Catheter Ablation of Atrial Tachycardia after Pulmonary Vein Isolation in a Patient with Common Ostium of Inferior Pulmonary Veins: Case Report
Abstract
1. Introduction
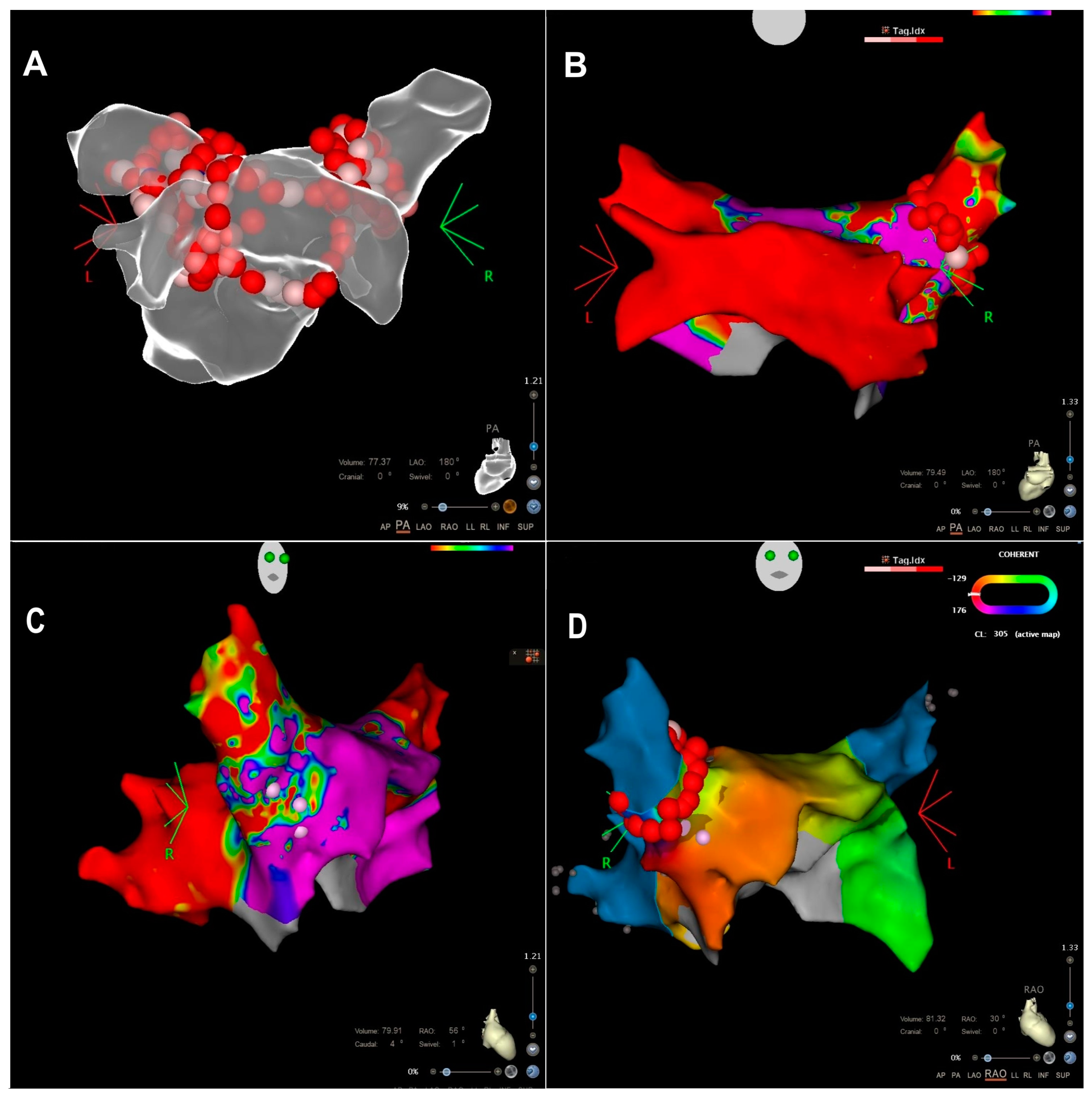
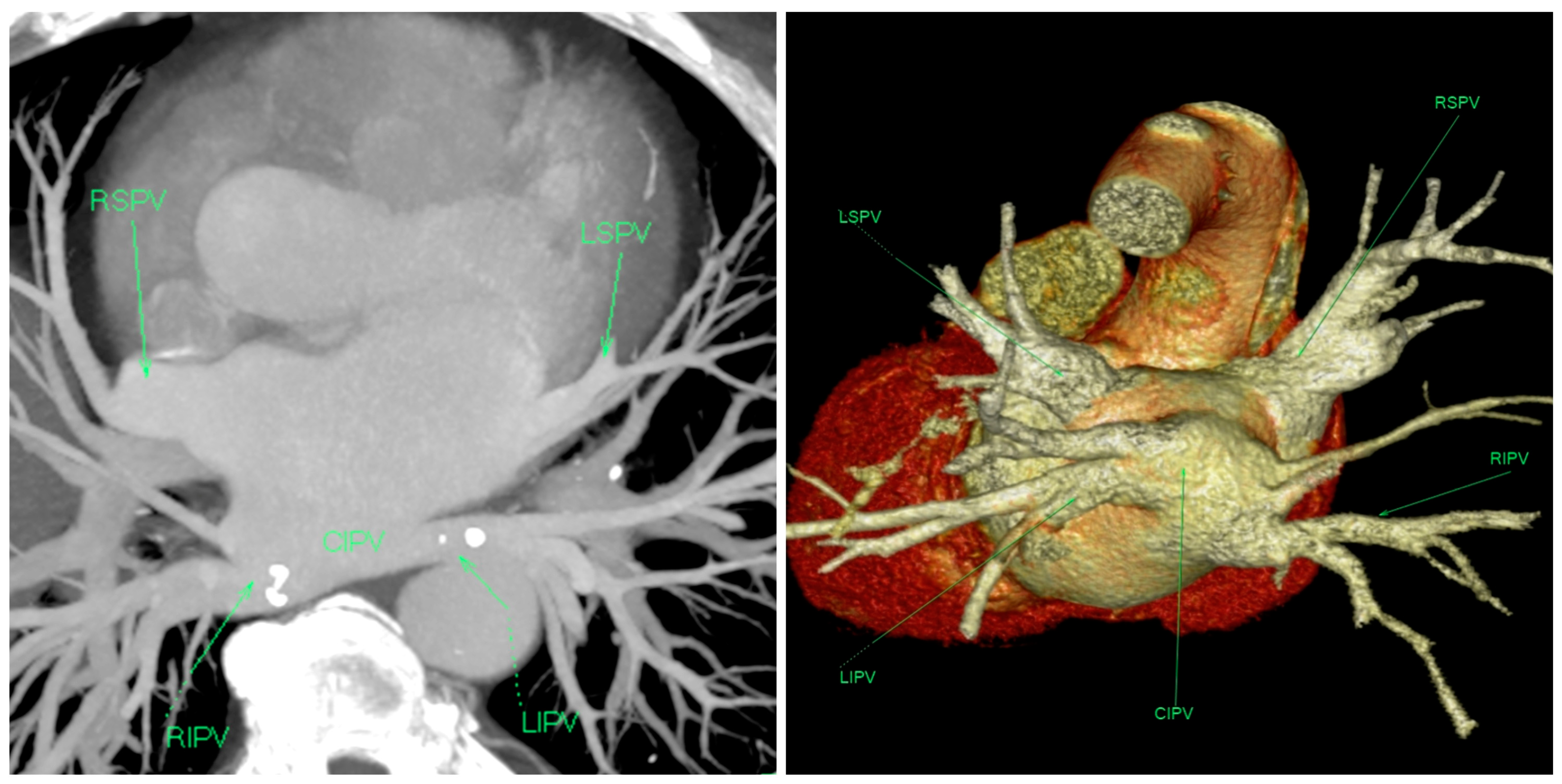
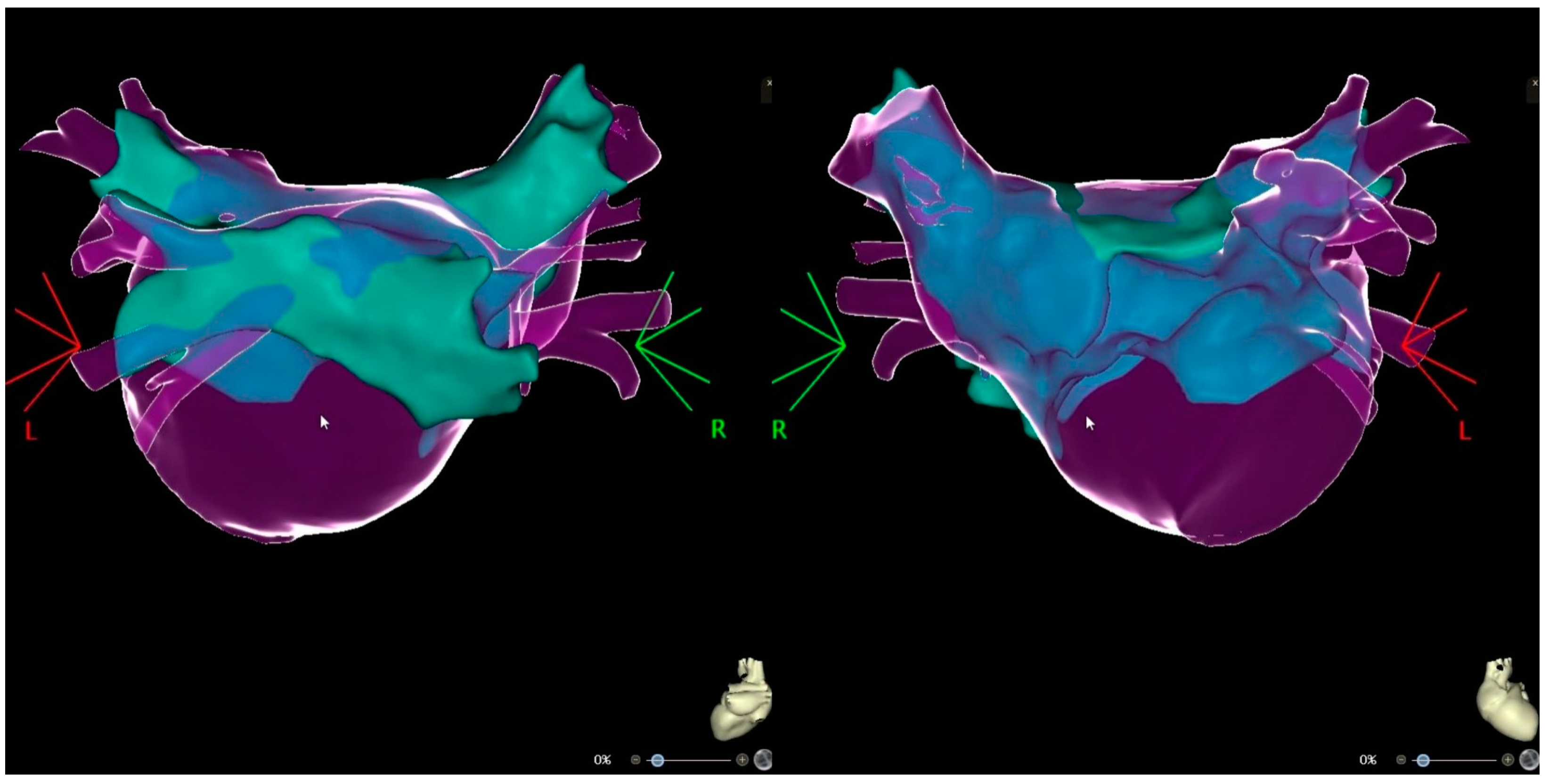
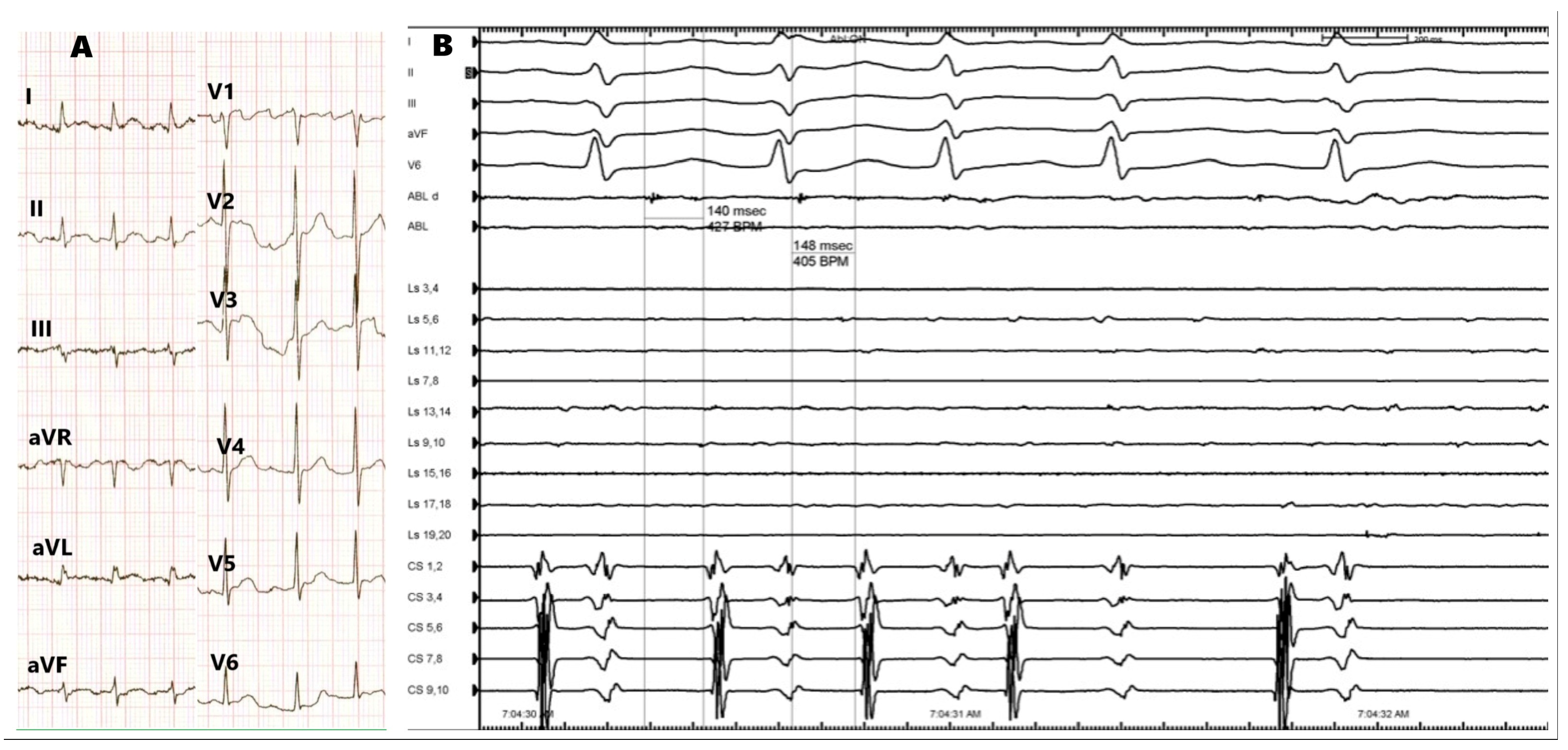
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Calkins, H.; Hindricks, G.; Cappato, R.; Kim, Y.-H.; Saad, E.B.; Aguinaga, L.; Akar, J.G.; Badhwar, V.; Brugada, J.; Camm, J.; et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm 2017, 14, e275–e444. [Google Scholar] [CrossRef] [PubMed]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef] [PubMed]
- Benali, K.; Lai, V.D.; Hammache, N.; Magnin-Poull, I.; de Chillou, C.; Sellal, J.M. Impact of pulmonary veins anatomy on the outcomes of radiofrequency ablation for paroxysmal atrial fibrillation in the era of contact force-sensing ablation catheters. J Interv. Card. Electrophysiol. 2023, 66, 931–940. [Google Scholar] [CrossRef] [PubMed]
