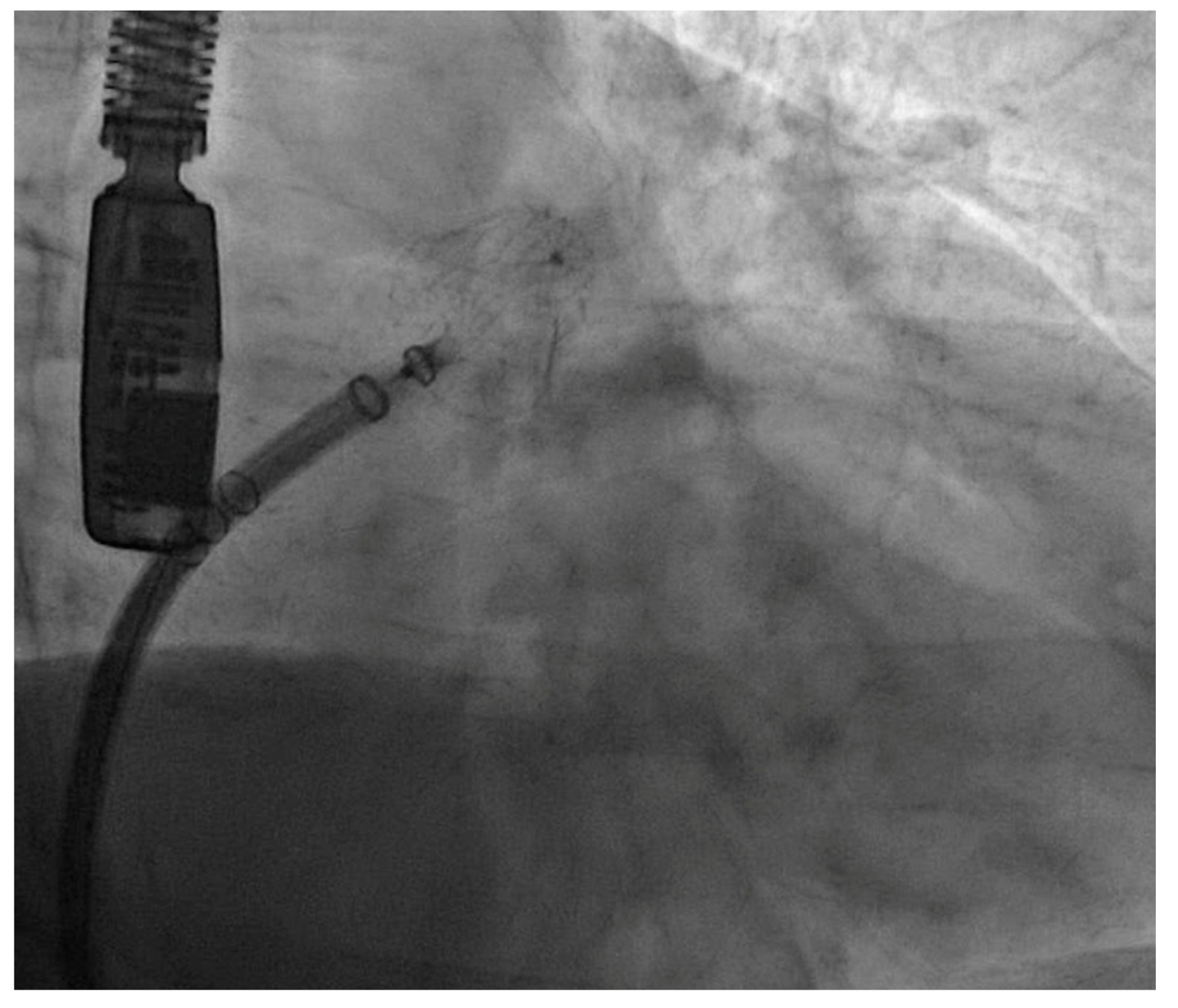
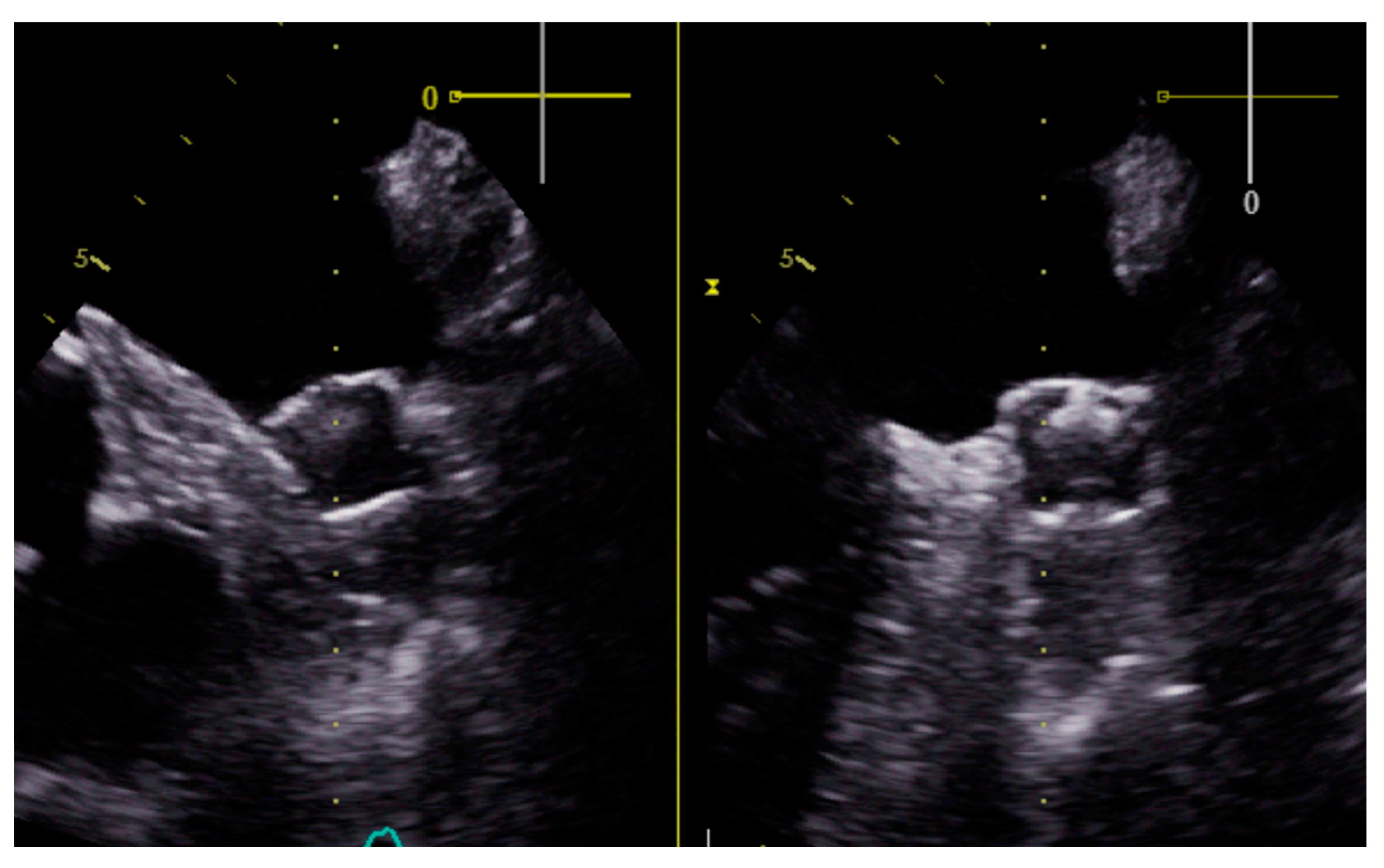
Percutaneous Left Atrial Appendage Closure in Patients with Non-Valvular Atrial Fibrillation and End-Stage Renal Disease on Hemodialysis: A Case Series
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baber, U.; Howard, V.J.; Halperin, J.L.; Soliman, E.Z.; Zhang, X.; McClellan, W.; Warnock, D.G.; Muntner, P. Association of Chronic Kidney Disease With Atrial Fibrillation Among Adults in the United States: REasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Circ. Arrhythmia Electrophysiol. 2011, 4, 26–32. [Google Scholar] [CrossRef]
- Genovesi, S.; Pogliani, D.; Faini, A.; Valsecchi, M.G.; Riva, A.; Stefani, F.; Acquistapace, I.; Stella, A.; Bonforte, G.; DeVecchi, A.; et al. Prevalence of Atrial Fibrillation and Associated Factors in a Population of Long-Term Hemodialysis Patients. Am. J. Kidney Dis. 2005, 46, 897–902. [Google Scholar] [CrossRef]
- Go, A.S.; Fang, M.C.; Udaltsova, N.; Chang, Y.; Pomernacki, N.K.; Borowsky, L.; Singer, D.E. Impact of Proteinuria and Glomerular Filtration Rate on Risk of Thromboembolism in Atrial Fibrillation: The Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. Circulation 2009, 119, 1363–1369. [Google Scholar] [CrossRef]
- Winkelmayer, W.C.; Patrick, A.R.; Liu, J.; Brookhart, M.A.; Setoguchi, S. The Increasing Prevalence of Atrial Fibrillation among Hemodialysis Patients. J. Am. Soc. Nephrol. 2011, 22, 349–357. [Google Scholar] [CrossRef]
- Bansal, N.; Fan, D.; Hsu, C.; Ordonez, J.D.; Marcus, G.M.; Go, A.S. Incident Atrial Fibrillation and Risk of End-Stage Renal Disease in Adults With Chronic Kidney Disease. Circulation 2013, 127, 569–574. [Google Scholar] [CrossRef]
- Zimmerman, D.; Sood, M.M.; Rigatto, C.; Holden, R.M.; Hiremath, S.; Clase, C.M. Systematic review and meta-analysis of incidence, prevalence and outcomes of atrial fibrillation in patients on dialysis. Nephrol. Dial. Transplant. 2012, 27, 3816–3822. [Google Scholar] [CrossRef]
- Bonde, A.N.; Lip, G.Y.H.; Kamper, A.-L.; Fosbøl, E.L.; Staerk, L.; Carlson, N.; Torp-Pedersen, C.; Gislason, G.; Olesen, J.B. Renal Function and the Risk of Stroke and Bleeding in Patients With Atrial Fibrillation: An Observational Cohort Study. Stroke 2016, 47, 2707–2713. [Google Scholar] [CrossRef] [PubMed]
