Coronary Artery Occlusion with Sharp Blood Pressure Drop during General Anesthesia Induction: A Case Report
Abstract
1. Introduction
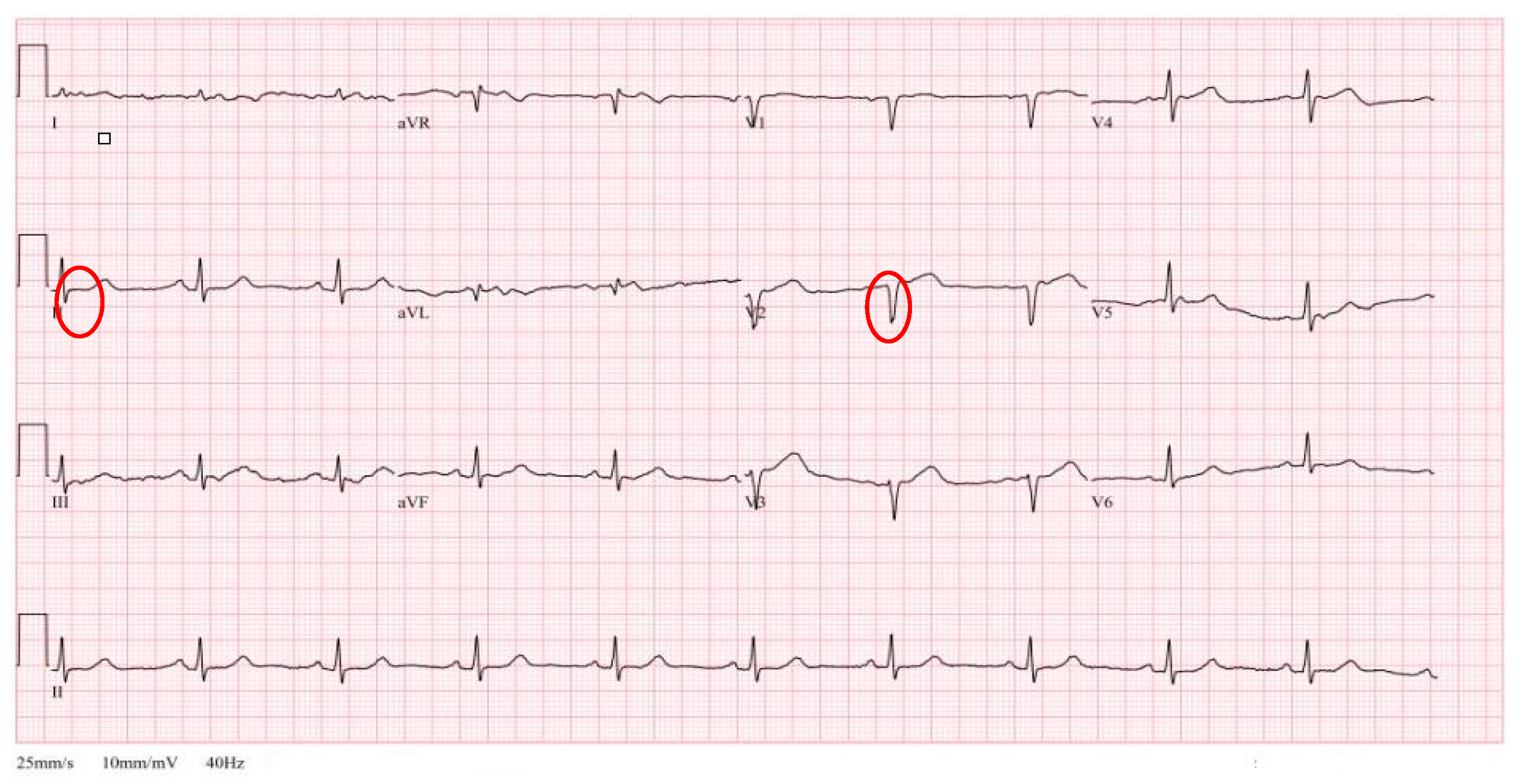
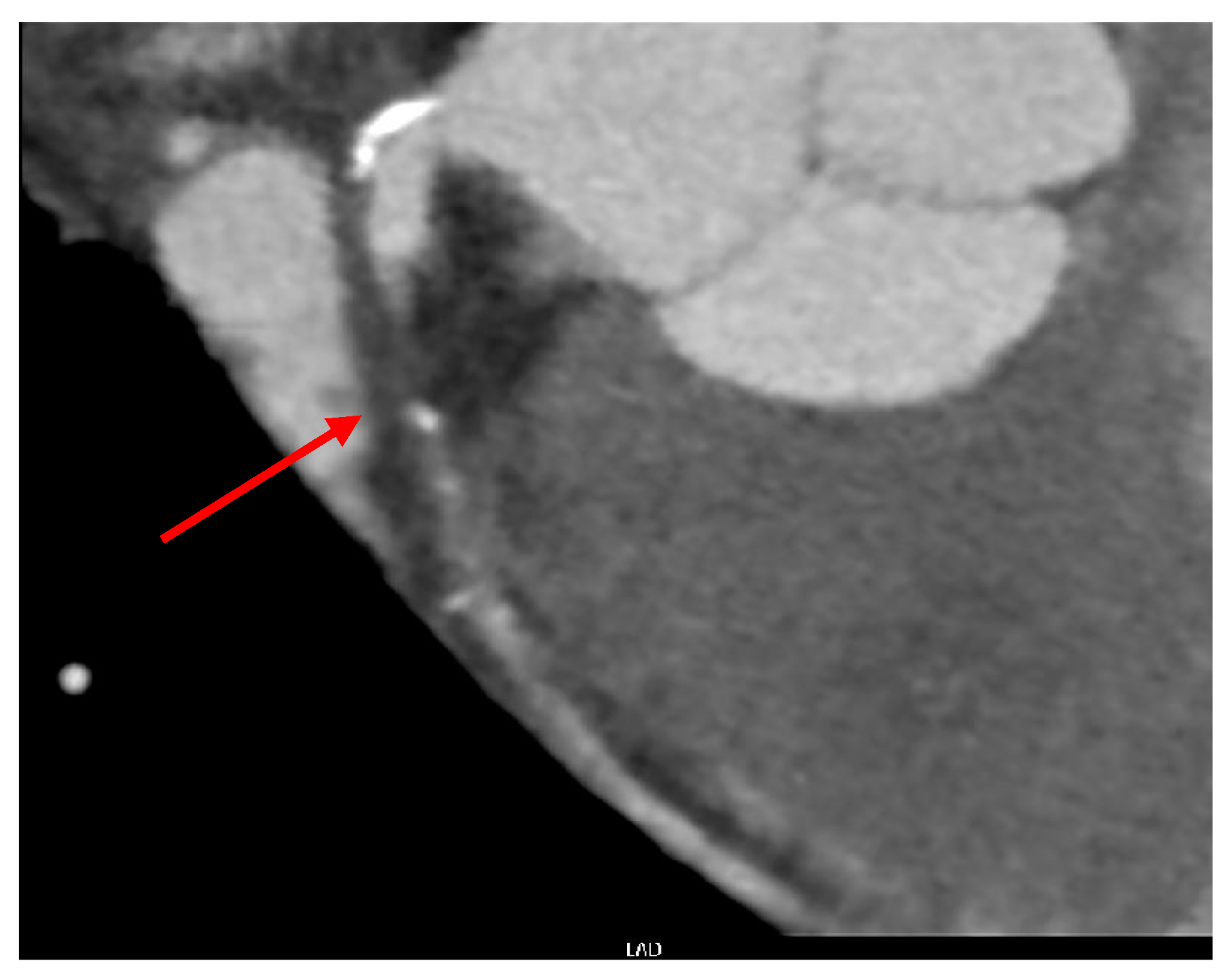
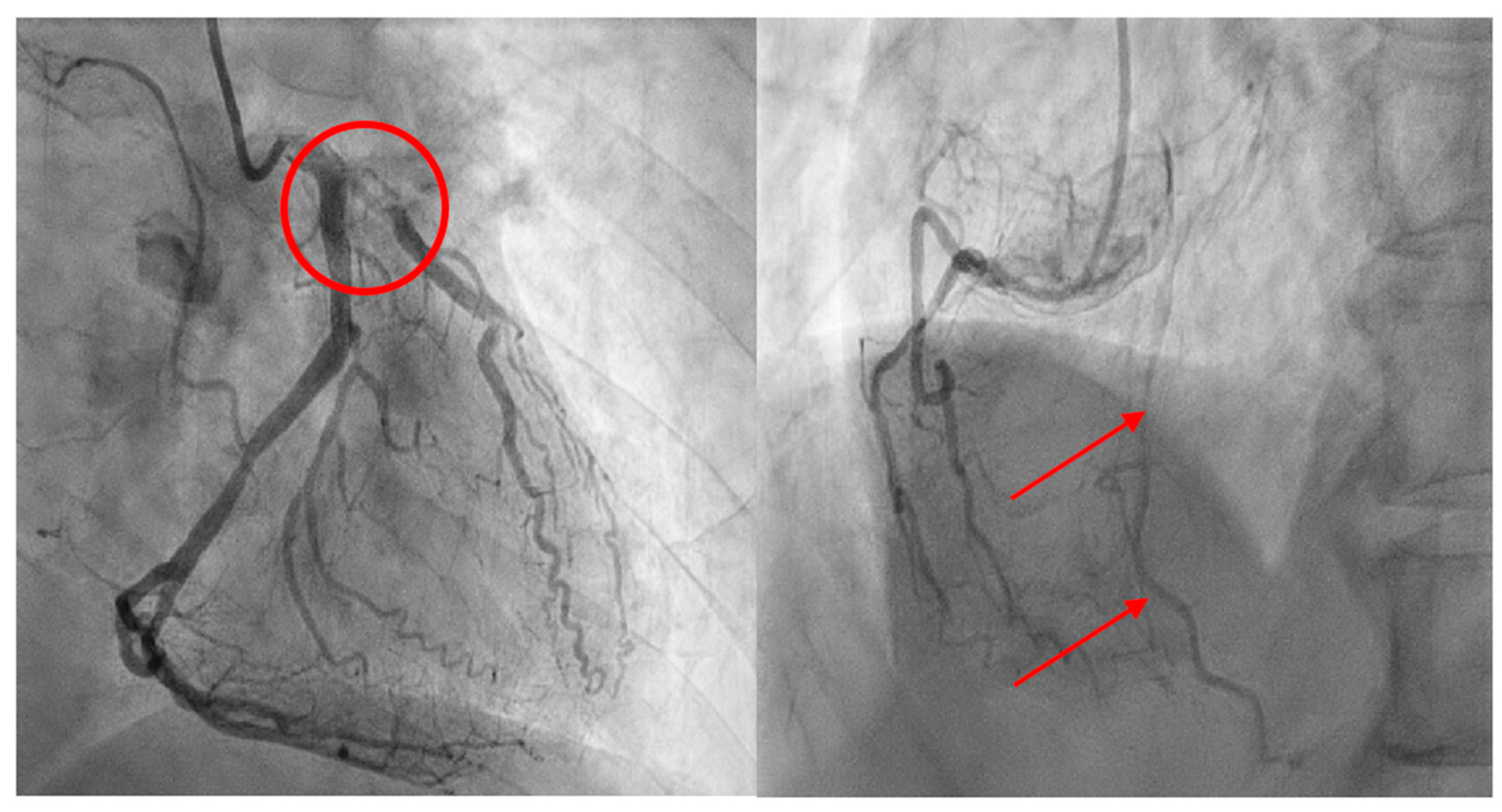
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dai, Z.-L.; Cai, X.-T.; Gao, W.-L.; Lin, M.; Lin, J.; Jiang, Y.-X.; Jiang, X. Etomidate vs. propofol in coronary heart disease patients undergoing major noncardiac surgery: A randomized clinical trial. World J. Clin. Cases 2021, 9, 1293–1303. [Google Scholar] [CrossRef]
- Rodgers, J.L.; Jones, J.; Bolleddu, S.I.; Vanthenapalli, S.; Rodgers, L.E.; Shah, K.; Karia, K.; Panguluri, S.K. Cardiovascular Risks Associated with Gender and Aging. J. Cardiovasc. Dev. Dis. 2019, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Ludders, J.W. Anesthesia for Patients with Dehydration/Hypovolemia. Vet. Clin. N. Am. Small Anim. Pract. 1992, 22, 495–496. [Google Scholar] [CrossRef] [PubMed]
- Dhakam, S.; Khalid, L. A Review of Cardiogenic Shock in Acute Myocardial Infarction. Curr. Cardiol. Rev. 2008, 4, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Martin, T.; Bhaskar, Y.; Umesh, K. Sensitivity and specificity of the electrocardiogram in predicting the presence of increased left ventricular mass index on the echocardiogram in Afro-Caribbean hypertensive patients. West Indian Med. J. 2007, 56, 134. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Deng, H.-M.; Chen, H.-Y.; Tang, S.-H.; Deng, F.; Lu, Y.-G.; Song, J.-C. The Impact of Age on Propofol Requirement for Inducing Loss of Consciousness in Elderly Surgical Patients. Front. Pharmacol. 2022, 13, 739552. [Google Scholar] [CrossRef] [PubMed]