- McLellan, A.J.A.; Ling, L.; Ruggiero, D.; Wong, M.C.G.; Walters, T.E.; Nisbet, A.; Shetty, A.K.; Azzopardi, S.; Taylor, A.J.; Morton, J.B.; et al. Pulmonary vein isolation: The impact of pulmonary venous anatomy on long-term outcome of catheter ablation for paroxysmal atrial fibrillation. Heart Rhythm 2014, 11, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Li, J.H.; Xie, H.Y.; Sun, Q.; Guo, X.G.; Chen, Y.Q.; Cao, Z.J.; Ma, J. Comparison of Using Second-Generation Cryoballoon and Radiofrequency Catheter for Atrial Fibrillation Ablation in Patients With the Common Ostium of Inferior Pulmonary Veins. Front. Cardiovasc. Med. 2022, 8, 794834. [Google Scholar] [CrossRef] [PubMed]
- Xie, H.Y.; Guo, X.G.; Yang, J.D.; Li, J.H.; Chen, Y.Q.; Cao, Z.J.; Sun, Q.; Li, X.Y.; Ma, J. Safety and Efficacy Using the Second-Generation Cryoballoon in Patients With Atrial Fibrillation and a Common Ostium of Inferior Pulmonary Veins. Front. Cardiovasc. Med. 2021, 8, 683315. [Google Scholar] [CrossRef] [PubMed]