- Ansari, N.; Manis, T.; Feinfeld, D.A. Symptomatic atrial arrhythmias in hemodialysis patients. Ren. Fail. 2001, 23, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Landray, M.J.; Wheeler, D.C.; Lip, G.Y.H.; Newman, D.J.; Blann, A.D.; McGlynn, F.J.; Ball, S.; Townend, J.N.; Baigent, C. Inflammation, endothelial dysfunction, and platelet activation in patients with chronic kidney disease: The chronic renal impairment in Birmingham (CRIB) study. Am. J. Kidney Dis. 2004, 43, 244–253. [Google Scholar] [CrossRef]
- Chung, M.K.; Martin, D.O.; Sprecher, D.; Wazni, O.; Kanderian, A.; Carnes, C.A.; Bauer, J.A.; Tchou, P.J.; Niebauer, M.J.; Natale, A.; et al. C-Reactive Protein Elevation in Patients With Atrial Arrhythmias: Inflammatory Mechanisms and Persistence of Atrial Fibrillation. Circulation 2001, 104, 2886–2891. [Google Scholar] [CrossRef] [PubMed]
- Kobori, H.; Nangaku, M.; Navar, L.G.; Nishiyama, A. The Intrarenal Renin-Angiotensin System: From Physiology to the Pathobiology of Hypertension and Kidney Disease. Pharmacol. Rev. 2007, 59, 251–287. [Google Scholar] [CrossRef]
- Yeyati, N.L.; Adrogué, H.J. Inappropriately High Plasma Renin Activity Accompanies Chronic Loss of Renal Function. Am. J. Nephrol. 1996, 16, 471–477. [Google Scholar] [CrossRef]
- Ruiz-Ortega, M.; Lorenzo, O.; Suzuki, Y.; Rupérez, M.; Egido, J. Proinflammatory actions of angiotensins. Curr. Opin. Nephrol. Hypertens. 2001, 10, 321–329. [Google Scholar] [CrossRef]
- Goette, A.; Staack, T.; Röcken, C.; Arndt, M.; Geller, J.C.; Huth, C.; Ansorge, S.; Klein, H.U.; Lendeckel, U. Increased expression of extracellular signal-regulated kinase and angiotensin-converting enzyme in human atria during atrial fibrillation. J. Am. Coll. Cardiol. 2000, 35, 1669–1677. [Google Scholar] [CrossRef]
- Pokorney, S.D.; Chertow, G.M.; Al-Khalidi, H.R.; Gallup, D.; Dignacco, P.; Mussina, K.; Bansal, N.; Gadegbeku, C.A.; Garcia, D.A.; Garonzik, S.; et al. Apixaban for Patients With Atrial Fibrillation on Hemodialysis: A Multicenter Randomized Controlled Trial. Circulation 2022, 146, 1735–1745. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; Dilaveris, P.E.; et al. Guía ESC 2020 sobre el diagnóstico y tratamiento de la fibrilación auricular, desarrollada en colaboración de la European Association of Cardio-Thoracic Surgery (EACTS). Rev. Española de Cardiol. 2021, 74, e1–e437. [Google Scholar] [CrossRef]
