doi.org/10.3390/medicina60020320
Barba M, Cola A, Melocchi T, De Vicari D, Costa C, Volontè S, Sandullo L, Frigerio M. High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair. Medicina. 2024; 60(2):320. https://doi.org/10.3390/medicina60020320
Chicago/Turabian StyleBarba, Marta, Alice Cola, Tomaso Melocchi, Desirèe De Vicari, Clarissa Costa, Silvia Volontè, Lucia Sandullo, and Matteo Frigerio. 2024. "High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair" Medicina 60, no. 2: 320. https://doi.org/10.3390/medicina60020320
APA StyleBarba, M., Cola, A., Melocchi, T., De Vicari, D., Costa, C., Volontè, S., Sandullo, L., & Frigerio, M. (2024). High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair. Medicina, 60(2), 320. https://doi.org/10.3390/medicina60020320