- Kanaji, Y.; Miyazaki, S.; Iwasawa, J.; Ichihara, N.; Takagi, T.; Kuroi, A.; Nakamura, H.; Taniguchi, H.; Hachiya, H.; Iesaka, Y. Pre-procedural evaluation of the left atrial anatomy in patients referred for catheter ablation of atrial fibrillation. J Cardiol. 2016, 67, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Canpolat, U.; Yorgun, H.; Hazirolan, T.; Aytemir, K. Common ostium of inferior pulmonary veins: An extremely rare variant described by preprocedural computerized tomography angiography. J. Arrhythm. 2021, 19, 450–451. [Google Scholar] [CrossRef] [PubMed]
- Maalouf, J.; Whiteside, H.L.; Pillai, A.; Omar, A.; Berman, A.; Saba, S.; Hreibe, H. Reduction of radiation and contrast agent exposure in a cryoballoon ablation procedure with integration of electromagnetic mapping and intracardiac echocardiography: A single center experience. J. Interv. Card. Electrophysiol. 2020, 59, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Mittal, A.; Fitzpatrick, N.; Szeplaki, G. Pulsed field ablation in common inferior pulmonary trunk. J. Interv. Card. Electrophysiol. 2023, 66, 809–810. [Google Scholar] [CrossRef] [PubMed]
- Nattel, S.; Burstein, B.; Dobrev, D. Atrial remodeling and atrial fibrillation: Mechanisms and implications. Circ. Arrhythm. Electrophysiol. 2008, 1, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Hung, Y.; Chang, S.L.; Lin, W.S.; Lin, W.Y.; Chen, S.A. Atrial Tachycardias after Atrial Fibrillation Ablation: How to Manage? Arrhythm. Electrophysiol. Rev. 2020, 9, 54–60. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Babic, M.; Djurdjevic, B.; Vukajlovic, D.; Jovicic, M.; Petrovic, M.; Kljajevic, J.; Tomovic, M.; Nikolic, A. Catheter Ablation of Atrial Tachycardia after Pulmonary Vein Isolation in a Patient with Common Ostium of Inferior Pulmonary Veins: Case Report. Medicina 2024, 60, 264. https://doi.org/10.3390/medicina60020264