- Glikson, M.; Wolff, R.; Hindricks, G.; Mandrola, J.; Camm, A.J.; Lip, G.Y.H.; Fauchier, L.; Betts, T.R.; Lewalter, T.; Saw, J.; et al. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion—An update. EuroIntervention 2020, 15, 1133–1180. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.-C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed]
- Sánchez González, C.; Herrero Calvo, J.A. Anticoagulantes Orales en la Enfermedad Renal Crónica; Lorenzo, V., López Gómez, J.M., Eds.; Nefrología al día; Spanish Society of Nephrology; Elsevier: Barcelona, Spain, 2023; ISSN 2659-2606. Available online: https://www.nefrologiaaldia.org/578 (accessed on 6 March 2023).
- Chan, K.E.; Lazarus, J.M.; Thadhani, R.; Hakim, R.M. Warfarin Use Associates with Increased Risk for Stroke in Hemodialysis Patients with Atrial Fibrillation. J. Am. Soc. Nephrol. 2009, 20, 2223–2233. [Google Scholar] [CrossRef] [PubMed]
- Mac-Way, F.; Poulin, A.; Utescu, M.S.; De Serres, S.A.; Marquis, K.; Douville, P.; Desmeules, S.; Larivière, R.; Lebel, M.; Agharazii, M. The impact of warfarin on the rate of progression of aortic stiffness in hemodialysis patients: A longitudinal study. Nephrol. Dial. Transplant. 2014, 29, 2113–2120. [Google Scholar] [CrossRef] [PubMed]
- Koos, R.; Krueger, T.; Westenfeld, R.; Kühl, H.P.; Brandenburg, V.; Mahnken, A.H.; Stanzel, S.; Vermeer, C.; Cranenburg, E.C.M.; Floege, J.; et al. Relation of circulating Matrix Gla-Protein and anticoagulation status in patients with aortic valve calcification. Thromb. Haemost. 2009, 101, 706–713. [Google Scholar]
- Giugliano, R.P.; Ruff, C.T.; Braunwald, E.; Murphy, S.A.; Wiviott, S.D.; Halperin, J.L.; Waldo, A.L.; Ezekowitz, M.D.; Weitz, J.I.; Špinar, J.; et al. Edoxaban versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2013, 369, 2093–2104. [Google Scholar] [CrossRef] [PubMed]
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151. [Google Scholar] [CrossRef] [PubMed]
- Granger, C.B.; Alexander, J.H.; McMurray, J.J.V.; Lopes, R.D.; Hylek, E.M.; Hanna, M.; Al-Khalidi, H.R.; Ansell, J.; Atar, D.; Avezum, A.; et al. Apixaban versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; Breithardt, G.; Halperin, J.L.; Hankey, G.J.; Piccini, J.P.; et al. Rivaroxaban versus Warfarin in Nonvalvular Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 883–891. [Google Scholar] [CrossRef] [PubMed]