- Flegal, M.C.; Fox, L.K.; Kuhlman, S.M. Principles of anesthesia monitoring and electrocardiogram. J. Investig. Surg. 2009, 22, 316–317. [Google Scholar] [CrossRef] [PubMed]
- Noel-Morgan, J.; Muir, W.W. Anesthesia-Associated Relative Hypovolemia: Mechanisms, Monitoring, and Treatment Considerations. Front. Veter. Sci. 2018, 5, 53. [Google Scholar] [CrossRef]
- Wolff, C.B.; Green, D.W. Clarification of the circulatory patho-physiology of anaesthesia—Implications for high-risk surgical patients. Int. J. Surg. 2014, 12, 1348–1356. [Google Scholar] [CrossRef]
- Rixen, D.; Siegel, J.H. Bench-to-bedside review: Oxygen debt and its metabolic correlates as quantifiers of the severity of hemorrhagic and post-traumatic shock. Crit. Care 2005, 9, 441–453. [Google Scholar] [CrossRef][Green Version]
- Miller, T.E.; Myles, P.S. Perioperative Fluid Therapy for Major Surgery. Anesthesiology 2019, 130, 825–832. [Google Scholar] [CrossRef]
- Farhan, M.; Hoda, M.Q.; Ullah, H. Prevention of hypotension associated with the induction dose of propofol: A randomized controlled trial comparing equipotent doses of phenylephrine and ephedrine. J. Anaesthesiol. Clin. Pharmacol. 2015, 31, 526–530. [Google Scholar] [CrossRef] [PubMed]
- Soh, S.; Song, J.W.; Choi, N.; Shim, J.-K. Anesthetic-induced myocardial protection in cardiac surgery: Relevant mechanisms and clinical translation. Anesth. Pain Med. 2018, 13, 1–9. [Google Scholar] [CrossRef]
- Meier, P.; Schirmer, S.H.; Lansky, A.J.; Timmis, A.; Pitt, B.; Seiler, C. The collateral circulation of the heart. BMC Med. 2013, 11, 143. [Google Scholar] [CrossRef] [PubMed]