Babic M, Djurdjevic B, Vukajlovic D, Jovicic M, Petrovic M, Kljajevic J, Tomovic M, Nikolic A. Catheter Ablation of Atrial Tachycardia after Pulmonary Vein Isolation in a Patient with Common Ostium of Inferior Pulmonary Veins: Case Report. Medicina. 2024; 60(2):264. https://doi.org/10.3390/medicina60020264
Chicago/Turabian StyleBabic, Milos, Branko Djurdjevic, Dejan Vukajlovic, Mihailo Jovicic, Masa Petrovic, Jelena Kljajevic, Milosav Tomovic, and Aleksandra Nikolic. 2024. "Catheter Ablation of Atrial Tachycardia after Pulmonary Vein Isolation in a Patient with Common Ostium of Inferior Pulmonary Veins: Case Report" Medicina 60, no. 2: 264. https://doi.org/10.3390/medicina60020264
APA StyleBabic, M., Djurdjevic, B., Vukajlovic, D., Jovicic, M., Petrovic, M., Kljajevic, J., Tomovic, M., & Nikolic, A. (2024). Catheter Ablation of Atrial Tachycardia after Pulmonary Vein Isolation in a Patient with Common Ostium of Inferior Pulmonary Veins: Case Report. Medicina, 60(2), 264. https://doi.org/10.3390/medicina60020264