- Shirani, J.; Alaeddini, J. Structural Remodeling of the Left Atrial Appendage in Patients with Chronic Non-Valvular Atrial Fibrillation. Cardiovasc. Pathol. 2000, 9, 95–101. [Google Scholar] [CrossRef]
- DeSimone, C.V.; Prakriti, B.G.; Tri, J.; Syed, F.; Sm, A.N.; Asirvatham, S.J. A Review Of The Relevant Embryology, Pathohistology, And Anatomy Of The Left Atrial Appendage For The Invasive Cardiac Electrophysiologist. J. Atr. Fibrillation 2015, 8, 1129. [Google Scholar] [CrossRef]
- Della Rocca, D.G.; Magnocavallo, M.; Van Niekerk, C.J.; Gilhofer, T.; Ha, G.; D’Ambrosio, G.; Mohanty, S.; Gianni, C.; Galvin, J.; Vetta, G.; et al. Prognostic value of chronic kidney disease in patients undergoing left atrial appendage occlusion. Europace 2023, 25, euad315. [Google Scholar] [CrossRef]
- Zhang, H.-F.; Zhang, Q.-X.; Zhang, Y.-Y.; Yang, D.; Xu, Z.; Jiao, Q.-B.; Zhang, X.-W. Efficacy and safety of left atrial appendage occlusion in atrial fibrillation patients with chronic kidney disease: A systematic review and meta-analysis. Rev. Cardiovasc. Med. 2020, 21, 443–451. [Google Scholar] [CrossRef]
- Genovesi, S.; Porcu, L.; Slaviero, G.; Casu, G.; Bertoli, S.; Sagone, A.; Buskermolen, M.; Pieruzzi, F.; Rovaris, G.; Montoli, A.; et al. Outcomes on safety and efficacy of left atrial appendage occlusion in end stage renal disease patients undergoing dialysis. J. Nephrol. 2021, 34, 63–73. [Google Scholar] [CrossRef]
- Fink, T.; Paitazoglou, C.; Bergmann, M.W.; Sano, M.; Keelani, A.; Sciacca, V.; Saad, M.; Eitel, C.; Heeger, C.; Skurk, C.; et al. Left atrial appendage closure in end-stage renal disease and hemodialysis: Data from a German multicenter registry. Cathet. Cardio. Interv. 2023, 101, 610–619. [Google Scholar] [CrossRef] [PubMed]
- Ueno, H.; Imamura, T.; Tanaka, S.; Ushijima, R.; Fukuda, N.; Kinugawa, K. Initial report of percutaneous left atrial appendage closure in hemodialysis patients with atrial fibrillation and high risk of bleeding in Japan. Cardiovasc. Interv. Ther. 2023, 38, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Alkhouli, M.; Ellis, C.R.; Daniels, M.; Coylewright, M.; Nielsen-Kudsk, J.E.; Holmes, D.R. Left Atrial Appendage Occlusion. JACC Adv. 2022, 1, 100136. [Google Scholar] [CrossRef]