- Habib, G.B.; Heibig, J.; Forman, A.S.; Brown, B.G.; Roberts, R.; Terrin, M.L.; Bolli, R. Influence of coronary collateral vessels on myocardial infarct size in humans. Results of phase I thrombolysis in myocardial infarction (TIMI) trial. The TIMI Investigators. Circulation 1991, 83, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Castellano, N.; García, E.J.; Abeytua, M.; Soriano, J.; Serrano, A.J.; Elízaga, J.; Botas, J.; López-Sendón, J.L.; Delcán, J.L. Influence of Collateral Circulation on In-Hospital Death From Anterior Acute Myocardial Infarction. J. Am. Coll. Cardiol. 1998, 31, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Kaul, S. Assessment of Myocardial Collateral Blood Flow with Contrast Echocardiography. Korean Circ. J. 2015, 45, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Saraon, T.; Chadow, H.L.; Castillo, R. The power of collateral circulation: A case of asymptomatic chronic total occlusion of the left main coronary artery. J. Invasive Cardiol. 2012, 24, E196–E198. [Google Scholar]
- Hedge, J.; Balajibabu, P.; Sivaraman, T. The patient with ischaemic heart disease undergoing non cardiac surgery. Indian J. Anaesth. 2017, 61, 705–711. [Google Scholar] [CrossRef]
- Fadah, K.; Hechanova, A.; Mukherjee, D. Epidemiology, Pathophysiology, and Management of Coronary Artery Disease in the Elderly. Int. J. Angiol. 2022, 31, 244–250. [Google Scholar] [CrossRef]
- Gilstrap, L.G.; Bhatia, R.S.; Weiner, R.B.; Dudzinski, D.M. Dobutamine stress echocardiography: A review and update. Res. Rep. Clin. Cardiol. 2014, 5, 69–81. [Google Scholar] [CrossRef][Green Version]
- Poldermans, D.; Fioretti, P.M.; Forster, T.; Thomson, I.R.; Boersma, E.; El-Said, E.M.; du Bois, A.N.; Roelandt, J.R.; van Urk, H. Dobutamine stress echocardiography for assessment of perioperative cardiac risk in patients undergoing major vascular surgery. Circulation 1993, 87, 1506–1512. [Google Scholar] [CrossRef] [PubMed]
- Yagi, Y.; Mizunoya, K.; Mori, T.; Saito, H.; Morimoto, Y. Intraoperative myocardial infarction and refractory cardiogenic shock during major hepatectomy: A case report. JA Clin. Rep. 2022, 8, 19. [Google Scholar] [CrossRef] [PubMed]
- Kipri, M.; Enes, S.A.; Çalışkan, E.; Karsli, A.; Aribogan, A. Sudden cardiac arrest during general anesthesia in a patient with no cardiovascular disease. Resuscitation 2019, 142, e44–e45. [Google Scholar] [CrossRef]
- Kurdi, M.; Theerth, K.; Deva, R. Ketamine: Current applications in anesthesia, pain, and critical care. Anesth. Essays Res. 2014, 8, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Valk, B.I.; Struys, M.M.R.F. Etomidate and its Analogs: A Review of Pharmacokinetics and Pharmacodynamics. Clin. Pharmacokinet. 2021, 60, 1253–1269. [Google Scholar] [CrossRef]
- Jakobsen, C.; Torp, P.; Vester, A.E.; Folkersen, L.; Thougaard, A.; Sloth, E. Ketamine reduce left ventricular systolic and diastolic function in patients with ischaemic heart disease. Acta Anaesthesiol. Scand. 2010, 54, 1137–1144. [Google Scholar] [CrossRef]