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | Patient 8 | |
|---|---|---|---|---|---|---|---|---|
| Age | 86 | 83 | 81 | 85 | 78 | 80 | 74 | 64 |
| Sex | Male | Female | Male | Male | Male | Male | Male | Male |
| Hypertension | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Type 2 diabetes mellitus | No | No | No | No | No | Yes | No | Yes |
| Dyslipidemia | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Smoker | No | No | Yes | No | Yes | Former | Yes | Yes |
| Time on dialysis until LAAC (months) | 71 | 1 | 59 | 65 | 38 | 13 | 54 | 12 |
| CHA2DS2-VASc | 4 | 8 | 4 | 5 | 5 | 6 | 3 | 3 |
| HAS-BLED | 5 | 6 | 3 | 2 | 5 | 3 | 4 | 3 |
| Previous stroke | No | Yes | No | No | No | No | No | No |
| Previous bleeding | Yes | Yes | No | Yes | No | Yes | Yes | Yes |
| Hemorrhagic shock secondary to UGB | Hemodynamic instability secondary to GI bleeding | Labile INR | UGB | Anemia | GI and GU bleeding | Bleeding from dialysis vascular access | Hematuria, anemization | |
| Permanent AF | No | Yes | No | No | Yes | No | No | No |
| Persistent/paroxysmal AF | Yes | No | Yes | Yes | No | Yes | Yes | Yes |
| Heart failure | No | No | Yes | No | Yes | Yes | No | No |
| Ischemic heart disease | Yes | No | Yes | Yes | Yes | No | No | No |
| Previous treatment | ||||||||
| - VKAs | Yes | Yes | Yes | No | No | No | No | No |
| - DOACs | No | No | No | No | No | Yes (Apixaban 2.5 mg/12 h) | Yes (Apixaban 2.5 mg/12 h) | Yes (Apixaban 2.5 mg/12 h) |
| - DAPT | No | No | No | Yes | Yes | No | No | No |
| Left ventricular ejection fraction (%) | 50 | 60 | 30 | 33 | 51 | 59 | 60 | 60 |
| Left atrium area (cm2) | 50 | 45 | 48 | 38 | 39 | 21 | 32 | 30 |
| LAAC device | Watchman FLX 27 mm | Watchman Flx 24 mm | Watchman Flx 24 mm | Watchman Flx 24 mm | Watchman FLX 24 mm | Watchman FLX 24 mm | Watchman FLX 31 mm | Watchman FLX 24 mm |
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | Patient 8 | |
|---|---|---|---|---|---|---|---|---|
| Intervention success | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Follow-up (months) | 17 | 26 | 12 | 14 | 26 | 12 | …. | 10 |
| Major or minor bleeding (<30 days) | No | No | No | Yes | No | No | …. | No |
| Major or minor bleeding (>30 days) | No | No | No | No | No | No | … | No |
| Stroke (<30 days) | No | No | No | No | No | No | … | No |