- Kawasaki, S.; Kiyohara, C.; Tokunaga, S.; Hoka, S. Prediction of hemodynamic fluctuations after induction of general anesthesia using propofol in non-cardiac surgery: A retrospective cohort study. BMC Anesthesiol. 2018, 18, 167. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, S.H.; Shim, S.H.; Kim, J.S.; Kwak, S.D.; Kim, C.S.; Ahn, K.R. Effects of Etomidate, Propofol and Thiopental Sodium on Intraocular Pressure during the Induction of Anesthesia. Korean J. Anesthesiol. 2000, 39, 309–313. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ji, J.Y.; Seo, Y.H.; Jung, H.S.; Chun, H.R.; Park, J.S.; Kim, W.J.; Ahn, J.M.; Park, Y.J.; Shin, Y.E.; Park, C.H. Coronary Artery Occlusion with Sharp Blood Pressure Drop during General Anesthesia Induction: A Case Report. Medicina 2024, 60, 232. https://doi.org/10.3390/medicina60020232
Ji JY, Seo YH, Jung HS, Chun HR, Park JS, Kim WJ, Ahn JM, Park YJ, Shin YE, Park CH. Coronary Artery Occlusion with Sharp Blood Pressure Drop during General Anesthesia Induction: A Case Report. Medicina. 2024; 60(2):232. https://doi.org/10.3390/medicina60020232
Chicago/Turabian StyleJi, Jae Young, Yong Han Seo, Ho Soon Jung, Hea Rim Chun, Jin Soo Park, Woo Jong Kim, Jae Min Ahn, Yu Jun Park, Ye Eun Shin, and Chan Ho Park. 2024. "Coronary Artery Occlusion with Sharp Blood Pressure Drop during General Anesthesia Induction: A Case Report" Medicina 60, no. 2: 232. https://doi.org/10.3390/medicina60020232
APA StyleJi, J. Y., Seo, Y. H., Jung, H. S., Chun, H. R., Park, J. S., Kim, W. J., Ahn, J. M., Park, Y. J., Shin, Y. E., & Park, C. H. (2024). Coronary Artery Occlusion with Sharp Blood Pressure Drop during General Anesthesia Induction: A Case Report. Medicina, 60(2), 232. https://doi.org/10.3390/medicina60020232