| Stroke (>30 days) | No | No | No | No | No | No | … | No |
| Myocardial infarction | No | No | No | Yes | No | No | … | No |
| Thrombosis or leaks at 3-month control echocardiogram | No | No | No | Yes (leak < 3 mm) | No | No | … | No |
| Death | No | No | No | No | No | No | Yes | No |
| Post procedural treatment | ASA + clopidogrel 5 weeks | Clopidogrel | Acenocoumarol 2 months | ASA + clopidogrel | ASA + Clopidogrel | Apixaban 2.5 mg/12 h 2 months | ASA + clopidogrel | Apixaban 2.5 mg/12 h 2 months |
| Long-term therapy | ASA | Clopidogrel | ASA | ASA + clopidogrel | ASA | ASA | ASA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basabe, E.; De La Flor, J.C.; López de la Manzanara, V.; Nombela-Franco, L.; Narváez-Mejía, C.; Cruzado, L.; Villa, D.; Zamora, R.; Tapia, M.; Sastre, M.Á.; et al. Percutaneous Left Atrial Appendage Closure in Patients with Non-Valvular Atrial Fibrillation and End-Stage Renal Disease on Hemodialysis: A Case Series. Medicina 2024, 60, 231. https://doi.org/10.3390/medicina60020231
Basabe E, De La Flor JC, López de la Manzanara V, Nombela-Franco L, Narváez-Mejía C, Cruzado L, Villa D, Zamora R, Tapia M, Sastre MÁ, et al. Percutaneous Left Atrial Appendage Closure in Patients with Non-Valvular Atrial Fibrillation and End-Stage Renal Disease on Hemodialysis: A Case Series. Medicina. 2024; 60(2):231. https://doi.org/10.3390/medicina60020231
Chicago/Turabian StyleBasabe, Elena, José C. De La Flor, Virginia López de la Manzanara, Luis Nombela-Franco, Carlos Narváez-Mejía, Leónidas Cruzado, Daniel Villa, Rocío Zamora, Manuel Tapia, Miguel Ángel Sastre, and et al. 2024. "Percutaneous Left Atrial Appendage Closure in Patients with Non-Valvular Atrial Fibrillation and End-Stage Renal Disease on Hemodialysis: A Case Series" Medicina 60, no. 2: 231. https://doi.org/10.3390/medicina60020231
APA StyleBasabe, E., De La Flor, J. C., López de la Manzanara, V., Nombela-Franco, L., Narváez-Mejía, C., Cruzado, L., Villa, D., Zamora, R., Tapia, M., Sastre, M. Á., López Soberón, E., Herrero Calvo, J. A., Suárez, A., & Martí Sánchez, D. (2024). Percutaneous Left Atrial Appendage Closure in Patients with Non-Valvular Atrial Fibrillation and End-Stage Renal Disease on Hemodialysis: A Case Series. Medicina, 60(2), 231. https://doi.org/10.3390/medicina60020231







